Abstract
Purpose of Review
Hemoptysis is an important symptom, which can be potentially life-threatening in some cases. Presence of hemoptysis necessitates a prompt and comprehensive evaluation so as to determine the underlying abnormality in the pulmonary parenchyma and/or thoracic vasculature. This would facilitate initiation of timely and accurate management.
Recent Findings
Mutli-detector row computed tomographic angiography (MDCT angiography) is a non invasive imaging tool, which provides all-inclusive information about the pulmonary parenchyma, airways and lung vasculature, correctly identifies the cause and site of bleeding in majority of the patients and serves as a guide for further management.
Summary
MDCT angiography an extremely useful imaging modality in initial evaluation of patients with hemoptysis and should be an integral part of preliminary assessment of all such cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hemoptysis is defined as expectoration of blood from lower respiratory tract, i.e., from tracheo-bronchial tree or the pulmonary parenchyma [1, 2]. It occurs in wide variety of conditions and is a clinical entity encountered commonly in patients attending chest clinics. In majority of the cases (approximately 90–95% cases), hemoptysis results from hypervascularity of lung parenchyma by bronchial and non-bronchial systemic arteries, while bleeding from pulmonary artery origin is rare (approximately 5–10% cases) [3–5].
Clinical assessment of patients with hemoptysis should take into account the volume of blood expectorated in a 24-h period and patient’s cardio respiratory reserves [1]. Majority of patients with mild or moderate hemoptysis can be managed conservatively. Hemoptysis is considered massive if there is more than 300 mL of blood loss over a period of 24 h [6]. Expectorated blood in large volumes can cause flooding of the airways leading to asphyxia, which is usually the cause of death in patients with severe hemoptysis, rather than blood loss [7] and conservative treatment of massive hemoptysis carries a very high mortality of 50–100% [6]. As a result, it is imperative to promptly identify the cause and site of bleeding so as to initiate an adequate treatment to avoid lethal complications. Imaging, especially with multi-detector CT angiogram (CTA) of chest plays an essential role in management of patients with hemoptysis.
Multi-detector CT angiogram provides an excellent, rapid, non-invasive, and comprehensive evaluation of the entire thorax in patients with hemoptysis, allowing clear depiction of the tracheo-bronchial tree, pulmonary parenchyma, and the lung vasculature in a single examination. It helps in identifying the cause of hemoptysis and localize the site of bleeding, as it provides a precise depiction of the bronchial arteries and non-bronchial systemic arteries [3, 8, 9] and also forms a basis for subsequent planning of therapeutic options (conservative, endovascular, or surgery) in such patients. Moreover, CT is superior to fiberoptic bronchoscopy in finding a cause of hemoptysis [10], and is currently considered a standard part of care in initial assessment of these patients [5].
In this article, we review the causes and pathophysiologic principles of hemoptysis, discuss the anatomy of the systemic arteries responsible for bleeding, and deliberate the utility of multi-detector CT in identification of these ‘culprit’ vessels and assessment of lung parenchyma in such patients.
Causes of Hemoptysis
Hemoptysis is usually caused by various pulmonary (parenchymal or airway) or cardiovascular diseases. List of main causes of hemoptysis is presented in Table 1 [1, 11•, 12]. Common causes of bleeding include pulmonary tuberculosis, bronchiectasis, pneumonia, lung cancer, pulmonary hypertension, and fungal infections [2, 13]. Bleeding in hemoptysis, may arise from small or large vessels [11•]. Bleeding from large vessels usually occurs in infectious diseases like active pulmonary tuberculosis, lung abscess, and fungal infections or in cardiovascular conditions such as arteriovenous malformations, bronchovascular fistulas, pulmonary embolism, and infarction. Neoplastic conditions including primary lung malignancies, bronchial adenoma, and lung metastasis are other known causes of large vessel hemoptysis [14]. Hemoptysis from small vessels usually occurs in immunologic and vasculitic disorders like Behçet disease, Wegner’s granulomatosis etc., and in various coagulatory diseases. Approximately 3–30% of cases with hemoptysis, may remain without an identified etiology, and are termed as cryptogenic hemoptysis [1, 8, 11•]. Large proportions of these patients are smokers. It is important to keep these patients on close follow-up and repeat CT examination after few months to look for an occult neoplasm [1]. A decrease in prevalence of cryptogenic hemoptysis is expected as more and more MDCT examinations are performed worldwide, in evaluation of patients with hemoptysis.
Pathophysiological Principles of Hemoptysis
Lung parenchyma has a dual arterial supply, from the pulmonary arteries and the bronchial arteries. Pulmonary arteries which provide 99% of the blood to the lung parenchyma, carry deoxygenated blood at a low pressure and take part in gas exchange [11•, 15•]. Bronchial arteries on the other hand provide remaining 1% of the blood supply. They carry oxygenated blood to the lungs, at a higher pressure and provide nourishment to the supporting structures of the lungs, namely: extra and intrapulmonary airways, vasa vasorum of pulmonary arteries, veins and aorta, and also to the mediastinal lymph nodes and visceral pleura. Bronchial arteries do not take part in gas exchange [7, 11•, 15•]. These two vascular systems are connected to each other through several complex capillary anastomoses at the level of alveoli and bronchioles [1, 11•].
In situations where pulmonary arterial supply is reduced (e.g., vasculitis or chronic thrombo-embolism), bronchial arteries undergo a compensatory hypertrophy and dilatation in order to maintain blood flow to the lung [1, 11•, 15•]. Similarly in neoplastic conditions and chronic inflammatory disorders (e.g., bronchiectasis and tuberculosis), there is release of angiogenic growth factors, which results in increase in the systemic arterial supply to the lungs. As a result, bronchial and/or non-bronchial systemic arterial neovascularization occurs. Hypertrophied bronchial arteries and these newly formed systemic vessels have thin walls, are fragile, and prone to rupture as they are exposed to systemic arterial pressure [1, 11•]. They tend to break in their distal segments, either in terminal bronchiole or alveoli, resulting in hemoptysis [12].
Visualization of dilated bronchial and/or non-bronchial systemic artery at imaging should prompt a radiologist to look for various associated disorders.
Imaging Protocol on MDCT
Currently available MDCT scanners with 16 row detector configuration and above, provide a faster, isotropic imaging of the entire thorax with excellent spatial resolution in a single breath hold [8, 11•]. CT images provide complete assessment of tracheo-bronchial tree and lung parenchyma, while post-contrast images also reveal an accurate, non-invasive, high-resolution, angiographic detail of the origin and course of bronchial and non-bronchial systemic arteries which are an important source of bleeding in patients with hemoptysis.
Multi-detector Row CT-Technique
MDCT image acquisition in patients with hemoptysis should extend from inferior portion of neck, to the level of renal arteries, in craniocaudal direction, in order to include the supra-aortic great vessels and the infra-diaphragmatic arteries, which may be a source of collateral vessels to the lung, in a single breath hold [1, 11•]. Post-contrast angiographic images are obtained after injecting 70–80 mL of high density, non-ionic iodinated contrast (Iohexol 350 mg of iodine per milliliter), at high flow rate (e.g., 4 mL/s), through an 18-gage intravenous cannula, placed in the antecubital vein or through a central venous line, followed by 30–40 mL of saline flush using a dual-head pressure injector [15•, 16]. To ensure accuracy in the timing of arterial phase images, real-time bolus tracking should be used with region of interest (ROI) placed in descending thoracic aorta, typically at 150 Hounsfield units (HU).
Scanning must be performed using low dose acquisition methods like automated tube current modulation with fast gantry rotation speeds (400 ms or less). These, in combination with iterative reconstruction protocols, present in all currently available multi-slice systems and help in significantly reducing radiation dose to the patients [7].
Data Manipulation/Image Reconstruction
Post-contrast images need to be reconstructed at 1 mm slice thickness with a reconstruction interval of 0.8 mm, giving at least 20% overlap. MDCT angiography raw data images should be evaluated on dedicated workstations with all post-processing capabilities. Assessment of lung parenchyma must be done as in routine CT chest examinations using lung window settings (window center, −600 HU; window width, 1600HU) [8]. Origins of bronchial arteries are best depicted on thin-section axial images, using mediastinal soft tissue window settings (window center, 50HU; window width, 350 HU). Two-dimensional multiplanar (MPR) images and maximum intensity projection (MIP) reformations in oblique and coronal planes are best to depict the tortuous course of bronchial and non-bronchial arteries from their origin to the lung parenchyma [11•, 17]. Slice thickness, plane, and degree of obliquity may vary on an individual case to case basis [12, 17]. Three dimensional volume rendered (VR) post-processed images depict the anatomy of the hypertrophied vessels in relation to surrounding structures and can provide a “road map” for planning surgical or endovascular treatment [11•].
Images that appear in this article have been obtained on a 64 slice and 160 slice MDCT scanners (Aquilion 64 & Aquilion Prime, Toshiba Medical Systems, Japan). All the post-processed images have been created on a commercially available dedicated CT workstation (Vitrea; Vital Images Inc, Minn, USA).
CT Assessment of Lung Parenchyma
Evaluation of CT images in patients with hemoptysis should begin with assessment of tracheo-bronchial tree and pulmonary parenchyma to look for possible cause of bleeding and localize the site of hemorrhage in lung window settings. MDCT is considered superior to fiberoptic bronchoscopy (FOB) in localizing the site of bleeding with accuracy rates of 63–100%, as it has the ability to evaluate distal airways beyond the reach of the bronchoscope [6, 11•]. Causes of hemoptysis like bronchiectasis, lung infections (tuberculosis and mycetoma), endobronchial, and pulmonary malignancies can be easily identified on lung window settings (Fig. 1) [1]. Bleeding within the lung parenchyma can produce ground glass opacities and/or alveolar consolidation which are not gravity dependent (Fig. 2) [4, 12]. Clots can also be present within the bronchial lumen, producing distal atelectasis (Fig. 3) [8]. Presence of clots in the bronchial lumen can mask small endobronchial tumors and it is advisable to follow up these patients with repeat scans after the episode of hemoptysis [1]. Whenever pulmonary findings are unilateral or located in one lobe, it becomes easy to identify the bleeding site. CT is however less accurate in localizing the site of bleeding whenever pulmonary changes are diffuse or bilateral [8, 11•]. It is very rare to observe extravasation of contrast into the bronchial lumen [4].
a–d Bronchial carcinoid presenting with hemoptysis. Axial (a) and coronal (b) thin-section MDCT images at parenchymal window settings and post-contrast MIP axial (c) and coronal (d) images in mediastinal window settings reveal an endobronchial lesion (arrows), partially obliterating the right upper lobe and right main bronchus, with partial collapse of distal right upper lobe lung segments. Obstructive over-inflation of right lower lobe is also noted (star)
a, b Axial thin-section MDCT obtained with parenchymal window settings in patient with hemoptysis demonstrates ground glass opacities in right lower lobe (arrows), consistent with areas of alveolar hemorrhage with bronchial impaction from blood clots in subsegmental branches of right lower lobe bronchi (arrowheads)
In addition images must be viewed on mediastinal window settings to look for enlarged lymph nodes and presence of any pleural disease.
CT Depiction and Analysis of Bronchial Arteries
Bronchial Artery Anatomy
Bronchial arteries are the most common source of bleeding in over 90% of patients with hemoptysis [1, 11•]. They are small vessels that usually arise directly from the descending thoracic aorta. CT is an excellent modality to depict bronchial artery anatomy and variants [5]. Bronchial arteries can be visualized in the posterior mediastinum, on post-contrast CT images, as tiny dot-like, nodular, or linear structures with an undulating course, having density equal to that of the aorta (Fig. 4). In about 70% of individuals, bronchial arteries arise from descending aorta, between the superior endplate of T5 vertebral body and the inferior endplate of T6 vertebral body (approximately in region of carina) and are termed as orthotopic bronchial arteries [12, 15•]. In remaining 30% of cases, bronchial arteries originate elsewhere from aorta or from other systemic arteries and are termed as ectopic bronchial arteries. Most common sites of origin of ectopic bronchial arteries are inferior surface of aortic arch, distal descending thoracic aorta, subclavian arteries, brachiocephalic artery, and internal mammary arteries [7, 15•]. Both orthotopic and ectopic bronchial arteries enter the lung parenchyma through the pulmonary hilum and run parallel to the bronchovascular bundle. Ectopic origin of the bronchial artery is an important cause of endovascular treatment failure as these vessels can get overlooked on catheter angiogram studies [8, 10]. Depiction of origin and course of ectopic bronchial arteries on MDCT angiogram, before an interventional procedure, can help in providing a road map to the treating interventionist.
Bronchial arteries also have high variability in their branching pattern and course [6]. One or two bronchial arteries can be seen supplying the lung parenchyma on each side and may arise independently from aorta, or as a common trunk [1]. In the most frequent pattern, seen in 80% of cases, right bronchial artery shares its origin with an intercoastal artery [11•], a finding commonly termed as right intercostobronchial trunk (ICBT), arising from the medial wall of aorta [5, 6]. Left bronchial artery in most situations arises directly from the aorta, usually from its anterior wall [15•] and in 70% cases two left bronchial arteries are noted [1]. Left bronchial arteries have a short mediastinal course as compared to the right. Because of the well-known individual variability in the number of bronchial arteries, it is useful to be aware of the number of bronchial arteries ipsilateral to the side of bronchial bleeding prior to embolization.
A normal bronchial artery on CT images has a diameter of 1.5 mm at point of its origin and gradually tapers as it enters the lung hilum, measuring almost 0.5 mm at this site [11•, 18].
Abnormal Bronchial Arteries-“The culprit vessel”
Bronchial arteries are considered abnormal and a possible source of hemoptysis, when bronchial artery is dilated and hypertrophied, measuring >2 mm in diameter, with a very tortuous mediastinal course and does not taper from the point of its origin at aorta till the pulmonary hilum [12, 15•]. Bronchial arteries which can be traced in their entire length from the point of origin till the entry into the lung hilum are more likely to be associated with hemoptysis (Fig. 5). MDCT angiogram is an excellent non-invasive modality to depict the trajectories of the dilated bronchial arteries from point of their origin till the lung parenchyma. This traceability of bronchial arteries is considered to be a better marker in identifying the “culprit vessel” causing hemoptysis rather than bronchial artery dilatation alone (Fig. 6) [18]. Dilated bronchial arteries can also be visualized on CT angiogram images in lung parenchymal opacities close to the pulmonary hilum. Bronchial artery aneurysms can also present as hemoptysis and usually result secondary to bronchial artery hypertrophy. They are a rare entity with reported incidence of <1% in patients undergoing selective bronchial artery catheter angiograms [19]. The most specific sign of bronchial bleeding however is extravasation of contrast, which is rarely observed on CT images [4].
a, b Coronal oblique post-contrast MIP reformatted images reveal hypertrophied orthotopic (a) and ectopic (b) right bronchial arteries. Entire tortuous course of these dilated vessels can be traced (arrows) from their point of origin at proximal descending aorta (a) and from the inferior surface of aortic arch (b), till the entry into the pulmonary hilum
a–d Post-contrast coronal oblique MIP reformatted images (a, b) in a patient with hemoptysis. Dilated orthotopic (a) right bronchial artery is seen (arrow) along with a dilated ectopic right bronchial artery (b) rising from proximal segment of right subclavian artery (arrow), entering into the right hilum. Multiple small calcified mediastinal nodes are also noted. Catheter angiogram images confirm distal parenchymal blush (arrows) from hypertrophied orthotopic (c) and ectopic (d) bronchial arteries
CT Depiction of Non-bronchial Systemic Arteries
Non-bronchial systemic arteries are also observed as a source of bleeding in significant number of patients with hemoptysis, with incidence of 11–40% in various studies [5, 10]. Arterial supply to the lung parenchyma from systemic non-bronchial arteries is also one of the major causes of recurrent hemoptysis in immediate post-procedure period, even after successful embolization of bronchial arteries. These non-bronchial systemic collaterals do not enter the pulmonary parenchyma through the hilum and their course is not parallel to the bronchi. These vessels usually enter the lung through the pleura or the inferior pulmonary ligament [17]. Most common branches that extend into the lung parenchyma as extra-bronchial collaterals arise from subclavian arteries, internal mammary vessels, pulmonary ligament arteries, intercoastal, and inferior phrenic arteries [4, 17]. The vessels are typically observed as dilated structures in the extra-pleural fat, and are usually associated with pleural thickening of more than 3 mm with an underlying lung abnormality (Fig. 7) [8, 9]. Axial MIP images of MDCT angiogram studies are best to depict the presence of dilated intercoastal arteries in extra-pleural fat, while course and trajectory of internal mammary and phrenic arteries is best appreciated on oblique axial or coronal MIP reformats. It is important that scanning of patients with hemoptysis is performed with an extended coverage from lower neck till the upper abdomen, to cover the origin and course of these systemic arteries, which can be a source of bleeding in such cases. In few cases, bleeding from bronchial arteries can coexist with bleeding from non-bronchial and pulmonary arteries as well in the same patient (Fig. 8) [20].
a–d Axial non-contrast high-resolution CT image (a) from a patient with hemoptysis shows an area of bronchiectasis in left upper lobe. Post-contrast axial MIP oblique image (b) reveals a dilated non-bronchial systemic artery from left internal mammary artery (LIMA) extending directly into the diseased lung parenchyma. Selective catheter angiogram (c) confirms the CT findings (arrow) and coil embolization (d) of the vessel is performed (arrow)
a-c Coronal non-contrast high-resolution CT image (a) shows extensive bronchiectasis and volume loss in right lung parenchyma. Post-contrast oblique coronal reformatted MIP images (b, c) reveal dilated orthotopic right bronchial artery (yellow arrow), ectopic right bronchial artery from right subclavian artery (white arrow), and right inferior phrenic artery (dark arrowheads), entering the lung parenchyma. Patient underwent right pneumonectomy for massive hemoptysis (Color figure online)
CT Assessment of Pulmonary Arteries
Although pulmonary arteries are an uncommon source of bleeding in patients presenting with hemoptysis, accounting for 5–10% of cases, careful assessment of pulmonary arterial circulatory pathway should always be performed [6, 11•, 12]. Presence of a pulmonary arterial abnormality in patients with hemoptysis completely changes the management schedule. MDCT angiogram with its multiplanar reconstruction capabilities can exquisitely demonstrate the pulmonary arterial vasculature and its pathologies. Most common causes of hemoptysis due to a pulmonary arterial disease include thrombo-embolism, pulmonary artery pseudo-aneurysms (Rasmussen aneurysm), vasculitis, invasion of pulmonary artery by neoplasm, and arteriovenous fistulas (Fig. 9) [5, 11•]. Acute thrombo-embolism and lung infarcts are frequent causes of non-massive hemoptysis that require urgent anticoagulation [1]. Bronchial artery dilatation which occurs in patients with chronic pulmonary embolism as a compensatory mechanism, may be responsible for bleeding, however embolization of these vessels is justified only in cases of life-threatening hemoptysis (Fig. 10) [5]. Pulmonary artery pseudo-aneurysms typically develop in wall of tubercular cavities or in areas of bronchiectasis and parenchymal destruction secondary to an infective or a neoplastic disease (Fig. 11). Rarely bronchial artery to pulmonary artery fistulas may develop after chronic inflammatory lung diseases usually related to systemic hypervascularization and is not a major CT sign for bleeding site (Fig. 12). Pulmonary vasculitis (Takayasu’s arteritis or Behçet’s disease) are also uncommon but important causes of hemoptysis. Behçet’s disease is a multi-systemic chronic inflammatory disorder of unknown etiology with involvement of the vascular system in 25–30% of cases [21]. Patients typically present with oral/genital ulcers in majority of cases. Venous/arterial occlusion and arterial aneurysms are the most frequent vascular complications [22] (Fig. 13).
a-c Pulmonary arteriovenous malformation (PAVM). Non-contrast axial (a) images reveal large area of alveolar consolidation in left lower lobe, suggesting pulmonary hemorrhage in a patient with hemoptysis. Post-contrast coronal MIP (b) and volume rendered (c) CT images show lobulated intensely enhancing serpiginous mass in relation to the left lower lobe pulmonary vessels, representing an aneurysmal PAVM
a-d Pulmonary thrombo-embolism. Coronal (a), axial (b) and oblique coronal MIP images (c, d) CT angiogram images. Acute thrombus is seen in right lower lobe pulmonary artery (white arrows in image a, b). Linear hypodense filling defect is also seen along the wall of left lower lobe pulmonary artery branch (yellow arrow in a), with a reduced vessel caliber, representing a chronic thrombus. Dilated orthotopic bronchial artery (blue arrows in image b, c), ectopic bronchial artery from LIMA (arrow in image d) and dilated intercoastal and phrenic arteries (arrowheads in image b, c) are seen on the left side secondary to left sided chronic pulmonary embolism (Color figure online)
a–c High-resolution CT image (a) in a case of massive hemoptysis, shows destroyed left lung with fibrocavitary lesions (arrows). Coronal CT angiography image (b) and selective catheter angiogram of left pulmonary artery reveal focal dilatation in distal left lower lobe pulmonary artery branch (arrow), suggesting pulmonary artery pseudo-aneurysm
a–d Non-contrast axial CT image (a) reveals fibro-bronchiectatic changes in upper lobes of both lungs, more marked on right. Post-contrast oblique coronal MIP images (b) from CT pulmonary angiographic phase reveal non-filling of a distal right upper lobe pulmonary artery branch (arrow). Oblique coronal MIP images from CT aortic angiographic phase (c, d) reveal dilated right bronchial artery (arrow in c), with reflux of contrast into right upper lobe pulmonary artery branch (arrow in d), suggesting presence of a systemic artery to pulmonary artery fistula
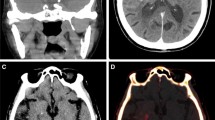
a–d Behçet disease with hemoptysis. Axial CT angiography images (a) reveal a pseudo-aneurysm in the descending aorta (arrow). Lung window settings at the same axial level (b) show a peripherally placed parenchymal opacity (arrow) in left lower lobe, representing a pulmonary infarct. Coronal MIP images (c, d) reveal multiple filling defects in distal right lower lobe (arrow in c) and left lower lobe (arrow in d) pulmonary artery branches, consistent with pulmonary embolism. Pulmonary infarct is also appreciated in territory of left pulmonary artery branches (arrowhead in d). Dilatation of right bronchial artery is also noted (block arrow in c)
Conclusions
MDCT angiography is a very useful method in evaluation of patients with hemoptysis as it correctly identifies the site and cause of bleeding in majority of the cases. MDCT angiography with its multiplanar reconstruction capabilities provides a rapid, non-invasive, detailed depiction of the lung parenchyma, pulmonary airways, and abnormal pulmonary/systemic vasculature, responsible for hemoptysis and helps in guiding further management in such cases. MDCT angiogram images serve as a road map for the interventional radiologist and/or for the thoracoscopic surgeon, increasing the overall efficiency of these procedures and improving the patient outcome.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Bruzzi JF, Rémy-Jardin M, Delhaye D, Teisseire A, Khalil C, Rémy J. Multi-detector row CT of hemoptysis. RadioGraphics. 2006;26:3–22. doi:10.1148/rg.261045726.
Davoodi M, Kordi M, Gharibvand MM, Shoushtari MH, Borsi H, Bahadoram M. Hemoptysis: comparison of diagnostic accuracy of multi detector CT Scan and bronchoscopy. Glob J Health Sci. 2015;7(3):9736–44. doi:10.5539/gjhs.v7n3p373.
Khalil A, Fartoukh M, Parrot A, Bazelly B, Marsault C, Carette MF. Impact of MDCT angiography on the management of patients with hemoptysis. AJR. 2010;195:772–8. doi:10.2214/AJR.09.4161.
Khalil A, Fartoukh M, Tassart M, Parrot A, Marsault C, Carette MF. Role of MDCT in identification of the bleeding site and the vessels causing hemoptysis. AJR. 2007;188:117–25. doi:10.2214/AJR.05.1578.
Gupta M, Srivastava DN, Seith A, Sharma S, Thulkar S, Gupta R. Clinical impact of multidetector row computed tomography before bronchial artery embolization in patients with hemoptysis: a prospective study. Can Assoc Radiol J. 2013;64:61–73. doi:10.1016/j.carj.2011.08.002.
Yoon W, Kim JK, Kim YH, Chung TW, Kang HK. Bronchial and non-bronchial systemic artery embolization for life- threatening hemoptysis: a comprehensive review. Radiographics. 2002;22:1395–409. doi:10.1148/rg.226015180.
Ittrich H, Klose H, Adam G. Radiologic Management of haemoptysis: diagnostic and interventional bronchial arterial embolisation. Fortschr Röntgenstr. 2015;187:248–59. doi:10.1055/s-0034-1385457.
Abdel-Ghany AF, Nassef MA, Osman NM. Multidetector CT chest with bronchial and pulmonary angiography determining causes, site and vascular origin of bleeding in patients with hemoptysis. Egypt J Radiol Nucl Med. 2013;44:769–78. doi:10.1016/j.ejrnm.2013.07.011.
Savvidou D, Malagari K, Kampanarou M, Laspas F, Rousakis A, Kelekis D, et al. The role of multislice computed angiography of the bronchial arteries before arterial embolization in patients with hemoptysis. Open J Med Imaging. 2014;4:133–41. doi:10.4236/ojmi.2014.43019.
Mohamed SAA, Mousa EM, Hamed AM, Amin SE, Abdel Aziz NMA. Utility of multidetector row computed tomography in the management of hemoptysis: an experience from upper Egypt. Egypt J Chest Tuberc. 2016;65:331–40. doi:10.1016/j.ejcdt.2015.08.014.
• Larici AR, Franchi P, Occhipinti M, Contegiacomo A, del Ciello A, Calandriello L, et al. Diagnosis and management of hemoptysis. Diagn Interv Radiol. 2014:20:299–309. Doi:10.5152/dir.2014.13426. An excellent review article elaborating all the diagnostic modalities in evaluation and management of hemoptysis. Authors highlight the usefulness of MDCT in workup of patients with hemoptysis.
Spinu C, González EC, Andreu M, Gallardo X, Mata Duaso JM, Tortajada Bustelo JC, et al. Life-threatening hemoptysis: role of MDCT angiography. ECR 2013 poster no: C-1432. Doi:10.1594/ecr2013/C-1432.
Andersen PE. Imaging and interventional radiological treatment of hemoptysis. Acta Radiol. 2006;47:780–92. doi:10.1080/02841850600827577.
Sirajuddin A, Mohammad TL. A 44- year old man with hemoptysis: a review of pertinent imaging studies and radiographic interventions. Cleve Clin J Med. 2008;75:601–7. doi:10.3949/ccjm.75.8.601.
• Walker CM, Rosado-de-Christenson ML, Martínez-Jiménez S, Kunin JR, Wible BC. Bronchial Arteries: anatomy, function, hypertrophy, and anomalies. Radiographics 2015:35:32–49. Doi:10.1148/rg.351140089. Article discusses in detail the anatomy, functions, variants of the bronchial arteries. All pathologies resulting in bronchial artery dilatation are discussed.
Morita Y, Takase K, Ichikawa H, Yamada T, Sato A, Higano S. Bronchial artery anatomy: preoperative 3D simulation with multidetector CT. Radiology. 2010;255(3):934–43.
Chung MJ, Lee JH, Lee KS, Yoon YC, Kwon OJ, Kim TS. Bronchial and non-bronchial systemic arteries in patients with hemoptysis: depiction on MDCT Angiography. AJR. 2006;186:649–55. doi:10.2214/AJR.04.1961.
Yoon YC, Lee KS, Jeong YJ, Shin SW, Chung MJ, Kwon OJ. Hemoptysis: bronchial and non-bronchial systemic arteries at 16–detector row CT. Radiology. 2005;234:292–8. doi:10.1148/radiol.2341032079.
Zhang LJ, Yang GF, Lu GM. Non invasive diagnosis of bronchial artery aneurysm using dual source computed tomography angiography. Acta Radiol. 2008;49(3):291–4. doi:10.1080/02841850701753714.
Noë GD, Jaffé SM, Molan MP. CT and CT angiography in massive haemoptysis with emphasis on pre-embolization assessment. Clin Radiol. 2011;66:869–75. doi:10.1016/j.crad.2011.03.001.
Ceylan N, Bayraktaroglu S, Mehmet Erturk S, Savas R, Alper H. Pulmonary and vascular manifestations of Behçet disease: imaging findings. AJR. 2010;194:158–64. doi:10.2214/AJR.09.2763.
Chae EJ, Do KH, Seo JB, Park SH, Kang JW, Jang YW, et al. Radiologic and clinical findings of Behçet Disease: comprehensive review of multi systemic involvement. Radiographics. 2008;28:e31. doi:10.1148/r.ge31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sandeep Vohra and Veena Chowdhury each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Additional information
This article is part of the Topical Collection on Thoracic Imaging.
Rights and permissions
About this article
Cite this article
Vohra, S., Chowdhury, V. Multi-detector CT in Evaluation of Hemoptysis. Curr Radiol Rep 5, 14 (2017). https://doi.org/10.1007/s40134-017-0208-x
Published:
DOI: https://doi.org/10.1007/s40134-017-0208-x