Abstract
Antibacterial efficacy of the water-fern, Azolla caroliniana Willd., symbiotic with the nitrogen fixing cyanobacterium, Anabaena azollae against seven multidrug resistant pathogenic bacteria were evaluated. Antioxidant and organoleptic properties of the fern were also assessed. Most Gram-negative and Gram-positive bacteria used in this study were highly resistant to 17 antibiotics of aminoglycoside, beta-lactam, cephalosporin and fluoroquinolone groups, as recorded from Kirby-Bauer method. The methanolic extract of A. caroliniana generated 20 mm as the maximum size of zone of inhibition against Staphylococcus aureus, as recorded from the agar-well diffusion method. The minimum inhibitory concentration value, 1.89 mg/ml was due to the methanolic extract against S. aureus and Proteus mirabilis, while the value, 4.27 mg/ml was against Enterococcus sp., Enterobacter aerogenes, Escherichia coli and Pseudomonas aeruginosa. The minimum bactericidal concentration value, 4.27 mg/ml was of the methanolic extract against S. aureus and P. mirabilis, while the value, 21.67 mg/ml was recorded against Citrobacter sp., E. aerogenes, E. coli and P. aeruginosa. Fifty percent inhibition concentration values of free radical scavenging activities of the fern with free radical generating chemicals, 1,1-diphenyl-2-picryl hydrazyl, as well as, 2, 2-azino-bis (ethylbenzthiazoline-6-sulfonic acid), hydrogen peroxide and nitric oxide of the methanolic extract were 8, 10, 10, and 78.8 µg/ml, respectively. In four solvent-extracts with methanol, ethanol, chloroform and n-hexane, several common phytochemicals and phenols were present, while alkaloids and saponins were absent. Processed Azolla was tasteless but not unpalatable. Azolla caroliniana could be used as an antibacterial as well as an antioxidant agent in complementary and alternate medicine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
After the introduction of antibiotics, just after 1940, to control infections, bacterial resistance to the used antibiotics have arisen soon after and slowly over the time, pathogenic bacteria have been achieving multi-resistance to the applied antibiotics and other antimicrobial drugs. Eventually, multidrug resistant (MDR) pathogenic bacteria have been emerging, which of course, are controlled mostly by newer antibiotics/drugs, progressively. However, the emergence of MDR bacteria has been a constant cause of consternation in clinical management now, worldwide, since many a time failures in the control of infections are reported [1]. For example, wounds infected with the silently violent, appalling MDR strains of Pseudomonas aeruginosa, the methicillin resistant Staphylococcus aureus (MRSA) as well as, Escherichia coli were found ghoulish and intractable, due to the emergence of quirk clonal nexuses [2–4], achieved by the surprising efficiency of the blizzard of outlandish bacterial genetic exchange mechanisms, operative in vivo and in vitro. Those strains have been raising spread of MDR strains to saturnine standards in gastro-intestinal and urinary tracts [5]. Moreover, two to three antibiotics are added each year from microbial sources [5]; and the pace at which, MDR pathogenic bacteria emerge, the development of newer antibiotics is not able to cope up. Consequently, morbidity and mortality increase due to the suffuse of MDR bacteria in community and hospitals, often precipitating alarming episodes in public health [6]. Moreover, artifices of pandrug resistant (PDR) bacterial strains of P. aeruginosa, Acinetobacter baumannii and Klebsiella pneumoniae resistant to almost all drugs/antibiotics of the time are so much widespread that public health episodes are frequent [7]. Further, the dreadful metallo-β-lactamase producing K. pneumoniae strain even in a neonate [8] and the totally drug resistant (TDR) tubercle bacilli (TB) strain [9] are so much complex and demanding that leaning to certain novel control sources for the search of avant-garde drugs would be a prudent approach for a solution. Secondly, as it is hard to think of an aspect of the contemporary life without the control of marauding pathogens, the search for newer antimicrobials from conventional/non-conventional sources has become the call of the day, as treatment options against MDR bacterial infections become progressively limited in mainstream medicine. For example, the treatment of MDR-TB has become utterly difficult now-a-days, for several obvious reasons detailed elsewhere [3]. In the odyssey of drug development, several generations of penicillin and cephalosporin, and the cavalcade of newer antibiotics, macrolides, fluoroquinolones, aminoglycosides, glycopeptides, lincosamides, sulfonamides and a few more groups have been introduced, sometimes even by altering natural structures of individual antibiotics. Anyway, for the control of MDR strains of bacteria, the use of alternate drugs has been thought up, and plants remain as the obvious palpable source of non-microbial antimicrobials. In the limit of course, dove-tailed antibiotics are costlier than plant based drugs.
Dating back to prehistory, people in all countries have been utilizing the healing power of plants, which even served as holistic bastions of health and well-being. However, up to as early as 1960s, the use of plant derivatives as antimicrobials in the modern drug module was non-existent, and today several phytochemicals have found their positions in the arsenal of antimicrobial drugs prescribed by physicians; several phytochemicals are tested for humans by now [7]. Further, a multitude of phytocompounds present in crude extracts are readily available over-the-counter as herbal drugs often with unreliable purity, but with popularity as healing agents. These medicines have generated the ‘medicinal plant trade’ in many nations in the tide of love for natural chemicals over synthetic ones for health, as well as failures in the elusive goal of mainstream medicine in many a treatment. Eventually, self-medication with crude phyto-drugs has become worldwide. Consequently, the concept of complementary and alternate medicine (CAM) has become embolden, derived from local schools of traditional/folklore medicines, independently, followed in each country from times immemorial; notwithstanding, too many of those are not proved for efficacy and/or host toxicity and non-target effects with scientific exactitude by apothecary. Much time is needed for the isolation of pure chemicals from plant extracts.
As a part of academic endeavour, the conventional use of ethnic knowledge on plants as therapeutics has been verified, with crude phyto-extracts mostly (with pure phyto-compounds, less often), against drug-sensitive pathogenic bacteria of type collection centres. The available literature is so enormous that those could fill a book or two [7, 9]. However, most recently MDR bacteria isolated from clinical samples were used in similar work of monitoring of antimicrobial activities of crude plant extracts [10, 11]. Indeed, crude phyto-extracts with an array of diverse phyto-compounds could never be breached upon by any pathogenic bacterium, no matter how much genetically well developed it may be. Indeed, there are areas of infection biology, for example infection of individual human viruses, MDR bacteria, fungi attacking different organs including heart and lungs and a few more, need be fixed by medicines with an iron hand with/without scientific exactitude. The unfortunate truth is that external infections become systemic, due to which extrication from pugnacious pathogens becomes a staggering victory. Further, crude extracts with exquisite coalesced phytochemicals of several plants individually, for example, Lantana camara [11], have been described with blithesome control over almost all MDR bacterial strains isolated from clinical samples. It has been seen that the mainstream medicine is increasingly resistive to antimicrobials and other drugs from plants; nevertheless, World Health Organisation (WHO) directives promote the use of phytochemicals [12]. As the goal to the control of MDR bacteria is formidably tough, phytochemicals are to be used with adept as antimicrobials.
The genus Azolla with 7 species, called often as ‘mosquito fern’ or ‘water fern’ is a small aquatic fern, naturally growing in rivers, ponds, ditches, canals and paddy fields containing idle water, distributed in both temperate and tropical regions [13]. Because of its symbiosis with the nitrogen-fixing cyanobacterium, Anabaena azollae, it adds nitrogenous compounds to the environment and grows fast; also, it is grown to fertilize rice fields prior to soil-puddling, as green manure or along with rice as the dual crop [13]. Further, the antimicrobial activity of Azolla was undertaken as an extension of the earlier similar work on the terrestrial wild fern, Lygodium flexuosum with a successful control of several pathogenic bacteria in vitro [14].
A preliminary work with ethanolic extract of Azolla filiculoides on two bacteria of undefined drug-sensitivity, E. coli and S. aureus recorded the negative effect [15]. However, a systematic search of database resulted in the absence of any other available report on the use of Azolla, as a source of antimicrobials [15]. This paper describes antimicrobial activity of A. caroliniana, against two MDR Gram-positive (GP) and five MDR Gram-negative (GN) bacteria, isolated from clinical samples of a tertiary care hospital. All these seven bacteria are often marked as uropathogens too, causing morbidity and mortality in females mainly, due to cystitis, pyelonephritis, urethritis and a few more associated with acute cases of urinary tract infection, by the retrograde ascent of bacteria from faecal flora via urethra to bladder and kidney [16]. All these ailments could lead to bacteremia at vital organs and similar infections at prostrate glands in males [16].
Because of its easy mass cultivation, Azolla has been used as feed/fodder for pigs, ducks, chicks and fish [17]. In fact, Azolla is much explored as feed and fodder than as food for humans. But in China, it has been suggested that after sterilization by steam, Azolla could be used as salad or stuffing in spring rolls [18]. Azolla also has been used in soup, meat balls, omelettes, burgers, fried sautéed, and baked form [17]. The rough protein content of Azolla was estimated at 20–30 % [17], whereas that of soybean was around 40 %, some of the newly bred Azolla strain contains as high as 35 % rough protein [17]. As Azolla is popular as feed and fodder, it was intuitive to verify its antioxidant ability that being absent in literature, this work was initiated with four chemicals, 1, 1-diphenyl-2-picryl hydrazyl (DPPH), 2, 2-azino-bis (ethylbenzthiazoline-6-sulfonic acid) (ABTS+), hydrogen peroxide (H2O2) and nitric oxide (NO), for a scientific explanation of the benefit of Azolla as feed and fodder.
Material and Methods
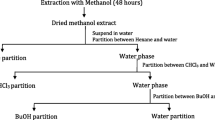
Preparations of Extracts
Azolla caroliniana Willdenow (Azollaceae) (Fig. 1), a species belonging to the group, Euazolla, was first introduced by Central Rice Research Institute, Cuttack in India [19, 20], and now it is commonly found in natural habitats at this part of the state besides the common and extensively used Azolla pinnata. It was grown in well-illuminated cemented tanks in open air with the local farm practice, with supplementation of super phosphate (P2O5, 16 % P) and potash (K2O, 60 % K). Total fern-fronds were harvested and were shade dried. For the cold extraction, 10 g of Azolla-frond powder was dissolved in an aliquot of 100 ml of n-hexane in a Tarson screw-cap bottle and the mixture was stored at 4 °C for 5 days; the same procedure was followed for the rest three organic solvents, chloroform, methanol and ethanol. Each solvent-extract after centrifugation was dried using a vacuum rotary evaporator until a semisolid mass was obtained; extracts with methanol, ethanol, chloroform and n-hexane had weight of 120, 100, 80, and 80 mg semisolid mass/10 g dry weight of Azolla frond powders. Each extract was further stored in small vials in 10 % dimethyl sulfoxide (DMSO) solution at 4 °C until further use.
Isolation and Identification of Pathogenic Bacteria
Two GP Enterococcus sp. and Staphylococcus aureus as well as, five GN bacteria (Citrobacter sp., Enterobacter aerogenes, Escherichia coli, Proteus mirabilis and Pseudomonas aeruginosa were isolated from in-house (intensive care unit or ICU, neonatal ICU, wards and cabins) patients of the hospital. Biochemical identifying methods of clinically isolated bacteria and their maintenance in axenic cultures on selective media were done, as described by Dubey and Padhy [11].
Antibiotic Susceptibility Test of Bacteria
All bacterial strains including Microbial Type Culture Collection (MTCC) standard strains (Table 1) were subjected to antibiotic sensitivity tests by the Kirby-Bauer’s/disc-diffusion method, using a 4 mm thick Mueller–Hinton (MH) agar (HiMedia, Mumbai) medium, in duplicates. An aliquot of 0.1 ml of 0.5 McFarland equivalents, approximately from an exponentially growing culture was spread on agar for the development of lawn of a bacterium at 37 °C in a BOD incubator (Remi CIM-12S). Further, on the lawn-agar of each plate, 8 high potency antibiotic discs (HiMedia) of 17 prescribed antibiotics were placed, separately at equal distances from one another. For GP bacteria 15 antibiotics, whereas for GN bacteria 16 antibiotics were used in the study. Plates were incubated for 18 h at 37 °C and were examined for size of zones of inhibition around each disc, following the standard antibiotic susceptibility test chart of Clinical Laboratory Standard Institute (CLSI) guidelines. Experiments were done three times and data of the third set of experiments were presented [2, 3].
Antibacterial Efficacy Test of Azolla-Extracts
Antibacterial activities of the four different solvent-extracts of the fern were done by the agar-well diffusion method. One strain from each bacterial species having resistance to maximum number of antibiotics was used, for monitoring antibacterial activities of plant extracts. Bacterial lawns were prepared with agar being 6 mm thick that was fully punched and 6-8 wells were prepared, when the lawn was 30 min old, and each well was based by 50 µl molten MH agar, in duplicates. Further, wells were filled with 100 µl aliquots of 30 mg/ml solvent-extracts of A. caroliniana, diluted from the original stock of plant extracts of individual organic solvents with the aqueous extract, by 10 % DMSO solution. Plates were incubated at 37 °C for 18–24 h. Antibacterial activities were evaluated by measuring the diameter values of zones of inhibition. Experiment of each solvent-extract was conducted thrice and data of the third repeated experiment are presented. An aliquot of 100 µl of gentamicin 30 µg/ml with an average diameter of zone of inhibition of 24.5 mm and 10 % DMSO solution were reference controls; 10 % DMSO solution had no antibacterial activity [11].
Determination of MIC and MBC Values
Minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) of three active extracts, prepared with methanol, ethanol and chloroform were determined, by suitable dilutions from original stock solutions of each extract, for concentrations of 0, 1.562, 3.125, 6.25, 12.5, 25, 50 and 100 mg plant-extract/ml in aliquots of 10 % DMSO solution. Separate experiments were conducted for each solvent-extract. An aliquot of 80 µl of each dilution of a solvent-extract was released to a well on a 96-welled (12 × 8) microtiter plate, along with an aliquot of 100 µl MH broth (HiMedia), an aliquot of 20 µl bacterial inoculum (109 CFU/ml) and a 5 µl-aliquot of 0.5 % 2,3,5-triphenyl tetrazolium chloride (TTC). After pouring all the above materials to a well, the micro-titre plate was incubated at 37 °C for 18 h. The development of pink colouration due to TTC in a well indicated bacterial growth and the absence of the colouration was taken as the growth inhibition. The first well of the micro-titre plate was the control, without any plant extract. The MIC value was noted at the well, where pink colour was not manifested. Further, bacteria from each well of the micro-titre plate were sub-cultured on nutrient agar; the level of dilution, where no bacterial growth on the nutrient agar was observed, was noted as the MBC value [11]. Results of the second repeated experiment were presented.
Phytochemical Analyses
With all four organic solvent extracts of the fern, the following phytochemical analyses were done, as described previously [10, 11].
Test for Anthraquinones
0.5 g of the extract was shaken with an aliquot of 10 ml of benzene, filtered and an aliquot 5 ml of 10 % ammonia solution was added to the filtrate and the mixture was shaken; the presence of a pink, red or violet colour in the ammoniac (lower) phase indicated the presence of anthraquinones.
Test for Saponins
0.5 g of An extract was dissolved in an aliquot of 10 ml of distilled water in a test-tube, which was shaken vigorously for 30 s and subsequently was allowed to stand for 45 min. The appearance of frothing on warming the solution indicated the presence of saponins.
Test For Flavonoids
To a portion of the dissolved extract, a few drops of 10 % ferric chloride solution were added. A green or blue colouration indicated the presence of flavonoids.
Test for Steroids/Terpenes
500 mg of The concentrated mass of the Azolla-extract from the rotary evaporator was dissolved in an aliquot of 2 ml of acetic anhydride and the mixture was cooled at 0 to 4 °C, to which a few drops of 12 N sulphuric acid were carefully added. A colour change from violet to blue-green indicated the presence of a steroidal nucleus.
Test for Tannins
0.5 g of The extract was dissolved in 5 ml aliquot of water followed by addition of a few drops of 10 % ferric chloride solution. A blue-black, green, or blue-green precipitate indicated the presence of tannins.
Test for Alkaloids
0.5 g of Plant-extract was stirred with an aliquot of 5 ml 1 % HCl on a steam bath, and the mixture was filtrated; to an aliquot of 1 ml of the filtrate, a few drops of Mayer’s reagent (1.36 g HgCl2, 5 g KI in 100 ml distilled water) was added, and to another aliquot of 1 ml of the filtrate, a few drops of Dragendorff’s reagent (two solutions in 1:1 ratio—‘solution A’ with 0.85 g bismuth nitrate, 10 ml glacial acetic acid and 40 ml distilled water, and ‘solution B’ with 8 g KI in 30 ml distilled water) were added. Turbidity or precipitation in tubes due to either of these reagents indicated the presence of alkaloids in the extract.
Test for Glycosides
An aliquot of 5 ml of each extract was mixed with an aliquot of 2 ml of glacial acetic acid (1.048 g/ml), one drop of 1 % FeCl3 solution, and mixed thoroughly to which, an aliquot of 1 ml of 12 N H2SO4 was added. A brown ring at the interface indicated the presence of glycosides.
Test for Terpenoids (Salkowski Test)
To 0.5 g of the extract, an aliquot of 2 ml of chloroform was added, followed by an addition of conc. H2SO4 (3 ml) to form a layer. A reddish brown colour formation at the interface was noted for the presence of terpenoids.
Test for Carbohydrates (Molisch’s Test)
A small quantity of the extract was dissolved in an aliquot of 5 ml of distilled water, filtered and to the filtrate 2–3 drops of α-naphthol were added. Further to the mixture, an aliquot of 1 ml of conc. H2SO4 was added; two layers were formed with the formation of a violet coloured ring at the interface indicating the presence of carbohydrates.
Test for Phenols
A little of the extract was diluted with water to which, an aliquot of 2 ml of 1 % ferric chloride solution was added for the formation of green or blue colour, for confirmation.
Test for Resins
To an aliquot of 10 ml of diluted extract, an aliquot of 10 ml of 1 % cupper acetate solution was added and the mixture was shaken vigorously; a separate green colour indicated the presence of resin.
Determination of Total Phenolic Content
Total phenolic content (TPC) of A. caroliniana was assessed using folin-cioclateu reagent [20]. Stock solutions of methanolic and ethanolic semi-solid extracts were separately prepared in methanol at 1 mg/ml. An aliquot of 1.5 ml from each stock solution was taken in a 25 ml size volumetric flask to which, a volume of 10 ml water and an aliquot of 1.5 ml folin-ciocalteu reagent were added. The mixture was kept for 5 min, and an aliquot of 4 ml 20 % sodium carbonate solution was added and the volume was made up to 25 ml, with doubled distilled water. After incubating the mixture for 90 min, its absorbance, of triplicate preparations were measured at 760 nm in a UV–VIS spectrophotometer. The total phenolic content was calculated as gallic acid equivalent by using equation obtained from the gallic acid calibration curve.
DPPH Free Radical Scavenging Assay
The free-radical scavenging activities of A. caroliniana extracts and ascorbic acid (standard antioxidant) were measured in terms of the reduction of hydrogen donating free radical scavenging ability with 1,1-diphenyl-2-picryl hydrazyl (DPPH), measured by reading as the absorbance (A) at 517 nm by a spectrophotometer [21]. An aliquot of 1.5 ml of 0.1 mM DPPH solution was mixed with an aliquot of 1.5 ml of each of increasing concentrations (5–500 µg/ml) of methanolic and ethanolic extracts of the fern along with ascorbic acid. The mixture was shaken vigorously and incubated at room temperature for 30 min in dark. Thus, there were three absorbance values (Atest or Acontrol) including that of the standard antioxidant; the solution with DPPH and methanol/ethanol without any extract was used as the control (Acontrol). The experiment was replicated as three independent assays. Percent inhibition values of antioxidant activity using DPPH free radicals were calculated with recorded absorbance by the following formula.
DPPH free radical scavenging activity (%) = [(Acontrol − Atest)/Acontrol] × 100, where, Acontrol was the absorbance of the solution without extract and Atest was the absorbance of a sample, extract or ascorbic acid. These values were plotted for getting the inhibition concentration 50 % (IC50) values of both extracts along with the standard.
ABTS Radical Scavenging Assay
The assay was based on the ability of two solvent extracts of the fern to scavenge free radicals of 2, 2-azino-bis (ethylbenzthiazoline-6-sulfonic acid) (ABTS+) in comparison with the standard antioxidant butylated hydroxytoluene (BHT). The stock solutions of 7 mM ABTS+ and 2.45 mM potassium persulfate were prepared separately. The working solution was prepared by mixing the two stock solutions in equal quantities and the mixture was allowed for 12 h in the dark at room temperature. The resulting solution was diluted by mixing 1 ml of freshly prepared ABTS+ solution with an aliquot of 1 ml methanol to obtain an absorbance of 0.706 ± 0.001 at 734 nm using the spectrophotometer [22]. Methanolic and ethanolic extracts in aliquot of 1 ml each was allowed to react with aliquots of 2.5 ml ABTS+ solution and absorbance was taken at 734 nm after 7 min. The experiment was conducted as three independent repeated assays and the mean absorbance value was used for computation of the percent inhibition values of scavenging capacity of the extracts which were calculated as under:
where, Acontrol was the absorbance of ABTS+ solution with methanol; Atest was the absorbance of ABTS solution with sample extract/standard. Those values were plotted for getting the IC50 values of both extracts along with the standard.
Hydrogen Peroxide Scavenging Activity
A solution of 40 mM H2O2 was prepared in phosphate buffer saline (PBS, pH 7.4) solution. The test extract of A. caroliniana in an aliquot of 4 ml, in distilled water at different concentrations was mixed with an aliquot of 0.6 ml 40 mM H2O2 solution in PBS and the mixture was incubated for 10 min [23]. The absorbance of the solution was taken at 230 nm against a blank solution containing only plant extract in PBS. Ascorbic acid was used as the standard. The radical scavenging activity of two extracts and standard were calculated using the following equation:
where, Acontrol was the absorbance of H2O2 radical with methanol; Atest was the absorbance of H2O2 radical with sample extract or standard. These values were plotted for getting the IC50 values of both extracts along with the standard.
Nitric Oxide (NO) Scavenging Activity
Activities of frond extracts to scavenge NO to produce nitrite ions were measured by the standard spectrophotometric method [24]. An aliquot of 1 ml 5 mM sodium nitroprusside in PBS was mixed with an aliquot of 1.0 ml ethanolic/methanolic extract in different concentrations and the mixture was incubated at 25º C for 30 min. Equivalent amount of methanol was used as control. After 30 min, the incubated solution in an aliquot of 1.5 ml was diluted with 1.5 ml of Griess reagent (1 % sulphanilamide, 2 % phosphoric acid and 0.1 % naphthyl ethylenediamine dihydrochloriode). The absorbance of the solution was measured at 546 nm. All the tests were performed in triplicate and absorbance was used for the computation of percentage of inhibition by the following formula:
where, Acontrol was the absorbance of the control (without extract) and Atest was the absorbance in the presence of the extract/standard. These values were plotted for getting IC50 values of both extracts along with the standard.
Organoleptic Evaluation
A considerable mass of A. caroliniana fronds were washed with tap water followed by sterilization by 1 N normal saline and final washing with sterile drinking water. The whole frond mass was mixed with gram flour with salt to taste and fried in hot edible oil. Organoleptic evaluation of fried materials was carried out by a panel of 10 persons by taking account of its smell, colour, test, toughness and chewiness with a measuring scale of 10 points [25].
Results and Discussion
Isolation and Identification of Bacterial Isolates
GP bacteria as medium to large, smooth, entire, slightly raised, creamy yellow, green/β-haemolytic colonies on blood agar, found positive to catalase and coagulase tests were confirmed to be S. aureus (Fig. 2). Further, cells positive to bile-esculin test, as well as, negative to catalase and coagulase tests were taken as Enterococcus sp., which produced greyish, round, small colonies with haemolytic zones on blood agar. Again, Citrobacter sp. was identified by its colony characteristics on MacConkey (MC) agar and results obtained from biochemical tests; it produced light pink-coloured late-lactose-fermenting (LLF) colonies after a 48 h incubation on MC agar; particularly, it was positive to catalase, methyl red (MR), citrate and nitrate tests, whereas it was negative to oxidase, indole, Voges-Proskauer (VP) and urease tests. On the triple sugar iron (TSI) test, the bacterium produced both acid and H2S gas during growth. Likewise, the rest four GN bacteria were identified from their colony and biochemical characters (Tables 1, 2).
Antibiotic Sensitivity of Bacterial Isolates
Antibiotic susceptibility tests of two GP bacteria were carried out using 15 antibiotics of six groups. The isolated Enterococcus sp. strain was sensitive to three antibiotics, ciprofloxacin, chloramphenicol and vancomycin fully and moderately sensitive to tetracycline, whereas it was found totally resistant to the rest 11 antibiotics (Table 3). Similarly, the S. aureus strain was resistant to antibiotics, ciprofloxacin, chloramphenicol, co-trimoxazole and vancomycin; but it was completely resistant to the rest 11 antibiotics. Further, antibiotic susceptibility tests of 5 GN bacteria were carried out using 16 antibiotics of six groups. Citrobacter sp. was sensitive only to gentamicin and chloramphenicol, but it was resistant to rest 14 antibiotics. Likewise, from antibiograms of the rest 4 GN bacterial strains, the number of resistant antibiotics out of the total antibiotics were as follows: E. aerogenes for 6, E. coli for 14, P. mirabilis for 13, and P. aeruginosa for 13 antibiotics (Table 3). The MTCC strains used in the study were sensitive to all the antibiotics used.
Antibacterial Efficacy of A. caroliniana Extracts
Among four solvent-extracts of the fern, the methanolic extract registered the maximum size of zone of inhibition against S. aureus (average, 20 mm), followed by Enterococcus sp., P. mirabilis and P. aeruginosa (18 mm, each); while, against, E. aerogenes and E. coli (15 mm, each); and the least against Citrobacter sp. (13 mm). Similarly, the ethanolic extract registered the maximum size of zone of inhibition, as 18 mm against, P. mirabilis, followed by S. aureus, E. aerogenes and P. aeruginosa (each, 16 mm), while E. coli and Enterococcus had 15 mm and Citrobacter sp. had 13 mm as inhibition-zone sizes. Likewise, the chloroform extract registered the maximum size of zone of inhibition as 18 mm against, E. aerogenes, with the decreasing trend, S. aureus (16 mm). P. aeruginosa strain had 14 mm and E. coli had 13 mm of inhibition-zone sizes, whereas the least value of the size of zone of inhibition against Citrobacter sp. and P. mirabilis was 12 mm. The n-hexane extract registered insignificant antibacterial activities, as compared to the other three solvent-extracts against all bacteria, except for S. aureus, against which the zone of inhibition was 12 mm (Table 4). In general, the methanolic extract was found to be the best in comparison to those extracted with ethanol, chloroform and n-hexane.
MIC and MBC Values of A. caroliniana Extracts
MIC and MBC values of the three leading extracts with solvents, methanol, ethanol and chloroform of the fern, were recorded. The MIC value, 1.89 mg/ml was of the methanolic extract recorded against S. aureus and P. mirabilis, while the value of 4.27 mg/ml was recorded against Enterococcus sp., E. aerogenes, E. coli and P. aeruginosa. Further, against Citrobacter sp. the MIC value of the methanolic extract was 9.63 mg/ml. Again, a MIC value 1.89 mg/ml was of the ethanolic extract recorded against P. mirabilis, while the value of 4.27 mg/ml was recorded against S. aureus, E. aerogenes, and E. coli. Further, against Enterococcus sp., Citrobacter sp. and P. aeruginosa, the recorded MIC value of the ethanolic extract was 9.63 mg/ml. Further, the MIC value of 4.27 mg/ml of the chloroform extract was recorded against S. aureus, E. aerogenes, E. coli, and P. mirabilis, while against Enterococcus sp., Citrobacter sp., and P. aeruginosa the MIC value was 9.63 mg/ml (Table 5). The MBC value, 4.27 mg/ml of the methanolic extract was recorded against S. aureus and P. mirabilis, while the value of 21.67 mg/ml was recorded against Enterococcus sp., Citrobacter sp., E. aerogenes, E. coli and P. aeruginosa. Again, the MBC value, 9.63 mg/ml of the ethanolic extract was recorded against S. aureus and P. mirabilis, while the value of 21.67 mg/ml was recorded against Enterococcus sp., Citrobacter sp., E. aerogenes, E. coli and P. aeruginosa. Further, the MBC value of 9.63 mg/ml of the chloroform extract was recorded against S. aureus, while against Enterococcus sp., Citrobacter sp., E. aerogenes, E. coli, P. mirabilis and P. aeruginosa, the MBC value of the chloroform extract was 21.67 mg/ml (Table 5).
Phytochemical Analysis of A. caroliniana Extracts
Extracts with four solvents, methanol, ethanol, chloroform and n-hexane were used for phytochemical analyses. In all extracts, both alkaloids and saponins were absent. Phytoconstituents, glycosides, terpenoids, carbohydrates, tannins, flavonoids, steroids, resins, phenols and anthraquinones were present in methanolic and ethanolic extracts. The chloroform extract had three phytoconstituents, glycosides, carbohydrates and phenols only, whereas the n-hexane extract had only one, the phenol. Thus, only phenols were detected in all four Azolla extracts (Table 6).
Total Phenolic Contents
Determined by the modified folin-ciocalteu method, TPCs of extracts were calculated using the standard curve of gallic acid (standard curve equation: Y = 0.004x + 0.063, R2 = 0.998) as gallic acid equivalent (GAE). TPC in the methanolic extract was 96.45 mg GAE/g and that of the ethanolic extract was 78.25 mg GAE/g.
DPPH Radical Scavenging Activity
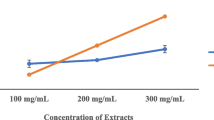
Methanolic and ethanolic extracts of A. caroliniana and the standard antioxidant, ascorbic acid significantly inhibited the free radical scavenging activity of DPPH in a concentration dependent manner. At 10 µg/ml concentration, the percentages of inhibition were 50.03, 0.2, and 74.81 for methanolic, ethanolic extracts and ascorbic acid, respectively. At the level of 50 µg/ml, the scavenging effects were 54.54, 12.41 and 88.72 % for extracts with methanol, ethanol and the ascorbic acid, respectively. The IC50 values of DPPH free radical scavenging activity for methanolic and ethanolic extracts as well as the standard antioxidant, ascorbic acid were 8, 120 and 5 µg/ml, respectively (Fig. 3). As seen, the methanolic extract had the highest scavenging activity, followed by that of ascorbic acid (Table 7).
Antioxidative activity of A. caroliniana by DPPH free radical scavenging assay with ascorbic acid as the control. Each inhibition concentration 50 value is extrapolated from the line running from X-axis to Y-axis touching the response curve. Extrapolated IC50 values of DPPH free radical scavenging activity for methanolic and ethanolic extracts as well as the standard antioxidant, ascorbic acid were 8, 120 and 5 µg/ml, respectively. Black circle ascorbic acid, blue circle methanolic extract, red circle ethanolic extract
ABTS Radical Scavenging Activity
Methanolic and ethanolic extracts of A. caroliniana along with the standard antioxidant, BHT were seen at 10, 50, 100, 200 and 500 μg/ml of both extracts and BHT for free ABTS scavenging activity. At 10 μg/ml concentration the percentage of inhibition values were 54.67, 0.42 and 77.62; while at 500 μg/ml, the percentage inhibition values were 85.41, 83.85 % and 95.46 %, respectively (Table 7). Extrapolated IC50 values of ABTS radial scavenging effects of methanol extract, ethanol extract and standard BHT were 10, 109.37 and 9.45 μg/ml, respectively (Fig. 4).
Antioxidative activity of A. caroliniana by ABTS free radical scavenging assay with BHT as the control. Each inhibition concentration 50 value is extrapolated from the line running from X-axis to Y-axis touching the response curve. Extrapolated IC50 value of ABTS radial scavenging effects of methanol extract, ethanol extract and standard BHT were 10, 109.37 and 9.45 μg/ml, respectively. Black circle BHT, blue circle methanolic extract, red circle ethanolic extract
Hydrogen peroxide radical scavenging activity
Methanolic and ethanolic extracts of A. caroliniana along with the standard antioxidant ascorbic acid were seen at 10, 50, 100, 200 and 500 μg/ml of both extracts and ascorbic acid for free H2O2 scavenging activity. At all levels antioxidant activities were noted. At 10 and 500 μg/ml percentages of inhibition values were 50.67, 0.5 and 76.78, respectively at the lowest level, and at 500 μg/ml level, percentages of inhibition values were 86.57, 82.95 and 95.46, respectively (Table 8). Extrapolated IC50 values of the methanolic extract, ethanolic extract and ascorbic acid were 10.0, 95.5 and 8.5 μg/ml, respectively (Fig. 5).
Antioxidative activity of A. caroliniana by H2O2 free radical scavenging assay with ascorbic acid as the control. Each inhibition concentration 50 value is extrapolated from the line running from X-axis to Y-axis touching the response curve. Extrapolated IC50 values of the methanolic extract, ethanolic extract and ascorbic acid were 10.0, 95.5 and 8.5 μg/ml, respectively. Black circle ascorbic acid, blue circle methanolic extract, red circle ethanolic extract
Nitric Oxide Scavenging Assay
Methanolic and ethanolic extracts of A. caroliniana along with the standard antioxidant ascorbic acid were seen at 10, 50, 100, 200 and 500 μg/ml of both extracts and ascorbic acid for free NO scavenging activity. At 10 μg/ml, methanolic extract, ethanolic extract and ascorbic acid successfully inhibited NO radial scavenging activity with percentage of inhibition values of 14.67, 0.2 and 48.90, respectively. At 500 μg/ml, the percentage inhibition values of methanolic, ethanolic extracts and ascorbic acid were 79.33 and 78.18 and 92.5, respectively (Table 8). Extrapolated IC50 values for methanolic and ethanolic extracts and ascorbic acid were 78.8, 175.8 and 12.8 μg/ml, respectively (Fig. 6).
Antioxidative activity of A. caroliniana by NO free radical scavenging assay with ascorbic acid as the control. Each inhibition concentration 50 value is extrapolated from the line running from X-axis to Y-axis touching the response curve. Extrapolated IC50 values for methanolic and ethanolic extracts and ascorbic acid were 78.8, 175.8 and 12.8 μg/ml, respectively. Black circle ascorbic acid, blue circle methanolic extract, red circle ethanolic extract
Organoleptic Properties of A. caroliniana
Organoleptic properties of A. caroliniana were calculated by the mean value of the individual marks obtained by each person in a 10-point rating scale and showed significant result for smell, test and colour. The overall acceptability was not significantly different from chewiness and toughness, as Azolla was having no taste (Table 9).
In the present study, antibiograms of all the seven bacterial strains used here clearly indicated that all the isolated strains were figuratively MDR; so, this work overrides all other similar antibacterial works with plants dealing with pathogenic bacteria without any report on their antibiotic-sensitivity patterns [7, 9]. The present work on pathogenic bacteria has an additional edge over any other antibacterial work on ‘drug sensitive pathogenic bacteria obtained from type culture centres’, as isolated bacteria were floridly MDR. Obviously, MDR pathogenic bacteria are the culprits of clinical annoyance.
Moreover, crude extracts of several plants are continually scaled up, for individual use or as coalesced concoctions against a myriad of health ailments, worldwide [7, 9]. A cavalcade of phyto-drugs, such as morphine, quinine, digoxin and many more iconic pure phytochemicals are unequivocally in use for specific health problems. Additionally, a survey on populations using CAM as health care needs, done by WHO could be given in succinct: Chille 71 %, Columbia 40 %, African nations 80 %, China 40 %, India 45 %, among developing countries; concomitantly, developed countries, Australia 48 %, Canada 70 %, USA 42 %, Belgium 38 %, and France 75 % populations use CAM [12]. Furthermore, cost involved with CAM was US $ 500 million in Malaysia, annually as compared to 300 million US $ for allopathic drugs, annually. In the US, the cost of CAM used was 300 million $ annually. In Australia, UK and Canada, the annual cost of used CAM was estimated at 80, 2,300, 2,400 million US $, respectively [12]. Specifically, the value of plant-based prescribed drugs in 1990 was estimated at 15.5 billion US $, which had been on the rise since then to 35 billion US $, during the last decade [7, 26]. Not surprisingly, about 42 % of 25 top-selling phyto-drugs marketed worldwide are either directly obtained from natural sources or their value-added products [7]. Particularly, the Indian herbal market grows fast and should have attained to the level of 265 billon US $ per annum by 2013, a priory, known from the available trends. Moreover, the industry based on Indian herbal market was estimated at 130 billion US $, and more than 65 billion US $ of herbal raw materials and medicines were exported from India by 2010 [26]. Such herbal trade markets and the use of herbal products must be developing in each country, unbeknownst to the systematically recorded databases. Indeed, herbal products are widely held today for the health boosting as preventives by the WHO mandates [12]. And in future these would be deeply held for more specific needs as CAM, if phyto-drugs could be scaled as remedial measures, without any dyslogistic prejudice in the face of mainstream medicines. Obviously, host-toxicity testing of non-edible/poisonous plant-products remains an essential corollary in CAM too, for the scientific validation and safety. Paradigmatically in India, people from the marginalized section, slum-ghettos and aborigines, as well as the sophisticated, well-heeled, elite mass use concoctions of crude phyto-drugs from Ayurvedic, Unani and Siddha systems, habitually [7, 27]. Similar medicinal systems too are in the cultural practices of people of other countries; eventually, phyto-toxicity studies with well known and lesser known plants against mammalian systems have been recorded frequently [28]. Moreover, apart from developing countries, the developed world has too a renewal of interest towards the use of resplendent herbal medicines for health-boosting or conditioning and for treating/preventing several common/non-common ailments, despite the ready availability of modern medicine [12]. As the coterie of pharmacology has been acknowledging medicinal plants as the potential sources of bioactive compounds, crude phyto-extracts need be considered logistically as CAM for fixing infections.
The traditional knowledge on the use of plants is the basis of their uses as TM; the concept of CAM has been emerged, as a result. After all, many safe and efficacious drugs in crude plant-preparations languish without a proper attention in focusing as microbial control agents, despite the development of suitable antimicrobials is central to the endeavour for the control of MDR bacterial pathogens. For a litany of preventive medicinal plant extracts, curative drugs are to be harnessed. For the purpose, fractional isolation with the available range of organic solvents should be done, and then fractions of a plant-extract should be pursued for microbial bioassay work with the frequently isolated MDR bacteria. The most effectivet phyto-compounds could be isolated and purified with the repertoire of pharmacognosy with finesse. This would, definitely, involve a long road till one or more compounds would be located as microbials from plants. For example, the combination therapy of dasatinib (the chemical drug ensconced for many types of cancer—chronic myeloid leukaemia, colorectal cancer etc.) and curcumin from Curcuma longa (turmeric) had been shown to demonstrate synergistic interactions of targeting/control of cellular growth and metastatic invasion of sub-populations of cancer stem cells at chemo-resistant colon cancer [29]. Today, preparation of adjuvant drugs with phytochemicals is the thrust area of coteries (pharmacognosy, pharmacology and pharmaceutics) of apothecary [29]. Thus, the preventive characteristics of medicinal plants could be prudently exploited, for the development of non-microbial antimicrobials along with other drugs in trials for the possible use as curative medicine.
Nosocomial accounts of three MDR bacteria, P. aeruginosa, S. aureus and E. coli of this hospital had been quantified, independently [2–4, 16], and it had been clear that prevalence of MDR strains of each pathogen increased with time, in the study period up to early of year 2013. One of these, E. coli, being a urinary tract infection causing pathogen and the other, S. aureus was a commensal-turned superbug of the health domain, and third P. aeruginosa—all causing mortality to saturnine heights, worldwide [16]. As evident in the present work, the rest other five pathogens were too amply MDR. The prime concern is that when each of these bacteria are MDR, the situation of multiple infection of two or more MDR strains could precipitate intractable episodes in public health; infant and under 5-mortality rates and decimation of slum-dwellers as well as rural rustics of the country could be of surprising standard, as noted [4, 10].
The emergence of MDR pathogenic bacteria occurred from several reasons, but the oblivious attitude of physicians to stringent antibiotic policy contributes sizably. For example, for an unknown viral infection an antibiotic course is prescribed unscrupulously, which is terminated at 3 or 4 days of drug intake, after the remission of severe symptoms. This induces resistance in some non-target commensal of body to become resistant to the drug applied; this was observed with the original commensal, S. aureus that transformed to the notorious/superbug, methicillin resistant S. aureus (MRSA). Secondly, the paramedical and supporting personnel of a hospital are intransigent to impeccable antiseptic practices, such as, proper hand-wash techniques, prevention of needle stick injuries, maintenance of hygienic environment of hospital interiors with a crowding of patients and their attendants, as well as scientific disposal of offal of the hospital and hospital sewage. No matter how small and clean a hospital would be, it lets space for the spread of bacterial spores nosocomially from and to health workers and patients [2, 4]. Most often, it had been recorded that an aged or immunocompromised patient admitted for an ailment into ICU or wards and cabins, while discharging from the hospital goes back to home with an acquired MDR pathogenic infection insidiously [2–4] eventually causing spread of MDR bacteria in community. Sometimes, a physician prescribes an antibiotic of a higher generation for a dramatic effect on the control of an infection. Often, this practice may promote the development of a drug resistant mutant of a pathogen or commensal in patient’s body, which survives in due course as a drug resistant pathogen. This situation occurs, because the applied antibiotic eliminates all the sensitive strains of the pathogen and the resistance pathogen being minor in quantity survives, multiplies and predominates even in the presence of the applied antibiotic. This confirms the biological rule: any limiting condition for the majority would be an excellent opportunity for the minority. Obviously, the population of a sensitive strain is in majority that would suffer elimination and the population of a resistant strain is in minority that would come up, to state in the Darwinian way! Application of combination/adjuvant therapy with 2 or more drugs, most often, would help escape from this conundrum of umpteen notorious pathogens, as followed for TB-chemotherapy [9]. Crude Azolla-extracts, obviously with many phytochemicals, used herein in vitro helped the control of 7 ferocious pathogens.
Total TPC was more in the methanolic extract of A. caroliniana and this extract had a better free radical scavenging activity than the ethanolic extract. Thus, it could be stated that phenolic compounds contributed to the antioxidant activity here too; nevertheless, the ethanolic extract had this activity to a considerable extent. Reactive oxygen species (ROS) include several metabolic by-products, hydrogen peroxide, hydroxyl radicals, nitric oxide, superoxide anions, peroxy nitrite and few more that are potential enough to trigger degenerative processes in human body [30]. Compounds such as, phenolic acids, polyphenols and flavonoids from plants are recognised as antioxidants, as they have the ability to scavenge free radical generating ROS, as in the present study.
Globally Azolla has been used mostly as feed and fodder and to a lesser extent as food. It is to be cultivated under hygienic conditions for the use as an antioxidant, since its older roots get detached from plants and decompose fast leading to growth of microorganisms and algae. Its mineral requirements in growth medium are already standardized [13]. The present finding of the presence of phenols in the four solvent extracts of Azolla and the universal previous reports of the link of phenols in rendering antioxidant properties is suggestive of the high levels of recorded antioxidant activity. Moreover, the absence of alkaloids and saponins in all the solvent extracts too qualify the fern to be devoid of unpalatable experiences as food, as usually seen with plants with these two types of phytocompounds. From organoleptic analysis, it could be inferred that the cooked fern was tasteless, but was not unpalatable; consequently it should not be suggested for the use as food. Thus, Azolla could be used for the preparation of antioxidant as well as antimicrobial for MDR bacteria, qualifying it as use as a unique, rather a cost-effective CAM. Large proportions of plant drugs are popular for their performance standards, and are in use by the elite mass. Here two epitomes would be: the use of the decoction of internodes of the anti-diabetic, Tinospora cordifolia in India, and the other one is Panax ginseng (ginseng) root—best known to lower blood sugar and cholesterol levels, protect against stress, enhance strength and promote relaxation, from the Eastern world with a remarkable popularity in the USA. Many health-boosting formulations, concocted with many herbal products have been slowly growing popular in Brazilian, American and Chinese societies [30, 31], and that should also be occurring in equal or lesser dimensions in many other countries.
Conclusion
The present work substantiates that, if Azolla could be grown in pollutant-free water in mass under controlled aesthetic conditions, it could be processed for the use as qualitative antioxidant as well as antimicrobial for MDR bacteria infecting humans. The use of Azolla as CAM could be seriously taken up for its both antioxidant and antimicrobial efficacy. Since, MDR strains of the iconic seven bacterial uropathogens described here are active in both hospital settings and community [16] causing beleaguering multi-morbid acute health conditions, such as initial cystitis, prostatitis, pyelonephritis followed subtly by blood steam infection from kidney to innards of humans of any age, eventually in causing bacteremia/septicaemia in chest and lungs. Often such patients are declared as having mortality from infections at chest and lungs. These could culminate in frequent public health episodes followed by disproportionate mortality, when infection dynamics of MDR bacteria are considered dispassionately [2–4]. This fern could be prudently used as CAM, as well as health boosting of aged, immunocompromised patients and pregnant women. However, the antimicrobial activity needs further scaling with its pure phytochemicals; host-toxicity work with animals and humans is redundant in this food plant, logistically. Secondly, the absence of alkaloids and saponins qualifies it as a food grade plant and its phenols support to its antioxidant activity. In parallel, the cyanobacterium, Spirulina grown in open-air tanks have been serving as a popular dietary supplement/antioxidant. If scaled up, Azolla could also help the development of market-based local units of commerce in developing countries as an antioxidant. The non-committal attitude on crude phyto-drugs for the use as antimicrobials, but seeking pure phytochemicals only for the purpose, would be tantamount to the love for academic/scientific study only, but it would not be an attempt for an immediate practical solution in the crusade against the fast evolving MDR bacteria, at least in resource settings, as in India and other developing countries’. Thus, use of plant based drugs should be not considered with a pejorative attitude towards the natural wealth of the prodigious healing agents, to state in sotto voce.
References
Giamarellos-Bourboulis EJ, Papadimitriou E, Galanakis N, Antonopoulou A, Tsaganos T, Kanellakopoulou K et al (2006) Multidrug resistance to antimicrobials as a predominant factor influencing patient survival. Int J Antimicrob Agent 27:476–481
Sahu MC, Dubey D, Rath S, Debata NK, Padhy RN (2012) Multidrug resistance of Pseudomonas aeruginosa as known from surveillance of nosocomial and community infections in an Indian teaching hospital. J Pub Health 20:413–423
Dubey D, Rath S, Sahu MC, Patnaik L, Debata NK, Padhy RN (2013) Surveillance of infection status of drug resistant Staphylococcus aureus in an Indian teaching hospital. Asian Pacif J Trop Dis 3:930–939
Rath S, Dubey D, Sahu MC, Padhy RN (2014) Surveillance of ESBL producing multidrug resistant Escherichia coli in a teaching hospital in India. Asian Pacif J Trop Dis 4:140–149
Bilington OJ, Gillespie SH (2001) Estimation of mutation rates in antibiotic research, chapter 23. In: Gillespie SH (ed) Methods in molecular medicine. Antibiotic resistance—methods and protocols, vol 48, pp 227–232. Humana Press, Totowa, New Jersey
Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L et al (2010) Neonatal, postneonatal, childhood and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards Millennium Development Goal 4. Lancet 375:1988–2008
Dubey D, Rath S, Sahu MC, Debata NK, Padhy RN (2012) Antimicrobials of plant origin against TB and other infections and economics of plant drugs—introspection. Ind J Trad Know 11:225–233
Dubey D, Sarangi R, Debata NK, Padhy RN (2013) Detection of metallo-β-lactamase producing Klebsiella pneumoniae in a neonatal septicemia. J Acute Dis 2:82–84
Dubey D, Rath S, Sahu MC, Nayak N, Debata NK, Padhy RN (2013) Status of multidrug resistance in tubercle bacillus and phytochemicals for the control. J Pub Health 21:115–119
Rath S, Padhy RN (2012) Surveillance of multidrug resistance of 10 enteropathogens in a teaching hospital and in vitro efficacy of 25 ethnomedicinal plants used by an Indian aborigine. Asian Pacif J Trop Dis 2(spl vol):S336–S346
Dubey D, Padhy RN (2013) Antibacterial activity of Lantana camara L. against multidrug resistant pathogens from ICU patients of a teaching hospital. J Herb Med 3:65–75
WHO (2011) WHO traditional medicine strategy. In: WHO/EMP/MIE/2011.2.3, Geneva, World Health Organization 2011; pp 1–14. Available via DIALOG. http://apps.who.int/medicinedocs/documents
Singh PK (1989) Use of Azolla in Asian agriculture. Appl Agri Res 4:149–161
Nayak N, Rath S, Mishra MP, Ghosh G, Padhy RN (2013) Antibacterial activity of the fern Lygodium flexuosum (L.) Sw. against multidrug resistant enteric- and uro-pathogenic bacteria. J Acute Dis 2:270–276
Angalao LA, Doctor JGP, Banwa T (2012) Antimicrobial Activities of Azolla filiculoides Lam. (Pteridophyte) and Brachythecium buchananii (Hook.) Jaeg. (Bryophyte). Int J Sci Clin Lab 2:71–81
Mishra MP, Debata NK, Padhy RN (2013) Surveillance of multidrug resistant uropathogenic bacteria in hospitalized patients—an Indian study. Asian Pacif J Trop Biomed 3:315–324
Subudhi BPR, Singh PK (1978) Nutritive value of water fern Azolla pinnata for chicks. Poultry Sci 57:378–380
Xiaofeng L, Chen M, Liu X, Liu C (2008) Research on some functions of Azolla in CELSS system. Acta Astronaut 63:1061–1066
Sjodin E (2012) The Azolla cooking and cultivation project. http://www.eriksjodin.net. Accessed on 20 Aug 2013
Tepe B, Sokmen M, Akpulat HA, Sokmen A (2006) Screening of the antioxidant potentials of six Salvia species from Turkey. Food Chem 95:200–204
Hsu CY, Chan YP, Chang J (2007) Antioxidant activity of extract from Polygonum cuspidatum. Biol Res 40:13–21
Re R, Pellegrini N, Proteggente A, Pannala A, Yang M, Rice-Evans C (1999) Antioxidant activity applying an improved ABTS radical cation decolorization assay. Free Radical Biol Med 26:1231–1237
Ruch RJ, Cheng SJ, Klaunig JE (1989) Prevention of cytotoxicity and inhibition of intracellular communication by antioxidant catechins isolated from Chinese green tea. Carcinogenesis 10:1003–1008
Madan NP, Raghavan G, Singh AK, Palpu RP (2005) Free radical scavenging potential of Saussarea costus. Acta Pharm 55:297–304
Ashaye OA, Babalola SO, Babalola AO, Aina JO, Fasoyiro SB (2005) Chemical and organoleptic characterization of pawpaw and guava leather. World J Agri Sci 1:50–51
Saini N, Saini K, Singh GK (2011) Establishment of an herbal industry in India. Int J Pharma Bio-arch 2:1011–1019
Ramya S, Kalaivani T, Rajasekaran C, Jepachanderamohan P, Alaguchamy N, Kalayansundaram M et al (2008) Antimicrobial activity of aqueous extracts of bark, root, leaves and fruits of Terminalia arjuna Wight and Arn. Ethnobot Leaflet 12:1192–1197
Jothy SL, Zakaria Z, Chen Y, Lau YL, Latha LY, Sreenivasan SS (2011) Acute oral toxicity of methanolic seed extract of Cassia fistula in mice. Molecule 16:5268–5282
Nautiyal J, Kanwar SS, Yu Y, Majumdar APN (2011) Combination of dasatinib and curcumin eliminates chemo-resistant colon cancer cells. J Molec Signal 6:7. http://www.jmolecularsignaling.com/content/6/1/7
Wang SY, Kuo YH, Chang HN, Kang PL, Tsay HS, Lin KF (2002) Profiling and characterization antioxidant activities in Anoectochilus formosanus Hayata. J Agri Food Chem 50:1859–1865
Lam KS (2007) New aspects of natural products in drug discovery. Trend Microbiol 15:279–289
Acknowledgments
This work is a part of PhD thesis of N Nayak in Biotechnology, who is supported by a fellowship from Siksha ‘O’ Anusandhan University. RN Padhy is an Emeritus Scientist from Council of Scientific and Industrial Research, New Delhi. PK Singh, FNAAS, FNA is a Senior Scientist from Indian National Science Academy (New Delhi), at BHU. Sri Gopabandhu Kar, MM of IMS and Sum Hospital, Bhubaneswar provided extended facilities. We thank Sri Somadatta Das, DEO at IMS and Sum Hospital for graphs and arduous secretarial help. Authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nayak, N., Padhy, R.N. & Singh, P.K. Evaluation of Antibacterial and Antioxidant Efficacy of the Fern Azolla caroliniana Symbiotic with the Cyanobacterium Anabaena azollae . Proc. Natl. Acad. Sci., India, Sect. B Biol. Sci. 85, 555–569 (2015). https://doi.org/10.1007/s40011-014-0370-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40011-014-0370-3