Abstract
Every year, 150 million people become affected, worldwide, by severe forms of multi-drug-resistant urinary tract infections (UTI). Several antibiotics are being tested to combat the diseases but newer types of resistance are emerging every year. This throws the challenge of searching of an alternative source of antibacterial compounds. The present study was conducted to evaluate the antimicrobial activities of in vitro and ex vitro grown plants of Coleus forskohlii against twenty MDR strains of UTI bacteria. When methanolic leaf extracts were tested, seventeen among twenty UTI pathogens were found to be sensitive at only 0.75 mg/cup concentration, and three were resistant even at the 6.0 mg/cup concentration. Both the in vitro and ex vitro plants exhibited the highest efficacy against the pathogenic strain of Klebsiella (Isolate no-42285) with the ZI 17.66 ± 0.33 and 18.66 ± 0.57 mm, respectively. Naturally propagated in vivo plants showed significantly low activities compared to those of ex vitro grown plants. In vitro optimal multiplication of 20.4 ± 0.28 shoots per explant was achieved in MS medium supplemented with 1.0 mg/l 6-benzylaminopurine and 0.1 mg/l α-naphthalene acetic acid. A total of 38 and 35 compounds were detected from in vitro and ex vitro plant crude extract, respectively, through GC–MS including thiopene-2-carboxamide, 2-pyrazoline which are known to have potent antimicrobial activity. As both the ex vitro and in vitro plants were found to be highly efficient against most of the UTI pathogens tested, they may serve as a potential source of antimicrobial drug for an alternative therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
“One day no antibiotics may be left to treat common bacterial infections,” warns the World Health Organization. Antibiotics, that were once important weapons in fighting bacterial infections, now have lesser impact against infection. Abusive use of these drugs in human as well as in animal is leading to the accelerated emergence of multi-drug resistance strains [1]. As the efficacy of the antibiotics is now under threat, it has become urgent to develop alternatives for fighting pathogenic bacteria. A survey of World Health Organization (WHO) indicates that about 70 − 80% of the world population in the developing countries depends on herbal sources as their primary healthcare system [2]. Phytomedicinal research is as commendable as to be awarded the Nobel Prize in the year 2015, to the Chinese scientist Youyou Tu for discovering the antimalarial drug ‘artemisinin’ from Artemisia annua L. [3]. It is said that the future of phytomedicine as a discipline lies within high-quality products, able to compete with synthetic drug regarding safety and efficacy [4]. Medicinal plants are known to have curative properties due to the presence of secondary metabolites such as tannins, terpenoids, alkaloids, flavonoids, phenols, steroids, and glycosides [5]. The phytochemicals derived from plant have shown great promise in the treatment of various human diseases. Many plants of Lamiaceae family are used in traditional medicine because of their antimicrobial and antioxidant activities [6]. Unlike the crop plants, the agricultural land is not available for cultivation of medicinal plants; therefore, in vitro biomass production is an alternative choice to produce pharmaceutical compounds throughout the year without cultivation of land [7].
UTI has become the most common hospital-acquired infection. The most common cause of UTI are Gram negative bacteria. Members of this family include different pathogenic strains of Escherichia, Klebsiella, Enterobacter and Proteus vulgaris UTI strains are commonly found to be resistant to ampicillin, tetracycline, & trimethoprim-sulfamethoxazole. Some strains of Pseudomonas and Proteus were resistant to almost all the antibiotics except gentamycin [8]. Due to this wide range of drug resistance, urinary tract infection, formerly describe as ‘mild,’ has been a cause of concern. That is why the present study was taken up to explore the therapeutic potential of bioactive compounds of plant origin against the UTI pathogen.
Coleus forskohlii (Willd.) Briq., a plant of Indian origin, belongs to the family of Lamiaceae (previously Labiatae). This plant is very useful and has a high therapeutic value [9]. Forskolin, the major bioactive compound present in C. forskohlii, is a labdane diterpenoid and used to treat heart disorders, high blood pressure as well as respiratory disorders [10]. It has also been found to have potential antimicrobial activity against different standard strains of gram positive and gram negative bacteria including S. aureus, Streptococcus mutans, Salmonella typhi, and Escherichia coli [11].
Forskolin has been detected in dried roots of field grown plants and stem extracts (0.3 and 0.03%, respectively) by many researchers but not in leaf extracts even through liquid chromatography–mass spectroscopy (LC–MS) [12]. A comprehensive review on the in vitro culture of C. forskohlii revealed that very less or negligible amount of forskolin is present in the stem, leaf or callus culture induced from their explant [13].
We analyzed the leaf extract of in vitro and ex vitro plants of C. forskohlii, not only for the presence of forskolin but also for other major phytochemical constituents, by gas chromatography–mass spectroscopy (GC–MS).
Similarly, the aim of the present study was first, to demonstrate the antimicrobial property of the extracts against clinically isolated UTI pathogens and to compare between the naturally grown, in vitro and ex vitro grown plants. Secondly, profiling of chemical components present in the extracts by GC–MS. This is the first report of GC–MS of tissue culture raised plants of C. forskohlii. However, elucidation of mechanism of action of the extract or its individual components was beyond the scope of this study.
Material and Methods
Plant Source
Naturally Propagated in vivo Plants
Coleus forskohlii (Willd.) Briq. (family Lamiaceae) plants growing in the experimental garden of RKMVC college were used for this study. The soil of the garden was prepared by adding 100 kg cow manure and 50 kg vermin-compost per 100 square meter area. Young and healthy shoot tips (0.8 cm) from four-month-old plants were used as initial explant for in vitro culture establishment. Moderately mature leaves (opposite decussate leaves of third to sixth nodes from the tip) from ten-month-old plants were collected for Soxhlet extraction.
In vitro Plants
Shoot multiplication and in vitro root induction of C. forskohlii plant were established following standard micropropagation technique. Explants were collected from the naturally grown plants, growing in the experimental garden of RKMVC college.
Micropropagation of C. forskohlii.
Shoot tips (1.0–1.2 cm) of field grown healthy plants of C. forskohlii (Willd.) Briq. (family Lamiaceae) were washed with 1.0% liquid detergent (Tween-20) for 2 min, then 2.0% fungicide (Bavistine®) for 10 min, finally disinfected with 0.1% mercuric chloride (HgCl2) for 6 min and rinsed thrice with sterile distilled water to remove trace of HgCl2. The shoot tips were implanted in MS medium [14] fortified with 1.0 mg/l 6-benzylaminopurine (BAP) and 0.1 mg/l α-naphthalene acetic (NAA). Tubes were then kept at 25 ˚C under 16 h/8 h photoperiod in the tissue culture laboratory. Elongated shoots of about 2.0–2.5 cm (after 2–3 weeks) were implanted in MS medium supplemented with 1.0 mg/l indole-3-butyric acid (IBA) for root induction.
Ex vitro Plants
About 3.5–4.0 cm long plantlets with well-developed root system were planted to small earthen pots containing ‘Soilrite’ and covered with transparent polybags to maintain 90–99% relative humidity as described by Haque and Ghosh [15]. After 3 weeks, the hardened plants were transferred to the experimental garden of RKMVC College, Rahara. The soil of the garden was prepared by adding 100 kg cow manure and 50 kg vermin-compost per 100 square meter area.
Microbes Used
In the present study, both the UTI causing pathogenic strains of bacteria (isolated from the UTI patients) and the corresponding standard, laboratory strains of bacteria (used as control) were used.
UTI Pathogens
UTI pathogens designating ISOLATE NO- 42,571, 42,423, 43,181, 43,529, 43,280, 43,509, 43,627, 42,369, 42,332, 42,313 (Escherichia coli), ISOLATE NO- 42,269, 43,164, 43,571, 42,436, 42,398 (Klebsiella pneumoniae), ISOLATE NO- 42,285, 42,006 (Klebsiella sp.) ISOLATE NO- 42,230 (Pseudomonas aeruginosa), ISOLATE NO- 43,546, 43,230 (Staphylococcus saprophyticus) were isolated from the urine samples of the patients. These strains were maintained and cultured in Luria broth (HiMedia®, India) incubating at 37 °C and used for experiments.
Isolation and Identification of UTI Pathogens
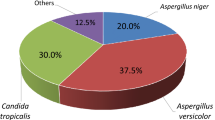
Urine samples from the diseased patients were collected (Ashok laboratory clinical testing center private limited, Kolkata 700,068, India, a BSL-3 laboratory and NABL accredited) and cultured for the isolation of bacteria following standard procedure. MacConkey agar and Nutrient agar plates (HiMedia®, India) were used to isolate UTI pathogens, loop full of urine samples was streaked on MacConkey agar and Nutrient agar plates (HiMedia®, India) and incubated for 24 h at 37 ± 2 °C. After incubation, isolated colonies were selected for further processing. Identification of the pathogenic bacteria was done in VITEK 2 COMPACT SYSTEM BIOMERIUEX machine. Vitek ID tubes containing 3.0 ml half-normal saline were incubated with 3–4 colonies of each sample and McFarland’s reading of ID tubes were taken with the instrument provided adjusting the MCF to s0.5 to s0.63. The suspensions from ID tubes were then transferred to AST tubes with the help of a pipette, and ID and AST cards were inserted into the tubes within 30 min of transfer. Data were collected after completion of the process. A routine presumptive identification was performed by Gram staining, oxidase activity, motility, catalase production, acid production in glucose, oxidation fermentation (OF) test (glucose lactose and sucrose fermentation), Indole test, Voges–Proskauer (VP) test and hydrogen sulfide production. A total of 120 samples of urine, collected from the UTI patients of different age and sex, were screened for the isolation of pathogens (online resource 1). The strains were then subjected to screening for antibiotic resistance.
Detection of Antibiotic Resistance Among the Test Strains
Antibiotic sensitivity assay was performed to demonstrate the resistance against eight antibiotics namely amoxicillin, ciprofloxacin, gentamycin, norfloxacin, nitrofurantoin, clotrimazole, cefotaxime, tetracyclin by the standard disk diffusion method [16]. All the antibiotic disks, used in this study, were purchased from the HiMedia Pvt. Ltd. (Bombay, India), and their efficacies were checked using E. coli B strain (an antibiotic sensitive strain). We screened one hundred and twenty urine samples and identified twenty strains were resistant to all or most of the antibiotics (online resource 2).
Standard Bacterial Strains
Standard strains of MTCC 3160 (S. aureus), MTCC 441 (Bacillus subtilis), MTCC 443 (Escherichia coli), MTCC 3542 (P. aeruginosa). MTCC 109 (K. pneumoniae) MTCC 3382 (S. epidermidis), MTCC 7621 (Pseudomonas syringae), MTCC 1972 (Streptococcus pyogenes) were procured from Microbial Type Culture Collection (MTCC), Chandigarh, India. Bacterial strains of MTCC 3160, 441, 3542, 109, 3382 were maintained in nutrient broth MTCC 443 in tryptic soy broth, MTCC 1972 in rabbit blood broth, MTCC 7621 in yeast manitol medium (according to MTCC manual). All the bacterial strains were cultured overnight in nutrient broth for experimental purpose (HiMedia®, India.).
Extraction of Plant Material
Moderately mature leaves of completely grown in vitro plants (8 weeks old with proper root, shoot and leaves) were collected for extraction. Leaves of (third to sixth nodes from the tip) ten months’ old naturally propagated in vivo plants and tissue culture raised ex vitro plants were collected from experimental garden. Freshly collected 60 g leaves (FW) of in vitro plants, tissue culture raised field grown ex vitro plants, and naturally propagated field grown plants were subjected to dry at 40 °C for 7 days. After completely drying, the plant leaves were powdered, and 5.0 g of each sample was used for extraction. The extraction was carried out using Soxhlet apparatus at 80 °C for 15 h using methanol as a solvent. After extraction, solvent was evaporated and dried samples were kept at 4 °C for further use.
Antibacterial Activity
Agar Well Diffusion Method
Antibacterial activities of the extracts were investigated using agar well diffusion method followed by Deans et al., with slight modification [17]. Wells of 6.0 mm diameter were punched into the Muller Hinton agar plates, and 60 µl of extracts were added to each hole. The dried plant extracts were re-suspended in dimethyl sulfoxide (DMSO) to make five concentrations, i.e., 0.75, 1.5, 3.0, 4.5 and 6.0 mg/cup were tested against all the microbial strains. The Petri dishes were incubated at 37 °C for 24 h. After incubation, the diameters of the zones of inhibition, formed around each hole, were measured and recorded. Testing was carried out for each bacterium and fungus, in triplicate. Negative control plates were prepared using 60 μl of DMSO, and positive control plates were prepared using each of chloramphenicol, ampicillin, amoxicillin, tetracycline at a concentration of 25 mg/ml.
Minimum Inhibitory Concentration
The ‘Twofold broth dilution method’ was used to determine the minimum inhibitory concentration (MIC) of the plant extracts against all the pathogenic and standard microorganisms with minor modification following Ericsson and Sherris [18]. The dried plant extracts were re-suspended in DMSO to make 50 mg/ml concentration and then added to Luria broth by serial dilution method. Exact 100 μl inoculum of such broth was then added to every tube and incubated at 37 °C for 24 h. The MIC values for all the bacteria were noted for the lowest concentration of the plant extracts used.
Minimum Bactericidal Activity
Minimum bactericidal activity (MBC) was determined by plating the respective concentrations of the extracts, used to analyze the MIC values. Exact 100 μl of inoculum was applied to the plate, and data collected after 24 h of incubation.
Gas Chromatography–Mass Spectroscopy
Methanol extracts of the leaves of in vitro, ex vitro and naturally grown C. forskohlii plants were analyzed by gas chromatography–mass spectroscopy (GC–MS) for the identification of different bioactive compounds present in the extracts. GC–MS was performed using column: TRWAXMS 30 × 0.25 mm × 0.25 µm df, equipment: Trace GC ultra, Thermo fisher scientific India pvt. Ltd. Gas flow: 1.0 ml/min split 20:1 detector: mass detector Polaris Q mass software data collection XCALIBUR. 1.0 µl of extract was injected in the injection port of GC column. Oven temperature program was: no hold up to 50 ºC, for 2 min at the flow rate of 10 ºC/min, 5 min hold up to 270 ºC. Injector temperature 250 ºC and total GC–MS running time 29 min. Helium Gas was used as carrier gas at a constant flow rate of 1 ml/min. MS program: library NIST (USA). Inlet line temperature was 250 ºC, and source temperature was 230 ºC. Mass scan was done at 50–650 m/z with solvent delay of 0–4 min and total mass spectrum running time was 51 min.
Statistical Data Analyses
Each experiment, for determination of antimicrobial activity by agar well diffusion method, was repeated thrice with 5 concentrations per replicate. All data were subjected to one-way analysis of variance (ANOVA) using SPSS software for Windows (IBM® SPSS, version 19.0, Chicago, IL). After conducting an ANOVA, the means were further separated using Tukey’s test at P ≤ 0.05.
Results and Discussion
Micropropagation
Profuse shoot growth occurred within 4 weeks of implantation with the production of 20.4 ± 0.28 shoots per explants. These multiplied shoots were elongated after one subculture in same medium composition (Fig. 1a). These shoots were well rooted in IBA (1.0 mg/l) containing root-inducing medium with 14.2 ± 0.18 roots per shoot after 4 weeks (Fig. 1b). After 3 weeks, the hardened plants were transferred to the experimental garden of R.K.M.V.C. College, Rahara. Total 83.2 ± 3.4% ex vitro plants were survived in the field conditions and grew healthily (Fig. 1c). Finally all ex vitro field grown plants were flowered after 10–11 months of field transfer (Fig. d, e). It is well known that the biomass production, using natural habitats of any plant, is time consuming and harvesting of wild population leads to the depletion of the resource, whereas biotechnological cultivation of plant through tissue culture is a cost effective, less time-consuming process which can easily be upgraded to industrial level [7]. Moreover, clonal propagation of any explant of a plant is essentially very useful for the production of the fruitful results. Morphological and health improvement of the plants were observed when plants were grown ex vitro compared to naturally grown plants. This fact led us to investigate the potency of tissue culture raised plants as a source of antimicrobial agents. Ex vitro grown plants seems fleshier and contains more hair with higher leaf content while naturally grown plants having lower leaf content and leaf hair also lesser than ex vitro grown plants. Morphologically ex vitro plants were more stable and healthy over naturally grown plants.
Micropropagation of Coleus forskohlii. a in vitro multiplication, b in vitro grown complete plant with well-developed root system, c tissue culture raised ex vitro field grown plants of 3 months of age, d tissue culture raised ex vitro field grown plants (10 months age) in flowering stage, e Flowers of ex vitro plant, f naturally propagated in vivo field grown plants (10 months age) in flowering stage
Antimicrobial Activity of Extract
Agar Well Diffusion
All the pathogenic (excepting three) and standard bacteria (excepting one) were found to be sensitive to the methanol extracts of both in vitro and ex vitro plants (Table 1) while nine bacteria including pathogen and non-pathogen found resistant against naturally grown plant extract. Because of much lower activity in case of naturally grown plants, only maximum concentration (6.0 mg/cup) is used to represent the antimicrobial potency. The ex vitro plant extracts were more effective as antimicrobial agent compared to those of in vitro plants and naturally grown plants. Maximum diameter of zone of inhibition (DZI) of 18.66 ± 0.57 mm was found with highest concentration of ex vitro plant extract (6.0 mg/cup) against pathogenic ISOLATE NO- 42,285 compared to its in vitro counterpart with a DZI of 17.66 ± 0.0.33 mm and naturally grown part with a DZI of 14 ± 0.57 mm. However, for ISOLATE NO- 42,423 and 42,313, all the concentrations of in vitro plant extracts were more effective than ex vitro extracts (DZI of 16.00 ± 0.81 mm and 12.33 ± 0.47 mm were obtained at a concentration of 6.0 mg/ml compared to 12.66 ± 0.47 mm and 9.66 ± 0.94 mm, respectively). Interestingly, in vitro extracts were found to be saturated at a concentration of 4.5 mg/cup as not much increase was found in DZI at higher concentrations. ISOLATE NO- 42,269 and 43,546 were found to be completely resistant to the plant extracts used and ISOLATE NO- 43,546 and 43,164 showed no or least inhibition. ISOLATE NO- 42313 showed an inhibition which is lesser than the average. Standard bacteria (excepting MTCC 109) showed inhibition with both types of plant extracts. Naturally grown plant extract were less effective against all the microbes tested than both in vitro and ex vitro plant extract. Here also, ex vitro extracts showed much higher inhibitory effects over in vitro extracts, as it was with clinical isolates. Undoubtedly, the outcome was very encouraging as, all the extracts of the plant leaves of naturally grown, in vitro and ex vitro, showed antibacterial activity against all the microbial strain tested in present study. According to effectivity, ex vitro plants were stronger, in vitro plants were moderately active and naturally grown were less effective against both pathogens and non-pathogens. Methanolic extracts of leaves have been used in our study, as the polarity index of methanol is 5.1, therefore all polar (and to some extent nonpolar) bioactive compounds are highly or at least fairly soluble. Previously, methanolic extracts of many plants of Lamiaceae family, including root and leaf extracts of C. aromaticus and C. forskohlii, has been shown to be antimicrobic in nature [19, 20]. Aqueous, ethanolic and methanolic extracts of nine species other than Coleus have also been reported to exhibit antimicrobial activity against UTI pathogens [21]. However, in this study, methanolic extracts showed better performance against UTI pathogens. It was also reported that if antimicrobial compound like commercial antibiotics were used with the plant extract it became more effective rather than using extract or antibiotics itself [22]. These initiatory studies motivated us to take up the plan of investigating UTI pathogens, which are resistant to multi-drugs. Among 20 such isolates, 18 were gram negative (ten Escherichia coli, seven K. pneumoniae and one Pseudomonas aeruginosa), and E. coli strains were found to be more effective than K. pneumoniae. According to the finding of Singh et al. 2017 [23], most of the strains including extended spectrum beta lactamase (ESBL) positive were found to be susceptible to the extract of the respective plant used in this study. Nevertheless, this study is unique and a class by itself with adequate detail and no such work has been done before with C. forskohlii.
MIC and MBC
The results of MIC and MBC of the plant extracts (in vitro and ex vitro) are summarized in Table 2. In case of pathogenic bacteria ISOLATE NO- 4257, the MIC and MBC were found to be lowest with ex vitro, in vitro extract (1.25 mg/ml and 1.75 mg/ml for in vitro and 0.75 mg/ml and 1.25 mg/ml for ex vitro plant extracts). Naturally grown plant extract shows less promising MIC and MBC than both in vitro and ex vitro plant extract. However, the plant extracts (in vitro and ex vitro) were not effective against MTCC 109 and pathogens designated as ISOLATE NO- 42,269, 42,436, and 43,280 wherein naturally grown plant extract ineffective against nine bacteria.
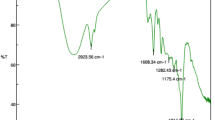
Gas Chromatography–Mass Spectroscopy
A total of 38 compounds were identified from in vitro plant extract and 35 compounds from ex vitro extract (Table 3) (Fig. 2a, b). Although a total of 27 compounds were detected in naturally grown plant extract, the major antimicrobial compound, found in the in vitro and ex vitro extracts, were either missing or barely found in this. So, the data were not compared with those of vitro and ex vitro extracts. Common compounds identified in both in vitro and ex vitro extracts were 2–3 butanediol, Pentanoic acid, 6,7-Dimethyl triazolo (4,3 b) (1,2,4) triazine, Triazine, Furfuryl glycidyl ester, 2ethyl 2 hexen-1-ol, 5 methyl-3- heptyne, Ethylene glycol, Hexagol and many other derivatives. Some compounds like Isocyanic acid 4-ethyl-2-Hexanyl 1–3 dioxolane, Oxalic acid, Oxirane, Propanoic acid, Ethylene oxide cyclic Hexamer are present only in ex vitro extracts but not in the other. Likewise, some like Acetamide derivative, 1- tetradecyne, Neo Hexane, Acetonitrile derivative, 1 aminocyclopropanecarbonitrile, Phthalic acid ester, 2-Octyne, Isopropyl derivative, Thiophene are present exclusively in in vitro extracts. Almost all the compounds found recurrently in both the extracts have antimicrobial activity. High antimicrobial activity containing compounds like 6,7- Dimethyl triazolo, 2- Pyrazoline, S- triazine, furfuryl glycidyl ester were not detected in naturally grown plant extract. Compounds like 2–3 butanediol, 2ethyl 2 hexen-1-ol, Oxalic acid, Oxirane, and Propanoic acid were present in naturally grown extract as like ex vitro and in vitro extract. Absence of major antimicrobial compounds and presence of some compound in low amount proves naturally grown extract significantly low in activity against pathogen and non-pathogens. Gas chromatography–mass spectroscopy (GC–MS) of the root extracts of C. forskohlii was previously done by few researchers [24]. Availability of the leaf biomass is easier as compare to root, because collection of root is only possible by scarifying the plants whereas leaf could be collected throughout the years without scarifying the plants. GC–MS profiling of the leaf extract of C. forskohlii shows presence of different type of phyto-constituents, many of them having the ability to kill microbes and also have anti-inflammatory and anti-cancerous activity. Flavonoids are mostly active against bacteria by disrupting their enzyme system. Bacterial membrane disruption is also done by tannin groups through interfering with protein synthesis process [25]. Many compounds are present in the ex vitro extract but absent in the in vitro extract and vice versa regarding to comparative data. Most of the compounds, present both in in vitro and ex vitro extracts, are known to have antimicrobial properties. They may contribute cumulatively toward the antimicrobial potential of the extracts. Presence of some additional antimicrobial compounds in ex vitro extracts may be the cause of showing enhanced activity over that of in vitro. Similar findings has been described by few other researchers where ex vitro field grown plants exhibited more antimicrobial activity as compare to in vitro plants [7]. Protein that was present in the plant extract mostly was antimicrobial. Plants generate those peptide or protein for initial defense mechanism [26]. Furfuryl glycidyl ester commonly named furan, found in in vitro extracts, is also reported as an active compound against bacteria and fungi [27]. Propionic acid, a common compound present both in in vitro and ex vitro extracts, is active against the growth of bacteria and molds and commonly used in the food industries [28]. Phthalic acid ester, although present in small amount, is a potent carcinogenic agent [29]. Pyrazoline is an active phyto-constituents present in the plant extract also having the antifungal antibacterial [30] activity.
Conclusions
The leaf extracts of C. forskohlii (naturally grown source plants, tissue culture raised in vitro and ex vitro plants) found to be effective on some multi-drug resistant pathogenic ESBL positive bacterial strains collected from the urine samples of UTI patients. Specially, the ex vitro plant extract is significantly effective against multi-drug resistant UTI pathogens and can be produced through tissue culture throughout the year. Although root was previously subjected to similar experiments, the present study is the first attempt using leaves of C. forskohlii and seems extensive good pathogen-killing ability. Leaf biomass of a single plant is much higher than the root, additionally leaf could be collected round the years but roots once after completing the lifespan. Therefore, leaf is better choice than root for continuous supply of antimicrobial phytocompounds. Further investigation using various other pathogens would be very promising and according to the resulted data the compounds and extract can be used as alternative therapy in future medicine.
References
Shalayel MHF, Asaad AM, Qureshi MA, Elhussein AB (2017) Anti-bacterial activity of peppermint (Mentha piperita) extracts against some emerging multi-drug resistant human bacterial pathogens. J Herb Med 7:27–30
WHO (1998) Regulatory situation of herbal medicine: a World Wide Review. World Health Organization, Geneva
Efferth T, Zacchino S, Georgiev MI, Liu L, Wagner H, Panossian A (2015) Nobel Prize for artemisinin brings phytotherapy into the spotlight. Phytomedicine 22:A1–A3
Efferth T (2017) The road in front of us: phytomedical research for the years to come. Phytomedicine 25:A1
Soni A, Sosa S (2013) Phytochemical analysis and free radical scavenging potential of herbal and medicinal plant extracts. J Pharmacogn Phytochem 2:22–29
Ulukanli Z, Cigremis Y, Ilcim A (2011) In vitro antimicrobial and antioxidant activity of acetone and methanol extracts from Thymus leucotrichius (Lamiaceae). Eur Rev Med Pharmaco 15:649–657
Haque SM, Chakraborty A, Dey D, Mukherjee S, Nayak S, Ghosh B (2017) Improved micropropagation of Bacopa monnieri (L.) Wettest. (Plantaginaceae) and antimicrobial activity of in vitro and ex vitro raised plants against multidrug-resistant clinical isolate of urinary tract infecting (UTI) and respiratory tract infecting (RTI) bacteria. Clin Phytoscience 3:17
Abejew AA, Denboba AA, Mekonnen AG (2014) Prevalence and antibiotic resistance pattern of urinary tract bacterial infections in Dessie area. North-East Ethiopia BMC Res Notes 7:687
Nikalje AP, Baheti S, Kamble S, Khan S, Sangshetti J (2017) Isolation of phyto constituents from the roots of Coleus forskohlii by column and flash chromatographic method. Indo Am j pharm 4:74–84
Kanne H, Burte NP, Prasanna V, Gujjula R (2015) Extraction and elemental analysis of Coleus forskohlii extract. Pharmacogn Res 7:237
Mothana RA, Khaled JM, El-Gamal AA, Noman OM, Kumar A, Alajmi MF, Al-Rehaily AJ, Al-Said MS (2019) Comparative evaluation of cytotoxic, antimicrobial and antioxidant activities of the crude extracts of three Plectranthus species grown in Saudi Arabia. Saudi Pharm J 27(2):162–170
Ganzera M, Choudhary MI, Khan IA (2003) Quantitative HPLC analysis of withanolides in Withania somnifera. Fitoterapia 74:68–76
Petersen M (1994) Coleus spp.: In vitro culture and the production of forskolin and rosmarinic acid. Med Aoma Plants 4:69–92
Murashige T, Skoog F (1962) A revised medium for rapid growth and bio assays with tobacco tissue cultures. Physiol Plantarum 15:473–497
Haque SM, Ghosh B (2013) High frequency micro cloning of Aloe vera and their true-to-type conformity by molecular cytogenetic assessment of two years old field growing regenerated plants. Bot Stud 54:46
Bayer AW, Kirby WM, Sherris JC, Turck M (1966) Antibiotic susceptibility testing by a standardized single disc method. Am J Clin Pathol 45(4):493–496
Deans SG, Ritchie G (1987) Antibacterial properties of plant essential oils. Int J Food Microbiol 5:165–180
Ericsson HM, Sherris JC (1971) Antibiotic sensitivity testing. Report of an international collaborative study. Acta Pathologica et Microbiologica Scandinavica (Suppl. 217)
Wadikar DD, Patki PE (2016) Coleus aromatics: a therapeutic herb with multiple potentials. J Food Sci Technol 53:2895–2901
Malleswari D, Bagyanarayana G, Hindumathi A (2013) Anti-bacterial activity of Coleus forskohlii extracts against some pathogenic bacteria. J Nat Prod Plant Resour 3:75–78
Mishra MP, Rath S, Swain SS, Ghosh G, Das D, Padhy RN (2015) In vitro antibacterial activity of crude extracts of 9 selected medicinal plants against UTI causing MDR bacteria. J King Saud Univ Sci 29:84–95
Rakholiya K, Chanda S (2012) In vitro interaction of certain antimicrobial agents in combination with plant extracts against some pathogenic bacterial strains. Asian Pac J Trop Biomed 2:S876–S880
Singh V, Jaryal M, Gupta J, Kumar P (2017) Antibacterial activity of medicinal plants against extended spectrum beta lactamase producing bacteria causing urinary tract infection. Int J Drug Res Tech 2:263–267
Rajkumar K, Malathi R (2015) Phytochemical investigation GC-MS analysis and in vitro antimicrobial activity of Coleus forskohlii. Bangladesh J Pharmacol 10:924–930
Cowan MM (1999) Plant products as antimicrobial agents. Clin Microbiol Rev 12:564–582
Vargas WA, Martín JMS, Rech GE, Rivera LP, Benito EP, Díaz-Mínguez JM, Thon MR, Sukno SA (2012) Plant defense mechanisms are activated during biotrophic and necrotrophic development of Colletotricum graminicola in maize. Plant Physiol 158:1342–1358
Alabi KA, Hassan GF (2014) Determination of minimum inhibitory concentrations of 2-(2-nitrovinyl) furan. Academia J Microbiol Res 2:028–032
Chen L, Guo G, Yuan X, Shimojo M, Yu C, Shao T (2014) Effect of applying molasses and propionic acid on fermentation quality and aerobic stability of total mixed ration silage prepared with whole-plant corn in Tibet. Asian-Australas J Anim Sci 27:349–356
Kluwe WM (1986) Carcinogenic potential of phthalic acid esters and related compounds: structure-activity relationships. Environ Health Perspect 65:271–278
Nauduri D, Reddy GBS (1998) Antibacetrials and antimycotics: Part 1: synthesis and activity of 2-pyrazoline derivatives. Chem Pharm Bull 46:1254–1260
Acknowledgements
AC, SMH and BG thankful to Swami Kamalasthananda, Principal, Ramakrishna Mission Vivekananda Centenary College, Rahara, Kolkata (India), for the facilities provided for the present study. SMH thankful to Dr. Sukla Hazra, Principal, East Calcutta Girls’ College, Lake Town, Kolkata (India), for giving the permission to do research in collaboration with R.K.M.V.C. College. DD acknowledges technical and management support provided by Ashok Laboratory Clinical Testing Centre Private Limited, Kolkata.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Significance Statement
Present day, one of the major concerns is, the emergence bacterial diseases caused by the deadly strains, resistant to multiple drugs commonly used in health treatment. The finding of the present study describes that the plant extracts of C. forskohlii are promising in this respect with the potentiality of killing multi-drug resistant UTI pathogens of human, significantly. Another important part of this study is the establishment of fast growing plant tissue cultures from various tissues of the plant through micropropagation technique, in order to get a steady supply of the in vitro plants in high amount, throughout the year. Compounds present in the plant extracts were also identified through GC–MS analysis and found to contain compounds known as bioactive and antimicrobial in nature. So it can be said that these extracts can be used as an alternative source for the production of next generation drugs, without side effects.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chakraborty, A., Haque, S.M., Dey, D. et al. Detection of UTI Pathogen-Killing Properties of Coleus forskohlii from Tissue Cultured In vitro and Ex vitro Plants. Proc. Natl. Acad. Sci., India, Sect. B Biol. Sci. 92, 157–169 (2022). https://doi.org/10.1007/s40011-021-01285-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40011-021-01285-4