Abstract
Purpose
Cardiac involvement in dengue fever is underdiagnosed due to low index of clinical suspicion and its contribution to hemodynamic instability in severe dengue is not well known.
Methods
A prospective observational study was conducted among admitted patients ≥ 14 years of age having confirmed dengue fever. Patients on medications affecting heart rhythm/rate, pre-existing heart disease and electrolyte abnormalities were excluded. A baseline electrocardiography (ECG), Trop-I and NT-proBNP were done for all patients. The biomarkers were measured using enzyme-linked fluorescent assay and recommended cut-off were used. Patients with elevated biomarkers underwent 2-dimensional echocardiography. Diagnosis of myocarditis was as per European Society of Cardiology (ESC) 2013 criteria.
Results
A total of 182 patients were recruited with mean age of 30 ± 12.6 years and 31% were females. Dengue with warning signs was present in 85 (47%) and severe dengue in 60 (33%) patients. ECG abnormalities were observed in 44 (24%) patients, biomarkers were elevated in 27 (15%) patients and 11 (6%) patients had echocardiographic abnormalities. According to ESC 2013 criteria, dengue fever with myocarditis was diagnosed in 13 [7.1% (95% CI 3.4–10.9)] patients. The patients with myocarditis were more likely to have shortness of breath, bleeding manifestations and higher respiratory rate at baseline. Clinical features of fluid overload were more common (69% vs. 1.7%, p < 0.01) and the duration of hospital stay longer in myocarditis group (7 ± 4.3 vs. 4.8 ± 1.9 days, p < 0.01).
Conclusion
Myocarditis among admitted dengue patients is not uncommon and may lead to increased morbidity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dengue is one of the most important mosquito-borne diseases in the world [1]. The spectrum of dengue includes undifferentiated fever to more serious forms of the disease including dengue with warning signs and severe dengue. Cardiac involvement although poorly recognised, may not be infrequent in patients with severe dengue. Since very few patients with dengue have a formal cardiac assessment, the frequency of subclinical dengue myocarditis and its relative contribution to the haemodynamic instability in severe dengue is unclear. A range of cardiac abnormalities have been reported including myocarditis, pericarditis, conduction disturbances, tachyarrhythmias and non-specific electrocardiographic changes [2,3,4,5,6,7,8]. Literature on the prevalence and outcomes related to dengue myocarditis is sparse and inconsistent due to varied diagnostic criteria. The reported range of myocarditis varies from 0 to 37.5% of dengue patients. In a recent study from China, the prevalence of myocarditis in hospitalized dengue patients was found to be 11.3% and these patients had more severe forms of the disease [9]. A study conducted by Miranda et al. reported evidence of myocarditis in 2.47% of hospitalized dengue patients [10]. In India a study reported the prevalence of myocarditis in dengue patients as 37.5% and these patients had a severe form of disease [11] In another study from India, the most common cardiac manifestations noted were transient rhythm abnormalities; however, none of them had myocarditis [12]. This study was conducted to determine the prevalence of myocarditis in hospitalized dengue patients and to evaluate their outcomes.
Materials and methods
This was a prospective observational study conducted among admitted patients with confirmed dengue at a tertiary care center in northern India. The study was conducted between September to November 2018 and Ethical clearance was obtained from the Institute Ethics Committee. The diagnosis of dengue was based on NS1 ELISA/ IgM-capture enzyme-linked immunosorbent assay (MAC-ELISA). We included patients ≥ 14 years of age with confirmed dengue, hospitalized in the medical wards and medical ICU. Patients on medications affecting heart rhythm/rate, patients with a pre-existing heart disease or patients with electrolyte abnormalities potentially affecting heart rate/rhythm were excluded from the study. Patients admitted to the emergency ward (< 24 h) and Pediatrics wards were also excluded.
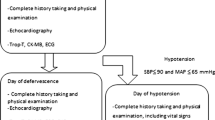
Baseline demographic, clinical and laboratory parameters were collected. Severity was classified based on WHO guidelines (2009). A baseline ECG, cardiac enzymes Trop I and NT-ProBNP were measured for all patients. The biomarkers were measured using an enzyme-linked fluorescent assay (VIDAS Troponin I Ultra and NT-proBNP, bioMérieux, France). Trop I was considered to be raised when serum levels were more than 19 ng/L; NT-proBNP levels were considered to be elevated when it was more than 450 ng/L (age < 50 years), 900 ng/L (age 50–75 years), and 1800 ng/L (age > 75 years). Patients with an elevated troponin I and/or NT-proBNP levels underwent 2-dimensional echocardiography. LV ejection fraction < 50% was considered abnormal. The ESC diagnostic criteria for clinically suspected myocarditis (2013) were used for the diagnosis of dengue myocarditis (Table 1) [13]. It uses clinical features along with (1) characteristic changes on ECG, (2) myocardiocytolysis markers, (3) functional and structural abnormalities on cardiac imaging [echo/angio/cardiovascular magnetic resonance (CMR)] and (4) tissue characterization by CMR. The diagnosis of myocarditis requires clinical features and ≥ 1 diagnostic criterion from different categories; in asymptomatic patients ≥ 2 diagnostic criteria needs to be fulfilled. All patients were followed up till their discharge/death.
Statistical analysis: Data was entered into an excel sheet (MS Excel 2010) and frequencies and mean were calculated. Statistical analysis was done using Stata 13. The qualitative variables were compared with Chi-square test or Fisher's exact test. Quantitative variables with a normal distribution were compared using Student's t test for two-group analysis. A p value of less than 0.05 was considered as significant.
Results
A total of 206 admitted patients were screened for eligibility and 182 patients with confirmed dengue satisfying the inclusion and exclusion criteria were recruited for this study (Fig. 1). The mean age of patients was 30 ± 12.6 years and 31% were females. Dengue with warning signs was present in 85 (47%) and severe dengue in 60 (33%) patients. The clinical and laboratory features at presentation are shown in Table 1.
Out of a total of 182 patients with dengue, 44 (24%) patients demonstrated some ECG abnormalities. Sinus tachycardia was observed in 30 (16.5%) patients. Sinus bradycardia was observed in 10 (5.5%) and non-specific ST segment changes were seen in 5 (2.7%) patients.
Cardiac enzymes were elevated in 27 (14.8%) patients (cTnI in 25 and NT-proBNP in 22). Among these 27 patients who underwent echocardiography, 11 (40.7%) patients had echocardiographic evidence of myocarditis. Two additional patients were classified as having myocarditis based on characteristic ECG findings and raised enzymes as per ESC 2013 criteria. Isolated enzyme elevation was seen in 14 patients. According to ESC 2013 criteria, dengue fever with myocarditis was diagnosed in 13 [7.1% (3.4–10.9, 95% CI)] patients (Fig. 1).
The patients with myocarditis were more likely to have shortness of breath, bleeding manifestations and higher respiratory rate at baseline (Table 1).
Clinical features of fluid overload were more common in myocarditis group [9 (69%) vs. 3 (1.8%), p ≤ 0.01]. Hospital stay was prolonged (7 ± 4.3 days) in patients with myocarditis compared to those patients without evidence of myocarditis (4.8 ± 1.9 days, p ≤ 0.001). There was a total of 5 (2.7%) deaths in the study population. All the patients who died, had severe dengue with myocarditis.
Discussion
In the present study, 7.1% (3.4–10.9, 95% CI) of admitted patients with dengue fever had evidence of myocarditis according to the ESC 2013 criteria. Overall, 24% patients had abnormalities on electrocardiography; all patients with myocarditis had characteristic ECG abnormalities. These patients were more likely to have clinical evidence of fluid overload and longer hospital-stay.
Few studies have evaluated the prevalence of myocarditis in patients with dengue. In a large study from China, Li and colleagues found evidence of myocarditis in 11.3% of hospitalized dengue patients. They also found that patients with concomitant myocarditis had more severe forms of the disease [9]. Miranda and colleagues found evidence of myocarditis in 2.47% of hospitalized dengue patients [10]. Khongphatthanayothin et al. determined prevalence of myocardial depression and its effect on clinical severity in patients with DHF/DSS. They observed ejection fraction < 50% in 13.8% and 36% of patients with DHF and DSS, respectively. DSS patients with poor ventricular function had significantly more tachycardia and hepatomegaly. Patients with lower ejection fraction developed larger pleural effusion and required more aggressive intravenous fluid resuscitation [14].
Literature from India on myocarditis in dengue is scarce with a wide variation in prevalence of myocarditis has been reported. Sheetal et al. in a study of 100 patients of dengue fever from South India, did not find any evidence of myocarditis [12]. On the other hand, Arora and colleagues reported a 37.5% prevalence of myocarditis with a positive correlation with the severity of dengue fever in their patients [11]. Lakshman et al. studied the prevalence of cardiac involvement among fifty admitted dengue patients and reported evidence of myocardial involvement in 16% and 30% patients based on 2D-echo and biomarker testing, respectively [15].
A few studies have evaluated left ventricular function in patients with Dengue. Datta et al. in their study on 120 dengue patients reported left ventricular systolic dysfunction (ejection fraction 35–45%) through echocardiography in 3.3% of the patients [16]. Wali and colleagues evaluated ventricular function by echocardiography and radionuclide ventriculography in patients with Dengue Haemorrhagic Fever/ Dengue Shock Syndrome. They found evidence of global hypokinesia in nearly 71% of their patients. The mean LV ejection fraction as assessed by radionuclide ventriculography and echocardiography was 41% and 47%, respectively [17]. The wide variation of prevalence of myocarditis reported is due to different diagnostic criteria being used across studies. In the present study, we have used standard criteria as given by European Society of Cardiology.
A wide range of electrocardiographic abnormalities have been identified in patients with dengue fever. These include abnormalities of rate, varying degrees of sinoatrial and atrioventricular conduction disturbances, supraventricular and ventricular tachyarrhythmias. Halstead et al. reported myocarditis, bradycardia and other arrhythmias as complications of dengue infection in the endemic and travellers’ population [18]. In a study conducted by Kularatne et al. in Sri Lanka, electrocardiographic abnormalities (T inversion, ST depression, bundle branch blocks) were identified in 62.5% patients [7]. Universal occurrence of electrocardiographic changes in patients with dengue fever complicated by myocarditis as noted by us, has been reported earlier [19]. These findings are important from the aspect that although not diagnostic, the presence of electrocardiographic abnormalities in patients with dengue fever must alert the clinician to keep the possibility of myocarditis in these patients. Since a large number of dengue patients are handled by primary care centres in resource limited countries, a screening electrocardiography seems an attractive prospect to identify those patients who may be at a higher risk for complications and thereby permit the referral of such patients to higher centres.
Miranda et al. reported elevation of cardiac biomarkers in 15% among 81 recruited patients. Among these 12 patients, 4 had abnormalities on echocardiography [10]. In a study conducted by Arora et al. on 120 dengue patients, elevation of cardiac biomarkers was found in 36.7% of patients, of which both CK-MB and Troponin I were elevated in 23.3%, only CK-MB was elevated in 10% and only Troponin I was elevated 3.3% of patients. None of these patients had any abnormality on echocardiography [11]. In our study, cardiac enzymes were elevated in 14.8% patients, of which 40.7% patients had echocardiographic abnormalities and diagnosed as having myocarditis.
There are a number of important limitations of the present study. Our study being an observational study has no comparator group or adjusting for confounding; therefore, it lacks power to discover association. We did not perform contrast-enhanced magnetic resonance imaging or endomyocardial biopsy for diagnosis of myocarditis in our patients. As majority of these patients had warning signs and severe dengue including major bleeding manifestations, any invasive or time-consuming investigations would have adversely affected clinical management, hence these were not performed. The patients with myocarditis were not followed-up as a part of this study to look for any persisting cardiac dysfunction. Furthermore, being a tertiary care referral centre, an over-reporting due to referral bias cannot be ruled out, hence sample size of our study may not be truly representative of the population. Myocarditis in a severely ill patient may be due to multiple factors particularly co-infections in a tropical country, drugs, etc.; however, none of our patients were diagnosed with any co-infections. Finally, consecutive patients could not be screened as many patients were admitted briefly (< 24 h) in emergency wards and children (< 14 years) were excluded.
Conclusion
Myocarditis among admitted dengue patients is not uncommon and may lead to increased morbidity. There is a need to have an algorithm for suspicion and diagnosis of myocarditis among patients with dengue fever.
References
Gibbons RV, Vaughn DW. Clinical review dengue: an escalating problem. BMJ. 2002;324:1563–6.
Agarwal R, Kapoor S, Nagar R, Misra A, Tandon R, Mathur A, et al. A clinical study of the patients with dengue hemorrhagic fever during the epidemic of 1996 at Lucknow, India. Southeast Asian J Trop Med Public Health. 1999;30:735–40.
National guidelines for clinical management of dengue fever (2015). https://www.searo.who.int/india/publications/national_guidelines_clinical_management_dengue1.pdf?ua=1. Accessed 12 Dec 2017.
Satarasinghe RL, Arultnithy K, Amerasena NL, Bulugahapitiya U, Sahayam DV. Asymptomatic myocardial involvement in acute dengue virus infection in a cohort of adult Sri Lankans admitted to a tertiary referral centre. Br J Cardiol. 2007;14:171–3.
Veloso HH, Ferreira JA, Paiva JM, Honorio JF, Bellei NC, Paola AA. Acute atrial fibrillation during dengue hemorrhagic fever. Braz J Infect Dis. 2003;7:418–22.
Promphan W, Sopontammarak S, Pruekprasert P, Kajornwattanakul W, Kongpattanayothin A. Dengue myocarditis. Southeast Asian J Trop Med Public Health. 2004;35:611–3.
Kularatne SAM, Pathirage MMK, Kumarasiri PVR, Gunasena S, Mahindawanse SI. Cardiac complications of a dengue fever outbreak in Sri Lanka, 2005. Trans R Soc Trop Med Hyg. 2007;101:804–8.
Khongphatthallayothin A, Chotivitayatarakorn P, Somchit S, Mitprasart A, Sakolsattayadorn S, Thisyakorn C. Morbitz type I second degree AV block during recovery from dengue hemorrhagic fever. Southeast Asian J Trop Med Public Health. 2000;31:642–5.
Li Y, Hu Z, Huang Y, Li J, Hong W, Qin Z, et al. Characterization of the Myocarditis during the worst outbreak of dengue infection in China. Medicine (Baltimore). 2016;95:e4051.
Miranda CH, Borges MDC, Matsuno AK, Vilar FC, Gali LG, Volpe GJ, et al. Evaluation of cardiac involvement during dengue viral infection. Clin Infect Dis. 2013;57:812–9.
Arora M, Patil RS. Cardiac manifestation in dengue fever. J Assoc Phys India. 2016;64:40–4.
Sheetal S, Jacob E. A study on the cardiac manifestations of dengue. J Assoc Phys India. 2016;64:30–4.
Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, Fu M, Heliö T, Heymans S, Jahns R, Klingel K. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2013;34:2636–48.
Khongphatthanayothin A, Lertsapcharoen P, Supachokchaiwattana P, La-orkhun V, Khumtonvong A, Boonlarptaveechoke C, et al. Myocardial depression in dengue hemorrhagic fever: prevalence and clinical description. Pediatr Crit Care Med. 2007;8:524–9.
Lakshman A, Balasubramanian P, Nampoothiri RV, Vijayvergiya R, Bhalla A, Varma SC. Elevated cardiac biomarkers and echocardiographic left ventricular dysfunction at admission in patients with dengue fever: report from a tertiary care center in Northwest India. Trop Doct. 2018;48:261–5.
Datta G, Mitra P. A study on cardiac manifestations of dengue fever. J Assoc Phys India. 2019;67:14–6.
Wali JP, Biswas A, Chandra S, Malhotra A, Aggarwal P, Handa R, et al. Cardiac involvement in dengue haemorrhagic fever. Int J Cardiol. 1998;64:31–6.
Halstead S, Wilder-Smith A. Severe dengue in travellers: pathogenesis, risk and clinical management. J Travel Med. 2019;26:taz062.
Salgado DM, Eltit JM, Mansfield K, Panqueba C, Castro D, Vega MR, et al. Heart and skeletal muscle are targets of dengue virus infection. Pediatr Infect Dis J. 2010;29:238–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Bhatt, M., Soneja, M., Farooqui, F.A. et al. Myocarditis in admitted patients with dengue fever. Infection 48, 899–903 (2020). https://doi.org/10.1007/s15010-020-01500-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-020-01500-w