Abstract
Purpose
We studied the incidence, morbidity and mortality of all patients presenting in our teaching hospital with proven influenza virus and/or respiratory syncytial virus (RSV) infection during the influenza epidemic season 2018 which was characterized by a predominant incidence of influenza virus B type B of the Yamagata line.
Methods
In the fall of 2017, specific precaution measures in addition to standard measures were implemented, including standardized testing for influenza virus A,B and RSV by multiplex PCR of pharyngeal swabsData from all consecutive patients were analyzed retrospectively.
Results
Overall 651 patients were examined for the presence of influenza virus and RSV; 214 patients had influenza virus A (n = 36), B (n = 152), and/or RSV (n = 30), including four patients with dual infection. 86% of cases had influenza virus (80% B), and 14% RSV infection. N = 23 cases were treated as outpatients. The rate of acute viral respiratory infections (influenza virus and RSV) was 191 of 2776 (6.9%) admissions to medical wards. Of n = 191 hospitalized cases, n = 44 cases (20.6%) had nosocomial infection. Viral infections were associated with a high morbidity (pneumonia 28.5%, mortality 4.7%). Independent predictors of prolonged hospitalization were the presence of pneumonia, NIV and renal complications, and independent predictors of pneumonia were age ≥ 65 years, bedridden status and CRP ≥ 2.9 mg/dL.
Conclusions
The rate of nosocomial cases was high despite established precaution measures. RSV was associated with morbidity and mortality comparable to influenza. Pneumonia remains the main complication of acute viral respiratory infections, and antimicrobial treatment should include both antiviral as well as antibacterial agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Data provided by the influenza surveillance of the Robert Koch-Institute (RKI) by the end of 2017 indicated the begin of an epidemic with influenza almost exclusively through influenza virus B type B of the Yamagata line [1]. Since the until January 2018 recommended trivalent vaccination did not include this line but the Victoria line instead, and in view of the low vaccination rates in Germany, a high number of influenza patients was expected to occur, both ambulatory and hospitalized. Therefore, in our hospital defined additional specific precaution measures were established including regular testing for influenza virus A and B as well as RSV by pharyngeal swabs and PCR.
RSV infections in adults represent a considerable diagnostic and therapeutic challenge [3,4,5,6]. Clinical characteristics are not distinctive to other viral infections [3, 7,8,9]. Excess hospitalisation and mortality rates comparable to nonpandemic influenza virus [5, 10,11,12,13] or even higher [14] have been reported. The incidence, morbidity and mortality of RSV as compared to influenza viruses varies from season to season [14, 15].
In fact, Germany suffered a strong epidemic season throughout all regions through January–April of 2018, including n = 608 outbreaks and n = 1287 deaths reported to the RKI up to week 16 of 2018 [2]. Accordingly, our hospital experienced an unusually high number of patients presenting with symptoms of acute respiratory infection, and it faced a strong challenge to limit nosocomial transmissions.
This well-defined epidemic offered a unique opportunity to study the following issues: (1) relation of influenza virus and RSV infections; (2) rate of nosocomial cases; (3) morbidity of viral respiratory infection, as reflected by rate of pneumonia, rate of need for ventilatory support, rate of complications, length of hospitalization; (4) mortality of viral respiratory infection; (5) predictors of death; (6) predictors of prolonged hospitalization; (7) analysis of pneumonia cases.
Methods
Epidemiologic background
Data on an ongoing influenza season are provided online weekly by the “Arbeitsgemeinschaft Influenza (AGI) am Robert Koch-Insitut (RKI)” (https://influenza.rki.de). These data are specified for each region in Germany. They are based on a nationwide network collecting data of viral respiratory tract infections from about 600 sentinel offices of pediatrics, general practitioners and specialists for internal medicine. The current activity of influenza is expressed in an index of activity called “Praxisindex”; the activity is reported as normal, mildly, moderately, strongly or very strongly elevated. In addition, data on viral isolations are collected to inform about the most prevalent circulating virus types.
The season 2017/2018 yielded a very strongly elevated influenza activity throughout Germany in particular during the sixth and tenth week of 2018. The virus types corresponded to influenza virus A (29%; 26% H1N1 and 3% H3N2) and influenza virus B (71%; 99% Yamagata line, 1% Victoria line) [1].
Setting and patients
All consecutive patients diagnosed with a respiratory tract infection through influenza virus A, influenza virus B and/or RSV during the influenza season (January–April 2018) at the “Augusta-Kranken-Anstalt Bochum” were retrospectively recorded.
The “Augusta-Kranken-Anstalt Bochum” is a 500-bed teaching hospital located in Bochum, North-Rhine Westfalia, Germany (http://augusta-bochum.de). It provides several specialities of internal medicine including a department of respiratory and infectious diseases, an emergency, an intermediate care and an intensive care unit.
In October 2017, specific precaution measures in addition to standard measures were implemented in the hospital with following key points: (1) definition of patients who receive testing for influenza virus A, B and RSV, i.e. all patients with symptoms and signs of respiratory infection; (2) testing by multiplex PCR of pharyngeal swabs; (3) isolation of (a) patients with clinical presentation typical for influenza and (b) with proven influenza infection for 5 days (if treated with oseltamivir), 7 days (if not treated) from the onset of symptoms; and at least 10 days in patients with severe immunosuppression; (4) offer of influenza vaccination free of charge for all staff members; (5) immediate notification of sickness and suspending from work of symptomatic staff members. In case of close contacts of patients with unexpected viral infections with asymptomatic patients or members of the staff, the latter received prophylactic oseltamivir 1 × 75 mg orally per day until results of PCR testing of patients were available.
Moreover, an anti-influenza treatment police was defined. Patients should receive immediate antiviral treatment with oseltamivir (2 × 75 mg orally) in case of (1) clinical presentation typical for influenza until result of PCR testing, (2) proven influenza infection and (3) severe acute respiratory infection and/or pneumonia until result of PCR testing, all in case of an onset of symptoms of less than 3 days in immunocompetent and 7 days in immunosuppressed cases. Regular treatment duration was defined as 5 days, but could be extended in severely ill patients. No specific treatment was defined for RSV infection. Antibacterial treatment was left to the discretion of the attending physicians.
Diagnosis
An etiological diagnosis of respiratory tract infection with influenza virus A, B, and/or RSV was made by a multiplex PCR of a pharyngeal swabThe RIDAGENE Flu and RSV R-Biopharm, Darmstadt, Germany, tests were used. According to manufacturer´s informations, the analytic sensitivity was 50 copies/mL; the sensitivity and specificity were 96 and 100% for influenza virus A, 91 and 100% for influenza virus B, and 100% each for RSV. Results were available within 24 h.
In patients with productive cough, a sputum sample was obtained. A sputum sample was judged as valid in the presence of neutrophils. In patients with pneumonia, diagnostic work-up included blood cultures and urinary antigen testing for S. pneumoniae and Legionella pneumophila.
Data collection
The following variables from patients with proven viral infection were recorded: age, sex, community- or nosocomially acquired, type of viral infection (influenza virus A, B and/or RSV), treatment setting (ambulatory or hospital) comorbidities (classified as cardiac, pulmonary, renal, hepatic, peripheral artery disease, CNS, psychiatric, neoplastic and diabetes mellitus), functional status (bedridden or not), severe immunosuppression (neutropenia, T- or B-cell deficiency, steroids and others), symptoms at diagnosis (fever, cough, expectoration, dyspnea, others), physical examination (respiratory rate, blood pressure, heart rate, confusion, others), laboratory parameters (hemoglobin, leucocyte and platelet count, GFR, creatinine, CRP, blood glucose), blood gas analyses (pH, pO2, pCO2, oxygen saturation), presence of infiltrates on chest radiograph, microbiological investigation (sputum cultures, blood cultures, urine antigen testing for pneumococci and Legionella), type of antimicrobial treatment, complications (cardiac, pulmonary, renal, CNS), ventilatory support [noninvasive ventilation (NIV) and/or invasive mechanical ventilation (MV)], outcomes (length of hospitalization, Definitions.
Nosocomial acquisition of viral infection was assumed in patients with symptoms suggestive of acute respiratory tract infection at more than 48 h after hospitalisation. Pneumonia was diagnosed in case of the symptoms and signs of lower respiratory tract infection together with the presence of infiltrates on chest radiograph. Complications were defined as acute events associated with viral infection: (a) cardiac: heart failure, arrhythmia or myocardial infarction; (b) pulmonary: acute or acute on chronic respiratory failure (hypoxemia defined as pO2 ≤ 55 mmHg and/or hypercapnia ≥ 50 mmHg on room air); (c) renal: serum-creatinine and GFR above the reference values in patients without known renal disease or acute on chronic deterioration (any increase of serum-creatinine and GFR) in patients with known renal disease; (d) neurological: disorientation or vascular events. Prolonged hospitalization was defined as a length of hospitalization longer than the median value of all hospitalized patients. Death was defined as in-hospital death.
Statistics
Continuous variables were compared by Student’s t-test, categorical variables with the chi-square test (or the Fisher’s exact-test in case of small expected values). Multivariate analysis of categorical variables was performed using a stepwise forward logistic regression model. Significant variables in univariate analysis were included in the multivariate model.
Statistics were applied using SPSS Version 25. Level of significance was set at p < 0.05.
Results
Epidemiology
During January–April 2018, n = 651 cases were examined by PCR for influenza virus and RSV. Overall 214 patients had a PCR swab positive for influenza virus A (n = 36), B (n = 152), and/or RSV (n = 30), including four patients with dual infection (n = 1) influenza virus B/RSV infection; n = 2 influenza virus A and B; n = 1 influenza virus A/RSV infection. Of the influenza cases, 80% had influenza virus B and 20% influenza virus A. Thus, 86% of cases had influenza virus, and 14% RSV infection.
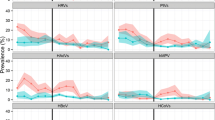
The distribution of influenza virus and RSV infection by weeks is given in Fig. 1a, b. Week 9 had the highest number of cases for both patients with influenza virus and RSV (n = 39, 18.2% of cases). The distribution of cases with influenza corresponded to the incidence in North-rhine Westfalia provided by the RKI surveillance (https://influenza.rki.de/Diagrams.aspx?agiRegion=7).
Overall n = 23 cases were treated as outpatients; of the n = 191 hospitalized cases, n = 44 cases (20.6%) had onset of symptoms and a diagnosis established more than 48 h after admission and were classified as nosocomial. Of influenza virus A, n = 8 (22.2%) were nosocomial, of influenza virus B n = 33 (21.7%), and of RSV n = 3 (10%).
The n = 44 cases included one outbreak of five cases.
The rate of acute viral respiratory infections (influenza virus and RSV) was 191 of 2776 (6.9%) admissions to medical wards during the period.
Patient characteristics
Mean age was 69.9 ± 15.4 years (range 19–98), n = 115 were male (54%) and n = 99 (46%) female. Of the whole population, n = 23 were treated as outpatients (11%).
The patients presented with fever as defined by temperature ≥ 38 grades Celsius (n = 88/175, 50%), cough (n = 181/203, 89%), expectoration (n = 71/202, 35%), and dyspnea (n = 112/204, 55%); an additional n = 43/201 (21%) had gastrointestinal symptoms, mainly diarrhea. Two patients had exclusively gastrointestinal symptoms.
The most common comorbidity was cardiac (48%), followed by renal disease (31%), pulmonary disease (27%; COPD: 20%) and diabetes mellitus (22%). Overall, n = 177 patients (77.9%) had at least one comorbidity. Other comorbidities are listed in Table 1. Immunosuppression was present in n = 26 (12.1%) of patients.
Mean respiratory rate was 21,6 / min (13–52), blood pressure was 135 (range 54–210) systolic and 78 (34–115) diastolic mmHg, heart rate 93 bpm (48–145), temperature 37.9 (range 35.8–40.1) grades Celsius. N = 30 (14%) patients were bedridden; n = 27 (12.6%) patients had new onset of confusion.
Laboratory results and blood gas analyses at admission are summarized in Table 2. Leukopenia < 2000/µL was present in n = 3 (1.4%), thrombopenia < 150,000/µL in n = 57 patients (26.6%). Overall, n = 28(13.1%) patients had severe hypoxia with pO2 ≤ 55 mmHg, and n = 8 patients (3.7%) had hypercapnia with pCO2 ≥ 50 mmHg.
Microbial investigation
Patients had productive sputum and were able to provide a sputum sample in n = 36 cases (16.8%). Overall n = 16 pathogens in valid sputum samples could be isolated in 15 cases, including Staphylococcus aureus (n = 5; MSSA n = 4 and MRSA n = 1), Haemophilus influenzae (n = 3), Moraxella catarrhalis (n = 1), enterobacteriaceae (n = 5; Klebsiella oxytoca n = 2, E. coli n = 3), Pseudomonas aeruginosa (n = 2).
A positive pneumococcal antigen test was found in n = 4 patients. Legionella antigen tests were negative throughout.
Blood cultures yielded a pathogen in n = 7 patients, including Staphylococcus aureus (n = 3) and Klebsiella pneumoniae (n = 1); three further isolates were not related to respiratory infection (Escherichia coli (n = 2), Staphylococcus epidermidis (n = 1)).
Complications
Pneumonia, as evidenced by infiltrates in chest radiographs was present in n = 61 cases (28.5%).
Fifty nine patients (31%) experienced acute or acute on chronic respiratory failure during hospitalization. Further complications included cardiac (n = 55, 25.7%), renal (n = 55, 25.7%), and neurological complications (n = 20, 9.3%).
N = 27 (12.6%) of patients were admitted at the IMC/ICU. Seven patients (3.3%) had to be transferred to the IMC/ICU during hospitalization.
Acute and/or acute on chronic respiratory hypercapnic failure required noninvasive ventilation in 25 cases (11.7%) and invasive mechanical ventilation in 8 cases (3.7%).
Antimicrobial treatment
A total of n = 45 (21%) patients had already received antibacterial agents as outpatients.
The majority of patients received antiviral treatment with oseltamivir (n = 145, 67.8%). Antibacterial treatment was administered in nearly half of the patients (n = 106, 49.5%), including the following agents: penicillins (n = 77, 36%), cephalosporins (n = 11, 5.1%), macrolides (n = 25, 11,7%), quinolones (n = 15, 7%) and carbapenems (n = 8, 3.7%).
Outcomes
The median hospitalization time was 9 days (range 1–68) (Fig. 2). Overall, ten patients (4.7%) died.
Predictors of death
In univariate analysis, male sex, confusion, pneumonia, bedridden status, NIV, MV and renal complications were associated with in-hospital lethal outcome (Table 3).
No association was found for nosocomial infection, type of respiratory viral infection (influenza virus A, B, RSV), age (69.8 ± 15.5 versus 71.5 ± 13.9 years, p = 0.74), comorbidities, immunosuppression, bacteremia, laboratory parameters and other than renal complications.
Also, treatment with oseltamivir was not found to be protective (OR 0.43 95% CI 0.1–1.5, p = 0.29). However, only half of the patients who died had received oseltamivir.
Pneumonia and MV were the strongest predictors of death (Table 3).
Predictors of hospitalization time
Nosocomial diagnosis, pneumonia, bedridden status, sputum production, dyspnea, peripheral artery disease, NIV, cardiac, renal and CNS-complications all predicted prolonged hospitalization time (above the median of 9 days) (Table 4). However, type of respiratory viral infection, age, sex, comorbidities, immunosuppression, bacteremia, laboratory parameters, and MV were not predictive.
Again, oseltamivir was not protective (OR 1.1, 95% CI 0.6–2.1, p = 0.81; 67 of 89 patients with prolonged hospitalization had received oseltamivir).
Pneumonia, NIV and renal complications were independent predictors of prolonged hospitalisation in multivariate analysis (Table 4).
Analysis of pneumonia cases
The distribution of type of viral infection in n = 61 patients with pneumonia was as follows: influenza virus A n = 16/33, 44.4%; influenza virus B n = 34/152, 22.4%, and RSV infection n = 15/30, 50%.
A bacterial co-infection could be defined in n = 12 cases (19.6%): Streptococcus pneumoniae (n = 3), Staphylococcus aureus (MSSA) (n = 4), MRSA (n = 1), Klebsiella pneumoniae (n = 1), Klebsiella oxytoca (n = 1), Pseudomonas aeruginosa (n = 2).
All patients with pneumonia were hospitalized; 16/61 cases (26.2%) were nosocomial. Three patients were admitted at IMC/ICU, and 4 further patients were transferred to it during follow up. Ventilatory support was administered in 20 cases (14 NIV, 6 MV). Pneumonia accounted for 56% of NIV and 75% of MV. Renal complications were present in 37.7% of patients with pneumonia.
Only 41/61 (67%) patients had received oseltamivir, and 5/9 (55.6%) patients with pneumonia who died had not received the drug. Conversely, six patients (9.8%) with pneumonia had not received antibacterial treatment.
Nine patients (14.8%) with pneumonia died, accounting for 90% of deaths overall.
Death rates according to type of virus infection were influenza virus A 2/16 (12.5%); influenza virus B 6/34 (17.4%); RSV 2/15 (13.3%); and mixed infection 1/4 (25%).
The following factors were found to be independently associated with pneumonia in multivariate anaylsis: age ≥ 65 years, bedridden status, CRP ≥ 2.9 mg/dL (Table 5). Sex, at least one comorbidity and nosocomial infection were not predictive.
Discussion
The main findings of the study are the following: (1) the rate of nosocomial cases was high (20.6%); (2) RSV infection was frequent (14% of viral infections); (3) viral infections were associated with a high morbidity, including a high rate of pneumonia (28.5%) and a considerable mortality (4.7%); (4) independent predictors of prolonged hospitalization were the presence of pneumonia, NIV and renal complications; independent predictors of pneumonia were age ≥ 65 years, bedridden status and CRP ≥ 2.9 mg/dL.
The rate of infections meeting the definition of nosocomial cases was high. However, the threshold of 48 h might not be entirely feasible for influenza virus and perhaps even less RSV which may have incubation times of up to 5 days. When the threshold for nosocomial cases was put at more than 5 days, the rate of nosocomial infections still reached 16% (31/193 cases). This rate was lower as compared to a recent German study reporting 30% nosocomial cases using a threshold of more than 4 days [16] but still resulted despite the elaborate definition and implementation of precaution measures. Although transmission may predominantly result from patient-to-patient, it could also reflect patients and visitors entering the hospital during the incubation period or asymptomatic or clinically atypical infection. Attempts to increase the compliance with precaution measures although indispensable may therefore not be sufficient to reduce nosocomial transmissions. Thus, it appears that in periods of influenza epidemics with exceptional infection rates, it may be considered to test all patients admitted to medical wards by PCR of pharyngeal swabs.
Another gap may be the notoriously low influenza vaccination rate of the staff and the failure to move back home in the presence of first symptoms of acute respiratory infection. Only continuous education and motivation will be able to improve compliance rates with vaccination and to establish personal discipline.
In our study, RSV was detected continuously during the influenza season in parallel to influenza virus infection in an approximate 1:7 relation. Half of the patients with RSV infection had pneumonia, comparable to influenza virus A but double as high compared to influenza virus B; likewise, death rates of pneumonia patients with RSV infection were comparable to influenza virus A and B but highest in mixed infections. Thus, our data confirm a high incidence in terms of morbidity and mortality of RSV infection in adults, and underline RSV as an underestimated etiology of respiratory tract infection in adults, including those not severely immunosuppressed [3, 5,6,7]. Treatment options are limited, and studies are needed to evaluate treatment regimen for adult patients with RSV infection.
Rates of nosocomial cases of RSV were half compared to influenza virus but still reached 10%. Nosocomial transmissions and outbreaks have been repeatedly described in hemato-oncologic units [17, 18]. However, they are not confined to immunosuppressed patients, and molecular testing in symptomatic patients should include both influenza virus and RSV.
The morbidity of patients hospitalized with acute viral infections was high. In particular, the rate of cases with pneumonia (28.5%) was impressive. In line with many reports of influenza epidemics, pneumonia was a potentially life-threatening complication [19]. An additional bacterial pathogen could be identified in 19% of cases and identified Streptococcus pneumoniae and Staphylococcus aureus whereas Haemophilus influenzae was only found in patients without pneumonia. These patterns correspond to the first comprehensive description of pulmonary complications of influenza virus infection, in particular to patients with “combined influenza virus and pneumonia” [20]. A recent meta-analysis found coinfection to be present in a range from 2 to 65%. Coinfection has been reported to occur in up to 16.6% of critically ill patients with influenza virus; in addition, the rate seemed to have increased to up to 23.4% over years [21, 22]. Influenza viruses enhance susceptibility to co-infection with common strains of bacteria, and bacterial coinfection seems to impact immunity to the virus as well [23].
In fact, pneumonia accounted for most deaths (90%) among patients with viral infections. The risk of pneumonia was independently associated with age ≥ 65 years, bedridden status, and CRP ≥ 2.9 mg/dL. Pneumonia was a predictor of death and also of prolonged hospitalization.
Since most patients were treated at the intermediate or intensive care unit, treatment limitation does not appear to account for the mortality rate. Treatment may result inadequate by failing to treat influenza virus infection as well as by failing to recognize bacterial superinfection. In fact, only two-thirds of patients with pneumonia had received oseltamivir, and only 55% of those dying with pneumonia, on the other hand, nearly 10% had not received antibacterial treatment. In future reviews and guidelines, it should be stressed that there is some evidence from the 2009 H1N1 epidemic for severe lower mortality of influenza virus infection treated with oseltamivir [24, 25], and that a positive PCR for viral pathogens does not imply to do without antibacterial treatment. Obviously, antibacterial regimen should be cautiously selected covering pneumococci and Staphylococcus aureus as well as enterobacteria and Pseudomonas aeruginosa when appropriate.
A major complication of acute viral respiratory infection is acute and acute on chronic respiratory failure. Whereas pneumonia accounted for 75% of cases with MV administered, 45% of those who received NIV did not have pneumonia. Accordingly, MV was a predictor of mortality, and NIV of prolonged hospitalization. Renal complications appeared to have additional impact on length of hospitalization as a surrogate for morbidity.
Limitations of this study include its retrospective design with its inherent potential of bias. Our database did not allow to differentiate transmission and delayed diagnosis in nosocomial cases, and we were neither able to analyze the exact success of the implementation of the precaution measures. In addition, we ignore the exact vaccination rate of the staff, as well as suspension policies in view of healthcare personnel with symptomatic acute respiratory illness. On the other hand, we provide a comprehensive analysis of patients with acute viral (influenza virus and RSV) respiratory infections during a well-defined influenza epidemic predominantly caused by influenza virus B on the background of a previous intervention aimed at the establishment of additional specific preventive measures.
Our study provides support for the need of a comprehensive preventive policy during the influenza season. In view of the high rate of nosocomial cases, regular testing for influenza virus and RSV by PCR in all patients admitted to medical wards may be considered during influenza epidemics. Pneumonia remains the main complication of acute viral respiratory infections, and antimicrobial treatment should include both antiviral as well as antibacterial agents. Acute respiratory failure (with and without pneumonia) is frequent and contributes to prolonged hospitalization .
Abbreviations
- NIV:
-
Noninvasive mechanical ventilation
- MV:
-
(Invasive) mechanical ventilation
References
https://influenza.rki.de/CirculatingViruses.aspx. Accessed 1 Sept 2018.
https://influenza.rki.de/Wochenberichte/2017_2018/2018-14.pdf. Accessed 1 Sept 2018.
Branche AR, Falsey AR. Respiratory syncytial virus infection in older adults: an under-recognized problem. Drugs Aging. 2015;32:261–9.
Binder W, Thorsen J, Borczuk P. RSV in adult ED patients: do emergency providers consider RSV as an admission diagnosis? Am J Emerg Med. 2017;35:1162–5.
Lee N, Lui GC, Wong KT, Li TC, Tse EC, Chan JY, Yu J, Wong SS, Choi KW, Wong RY, Ngai KL, Hui DS, Chan PK. High morbidity and mortality in adults hospitalized for respiratory syncytial virus infections. Clin Infect Dis. 2013;57:1069–77.
Falsey AR, McElhaney JE, Beran J, van Essen GA, Duval X, Esen M, Galtier F, Gervais P, Hwang SJ, Kremsner P, Launay O, Leroux-Roels G, McNeil SA, Nowakowski A, Richardus JH, Ruiz-Palacios G, St Rose S, Devaster JM, Oostvogels L, Durviaux S, Taylor S. Respiratory syncytial virus and other respiratory viral infections in older adults with moderate to severe influenza-like illness. J Infect Dis. 2014;209:1873–81.
Loubet P, Lenzi N, Valette M, Foulongne V, Krivine A, Houhou N, Lagathu G, Rogez S, Alain S, Duval X, Galtier F, Postil D, Tattevin P, Vanhems P, Carrat F, Lina B, Launay O, FLUVAC Study Group. Clinical characteristics and outcome of respiratory syncytial virus infection among adults hospitalized with influenza-like illness in France. Clin Microbiol Infect. 2017;23:253–9.
Saxena S, Singh D, Zia A, Umrao J, Srivastava N, Pandey A, Singh S, Bhattacharya P, Kumari R, Kushwaha R, Dhole TN. Clinical characterization of influenza A and human respiratory syncytial virus among patients with influenza like illness. J Med Virol. 2017;89:49–54.
Volling C, Hassan K, Mazzulli T, Green K, Al-Den A, Hunter P, Mangat R, Ng J, McGeer A. Respiratory syncytial virus infection-associated hospitalization in adults: a retrospective cohort study. BMC Infect Dis. 2014;14:665.
Jansen AG, Sanders EA, Hoes AW, van Loon AM, Hak E. Influenza- and respiratory syncytial virus-associated mortality and hospitalisations. Eur Respir J. 2007;30:1158–66.
Matias G, Taylor R, Haguinet F, Schuck-Paim C, Lustig R, Shinde V. Estimates of mortality attributable to influenza and RSV in the United States during 1997–2009 by influenza type or subtype, age, cause of death, and risk status. Influenza Other Respir Viruses. 2014;8:507–15.
Matias G, Taylor R, Haguinet F, Schuck-Paim C, Lustig R, Shinde V. Estimates of hospitalization attributable to influenza and RSV in the US during 1997–2009, by age and risk status. BMC Public Health. 2017;17:271.
Malosh RE, Martin ET, Callear AP, Petrie JG, Lauring AS, Lamerato L, Fry AM, Ferdinands J, Flannery B, Monto AS. Respiratory syncytial virus hospitalization in middle-aged and older adults. J Clin Virol. 2017;96:37–43.
Kwon YS, Park SH, Kim MA, Kim HJ, Park JS, Lee MY, Lee CW, Dauti S, Choi WI. Risk of mortality associated with respiratory syncytial virus and influenza infection in adults. BMC Infect Dis. 2017;17:785.
Fleming DM, Cross KW. Respiratory syncytial virus or influenza? Lancet. 1993;342:1507–1510.
Hagel S, Ludewig K, Moeser A, Baier M, Löffler B, Schleenvoigt B, Forstner C, Pletz MW. Characteristics and management of patients with influenza in a German hospital during the 2014/2015 influenza season. Infection. 2016;44:667–72.
Jensen TO, Stelzer-Braid S, Willenborg C, Cheung C, Andresen D, Rawlinson W, Clezy K. Outbreak of respiratory syncytial virus (RSV) infection in immunocompromised adults on a hematology ward. J Med Virol. 2016;88:1827–31.
Nabeya D, Kinjo T, Parrott GL, Uehara A, Motooka D, Nakamura S, Nahar S, Nakachi S, Nakamatsu M, Maeshiro S, Haranaga S, Tateyama M, Tomoyose T, Masuzaki H, Horii T, Fujita J. The clinical and phylogenetic investigation for a nosocomial outbreak of respiratory syncytial virus infection in an adult hemato-oncology unit. J Med Virol. 2017;89:1364–1137.
Martin-Loeches I, van Someren Gréve F, Schultz MJ. Bacterial pneumonia as an influenza complication. Curr Opin Infect Dis. 2017;30:201–20.
Louria DB, Blumenfeld HL, Ellis JT, et al. Studies on influenza in the pandemic of 1957–1958. II. Pulmonary complications of influenza. J Clin Invest. 1959;38:213–65.
Klein EY, Monteforte B, Gupta A, Jiang W, May L, Hsieh YH, Dugas A. The frequency of influenza and bacterial coinfection: a systematic review and meta-analysis. Influenza Other Respir Viruses. 2016;10:394–403.
Martin-Loeches I, Schultz J, Vincent M, Alvarez-Lerma J-L, Bos F, Solé-Violán LD, Torres J, Rodriguez A. Increased incidence of co-infection in critically ill patients with influenza. Intensive Care Med. 2017;43:48–58.
Cauley LS, Vella AT. Why is co-infection with influenza virus and bacteria so difficult to control? Discov Med. 2015;19:33–40.
Louie JK, Yang S, Acosta M, Yen C, Samuel MC, Schechter R, Guevara H, Uyeki TM. Treatment with neuraminidase inhibitors for critically ill patients with influenza A (H1N1)pdm09. Clin Infect Dis. 2012;55:1198–1204.
Muthuri SG, Venkatesan S, Myles PR, Leonardi-Bee J, Al Khuwaitir TS, Al Mamun A, Anovadiya AP, Azziz-Baumgartner E, Báez C, Bassetti M, Beovic B, Bertisch B, Bonmarin I, Booy R, Borja-Aburto VH, Burgmann H, Cao B, Carratala J, Denholm JT, Dominguez SR, Duarte PA, Dubnov-Raz G, Echavarria M, Fanella S, Gao Z, Gérardin P, Giannella M, Gubbels S, Herberg J, Iglesias AL, Hoger PH, Hu X, Islam QT, Jiménez MF, Kandeel A, Keijzers G, Khalili H, Knight M, Kudo K, Kusznierz G, Kuzman I, Kwan AM, Amine IL, Langenegger E, Lankarani KB, Leo YS, Linko R, Liu P, Madanat F, Mayo-Montero E, McGeer A, Memish Z, Metan G, Mickiene A, Mikić D, Mohn KG, Moradi A, Nymadawa P, Oliva ME, Ozkan M, Parekh D, Paul M, Polack FP, Rath BA, Rodríguez AH, Sarrouf EB, Seale AC, Sertogullarindan B, Siqueira MM, Skręt-Magierło J, Stephan F, Talarek E, Tang JW, To KK, Torres A, Törün SH, Tran D, Uyeki TM, Van Zwol A, Vaudry W, Vidmar T, Yokota RT, Zarogoulidis P, PRIDE Consortium Investigators, Nguyen-Van-Tam JS. Effectiveness of neuraminidase inhibitors in reducing mortality in patients admitted to hospital with influenza A H1N1pdm09 virus infection: a meta-analysis of individual participant data. Lancet Respir Med. 2014;2:395–404.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Topoulos, S., Giesa, C., Gatermann, S. et al. Analysis of acute respiratory infections due to influenza virus A, B and RSV during an influenza epidemic 2018. Infection 47, 425–433 (2019). https://doi.org/10.1007/s15010-018-1262-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-018-1262-x