Abstract
Purpose
Ceftazidime–avibactam is an antimicrobial association active against several Enterobacteriaceae species, including those resistant to carbapenem. Considering the importance of this drug in the current panorama of multidrug-resistant bacteria, we performed a systematic review about ceftazidime–avibactam with emphasis on clinical and pharmacological published data.
Methods
A systematic search of the medical literature was performed. The databases searched included MEDLINE, EMBASE and Web of Science (until September 2017). The search terms used were ‘avibactam’, ‘NXL104’ and ‘AVE1330A’. Bibliographies from those studies were also reviewed. Ceftazidime was not included as a search term, once relevant studies about avibactam in association with other drugs could be excluded. Only articles in English were selected. No statistical analysis or quality validation was included in this review.
Results
A total of 151 manuscripts were included. Ceftazidime–avibactam has limited action against anaerobic bacteria. Avibactam is a potent inhibitor of class A, class C, and some class D enzymes, which includes KPC-2. The best pharmacodynamic profile of ceftazidime–avibactam is ƒT > MIC, validated in an animal model of soft tissue infection. Three clinical trials showed the efficacy of ceftazidime–avibactam in patients with intra-abdominal and urinary infections. Ceftazidime–avibactam has been evaluated versus meropenem/doripenem in hospitalized adults with nosocomial pneumonia, neutropenic patients and pediatric patients.
Conclusion
Ceftazidime–avibactam has a favorable pharmacokinetic profile for severe infections and highly active against carbapenemases of KPC-2 type.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent decades, there has been few options of antibiotics against multidrug-resistant bacteria, especially those producing carbapenemases. Until a few years ago, there was a great concern regarding carbapenem resistance in Pseudomonas aeruginosa and Acinetobacter baumannii. Since 2001, a new carbapenemase class was described, Klebsiella pneumoniae carbapenemase (KPC), found mainly in Klebsiella pneumoniae and other Enterobacteriaceae [1]. This type of antibiotic resistance can spread quickly among different bacterial genera [2]. Klebsiella pneumoniae carbapenemase (KPC) is a beta-lactamase that confers resistance to all beta-lactam antibiotics, including carbapenems [3]. The mortality of infections caused by KPC-producing bacteria is around 50%. Although some of the isolates show sensitivity to carbapenems, the clinical significance of this phenomenon is still under study. Current therapeutic recommendations are the association of anti-infectives, such as tigecycline and polymyxin, a fact that increases hospital costs [4].
The KPC gene is called bla KPC, which is present in a mobile element associated with the easy transmission (transposon). This feature has an epidemiological importance [5]. Another concern about transposons is the fact that transmission can occur between different genera, not only Klebsiella, but also Escherichia coli, Salmonella, Citrobacter and several Gram-negative bacilli [6]. KPC-producing bacteria have been identified in several countries [7,8,9,10]. The presence of bla KPC in Brazil was described in 2005, although the article has been published only in 2009 [11]. Since then, several cases have been reported in different states of Brazil [12,13,14].
The SENTRY Antimicrobial Surveillance Program evaluated 5704 Gram-negative bacilli between January 2008 and December 2010 from Argentina, Brazil, Chile, and Mexico. Meropenem-nonsusceptible Klebsiella spp. rate was highest in Brazil (11.1%), followed by Argentina (8.2%). KPC-producing K. pneumoniae was not detected in 2008, but emerged in 2009 (10 strains) and increased significantly in 2010 (44; p < 0.0001) [15].
In the last years, there was a significant increase in infections caused by KPC-producing bacteria [16, 17]. Few drugs have been developed, some of them with activity against carbapenemase-producing bacteria. The ceftazidime and avibactam combination is one of these options.
Ceftazidime is a third-generation cephalosporin with broad-spectrum activity against Gram-negative bacilli, including Pseudomonas aeruginosa [18, 19]. It was introduced into clinical use in the 1980s, but nowadays, the usefulness of all cephalosporins has become compromised after the appearance of extended-spectrum β-lactamases (ESBLs) [20, 21], Klebsiella pneumoniae carbapenemases (KPCs) [22] and metallo-β-lactamases [23].
One alternative for restoring ceftazidime activity in the presence of β-lactamases is to use β-lactamase inhibitors. Avibactam is a β-lactamase inhibitor that has as substrate the β-lactamase enzymes of Ambler molecular classification A, C and some of class D. Accordingly, in association with a β-lactam, the antibiotic shows activity again. Thus, avibactam can be associated with broad-spectrum cephalosporins such as ceftazidime and ceftaroline [24,25,26].
In phase 2 studies, ceftazidime–avibactam showed efficacy in the treatment of intra-abdominal infections (associated with metronidazole) and complicated urinary tract infections [27, 28].
In view of the growing number of multidrug-resistant bacteria and the lack of treatment options available, in 2015 the FDA (US Food and Drug Administration) approved the use of ceftazidime–avibactam to treat those infections when there is no other option available until phase 3 studies are completed. In the same year the phase 3 study for intra-abdominal infections, showing non-inferiority compared to meropenem, was submitted for publication [29].
Although approved for those infections, the most important feature of this medication is its broad spectrum of activity, including activity against carbapenemase-producing bacteria, such as Enterobacteriaceae and Pseudomonas aeruginosa [30, 31]. After FDA approval and phase 3 study publication, ceftazidime–avibactam will be available in several countries. Considering all these facts, we performed a systematic review about ceftazidime–avibactam with emphasis on clinical and pharmacological published data.
Methods
A systematic search of the medical literature was performed. The databases searched included MEDLINE, EMBASE and Web of Science (until September 2017). The search terms used were ‘avibactam’, ‘NXL104’ and ‘AVE1330A’. Bibliographies from those studies were also reviewed. Ceftazidime was not included as a search term, once relevant studies about avibactam in association with other drugs could be excluded. Only articles in English were selected. No statistical analysis or quality validation was included in this review.
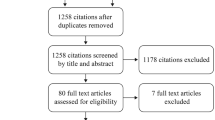
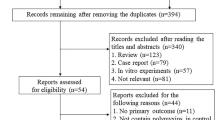
A total of 323 manuscripts were found, of which 172 were excluded: only aztreonam–avibactam was evaluated (16), repeated study (17), not related to avibactam, other drugs (18), ceftaroline–avibactam (15), review (79) and others (27).
Articles will not be described individually, but are included as reference in the text in each “Results” subsection.
Results
Molecule features
Ceftazidime consists of a β-lactam ring (cephem nucleus) as in other cephalosporins [32]. The methylpyridinium group in position 3 provides its anti-pseudomonal activity, the aminothiadiazole ring in position 7 is responsible for the activity against Gram-negative rods, and the carboxypropyl-oxyimino group provides the anti-pseudomonal activity. However, ceftazidime presents reduced activity against Enterobacteriaceae when compared to ceftriaxone, which has the methoxyimino group [19]. The ceftazidime activity may also be lower than other cephalosporins against Gram-positive cocci, so its use has been restricted to infections with P. aeruginosa as possible etiology (Tables 1, 2).
Avibactam is a non-β-lactam β-lactamase inhibitor. Avibactam is a representative of a bridged bicyclic ((2S,5R)-7-oxo-6-(sulfooxy)-1,6-diazabicyclo [3,2,1] octane-2-carboxamide) (DBO) scaffold that was rationally designed by incorporating the existing knowledge about beta-lactams into the properties of a novel scaffold [33] (Fig. 1). Some characteristics resemble the β-lactam ring of cephalosporins, including ceftazidime. The sulfate in position 6 is similar to the carboxyl group in ceftazidime in position 4, and the carboxamide in position 2 is similar to the aminoacyl side chain in ceftazidime in position 7. It is important to remember that all β-lactamase inhibitors have similar structure to β lactam antibiotics, which does not happen with avibactam. Sulbactam, for example, is the active agent for the treatment of infections caused by Acinetobacter spp. [34].
Ceftazidime (2000 mg) is combined with a fixed dosage of avibactam (500 mg) (AVYCAZ®). They do not have interactions that may disrupt activity and kinetic characteristics [35]. There is already an automated sensitivity test validated with the usual bacteria for ceftazidime–avibactam [36]. Disk diffusion with ceftazidime–avibactam 30/20 μg is standardized for susceptibility tests in E. coli, S. aureus, P. aeruginosa, K. pneumoniae as well as MIC in broth dilution with unsupplemented Mueller–Hinton medium [37].
A brief review of β-lactamases
The main mechanism of resistance of Gram-negative bacilli to β-lactam is the production of beta-lactamases. These enzymes hydrolyze the β-lactam ring, with different affinity for each cephalosporin. There are hundreds of β-lactamases and different classifications. One of the most used is the Ambler molecular classification. In this classification, there are 4 β-lactamase groups (A–D). Class A includes, for example, enzymes present in Esnterobacteriaceae, such as TEM and SHV, and β-lactamase inhibitors (clavulanate, tazobactam, sulbactam) that can inactivate those enzymes. On the other hand, enzymes as ESBL and KPC are also part of this group [38].
Class B includes the so-called β-lactamases, and its activity is zinc cofactor-dependent. There are no β-lactamase inhibitors against this type of enzyme.
Beta-lactamases class C are also known as the AmpC group, usually encoded by chromosomal genes. However, the emergence of this type of enzyme genes in plasmids has become increasingly common, causing AmpC no longer being a chromosomal gene but becoming a transferable gene from bacterium to bacterium [39]. These β-lactamases can be inducible by the use of antimicrobials, especially those present in Serratia, P. aeruginosa, indole-positive Proteus, Citrobacter and Enterobacter. In general, β-lactamase inhibitors have no activity against these enzymes.
Finally, we have the β-lactamases D group, also called oxacilinases, presenting broad spectrum of inhibition, including carbapenems. Classic β-lactamase inhibitors (e.g., clavulanate, tazobactam, sulbactam) do not have good activity against this class of enzymes [40].
Mechanism of action
Ceftazidime
Ceftazidime is a cephalosporin that promotes bactericidal effect through cell lysis by inhibiting cell wall synthesis. More specifically, ceftazidime binds to enzymes termed PBP (penicillin-binding protein). These enzymes are responsible for the polymerization of peptidoglycan, the main component of the bacterial cell wall.
There are several PBPs, being characteristic for each bacterial species. In addition, antibiotics may have different affinity for each of those PBPs, which explains the different spectrum of action and potency of beta-lactams [41]. The main resistance mechanism against ceftazidime is the production of β-lactamases, as described earlier. In addition, other less common mechanisms for this group of antibiotics are porins and efflux pumps, as well as changes in permeability, which can be associated with overexpression of carbapenemase [42].
Avibactam
Avibactam is a β-lactamase inhibitor that forms a covalent bond with β-lactamase [43]. This covalent bond occurs through reversible acylation [44, 45]. In case of other β-lactamase inhibitors, the reaction is irreversible and there is production of intermediates, which are hydrolyzed (Fig. 2).
Avibactam is able to covalently bind not only to β-lactamase, but also to some bacterial PBPs [46], notably E. coli and H. influenzae PBP2, to PBPs 2 and 3 of P. aeruginosa and S. aureus, and to PBP3 of S. pneumoniae. This may explain the antibacterial activity against some bacterial strains and species [47].
The analysis of avibactam reaction with CMY-2 (a plasmid-encoded Ambler class C cephalosporinase) revealed that the CMY-2–avibactam acyl-enzyme complex was stable for as long as 24 h. A hypothesis is that successive hydrogen-bonding interactions can occur between avibactam and CMY-2 [48].
Avibactam exhibits activity against Ambler class A β-lactamases (ESBLs and KPCs), class C β-lactamases, and some class D β-lactamases. Other β-lactamase inhibitors do not exhibit activity against class B β-lactamases. More than 650 class A enzymes were evaluated to determine the potential subtypes that could impact in avibactam inhibition [49]. Only the differences in the Ω-loop of type PER enzymes were found to impact the ability of avibactam. Nevertheless, a similar study evaluated several types of class B (serine and metallo-β-lactamases) against whom avibactam showed limited activity [50].
The advantage of avibactam is its long half-life, complex reversibility through deacylation, small molecular size, low molecular weight, polarity and interaction with important catalytic residues near the active sites of β-lactamases. Another advantage of avibactam over other β-lactamase inhibitors is related to the low potential for inducing resistance [51]. As the former β-lactamase inhibitors have structures similar to β-lactams, they can induce β-lactamase expression of chromosomal genes, such as the AmpC gene. A study compared avibactam to clavulanate, and it was shown that avibactam has no such potential [52].
Against TEM-1, avibactam was 5- and 16-fold more active than tazobactam and clavulanic acid, respectively [53]. This is probably due to the better avibactam bond to TEM-1 enzyme [54]. Interestingly, in a study evaluating avibactam with ceftriaxone, this association showed lower minimum inhibitory concentrations than in ceftazidime combination with avibactam against KPC-producing Klebsiella pneumoniae, probably due to ceftriaxone’s better spectrum for this enterobacterium [55].
The most common mechanism of resistance to ceftazidime–avibactam is the presence of β-lactamase that is not inactivated by avibactam, such as the class B β-lactamases and the majority of the class D β-lactamases. Other mechanisms would be those that act on ceftazidime not by hydrolysis, such as efflux pump and loss of porins [56]. Several mechanisms will be detailed below.
Spectrum of action
Gram-negative bacilli: Enterobacteriaceae
The novel β-lactamase inhibitor avibactam is a potent inhibitor of class A, class C, and some class D enzymes [57]. The addition of avibactam ceftazidime decreases its MIC when used in combination [58,59,60]. A study evaluating those three classes of β-lactamases in Escherichia coli, avibactam combined with ceftazidime, ceftaroline, or aztreonam reduced the MIC in 91.4, 80.0, and 80.0% of isolates, respectively [61].
The ceftazidime–avibactam combination has excellent activity against ESBL- and AmpC-producing Enterobacteriaceae, including strains producing both enzymes [62,63,64,65]. In a test with more than 700 samples of ESBL-producing Enterobacteriaceae, ceftazidime–avibactam proved to be extremely active in various regions of the United States [66]. In a Spanish collection, similar results were found in ESBLs, acquired AmpC β-lactamases and porin loss in Klebsiella pneumoniae [67]. The largest study included 36,380 isolates published in 2017, with 99.2% of susceptibility among Enterobacteriaceae tested in United States. However, only 2953 were multidrug-resistant with 513 carbapenem-resistant Enterobacteriaceae (97.5% susceptible) [68]. Another large sample of isolates tested for ceftazidime–avibactam was published in 2016 with 34,062 isolates of Enterobacteriaceae from patients with intra-abdominal, urinary tract, skin and soft tissue, lower respiratory tract, and blood infections collected in the INFORM (International Network For Optimal Resistance Monitoring) global surveillance study (176 medical center laboratories in 39 countries) [69]. Overall, 99.5% of Enterobacteriaceae isolates were susceptible to ceftazidime–avibactam using FDA-approved breakpoints (susceptible MIC ≤ 8 μg/mL; resistant MIC ≥ 16 μg/mL). Ceftazidime–avibactam demonstrated potent activity against molecularly confirmed ESBL-producing (n = 5354; MIC90, 0.5 μg/mL; 99.9% susceptible), plasmid-mediated AmpC-producing (n = 246; MIC90, 0.5 μg/mL; 100% susceptible), and ESBL- and AmpC-producing (n = 152; MIC90, 1 μg/mL; 100% susceptible) isolates of E. coli, K. pneumoniae, K. oxytoca, and P. mirabilis. In other two surveys with isolates only from intra-abdominal and urinary infections showed that ceftazidime–avibactam had high susceptibility [70]. A subpopulation of isolates from patients hospitalized by pneumonia in US from 2011 and 2015 showed high susceptibility to ceftazidime–avibactam, achieving 99.9% against Enterobacteriaceae [71].
For Gram-negative bacilli it has activity against strains producing class D carbapenemases as OXA-24 and OXA-48 [72], as well as OXA-40 and OXA-69 [73]. In some SHV enzymes such as SHV-1, resistance has been reported related to some mutations [74]. A high percentage of susceptibility (> 95%) to ceftazidime–avibactam was also demonstrated in isolates from airways of patients with mechanical ventilation-associated pneumonia in the intensive care unit [75, 76].
FLAMM et al. studied ceftazidime–avibactam in over 1500 isolates from urine samples from Europe, United States and Latin America [77]. This study also verified the high sensitivity of pathogens to ceftazidime associated with avibactam. Similar results were observed in Brazilian isolates [78] and two studies with isolates from patients with cancer in USA [79, 80]. In a European study including samples from France, Germany, Spain and Italy, the combination of 4 mg/L avibactam with ceftazidime broadens their spectrum of activity to include the majority of β-lactam-resistant Enterobacteriaceae against which this antibiotic alone has poor activity [81]. Despite the unfavorable current sensitivity profile of Enterobacteriaceae to quinolones and resistance profile associated with other genes, including β-lactamase, testing of Enterobacteriaceae strains resistant to fluoroquinolones did not change the activity spectrum of ceftazidime–avibactam against sensitive strains [82]. With the increase in use of aminoglycosides due to the emergence of carbapenemases and polymyxins resistance, 338 isolates of Enterobacteriaceae and P. aeruginosa resistant to aminoglycosides were tested in Canada, yielding 100 and 87.8% of MIC ≤ 8 μg/mL, respectively [83]. The resistance to aminoglycoside in these samples was from methylases (ArmA, RmtA, RmtB, RmtC and RmtD) and modifying enzymes and aminoglycosides (AAC(3)-Ia, AAC(3)-IIa, AAC(3)-IVa, AAC(6′)-Ib/II, ANT(2″)-Ia, APH(3′)-Via). Avibactam also showed to be active against KPC-2-producing bacteria when associated with different β-lactams, such as aztreonam, piperacillin, cefotaxime, ceftazidime and cefepime [84]. The association with ceftaroline was also effective at ≤ 4 mg/L, except for metallo-β-lactamases (VIM and IMP) [85, 86]. In several carbapenemases, not in group B, ceftazidime–avibactam showed sensitivity close to 100% [87, 88]. In one case it has been reported that S130 residues, as well as K234 and R220, contribute significantly to the avibactam inactivation mechanism of KPC-2 [89]. Ceftazidime–avibactam was very active against isolates producing the most common β-lactamases detected in US hospitals, including CTX-M and KPC variants [90, 91]. The resistance of KPC-producing Enterobacteriaceae to ceftazidime–avibactam can occur due to mutations that increase ceftazidimase specificity rather than conferring avibactam resistance; however, the clinical relevance remains uncertain [24]. In 2015 the first case of ceftazidime–avibactam resistance in a KPC-3-producing K. pneumoniae was published [92] and more cases have been described ever since. [93]. For this reason, despite being a promising drug, its use should be cautious [25]. This is because, unlike other β-lactamases, the bond between avibactam and KPC-2 and KPC-3 is different in relation to the others, which theoretically could reduce potency or induce resistance [94].
In the case of NDM enzyme, which is a metallo-β-lactamase, the resistance to ceftazidime–avibactam is well established [95]. Avibactam associated with aztreonam would be an option [96, 97], but there are studies already showing that mutation in PBP3 can confer resistance to the scheme [98]. Furthermore, no synergic activity was found with ceftazidime–avibactam and carbapenem [99]. In other study including KPC-carrying isolates of Klebsiella pneumoniae, synergism was found with amikacin and polymyxin [100].
Ceftazidime hydrolytic activity may limit the usefulness of ceftazidime/avibactam monotherapies in infections caused by isolates carrying blaCTX-M-14 and blaOXA-48 [101]. Recently, it was described a resistance mechanism based on a mutation of an AmpC variant by deletion of one amino acid in the omega loop [102]. Another author also described a lower affinity for extended-spectrum AmpC (ESAC) β-lactamase enzymes in Enterobacter cloacae [103, 104].
Mutations within the KPC Ω-loop (positions 165–179), including a report in KPC-3, can enhance ceftazidime affinity and restrict avibactam binding [25]. Although rare, mutations in specific PBP can be associated with resistance to beta-lactams. Carbapenems have high affinity to PBP2 and PBP3 from E. coli, in contrast to ceftazidime. Single point mutations in PBPs are associated with resistance do ceftazidime, a mechanism which is not reversible with avibactam [105]. A specific mutation of carbapenemase type 2 (KPC-2) harboring the D179Y substitution impaired inhibition by avibactam combined with significant residual activity for ceftazidime hydrolysis, which accounts for resistance. However, such mutations are more common with KPC-3 [106, 107].
Until 2016, resistance to ceftazidime–avibactam was restricted to case reports [108]. Unfortunately, considering recent data, it is important to know that resistance is increasing. As for the KPC-2 enzyme, one of carbapenemases that has brought greater concern nowadays, there is evidence of avibactam hydrolysis by this carbapenemase, and slow deacylation properties [109]. In this slow deacylation, there is no evidence that this could have clinical significance so far. When tested in colistin-resistant Enterobacteriaceae, all the avibactam/ceftazidime activity was independent of the presence of efflux pumps or loss of porins [110]. Nevertheless, in China decreased ceftazidime/avibactam susceptibility in KPC-producing Klebsiella pneumoniae clinical isolates was caused by high ceftazidime hydrolysis activity and OmpK35 porin deficiency in the majority of isolates [111]. On the other hand, in E. coli, none of the porin experimental mutations caused a decrease in susceptibility to ceftazidime–avibactam [112].
Gram-negative bacilli: non-fermenter
In another USA study, over 95% of Pseudomonas aeruginosa isolates from BSI, from pneumonia patients, from intra-abdominal infection and urine exhibited a ceftazidime–avibactam MIC ≤ 8 mg/L (CLSI susceptible breakpoint for ceftazidime when tested alone against P. aeruginosa) [113].
Similarly, ceftazidime–avibactam is effective against P. aeruginosa [114, 115]. Another study evaluating P. aeruginosa showed 18% resistance, but the resistance mechanism was related to loss of porin and efflux pump [116]. The sensitivity profile for P. aeruginosa was good even in strains with high resistance, such as those isolated from patients with cystic fibrosis [117]. A survey of 3902 isolates of P. aeruginosa from 75 US medical centers identified that 96.9% of the strains were susceptible (MIC ≤ 8 μg/mL) [118]. In the same study, susceptibility to ceftazidime–avibactam for multidrug-resistant and extensively drug-resistant phenotypes was 81.0 and 73.7%, respectively. In 2017, the same authors evaluated 7686 isolates from same hospitals, showing similar results [68]. The enzymatically driven β-lactam resistance is the most searched mechanism. One study revealed the exclusive presence of VIM among only 4% of the subset of P. aeruginosa isolates nonsusceptible to ceftazidime–avibactam [119]. Ceftazidime–avibactam has been compared with ceftolozane–tazobactam against P. aeruginosa with similar susceptibility percentages, but lower MIC for ceftolozane–tazobactam [120].
Emergence of resistance during therapy with ceftazidime–avibactam has also been reported. In one case of P. aeruginosa surgical site infection, both initial and final isolates were resistant to carbapenems and evolved with resistance to ceftazidime–avibactam. Sequencing identified blaOXA-2 in initial isolate, but the final isolate contained a 3-bp insertion leading to the duplication of a key residue, designated as OXA-539 [121].
Avibactam increased the potency of ceftazidime against many β-lactamase-producing P. aeruginosa and B. cepacia strains complex but not for efflux-mediated resistance, including a high affinity by PenaA carbapenemase found in some strains of B. cepacia complex [122]. Unfortunately, there are few epidemiological studies evaluating B. cepacia complex, one of them with seven isolates [123].
In a previous study, there was a lack of potentiation of ceftazidime with avibactam against A. baumannii, which was (supposed) to be a failure of avibactam to penetrate and inhibit relevant (OXA-23, -40, -51 and -58) carbapenemases [85, 86, 124]. For P. aeruginosa, the ceftazidime–avibactam activity was superior to imipenem in a study [125]. Part of the resistance in these cases is due to metallo-β-lactamases, or other common mechanisms in P. aeruginosa as efflux pump and loss of porins [126]. On the other hand, there are rare cases of AmpC resistant to avibactam in P. aeruginosa [127]. In P. aeruginosa isolates resistant to carbapenems but without carbapenemases (loss of porin), ceftazidime–avibactam proved to be active in 92% [128]. Avibactam cannot inhibit metallo-carbapenemases, and nor can any other inhibitor in advanced development. The use of a monobactam as the partner drug can be a choice since these are stable to metallo-carbapenemases [87]. Livermore et al. presented a study illustrating the potential of this approach, with MICs of aztreonam–avibactam found to be ≤ 4 μg/mL against all carbapenemase producers, including those with metallo-enzymes [129]. However, in vitro resistance data found were discordant to ceftazidime–avibactam compared to the in vivo response [63].
Anaerobics
Ceftazidime–avibactam has limited action against anaerobic bacteria. Production of beta-lactamases by anaerobes is common in Bacteroides isolates (80–100%) [130]. Most enzymes are chromosomally mediated including serine at the active site as well as metallo-beta-lactamases (class B) [131].
A study with 396 samples demonstrated the inefficiency of this combination against anaerobics, mainly in the most relevant such as Bacteroides fragilis, as well as in other less important bacteria, such as Prevotella spp., Porphyromonas spp., Bilophila wadsworthia, Desulfovibrio spp., Campylobacter spp., Fusobacterium spp., Clostridium clostridioforme group spp., and Eggerthella lenta [132]. In another study, ceftazidime–avibactam was tested in combination with metronidazole then demonstrating superior activity to monotherapy [133]. However, in the study of Goldstein et al., avibactam improved anaerobicide activity of ceftaroline in strains from diabetic foot infection [134].
Other
Some mycobacteria can produce β-lactamases. Mycobacterium abscessus has recently been shown to produce a broad-spectrum β-lactamase (BlaMab). Ceftazidime–avibactam activity was evaluated in an animal model of M. abscessus infection, showing an efficient activity against BlaMab [135].
A macrolide, an aminoglycoside and a β-lactam are used in the treatment of pulmonary infection caused by M. abscessus. Another study evaluated the bactericidal activity of drug combinations assayed in broth and in human macrophages [136]. Inhibition of BlaMab by avibactam improved the efficacy of imipenem. The substitution N132G in the SDN motif of class A β-lactamases from rapidly growing mycobacteria impair the activity of avibactam [137]. This substitution was included in Enterobacteriaceae, but no interference in the activity was detected [138].
Pharmacokinetics
In the mass balance study, the measurement of plasma avibactam and total radioactivity in plasma, whole blood, urine, and feces indicated that most of the avibactam was excreted unchanged in urine with a renal clearance of 158 mL/min, suggesting active tubular secretion. There was no evidence of metabolism in plasma and urine. Avibactam did not interact with various membrane transport proteins or cytochrome P450 enzymes in vitro, decreasing interactions involving cytochrome P450 enzymes [139]. Avibactam is excreted largely unchanged in urine. Ceftazidime–avibactam in patients under continuous venovenous hemofiltration (CVVH) was reported in one case. The authors described the pharmacokinetic; however, it was not possible to predict any drug adjustment [140].
Avibactam was generally well tolerated in healthy young and elderly male and female cohorts in the present study. There were no notable differences in pharmacokinetic parameters between male and female cohorts. The small differences in pharmacokinetic parameters between the young and elderly cohorts are not sufficient to warrant dose adjustments based on age beyond that necessary due to reduced renal function [141, 142]. The pharmacokinetic of avibactam follows a similar tendency of ceftazidime in patients with renal failure, including anuric patients. Thus, the adjustment of dose must maintain the relation with ceftazidime adjustment [143].
A pharmacokinetic evaluation in two patients with acute kidney injury showed that, despite reduced renal clearance, the obesity and large distribution volume can interfere with serum levels of ceftazidime–avibactam, suggesting that dosage for obese patient or increased distribution volume should be reevaluated [144].
Pharmacokinetic parameters of ceftazidime–avibactam are similar to those found in other β-lactams. As a hydrophilic drug, it has distribution volume compatible with its characteristic, being restricted to the extracellular volume.
The penetration of ceftazidime–avibactam in lung tissue is around 30%, based on the drug concentration in lung epithelial fluid [145]. Studies in critically ill patients are needed for future optimized doses for this group of patients.
Ceftazidime–avibactam was described by 1-compartment models in acute pulmonary exacerbation in cystic fibrosis [146]. Total body clearances (CAZ CLt: 7.53 ± 1.28 L/h, AVI CLt: 12.30 ± 1.96 L/h) and volumes of distribution (CAZ Vd: 18.80 ± 6.54 L, AVI Vd: 25.30 ± 4.43 L) were broadly similar to published in healthy adults.
It is important to report that ceftazidime–avibactam was incompatible with vancomycin [147].
Pharmacodynamics
The best pharmacodynamic profile of ceftazidime–avibactam is ƒT > MIC, validated in an animal model of soft tissue infection [59, 60].
An in vitro study of continuous infusion of ceftazidime–avibactam or ceftazidime continuous with avibactam as bolus showed that in this case, both drugs should run in continuous infusion, as the time period that ceftazidime is uncovered by avibactam allows bacterial regrowth [148]. Ceftazidime–avibactam showed no antagonism when combined with tobramycin, levofloxacin, linezolid, vancomycin, tigecycline and colistin [149]. Furthermore, it was shown that ceftazidime/avibactam activity is not influenced by the surfactant, as with daptomycin. A pharmacodynamic simulation using KPC-producing K. pneumoniae, CTX-M producing E. coli and AmpC-hyperproducing Enterobacter cloacae showed that higher level of avibactam (2–4 times) are necessary to achieve antibacterial effect in carbapenemase-producing isolate [150].
In chronic dialysis patients, a dose of 1 g ceftazidime after dialysis is sufficient to maintain a ƒT > MIC profile of 70%, a value defined by the author [151]. With larger phase 3 studies, more pharmacodynamic information is available for evaluation and mathematical models of projection.
Pseudomonas aeruginosa can present intracellular and extracellular forms, which can be associated with therapeutic failure. Buyck et al. evaluated the concentration of ceftazidime–avibactam in these different compartments. The efficacy of ceftazidime–avibactam against intracellular isolates was suboptimal, probably associated with concentrations near to MIC [152]. In a time–kill curve model using P. aeruginosa resistant to carbapenem, ceftazidime and piperacillin–tazobactam, the activity of ceftazidime was restored [153].
The post-antibiotic effect is a well studied characteristic of aminoglycosides. However, beta-lactamics can also present a variable effect. In this aspect, avibactam was evaluated and curiously, the effect was not a constant, but strain dependent, a mechanism that needs more studies to be confirmed [154].
In vivo studies
A time–kill curve (TKC) study showed that ceftazidime–avibactam has potent bactericidal activity in 18 strains of P. aeruginosa [155]. Several carbapenemases were tested, and regrowth occurred in a few isolates.
A study in the mouse septicemia model demonstrated that the potent in vitro activity observed with the ceftazidime–avibactam combination against ceftazidime-resistant Enterobacteriaceae species bearing class A and class (TEM-1, TEM-2, SHV-5, SHV-4, CTX-M-2, CTX-M-15, CTXM-16) C-lactamases (AmpC).
In two murine models of infection by KPC-producing K. pneumoniae with MIC ≥ 256 mg/L to ceftazidime, ceftazidime–avibactam proved to be active and was effective in models of septicemia and soft tissue infection [156].
In a pharmacokinetics simulation in an infection model in mice, the standard would be the ideal conditions of ƒT > MIC of 100%. In this model, the ceftaroline/avibactam combination demonstrated efficacy in the treatment of ESBL- and KPC-producing bacteria when MIC ≤ 1 mg/L [157]. A similar study was conducted by the same group, but testing P. aeruginosa with high MIC for ceftazidime and aztreonam–avibactam [158, 159]. In vitro synergy was observed with ceftazidime–avibactam and aztreonam against Klebsiella pneumoniae harboring blaNDM, blaOXA-48, and blaCTX-M. Despite the in vitro synergism, no in vivo synergy was observed [160].
Ceftazidime–avibactam was evaluated in a murine model of pneumonia caused by P. aeruginosa. This model showed that a dose equivalent to 2 g ceftazidime and 500 mg avibactam every 8 h was sufficient to inhibit the growth of strains with MIC < 32. However, when the MIC was ≥ 32, the response was not effective. It was evident that ceftazidime–avibactam is an effective drug combination in pneumonia caused by P. aeruginosa [161]. Another study also has measured the ceftazidime–avibactam levels in the epithelial lining fluid (ELF), which were linear with serum levels and probably effective for lower respiratory tract infection [59].
Effect on human microbiota
Ceftazidime–avibactam is a broad-spectrum antibiotic, and thus it is expected to cause modification of the intestinal microbiota. The number of Escherichia coli and other Enterobacteriaceae decreases significantly during administration, whereas the number of enterococci increases. Lactobacilli, bifidobacteria, clostridia and Bacteroides decrease significantly during ceftazidime–avibactam administration. Toxigenic Clostridium difficile strains were detected in five volunteers during the study. Feces samples were collected and ceftazidime–avibactam concentrations varied from 0 to 468.2 mg/kg and avibactam 0–146.0 mg/kg of feces, respectively [162].
Clinical trials
Intra-abdominal infection
The phase II study published in 2014 evaluated the efficacy, safety and tolerability of ceftazidime–avibactam plus metronidazole versus meropenem in the treatment of complicated intra-abdominal infections in 204 hospitalized adults [27]. Patients were enrolled by the clinical investigator and randomized in a 1: 1 ratio balanced according to the baseline severity of disease. The dose was a combination of 2000 mg ceftazidime and 500 mg avibactam iv every 8 h. Treatment was given for a minimum of 5 days and a maximum of 14 days, depending upon clinical response. No other concomitant systemic antibiotics were permitted except for vancomycin, linezolid or daptomycin, which were permitted for suspected or documented MRSA or enterococcal infections. The primary efficacy endpoint was the clinical response at the test-of-cure (TOC) visit in the microbiologically evaluable (ME) population, a subset of the clinically evaluable (CE) population.
Clinical response in the ME population at the TOC visit was observed in 91.2% (62/68) and 93.4% (71/76) of ceftazidime–avibactam plus metronidazole and meropenem patients, respectively. The estimated difference in response rates was − 2.2% (95% CI − 20.4, 12.2%). At the end of iv therapy, a favorable clinical response was observed in 97.1% (66/68) and 97.4% (74/76) of ME patients in the ceftazidime–avibactam plus metronidazole and meropenem groups, respectively (observed difference: − 0.3%; 95% CI − 17.1, 15.4%).
A phase 3 study with data from 2 identical, prospective, randomized, multicenter, double-dummy, double-blind, comparative, global studies at 136 centers in 30 countries [29]. Patients were randomly allocated 1:1 to receive either ceftazidime–avibactam (2000 mg ceftazidime and 500 mg avibactam as a 2-h intravenous infusion every 8 h), followed by metronidazole (500 mg as a 60-min intravenous infusion every 8 h); or meropenem (1000 mg as a 30-min intravenous infusion every 8 h). Of 1066 patients, 529 received ≥ 1 dose of ceftazidime–avibactam plus metronidazole, and 529 ≥ 1 dose of meropenem. At the end of iv therapy, a favorable clinical response was observed in 97.1 and 92.5% of ME patients in the ceftazidime–avibactam plus metronidazole and meropenem groups, respectively (observed difference: − 0.3%; 95% CI − 17.1, 15.4%). Similar results were found in another phase 3 study in Asia. This study included 441 patients with similar clinical response between meropenem and ceftazidime–avibactam plus meropenem, 93.8% (166/177) and 94.0% (173/184) of subjects, respectively.
A post hoc analysis of clinical cure according with type of beta-lactamase was performed. Ceftazidime–avibactam had clinical cure rates of more than 90% among patients infected with ESBL- and/or carbapenemase-producing Enterobacteriaceae, but only 75% among patients with pathogens producing AmpC enzymes [163].
Urinary infection
Ceftazidime–avibactam was tested in a prospective phase II, randomized, investigator-blind study to compare the efficacy and safety using imipenem as comparator in hospitalized adults with serious complicated urinary tract infection (cUTI) [28]. Patients were stratified by infection type (acute pyelonephritis or other cUTI) and randomized 1:1 to receive intravenous ceftazidime 500 mg plus avibactam 125 mg every 8 h or imipenem–cilastatin 500 mg every 6 h. The primary efficacy objective was a favorable microbiological response at the test-of-cure (TOC) visit 5–9 days post-therapy in microbiologically evaluable (ME) patients. Sixty-two patients were included in the ME population (ceftazidime–avibactam, n = 27; imipenem–cilastatin, n = 35) with favorable microbiological response achieved in 70.4% of ME patients receiving ceftazidime–avibactam and 71.4% receiving imipenem–cilastatin at the TOC visit [observed difference − 1.1% (95% CI − 27.2, 25.0%)].
The phase III study, ceftazidime–avibactam was compared with doripenem for the treatment of cUTI, including pyelonephritis. From 1033 patients, the drug were equally effective, however, ceftazidime–avibactam is an option to avoid carbapenem use in ESBL isolates [164].
After 1 year, the activity of ceftazidime–avibactam against ceftazidime-nonsusceptible Gram-negative isolates from both clinical trials was evaluated. Overall, the ceftazidime–avibactam activity was comparable to previously reported against ceftazidime-susceptible isolates [165].
Other
Ceftazidime–avibactam is been evaluated versus meropenem in hospitalized adults with nosocomial pneumonia (NCT01808092) and neutropenic patients (NCT02732327). In pediatric patients, the first study (NCT01893346), a phase I study, assessed the pharmacokinetic profile and safety of a single dose of ceftazidime–avibactam. Four cohorts were evaluated, including age ≥ 12 to < 18 years and ≥ 3 months to < 2 years. The dose varied as 12.5–50 mg/kg, showing similar profile of adults’ patients. The study evaluates only one dose; thus, more studies are necessary to evaluate the kinetic and safety after multiple doses [166].
Although clinical studies direct the drug for intra-abdominal and urinary infection, ceftazidime–avibactam is a drug with perspective for use in carbapenemase-producing bacteria, which usually involve critically ill patients in the ICU. The pharmacokinetic properties of ceftazidime in severely ill patients are already known; however, it lacks studies for avibactam. Anyway, there are already reports of treatment of serious infections in this population. A study comparing colistin versus ceftazidime–avibactam showed good response, including lower mortality percentage, but with a small number of patients to reach a conclusion [167]. The fact is that it is hard to believe that a drug with ceftazidime–avibactam profile will have a response lower to that of polymyxins, knowing the poor pharmacokinetic profile of polymyxins in critically ill patients, when compared with a β-lactam.
After clinical trial, some retrospective studies have been published, including comparative analysis against polymyxin and amikacin in the treatment of carbapenem-resistant Klebsiella spp. [168]. Ceftazidime–avibactam treatment of carbapenem-resistant Klebsiella pneumoniae bacteremia was associated with higher rates of clinical success and survival than aminoglycoside- or colistin-containing regimens. According to the authors from a retrospective study with only descriptive data, ceftazidime–avibactam was an appropriate option with in-hospital mortality of 32% in 60 patients [169]. Another study evaluated bacteremia by carbapenem-resistant Enterobacteriaceae in hematologic patients, suggesting better results than comparator (85.7 vs. 34.8%, respectively, p = 0.031) [170].
Other descriptive studies have shown discrepant results, in general, with few patients [171]. One study evaluated 121 patients with carbapenem-resistant Enterobacteriaceae bacteremia. The mortality was high, independent of therapy choice, including ceftazidime–avibactam. However, there was a median of 47 h until patients receive active antimicrobial therapy [172].
In a compassionate-use basis, ceftazidime–avibactam was used for treatment of 36 patients with severe infection caused by carbapenem-resistant bacteria. Survival was attributed to microbiological cure (71.4% mortality in patients without microbiological cure, p = 0.01). Most of these patients received previous therapy and the mean duration of ceftazidime–avibactam therapy was 16 days. This report reaffirms the importance of microbiological cure to improve survival. However, with recent publications of ceftazidime–avibactam resistance, a careful stewardship program is important to avoid rapid resistance emergence [173]. In another descriptive study, microbiological cure failure was associated with low susceptibility of isolates to ceftazidime–avibactam, achieving 30% in ten isolates from 37 patients evaluated [174].
In summary, ceftazidime–avibactam is a very attractive antimicrobial combination given its broad spectrum of action, including multidrug-resistant bacteria. The pharmacokinetic profile is similar to that of injectable cephalosporins. The susceptibility profile is still high, but there are already resistant strains and the risk is higher in carbapenemases of KPC-2 type. It will be a very important drug in the treatment of nosocomial infections.
References
Yigit H, Queenan AM, Anderson GJ, Domenech-Sanchez A, Biddle JW, Steward CD, Alberti S, Bush K, Tenover FC. Novel carbapenem-hydrolyzing beta-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother. 2001;45:1151–61.
Endimiani A, Luzzaro F, Brigante G, Perilli M, Lombardi G, Amicosante G, Rossolini GM, Toniolo A. Proteus mirabilis bloodstream infections: risk factors and treatment outcome related to the expression of extended-spectrum beta-lactamases. Antimicrob Agents Chemother. 2005;49:2598–605.
Yigit H, Queenan AM, Rasheed JK, Biddle JW, Domenech-Sanchez A, Alberti S, Bush K, Tenover FC. Carbapenem-resistant strain of Klebsiella oxytoca harboring carbapenem-hydrolyzing beta-lactamase KPC-2. Antimicrob Agents Chemother. 2003;47:3881–9.
Qureshi ZA, Paterson DL, Potoski BA, Kilayko MC, Sandovsky G, Sordillo E, Polsky B, Adams-Haduch JM, Doi Y. Treatment outcome of bacteremia due to KPC-producing Klebsiella pneumoniae: superiority of combination antimicrobial regimens. Antimicrob Agents Chemother. 2012;56:2108–113.
Kitchel B, Rasheed JK, Endimiani A, Hujer AM, Anderson KF, Bonomo RA, Patel JB. Genetic factors associated with elevated carbapenem resistance in KPC-producing Klebsiella pneumoniae. Antimicrob Agents Chemother. 2010;54:4201–7.
Naas T, Cuzon G, Villegas MV, Lartigue MF, Quinn JP, Nordmann P. Genetic structures at the origin of acquisition of the beta-lactamase bla KPC gene. Antimicrob Agents Chemother. 2008;52:1257–63.
Bratu S, Brooks S, Burney S, Kochar S, Gupta J, Landman D, Quale J. Detection and spread of Escherichia coli possessing the plasmid-borne carbapenemase KPC-2 in Brooklyn, New York. Clin Infect Dis. 2007;44:972–5.
Leavitt A, Carmeli Y, Chmelnitsky I, Goren MG, Ofek I, Navon-Venezia S. Molecular epidemiology, sequence types, and plasmid analyses of KPC-producing Klebsiella pneumoniae strains in Israel. Antimicrob Agents Chemother. 2010;54:3002–6.
Villegas MV, Lolans K, Correa A, Suarez CJ, Lopez JA, Vallejo M, Quinn JP. Colombian nosocomial resistance study G. First detection of the plasmid-mediated class A carbapenemase KPC-2 in clinical isolates of Klebsiella pneumoniae from South America. Antimicrob Agents Chemother. 2006;50:2880–2.
Woodford N, Zhang J, Warner M, Kaufmann ME, Matos J, Macdonald A, Brudney D, Sompolinsky D, Navon-Venezia S, Livermore DM. Arrival of Klebsiella pneumoniae producing KPC carbapenemase in the United Kingdom. J Antimicrob Chemother. 2008;62:1261–4.
Pavez M, Mamizuka EM, Lincopan N. Early dissemination of KPC-2-producing Klebsiella pneumoniae strains in Brazil. Antimicrob Agents Chemother. 2009;53:2702.
Peirano G, Seki LM, Val Passos VL, Pinto MC, Guerra LR, Asensi MD. Carbapenem-hydrolysing beta-lactamase KPC-2 in Klebsiella pneumoniae isolated in Rio de Janeiro, Brazil. J Antimicrob Chemother. 2009;63:265–8.
Fehlberg LC, Carvalho AM, Campana EH, Gontijo-Filho PP, Gales AC. Emergence of Klebsiella pneumoniae-producing KPC-2 carbapenemase in Paraiba, Northeastern Brazil. Braz J Infect Dis. 2012;16:577–80.
Cabral AB, Melo Rde C, Maciel MA, Lopes AC. Multidrug resistance genes, including bla(KPC) and bla(CTX)-M-2, among Klebsiella pneumoniae isolated in Recife, Brazil. Rev Soc Bras Med Trop. 2012;45:572–8.
Gales AC, Castanheira M, Jones RN, Sader HS. Antimicrobial resistance among Gram-negative bacilli isolated from Latin America: results from SENTRY Antimicrobial Surveillance Program (Latin America, 2008–2010). Diagn Microbiol Infect Dis. 2012;73:354–60.
Nordmann P, Cuzon G, Naas T. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect Dis. 2009;9:228–36.
Rossi F. The challenges of antimicrobial resistance in Brazil. Clin Infect Dis. 2011;52:1138–43.
Wise R, Andrews JM, Bedford KA. Comparison of in vitro activity of GR 20263, a novel cephalosporin derivative, with activities of other beta-lactam compounds. Antimicrob Agents Chemother. 1980;17:884–9.
Clarke AM, Zemcov SJ. Ro 13-9904 and GR 20263, two new cephalosporins with broad-spectrum activity: an in vitro comparison with other beta-lactam antibiotics. J Antimicrob Chemother. 1981;7:515–20.
Philippon A, Ben Redjeb S, Fournier G, Ben Hassen A. Epidemiology of extended spectrum beta-lactamases. Infection. 1989;17:347–54.
Nathisuwan S, Burgess DS, Lewis JS 2nd. Extended-spectrum beta-lactamases: epidemiology, detection, and treatment. Pharmacotherapy. 2001;21:920–8.
Lomaestro BM, Tobin EH, Shang W, Gootz T. The spread of Klebsiella pneumoniae carbapenemase-producing K. pneumoniae to upstate New York. Clin Infect Dis. 2006;43:e26–8.
Osano E, Arakawa Y, Wacharotayankun R, Ohta M, Horii T, Ito H, Yoshimura F, Kato N. Molecular characterization of an enterobacterial metallo beta-lactamase found in a clinical isolate of Serratia marcescens that shows imipenem resistance. Antimicrob Agents Chemother. 1994;38:71–8.
Livermore DM, Warner M, Jamrozy D, Mushtaq S, Nichols WW, Mustafa N, Woodford N. In vitro selection of ceftazidime-avibactam resistance in Enterobacteriaceae with KPC-3 carbapenemase. Antimicrob Agents Chemother. 2015;59:5324–30.
Shields RK, Nguyen MH, Press EG, Chen L, Kreiswirth BN, Clancy CJ. In vitro selection of meropenem resistance among ceftazidime-avibactam resistant, meropenem susceptible Klebsiella pneumoniae isolates with variant KPC-3 carbapenemases. Antimicrob Agents Chemother. 2017.
Livermore DM, Mushtaq S, Warner M, Miossec C, Woodford N. NXL104 combinations versus Enterobacteriaceae with CTX-M extended-spectrum beta-lactamases and carbapenemases. J Antimicrob Chemother. 2008;62:1053–6.
Lucasti C, Popescu I, Ramesh MK, Lipka J, Sable C. Comparative study of the efficacy and safety of ceftazidime/avibactam plus metronidazole versus meropenem in the treatment of complicated intra-abdominal infections in hospitalized adults: results of a randomized, double-blind. Phase II trial. J Antimicrob Chemother. 2013;68:1183–92.
Vazquez JA, Gonzalez Patzan LD, Stricklin D, Duttaroy DD, Kreidly Z, Lipka J, Sable C. Efficacy and safety of ceftazidime-avibactam versus imipenem-cilastatin in the treatment of complicated urinary tract infections, including acute pyelonephritis, in hospitalized adults: results of a prospective, investigator-blinded, randomized study. Curr Med Res Opin. 2012;28:1921–31.
Mazuski JE, Gasink LB, Armstrong J, Broadhurst H, Stone GG, Rank D, Llorens L, Newell P, Pachl J. Efficacy and safety of ceftazidime-avibactam plus metronidazole versus meropenem in the treatment of complicated intra-abdominal infection: results from a randomized, controlled, double-blind, phase 3 program. Clin Infect Dis. 2016;62:1380–9.
de Jonge BL, Karlowsky JA, Kazmierczak KM, Biedenbach DJ, Sahm DF, Nichols WW. In vitro susceptibility to ceftazidime-avibactam of carbapenem-nonsusceptible Enterobacteriaceae isolates collected during the INFORM global surveillance study (2012–2014). Antimicrob Agents Chemother. 2016;60:3163–9.
Sader HS, Castanheira M, Flamm RK, Farrell DJ, Jones RN. Antimicrobial activity of ceftazidime-avibactam against Gram-negative organisms collected from US medical centers in 2012. Antimicrob Agents Chemother. 2014;58:1684–92.
Verbist L, Verhaegen J. GR-20263: a new aminothiazolyl cephalosporin with high activity against Pseudomonas and Enterobacteriaceae. Antimicrob Agents Chemother. 1980;17:807–12.
Aszodi J, Rowlands DA, Mauvais P, Collette P, Bonnefoy A, Lampilas M. Design and synthesis of bridged gamma-lactams as analogues of beta-lactam antibiotics. Bioorg Med Chem Lett. 2004;14:2489–92.
Kitzis MD, Goldstein FW, Labia R, Acar JF. Activity of sulbactam and clavulanic acid, alone and combined, on Acinetobacter calcoaceticus. Ann Microbiol (Paris). 1983;134A:163–8.
Das S, Li J, Armstrong J, Learoyd M, Edeki T. Randomized pharmacokinetic and drug-drug interaction studies of ceftazidime, avibactam, and metronidazole in healthy subjects. Pharmacol Res Perspect. 2015;3:e00172.
Jones RN, Holliday NM, Krause KM. Validation of sensititre dry-form broth microdilution panels for susceptibility testing of ceftazidime-avibactam, a broad-spectrum-beta-lactamase inhibitor combination. Antimicrob Agents Chemother. 2015;59:5036–9.
CLSI. Clinical Laboratory Standard Institute—performance standard for antimicrobial susceptibility testing; Twenty-Third Informational Supplement. 2017.
Drawz SM, Bonomo RA. Three decades of beta-lactamase inhibitors. Clin Microbiol Rev. 2010;23:160–201.
Bonomo RA. Beta-Lactamases: a focus on current challenges. Cold Spring Harb Perspect Med. 2017;7.
Walther-Rasmussen J, Hoiby N. OXA-type carbapenemases. J Antimicrob Chemother. 2006;57:373–83.
Macheboeuf P, Contreras-Martel C, Job V, Dideberg O, Dessen A. Penicillin binding proteins: key players in bacterial cell cycle and drug resistance processes. FEMS Microbiol Rev. 2006;30:673–91.
Humphries RM, Hemarajata P. Resistance to Ceftazidime-Avibactam in Klebsiella pneumoniae Due to Porin Mutations and the Increased Expression of KPC-3. Antimicrob Agents Chemother. 2017;61. Epub 2017/04/12.
Sgrignani J, Grazioso G, De Amici M, Colombo G. Inactivation of TEM-1 by avibactam (NXL-104): insights from quantum mechanics/molecular mechanics metadynamics simulations. Biochemistry. 2014;53:5174–85.
Ehmann DE, Jahic H, Ross PL, Gu RF, Hu J, Kern G, Walkup GK, Fisher SL. Avibactam is a covalent, reversible, non-beta-lactam beta-lactamase inhibitor. Proc Natl Acad Sci USA. 2012;109:11663–8.
Lahiri SD, Mangani S, Durand-Reville T, Benvenuti M, De Luca F, Sanyal G, Docquier JD. Structural insight into potent broad-spectrum inhibition with reversible recyclization mechanism: avibactam in complex with CTX-M-15 and Pseudomonas aeruginosa AmpC beta-lactamases. Antimicrob Agents Chemother. 2013;57:2496–505.
Choi H, Paton RS, Park H, Schofield CJ. Investigations on recyclisation and hydrolysis in avibactam mediated serine beta-lactamase inhibition. Org Biomol Chem. 2016;14:4116–28.
Asli A, Brouillette E, Krause KM, Nichols WW, Malouin F. Distinctive binding of avibactam to penicillin-binding proteins of Gram-Negative and Gram-Positive bacteria. Antimicrob Agents Chemother. 2016;60:752–6.
Papp-Wallace KM, Winkler ML, Gatta JA, Taracila MA, Chilakala S, Xu Y, Johnson JK, Bonomo RA. Reclaiming the efficacy of beta-lactam-beta-lactamase inhibitor combinations: avibactam restores the susceptibility of CMY-2-producing Escherichia coli to ceftazidime. Antimicrob Agents Chemother. 2014;58:4290–7.
Lahiri SD, Bradford PA, Nichols WW, Alm RA. Structural and sequence analysis of class A beta-lactamases with respect to avibactam inhibition: impact of Omega-loop variations. J Antimicrob Chemother. 2016;71:2848–55.
Abboud MI, Damblon C, Brem J, Smargiasso N, Mercuri P, Gilbert B, Rydzik AM, Claridge TD, Schofield CJ, Frere JM. Interaction of avibactam with Class B metallo-beta-lactamases. Antimicrob Agents Chemother. 2016;60:5655–62 Epub 2016/07/13.
Lister PD, Gardner VM, Sanders CC. Clavulanate induces expression of the Pseudomonas aeruginosa AmpC cephalosporinase at physiologically relevant concentrations and antagonizes the antibacterial activity of ticarcillin. Antimicrob Agents Chemother. 1999;43:882–9.
Miossec C, Claudon M, Levasseur P, Black MT. The beta-lactamase inhibitor avibactam (NXL104) does not induce ampC beta-lactamase in Enterobacter cloacae. Infect Drug Resist. 2013;6:235–40.
Bonnefoy A, Dupuis-Hamelin C, Steier V, Delachaume C, Seys C, Stachyra T, Fairley M, Guitton M, Lampilas M. In vitro activity of AVE1330A, an innovative broad-spectrum non-beta-lactam beta-lactamase inhibitor. J Antimicrob Chemother. 2004;54:410–7.
Stachyra T, Pechereau MC, Bruneau JM, Claudon M, Frere JM, Miossec C, Coleman K, Black MT. Mechanistic studies of the inactivation of TEM-1 and P99 by NXL104, a novel non-beta-lactam beta-lactamase inhibitor. Antimicrob Agents Chemother. 2010;54:5132–8.
Stachyra T, Levasseur P, Pechereau MC, Girard AM, Claudon M, Miossec C, Black MT. In vitro activity of the {beta}-lactamase inhibitor NXL104 against KPC-2 carbapenemase and Enterobacteriaceae expressing KPC carbapenemases. J Antimicrob Chemother. 2009;64:326–9.
Nelson K, Hemarajata P, Sun D, Rubio-Aparicio D, Tsivkovski R, Yang S, Sebra R, Kasarskis A, Nguyen H, Hanson BM, Leopold S, Weinstock G, Lomovskaya O, Humphries RM. Resistance to ceftazidime-avibactam is due to transposition of KPC in a porin-deficient strain of Klebsiella pneumoniae with increased efflux activity. Antimicrob Agents Chemother. 2017;61 (Epub 2017/07/26).
Levasseur P, Girard AM, Miossec C, Pace J, Coleman K. In vitro antibacterial activity of the ceftazidime-avibactam combination against enterobacteriaceae, including strains with well-characterized beta-lactamases. Antimicrob Agents Chemother. 2015;59:1931–4.
Berkhout J, Melchers MJ, van Mil AC, Nichols WW, Mouton JW. In vitro activity of ceftazidime-avibactam combination in in vitro checkerboard assays. Antimicrob Agents Chemother. 2015;59:1138–44.
Berkhout J, Melchers MJ, van Mil AC, Seyedmousavi S, Lagarde CM, Nichols WW, Mouton JW. Pharmacokinetics and penetration of ceftazidime and avibactam into epithelial lining fluid in thigh- and lung-infected mice. Antimicrob Agents Chemother. 2015;59:2299–304.
Berkhout J, Melchers MJ, van Mil AC, Seyedmousavi S, Lagarde CM, Schuck VJ, Nichols WW, Mouton JW. Pharmacodynamics of ceftazidime and avibactam in neutropenic mice with thigh or lung infection. Antimicrob Agents Chemother. 2015;60:368–75.
Papp-Wallace KM, Bajaksouzian S, Abdelhamed AM, Foster AN, Winkler ML, Gatta JA, Nichols WW, Testa R, Bonomo RA, Jacobs MR. Activities of ceftazidime, ceftaroline, and aztreonam alone and combined with avibactam against isogenic Escherichia coli strains expressing selected single beta-lactamases. Diagn Microbiol Infect Dis. 2015;82:65–9.
Lagace-Wiens P, Walkty A, Karlowsky JA. Ceftazidime-avibactam: an evidence-based review of its pharmacology and potential use in the treatment of Gram-negative bacterial infections. Core Evid. 2014;9:13–25.
MacVane SH, Crandon JL, Nichols WW, Nicolau DP. In vivo efficacy of humanized exposures of ceftazidime-avibactam in comparison with ceftazidime against contemporary Enterobacteriaceae isolates. Antimicrob Agents Chemother. 2014;58:6913–9.
MacVane SH, Crandon JL, Nichols WW, Nicolau DP. Unexpected in vivo activity of ceftazidime alone and in combination with avibactam against New Delhi metallo-beta-lactamase-producing Enterobacteriaceae in a murine thigh infection model. Antimicrob Agents Chemother. 2014;58:7007–9.
Li H, Estabrook M, Jacoby GA, Nichols WW, Testa RT, Bush K. In vitro susceptibility of characterized beta-lactamase-producing strains tested with avibactam combinations. Antimicrob Agents Chemother. 2015;59:1789–93.
Castanheira M, Farrell SE, Krause KM, Jones RN, Sader HS. Contemporary diversity of beta-lactamases among Enterobacteriaceae in the nine US census regions and ceftazidime-avibactam activity tested against isolates producing the most prevalent beta-lactamase groups. Antimicrob Agents Chemother. 2014;58:833–8.
Lopez-Hernandez I, Alonso N, Fernandez-Martinez M, Zamorano L, Rivera A, Oliver A, Conejo MC, Martinez-Martinez L, Navarro F, Pascual A. Activity of ceftazidime-avibactam against multidrug-resistance Enterobacteriaceae expressing combined mechanisms of resistance. Enferm Infecc Microbiol Clin. 2017;35:499–504 Epub 2016/11/27.
Sader HS, Castanheira M, Shortridge D, Mendes RE, Flamm RK. Antimicrobial activity of ceftazidime-avibactam tested against multidrug-resistant Enterobacteriaceae and Pseudomonas aeruginosa isolates from United States Medical Centers (2013–2016). Antimicrob Agents Chemother. 2017 (Epub 2017/08/23).
Karlowsky JA, Biedenbach DJ, Kazmierczak KM, Stone GG, Sahm DF. Activity of ceftazidime-avibactam against extended-spectrum- and AmpC beta-lactamase-producing Enterobacteriaceae collected in the INFORM global surveillance study from 2012 to 2014. Antimicrob Agents Chemother. 2016;60:2849–57.
Sader HS, Castanheira M, Flamm RK, Huband MD, Jones RN. Ceftazidime-avibactam activity against aerobic Gram negative organisms isolated from intra-abdominal infections in United States Hospitals, 2012–2014. Surg Infect (Larchmt). 2016;17:473–8.
Sader HS, Castanheira M, Flamm RK. Antimicrobial activity of ceftazidime-avibactam against gram-negative bacteria isolated from patients hospitalized with pneumonia in US Medical Centers, 2011–2015. Antimicrob Agents Chemother. 2011;2017:61 Epub 2017/01/11.
Lahiri SD, Mangani S, Jahic H, Benvenuti M, Durand-Reville TF, De Luca F, Ehmann DE, Rossolini GM, Alm RA, Docquier JD. Molecular basis of selective inhibition and slow reversibility of avibactam against class D carbapenemases: a structure-guided study of OXA-24 and OXA-48. ACS Chem Biol. 2015;10:591–600.
Yoshizumi A, Ishii Y, Aoki K, Testa R, Nichols WW, Tateda K. In vitro susceptibility of characterized beta-lactamase-producing Gram-negative bacteria isolated in Japan to ceftazidime-, ceftaroline-, and aztreonam-avibactam combinations. J Infect Chemother. 2015;21:148–51.
Winkler ML, Papp-Wallace KM, Taracila MA, Bonomo RA. Avibactam and inhibitor-resistant SHV beta-lactamases. Antimicrob Agents Chemother. 2015;59:3700–9.
Sader HS, Castanheira M, Flamm RK, Mendes RE, Farrell DJ, Jones RN. Ceftazidime/avibactam tested against Gram-negative bacteria from intensive care unit (ICU) and non-ICU patients, including those with ventilator-associated pneumonia. Int J Antimicrob Agents. 2015;46:53–9.
Flamm RK, Nichols WW, Sader HS, Farrell DJ, Jones RN. In vitro activity of ceftazidime/avibactam against Gram-negative pathogens isolated from pneumonia in hospitalised patients, including ventilated patients. Int J Antimicrob Agents. 2016;47:235–42.
Flamm RK, Sader HS, Farrell DJ, Jones RN. Ceftazidime-avibactam and comparator agents tested against urinary tract isolates from a global surveillance program (2011). Diagn Microbiol Infect Dis. 2014;80:233–8.
Rossi F, Cury AP, Franco MRG, Testa R, Nichols WW. The in vitro activity of ceftazidime-avibactam against 417 Gram-negative bacilli collected in 2014 and 2015 at a teaching hospital in Sao Paulo, Brazil. Braz J Infect Dis. 2017 (Epub 2017/04/25).
Hachem R, Reitzel R, Rolston K, Chaftari AM, Raad I. Antimicrobial activities of ceftazidime-avibactam and comparator agents against clinical bacteria isolated from patients with cancer. Antimicrob Agents Chemother. 2017;61 (Epub 2017/01/25).
Sader HS, Castanheira M, Jones RN, Flamm RK. Antimicrobial activity of ceftazidime-avibactam and comparator agents when tested against bacterial isolates causing infection in cancer patients (2013–2014). Diagn Microbiol Infect Dis. 2017;87:261–5 Epub 2017/01/11.
Testa R, Canton R, Giani T, Morosini MI, Nichols WW, Seifert H, Stefanik D, Rossolini GM, Nordmann P. In vitro activity of ceftazidime, ceftaroline and aztreonam alone and in combination with avibactam against European Gram-negative and Gram-positive clinical isolates. Int J Antimicrob Agents. 2015;45:641–6.
Pitart C, Marco F, Keating TA, Nichols WW, Vila J. Activity of ceftazidime-avibactam against fluoroquinolone-resistant Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2015;59:3059–65.
Denisuik AJ, Karlowsky JA, Denisuik T, Nichols WW, Keating TA, Adam HJ, Baxter M, Walkty A, Zhanel GG. In vitro activity of ceftazidime-avibactam against 338 molecularly characterized gentamicin-nonsusceptible Gram-negative clinical isolates obtained from patients in Canadian hospitals. Antimicrob Agents Chemother. 2015;59:3623–6.
Endimiani A, Hujer KM, Hujer AM, Armstrong ES, Choudhary Y, Aggen JB, Bonomo RA. ACHN-490, a neoglycoside with potent in vitro activity against multidrug-resistant Klebsiella pneumoniae isolates. Antimicrob Agents Chemother. 2009;53:4504–7.
Mushtaq S, Warner M, Livermore DM. In vitro activity of ceftazidime + NXL104 against Pseudomonas aeruginosa and other non-fermenters. J Antimicrob Chemother. 2010;65:2376–81.
Mushtaq S, Warner M, Williams G, Critchley I, Livermore DM. Activity of chequerboard combinations of ceftaroline and NXL104 versus beta-lactamase-producing Enterobacteriaceae. J Antimicrob Chemother. 2010;65:1428–32.
Vasoo S, Cunningham SA, Cole NC, Kohner PC, Menon SR, Krause KM, Harris KA, De PP, Koh TH, Patel R. In vitro activities of ceftazidime-avibactam, aztreonam-avibactam, and a panel of older and contemporary antimicrobial agents against carbapenemase-producing Gram-Negative Bacilli. Antimicrob Agents Chemother. 2015;59:7842–6.
Dupont H, Gaillot O, Goetgheluck AS, Plassart C, Emond JP, Lecuru M, Gaillard N, Derdouri S, Lemaire B, Girard de Courtilles M, Cattoir V, Mammeri H. Molecular characterization of carbapenem-nonsusceptible enterobacterial isolates collected during a prospective interregional survey in France and susceptibility to the novel ceftazidime-avibactam and aztreonam-avibactam combinations. Antimicrob Agents Chemother. 2015;60:215–21.
Papp-Wallace KM, Winkler ML, Taracila MA, Bonomo RA. Variants of beta-lactamase KPC-2 that are resistant to inhibition by avibactam. Antimicrob Agents Chemother. 2015;59:3710–7.
Castanheira M, Mills JC, Costello SE, Jones RN, Sader HS. Ceftazidime-avibactam activity tested against Enterobacteriaceae isolates from US hospitals (2011–2013) and characterization of beta-lactamase-producing strains. Antimicrob Agents Chemother. 2011;2015(59):3509–17.
Castanheira M, Mendes RE, Sader HS. Low frequency of ceftazidime-avibactam resistance among Enterobacteriaceae isolates carrying blaKPC Collected in US Hospitals from 2012 to 2015. Antimicrob Agents Chemother. 2017;61 (Epub 2016/12/30).
Humphries RM, Yang S, Hemarajata P, Ward KW, Hindler JA, Miller SA, Gregson A. First report of ceftazidime-avibactam resistance in a KPC-3-expressing Klebsiella pneumoniae isolate. Antimicrob Agents Chemother. 2015;59:6605–7.
Haidar G, Clancy CJ, Chen L, Samanta P, Shields RK, Kreiswirth BN, Nguyen MH. Identifying spectra of activity and therapeutic niches for ceftazidime-avibactam and imipenem-relebactam against carbapenem-resistant Enterobacteriaceae. Antimicrob Agents Chemother. 2017;61 (Epub 2017/06/21).
Krishnan NP, Nguyen NQ, Papp-Wallace KM, Bonomo RA, van den Akker F. Inhibition of Klebsiella beta-Lactamases (SHV-1 and KPC-2) by avibactam: a structural study. PLoS One. 2015;10:e0136813.
Aitken SL, Tarrand JJ, Deshpande LM, Tverdek FP, Jones AL, Shelburne SA, Prince RA, Bhatti MM, Rolston KVI, Jones RN, Castanheira M, Chemaly RF. High rates of nonsusceptibility to ceftazidime-avibactam and identification of New Delhi metallo-beta-lactamase production in enterobacteriaceae bloodstream infections at a major cancer center. Clin Infect Dis. 2016;63:954–8 Epub 2016/06/18.
Davido B, Fellous L, Lawrence C, Maxime V, Rottman M, Dinh A. Ceftazidime-Avibactam and aztreonam, an interesting strategy to overcome beta-lactam resistance conferred by metallo-beta-lactamases in Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2017;61 (Epub 2017/06/21).
Marshall S, Hujer AM, Rojas LJ, Papp-Wallace KM, Humphries RM, Spellberg B, Hujer KM, Marshall EK, Rudin SD, Perez F, Wilson BM, Wasserman RB, Chikowski L, Paterson DL, Vila AJ, van Duin D, Kreiswirth BN, Chambers HF, Fowler VG, Jr., Jacobs MR, Pulse ME, Weiss WJ, Bonomo RA. Can ceftazidime-avibactam and aztreonam overcome beta-lactam resistance conferred by metallo-beta-lactamases in Enterobacteriaceae? Antimicrob Agents Chemother. 2017;61 (Epub 2017/02/09).
Alm RA, Johnstone MR, Lahiri SD. Characterization of Escherichia coli NDM isolates with decreased susceptibility to aztreonam/avibactam: role of a novel insertion in PBP3. J Antimicrob Chemother. 2015;70:1420–8.
Wenzler E, Deraedt MF, Harrington AT, Danizger LH. Synergistic activity of ceftazidime-avibactam and aztreonam against serine and metallo-beta-lactamase-producing Gram-negative pathogens. Diagn Microbiol Infect Dis. 2017;88:352–4 Epub 2017/06/13.
Manning N, Balabanian G, Rose M, Landman D, Quale J. Activity of ceftazidime-avibactam against clinical isolates of Klebsiella pneumoniae, including KPC-carrying isolates, Endemic to New York City. Microb Drug Resist. 2017 (Epub 2017/06/08).
Both A, Buttner H, Huang J, Perbandt M, Belmar Campos C, Christner M, Maurer FP, Kluge S, Konig C, Aepfelbacher M, Wichmann D, Rohde H. Emergence of ceftazidime/avibactam non-susceptibility in an MDR Klebsiella pneumoniae isolate. J Antimicrob Chemother. 2017;72:2483–8 Epub 2017/06/24.
Porres-Osante N, Dupont H, Torres C, Ammenouche N, de Champs C, Mammeri H. Avibactam activity against extended-spectrum AmpC beta-lactamases. J Antimicrob Chemother. 2014;69:1715–6.
Lahiri SD, Giacobbe RA, Johnstone MR, Alm RA. Activity of avibactam against Enterobacter cloacae producing an extended-spectrum class C beta-lactamase enzyme. J Antimicrob Chemother. 2014;69:2942–6.
Lahiri SD, Johnstone MR, Ross PL, McLaughlin RE, Olivier NB, Alm RA. Avibactam and class C beta-lactamases: mechanism of inhibition, conservation of the binding pocket, and implications for resistance. Antimicrob Agents Chemother. 2014;58:5704–13.
Zhang Y, Kashikar A, Brown CA, Denys G, Bush K. Unusual Escherichia coli PBP 3 insertion sequence identified from a collection of carbapenem-resistant Enterobacteriaceae tested in vitro with a combination of ceftazidime-, ceftaroline-, or aztreonam-avibactam. Antimicrob Agents Chemother. 2017;61 (Epub 2017/06/01).
Compain F, Arthur M. Impaired inhibition by avibactam and resistance to the ceftazidime-avibactam combination due to the D179Y substitution in the KPC-2 beta-Lactamase. Antimicrob Agents Chemother. 2017;61 (Epub 2017/05/04).
Shields RK, Nguyen MH, Press EG, Chen L, Kreiswirth BN, Clancy CJ. In vitro selection of meropenem resistance among ceftazidime-avibactam-resistant, meropenem-susceptible Klebsiella pneumoniae isolates with variant KPC-3 carbapenemases. Antimicrob Agents Chemother. 2017;61 (Epub 2017/03/01).
Fernea A, Galleni M, Frere JM. Kinetics of the interaction between avibactam and the CHE-1 class C beta-lactamase. J Antimicrob Chemother. 2015;70:951–3.
Ehmann DE, Jahic H, Ross PL, Gu RF, Hu J, Durand-Reville TF, Lahiri S, Thresher J, Livchak S, Gao N, Palmer T, Walkup GK, Fisher SL. Kinetics of avibactam inhibition against Class A, C, and D beta-lactamases. J Biol Chem. 2013;288:27960–71.
Pages JM, Peslier S, Keating TA, Lavigne JP, Nichols WW. Role of the outer membrane and porins in susceptibility of beta-lactamase-producing Enterobacteriaceae to ceftazidime-avibactam. Antimicrob Agents Chemother. 2015;60:1349–59.
Shen Z, Ding B, Ye M, Wang P, Bi Y, Wu S, Xu X, Guo Q, Wang M. High ceftazidime hydrolysis activity and porin OmpK35 deficiency contribute to the decreased susceptibility to ceftazidime/avibactam in KPC-producing Klebsiella pneumoniae. J Antimicrob Chemother. 2017;72:1930–6 Epub 2017/03/24.
McLeod SM, Patey SA, Huband MD, Nichols WW. Impact of defined cell envelope mutations in Escherichia coli on the in vitro antibacterial activity of avibactam/beta-lactam combinations. Int J Antimicrob Agents. 2017;49:437–42 Epub 2017/03/01.
Flamm RK, Farrell DJ, Sader HS, Jones RN. Ceftazidime/avibactam activity tested against Gram-negative bacteria isolated from bloodstream, pneumonia, intra-abdominal and urinary tract infections in US medical centres (2012). J Antimicrob Chemother. 2014;69:1589–98.
Huband MD, Castanheira M, Flamm RK, Farrell DJ, Jones RN, Sader HS. in vitro activity of ceftazidime-avibactam against contemporary Pseudomonas aeruginosa isolates from US Medical Centers by Census Region, 2014. Antimicrob Agents Chemother. 2016;60:2537–41.
Walkty A, Adam H, Baxter M, Denisuik A, Lagace-Wiens P, Karlowsky JA, Hoban DJ, Zhanel GG. In vitro activity of plazomicin against 5015 gram-negative and gram-positive clinical isolates obtained from patients in canadian hospitals as part of the CANWARD study, 2011–2012. Antimicrob Agents Chemother. 2014;58:2554–63.
Winkler ML, Papp-Wallace KM, Hujer AM, Domitrovic TN, Hujer KM, Hurless KN, Tuohy M, Hall G, Bonomo RA. Unexpected challenges in treating multidrug-resistant Gram-negative bacteria: resistance to ceftazidime-avibactam in archived isolates of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2015;59:1020–9.
Chalhoub H, Tunney M, Elborn JS, Vergison A, Denis O, Plesiat P, Kahl BC, Van Bambeke F, Tulkens PM. Avibactam confers susceptibility to a large proportion of ceftazidime-resistant Pseudomonas aeruginosa isolates recovered from cystic fibrosis patients. J Antimicrob Chemother. 2015;70:1596–8.
Sader HS, Castanheira M, Mendes RE, Flamm RK, Farrell DJ, Jones RN. Ceftazidime-avibactam activity against multidrug-resistant Pseudomonas aeruginosa isolated in US medical centers in 2012 and 2013. Antimicrob Agents Chemother. 2015;59:3656–9.
Grupper M, Sutherland C, Nicolau DP. Multicenter evaluation of ceftazidime-avibactam and ceftolozane-tazobactam inhibitory activity against meropenem-nonsusceptible Pseudomonas aeruginosa from blood, respiratory tract, and wounds. Antimicrob Agents Chemother. 2017;61 (Epub 2017/07/26).
Alatoom A, Elsayed H, Lawlor K, AbdelWareth L, El-Lababidi R, Cardona L, Mooty M, Bonilla MF, Nusair A, Mirza I. Comparison of antimicrobial activity between ceftolozane-tazobactam and ceftazidime-avibactam against multidrug-resistant isolates of Escherichia coli, Klebsiella pneumoniae, and Pseudomonas aeruginosa. Int J Infect Dis. 2017;62:39–43 Epub 2017/06/15.
Fraile-Ribot PA, Mulet X, Cabot G, Del Barrio-Tofino E, Juan C, Perez JL, Oliver A. In vivo emergence of resistance to novel cephalosporin-beta-lactamase inhibitor combinations through the duplication of amino acid D149 from OXA-2 beta-Lactamase (OXA-539) in sequence type 235 Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2017;61 (Epub 2017/07/05).
Papp-Wallace KM, Becka SA, Zeiser ET, Ohuchi N, Mojica MF, Gatta JA, Falleni M, Tosi D, Borghi E, Winkler ML, Wilson BM, LiPuma JJ, Nukaga M, Bonomo RA. Overcoming an extreme drug resistant (XDR) pathogen: avibactam restores susceptibility to ceftazidime for Burkholderia cepacia complex isolates from Cystic Fibrosis patients. ACS Infect Dis. 2017.
Everaert AC. T. Effect of β-Lactamase inhibitors on in vitro activity of β-Lactam antibiotics against Burkholderia cepacia complex species. Antimicrob Resist. Infect Control. 2017;16:1.
Curcio D. Activity of a novel combination against multidrug-resistant nonfermenters: ceftazidime plus NXL104. Expert Rev Anti Infect Ther. 2011;9:173–6.
Aktas Z, Kayacan C, Oncul O. In vitro activity of avibactam (NXL104) in combination with beta-lactams against Gram-negative bacteria, including OXA-48 beta-lactamase-producing Klebsiella pneumoniae. Int J Antimicrob Agents. 2012;39:86–9.
Levasseur P, Girard AM, Claudon M, Goossens H, Black MT, Coleman K, Miossec C. In vitro antibacterial activity of the ceftazidime-avibactam (NXL104) combination against Pseudomonas aeruginosa clinical isolates. Antimicrob Agents Chemother. 2012;56:1606–8.
Lahiri SD, Walkup GK, Whiteaker JD, Palmer T, McCormack K, Tanudra MA, Nash TJ, Thresher J, Johnstone MR, Hajec L, Livchak S, McLaughlin RE, Alm RA. Selection and molecular characterization of ceftazidime/avibactam-resistant mutants in Pseudomonas aeruginosa strains containing derepressed AmpC. J Antimicrob Chemother. 2015;70:1650–8.
Buehrle DJ, Shields RK, Chen L, Hao B, Press EG, Alkrouk A, Potoski BA, Kreiswirth BN, Clancy CJ, Nguyen MH. Evaluation of the in vitro activity of ceftazidime-avibactam and ceftolozane-tazobactam against meropenem-resistant Pseudomonas aeruginosa isolates. Antimicrob Agents Chemother. 2016;60:3227–31.
Livermore DM, Mushtaq S, Warner M, Zhang JC, Maharjan S, Doumith M, Woodford N. Activity of aminoglycosides, including ACHN-490, against carbapenem-resistant Enterobacteriaceae isolates. J Antimicrob Chemother. 2011;66:48–53.
Rasmussen BA, Bush K, Tally FP. Antimicrobial resistance in anaerobes. Clin Infect Dis. 1997;24(Suppl 1):S110–20 Epub 1997/01/01.
Hedberg M, Nord CE. Beta-lactam resistance in anaerobic bacteria: a review. J Chemother. 1996;8:3–16 Epub 1996/02/01.
Citron DM, Tyrrell KL, Merriam V, Goldstein EJ. In vitro activity of ceftazidime-NXL104 against 396 strains of beta-lactamase-producing anaerobes. Antimicrob Agents Chemother. 2011;55:3616–20.
Dubreuil LJ, Mahieux S, Neut C, Miossec C, Pace J. Anti-anaerobic activity of a new beta-lactamase inhibitor NXL104 in combination with beta-lactams and metronidazole. Int J Antimicrob Agents. 2012;39:500–4.
Goldstein EJ, Citron DM, Merriam CV, Tyrrell KL. Comparative in vitro activity of ceftaroline, ceftaroline-avibactam, and other antimicrobial agents against aerobic and anaerobic bacteria cultured from infected diabetic foot wounds. Diagn Microbiol Infect Dis. 2013;76:347–51.
Dubee V, Bernut A, Cortes M, Lesne T, Dorchene D, Lefebvre AL, Hugonnet JE, Gutmann L, Mainardi JL, Herrmann JL, Gaillard JL, Kremer L, Arthur M. beta-Lactamase inhibition by avibactam in Mycobacterium abscessus. J Antimicrob Chemother. 2015;70:1051–8.
Lefebvre AL, Le Moigne V, Bernut A, Veckerle C, Compain F, Herrmann JL, Kremer L, Arthur M, Mainardi JL. Inhibition of the beta-lactamase BlaMab by avibactam improves the in vitro and in vivo efficacy of imipenem against Mycobacterium abscessus. Antimicrob Agents Chemother. 2017;61 (Epub 2017/01/18).
Soroka D, Ourghanlian C, Compain F, Fichini M, Dubée V, Mainardi JL, Hugonnet JE, Arthur M. Inhibition of β-lactamases of mycobacteria by avibactam and clavulanate. J Antimicrob Chemother. 2017;72:1081–8.
Ourghanlian C, Soroka D, Arthur M. Inhibition by avibactam and clavulanate of the beta-lactamases KPC-2 and CTX-M-15 harboring the substitution N132G in the conserved SDN Motif. Antimicrob Agents Chemother. 2017;61 (Epub 2017/01/11).
Vishwanathan K, Mair S, Gupta A, Atherton J, Clarkson-Jones J, Edeki T, Das S. Assessment of the mass balance recovery and metabolite profile of avibactam in humans and in vitro drug–drug interaction potential. Drug Metab Dispos. 2014;42:932–42.
Wenzler E, Bunnell KL, Bleasdale SC, Benken S, Danziger LH, Rodvold KA. Pharmacokinetics and dialytic clearance of ceftazidime-avibactam in a critically ill patient on continuous venovenous hemofiltration. Antimicrob Agents Chemother. 2017;61 (Epub 2017/04/19).
Tarral A, Merdjan H. Effect of age and sex on the pharmacokinetics and safety of avibactam in healthy volunteers. Clin Ther. 2015;37:877–86.
Merdjan H, Rangaraju M, Tarral A. Safety and pharmacokinetics of single and multiple ascending doses of avibactam alone and in combination with ceftazidime in healthy male volunteers: results of two randomized, placebo-controlled studies. Clin Drug Investig. 2015;35:307–17.
Merdjan H, Tarral A, Das S, Li J. Phase 1 study assessing the pharmacokinetic profile and safety of avibactam in patients with renal impairment. J Clin Pharmacol. 2017;57:211–8.
Veillette JJ, Truong J, Forland SC. Pharmacokinetics of ceftazidime-avibactam in two patients with KPC-producing Klebsiella pneumoniae Bacteremia and renal impairment. Pharmacotherapy. 2016;36:172–7.
Nicolau DP, Siew L, Armstrong J, Li J, Edeki T, Learoyd M, Das S. Phase 1 study assessing the steady-state concentration of ceftazidime and avibactam in plasma and epithelial lining fluid following two dosing regimens. J Antimicrob Chemother. 2015;70:2862–9.
Bensman TJ, Wang J, Jayne J, Fukushima L, Rao AP, D’Argenio DZ, Beringer PM. Pharmacokinetic–pharmacodynamic target attainment analyses to determine optimal dosing of ceftazidime-avibactam for the treatment of acute pulmonary exacerbations in patients with cystic fibrosis. Antimicrob Agents Chemother. 2017;61 (Epub 2017/08/09).
Meyer K, Santarossa M, Danziger LH, Wenzler E. Compatibility of ceftazidime-avibactam, ceftolozane-tazobactam, and piperacillin-tazobactam with vancomycin in dextrose 5% in water. Hosp Pharm. 2017;52:221–8 Epub 2017/04/26.
Coleman K, Levasseur P, Girard AM, Borgonovi M, Miossec C, Merdjan H, Drusano G, Shlaes D, Nichols WW. Activities of ceftazidime and avibactam against beta-lactamase-producing Enterobacteriaceae in a hollow-fiber pharmacodynamic model. Antimicrob Agents Chemother. 2014;58:3366–72.
Dallow J, Otterson LG, Huband MD, Krause KM, Nichols WW. Microbiological interaction studies between ceftazidime-avibactam and pulmonary surfactant and between ceftazidime-avibactam and antibacterial agents of other classes. Int J Antimicrob Agents. 2014;44:552–6.
MacGowan A, Tomaselli S, Noel A. K. B. The pharmacodynamics of avibactam in combination with ceftaroline or ceftazidime against β-lactamase-producing Enterobacteriaceae studied in an in vitro model of infection. J Antimicrob Chemother. 2017;72:762–9.
Goh JH, Lee SY, Ooi ST, Lee Soon UL, Hee KH, Renaud CJ. Post-hemodialysis dosing of 1 vs. 2 g of ceftazidime in anuric end-stage renal disease patients on low-flux dialysis and its pharmacodynamic implications on clinical use. Hemodial Int. 2016;20:253–60.
Buyck JM, Luyckx C, Muccioli GG, Krause KM, Nichols WW, Tulkens PM, Van Bambeke F. Pharmacodynamics of ceftazidime/avibactam against extracellular and intracellular forms of Pseudomonas aeruginosa. J Antimicrob Chemother. 2017;72:1400–9 Epub 2017/02/01.
Sy SK, Zhuang L, Beaudoin ME, Kircher P, Tabosa MA, Cavalcanti NC, Grunwitz C, Pieper S, Schuck VJ, Nichols WW, Derendorf H. Potentiation of ceftazidime by avibactam against beta-lactam-resistant Pseudomonas aeruginosa in an in vitro infection model. J Antimicrob Chemother. 2017;72:1109–17 Epub 2017/01/13.
Pillar CM, Stoneburner A, Shinabarger DL, Krause KM, Nichols WW. The postantibiotic effect and post-beta-lactamase-inhibitor effect of ceftazidime, ceftaroline and aztreonam in combination with avibactam against target Gram-negative bacteria. Lett Appl Microbiol. 2016;63:96–102 Epub 2016/05/26.
Keepers TR, Gomez M, Celeri C, Nichols WW, Krause KM. Bactericidal activity, absence of serum effect, and time-kill kinetics of ceftazidime-avibactam against beta-lactamase-producing Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2014;58:5297–305.
Endimiani A, Hujer KM, Hujer AM, Pulse ME, Weiss WJ, Bonomo RA. Evaluation of ceftazidime and NXL104 in two murine models of infection due to KPC-producing Klebsiella pneumoniae. Antimicrob Agents Chemother. 2011;55:82–5.
Wiskirchen DE, Crandon JL, Furtado GH, Williams G, Nicolau DP. In vivo efficacy of a human-simulated regimen of ceftaroline combined with NXL104 against extended-spectrum-beta-lactamase (ESBL)-producing and non-ESBL-producing Enterobacteriaceae. Antimicrob Agents Chemother. 2011;55:3220–5.
Crandon JL, Nicolau DP. Human simulated studies of aztreonam and aztreonam-avibactam to evaluate activity against challenging Gram-negative organisms, including metallo-beta-lactamase producers. Antimicrob Agents Chemother. 2013;57:3299–306.
Crandon JL, Schuck VJ, Banevicius MA, Beaudoin ME, Nichols WW, Tanudra MA, Nicolau DP. Comparative in vitro and in vivo efficacies of human simulated doses of ceftazidime and ceftazidime-avibactam against Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2012;56:6137–46.
Monogue ML, Abbo LM, Rosa R, Camargo JF, Martinez O, Bonomo RA, Nicolau DP. In vitro discordance with in vivo activity: humanized exposures of ceftazidime-avibactam, aztreonam, and tigecycline alone and in combination against New Delhi metallo-beta-lactamase-producing Klebsiella pneumoniae in a Murine lung infection model. Antimicrob Agents Chemother. 2017;61 (Epub 2017/04/19).
Housman ST, Crandon JL, Nichols WW, Nicolau DP. Efficacies of ceftazidime-avibactam and ceftazidime against Pseudomonas aeruginosa in a murine lung infection model. Antimicrob Agents Chemother. 2014;58:1365–71.
Rashid MU, Rosenborg S, Panagiotidis G, Lofdal KS, Weintraub A, Nord CE. Ecological effect of ceftazidime/avibactam on the normal human intestinal microbiota. Int J Antimicrob Agents. 2015;46:60–5.
Mendes RE, Castanheira M, Woosley LN, Stone GG, Bradford PA, Flamm RK. Molecular beta-lactamase characterization of aerobic Gram-negative pathogens recovered from patients enrolled in the ceftazidime-avibactam phase 3 trials for complicated intra-abdominal infections, with efficacies analyzed against susceptible and resistant subsets. Antimicrob Agents Chemother. 2017;61 (Epub 2017/03/30).
Wagenlehner FM, Sobel JD, Newell P, Armstrong J, Huang X, Stone GG, Yates K, Gasink LB. Ceftazidime-avibactam versus doripenem for the treatment of complicated urinary tract infections, including acute pyelonephritis: RECAPTURE, a phase 3 randomized trial program. Clin Infect Dis. 2016;63:754–62 Epub 2016/06/18.
Stone GG, Bradford PA, Newell P, Wardman A. In vitro activity of ceftazidime-avibactam against isolates in a phase 3 open-label clinical trial for complicated intra-abdominal and urinary tract infections caused by ceftazidime-nonsusceptible Gram-negative pathogens. Antimicrob Agents Chemother. 2017;61 (Epub 2016/11/23).
Bradley JS, Armstrong J, Arrieta A, Bishai R, Das S, Delair S, Edeki T, Holmes WC, Li J, Moffett KS, Mukundan D, Perez N, Romero JR, Speicher D, Sullivan JE, Zhou D. Phase I study assessing the pharmacokinetic profile, safety, and tolerability of a single dose of ceftazidime-avibactam in hospitalized pediatric patients. Antimicrob Agents Chemother. 2016;60:6252–9 Epub 2016/08/10.
van Duin D, Bonomo RA. Ceftazidime/avibactam and ceftolozane/tazobactam: second-generation beta-lactam/beta-lactamase inhibitor combinations. Clin Infect Dis. 2016;63:234–41.
Shields RK, Nguyen MH, Chen L, Press EG, Potoski BA, Marini RV, Doi Y, Kreiswirth BN, Clancy CJ. Ceftazidime-avibactam is superior to other treatment regimens against carbapenem-resistant Klebsiella pneumoniae Bacteremia. Antimicrob Agents Chemother. 2017;61 (Epub 2017/06/01).
King M, Heil E, Kuriakose S, Bias T, Huang V, El-Beyrouty C, McCoy D, Hiles J, Richards L, Gardner J, Harrington N, Biason K, Gallagher JC. Multicenter Study of outcomes with ceftazidime-avibactam in patients with carbapenem-resistant Enterobacteriaceae infections. Antimicrob Agents Chemother. 2017;61 (Epub 2017/05/10).
Caston JJ, Lacort-Peralta I, Martin-Davila P, Loeches B, Tabares S, Temkin L, Torre-Cisneros J, Pano-Pardo JR. Clinical efficacy of ceftazidime/avibactam versus other active agents for the treatment of bacteremia due to carbapenemase-producing Enterobacteriaceae in hematologic patients. Int J Infect Dis. 2017;59:118–23 Epub 2017/04/11.
Krapp F, Grant JL, Sutton SH, Ozer EA, Barr VO. Treating complicated carbapenem-resistant enterobacteriaceae infections with ceftazidime/avibactam: a retrospective study with molecular strain characterisation. Int J Antimicrob Agents. 2017;49:770–3 Epub 2017/04/09.
Satlin MJ, Chen L, Patel G, Gomez-Simmonds A, Weston G, Kim AC, Seo SK, Rosenthal ME, Sperber SJ, Jenkins SG, Hamula CL, Uhlemann AC, Levi MH, Fries BC, Tang YW, Juretschko S, Rojtman AD, Hong T, Mathema B, Jacobs MR, Walsh TJ, Bonomo RA, Kreiswirth BN. multicenter clinical and molecular epidemiological analysis of bacteremia due to carbapenem-resistant Enterobacteriaceae (CRE) in the CRE epicenter of the United States. Antimicrob Agents Chemother. 2017;61 (Epub 2017/02/09).
Temkin E, Torre-Cisneros J, Beovic B, Benito N, Giannella M, Gilarranz R, Jeremiah C, Loeches B, Machuca I, Jiménez-Martín M, Martínez JA, Mora-Rillo M, Navas E, Osthoff M, Pozo JC, Ramos Ramos JC, Rodriguez M, Sánchez-García M, Viale P, Wolff M, Carmeli Y. Ceftazidime-avibactam as salvage therapy for infections caused by carbapenem-resistant organisms. Antimicrob Agents Chemother. 2017;61:1916–64.
Shields RK, Potoski BA, Haidar G, Hao B, Doi Y, Chen L, Press EG, Kreiswirth BN, Clancy CJ, Nguyen MH. Clinical outcomes, drug toxicity, and emergence of ceftazidime-avibactam resistance among patients treated for carbapenem-resistant Enterobacteriaceae infections. Clin Infect Dis. 2016;63:1615–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FFT and JLR received grants from Astra-Zeneca. Marcelo R. Formigoni-Pinto works in the medical scientific division of Astra-Zeneca.
Rights and permissions
About this article
Cite this article
Tuon, F.F., Rocha, J.L. & Formigoni-Pinto, M.R. Pharmacological aspects and spectrum of action of ceftazidime–avibactam: a systematic review. Infection 46, 165–181 (2018). https://doi.org/10.1007/s15010-017-1096-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-017-1096-y