Abstract
Introduction
Changes in the epidemiology of Staphylococcus aureus bacteremia (SAB) have been described in recent decades. Decreased mortality has been reported over time, mostly from countries with low methicillin resistance rates. We aimed to describe time trends in SAB in a tertiary center with high methicillin resistance rates.
Methods
We retrospectively analyzed 1692 patients with SAB, and compared between three time periods: 1988–1994 (342 patients), 1998–2004 (597 patients) and 2005–2010 (753 patients).
Results
In our cohort, 30 days mortality increased significantly with time, reaching 42.9 % during 2005–2010. The latter period was characterized by higher rates of older patients (35.1 % aged 80 years and older), with lower functional capacity (46.5 % bedridden) and higher rates of comorbidities (33.6 % renal disease, 24.8 % heart failure, 19.0 % dementia). These patients were more likely to be ventilated (18.7 %) and carry a urinary catheter at presentation (46.6 %); present with septic shock (15.9 %) and have pneumonia (20.5 %) or endocarditis (7.2 %) as source. Similar characteristics were found among patients younger than 50 years and with independent functional status. No significant increase in methicillin resistant Staph aureus (MRSA) rates or inappropriate empirical therapy was demonstrated during 2005–2010.
Conclusions
In our cohort, increased mortality in recent years in patients with SAB can be explained by baseline condition of patients. MRSA or inappropriate empiric therapy did not explain the increase in mortality. The patients afflicted with SAB changed over time. Epidemiology and outcomes of SAB vary with time and according to geographical location. External validity of studies should be taken into consideration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Staphylococcus aureus (S. aureus) is a leading cause of bacteremia. The annual incidence of S. aureus bacteremia (SAB) in the United States is 4–38 per 100,000 person-years, with 30-day all-cause mortality of ~20 % [1, 2].
During the last decades, several changes in the epidemiology of SAB were described. In Denmark the incidence of SAB increased between 1957 and 1990. However, since 1990 the overall SAB incidence has been relatively stable [3, 4]. In the early 2000s the incidence of methicillin resistant S. aureus (MRSA) in USA raised dramatically, while in the last few years, hospital onset MRSA incidence is declining [5, 6].
The incidence of SAB is higher in older patients (>100 per 100,000 person-years among subjects >70 years of age), men (male–female ration ~1.5) and hemodialysis patients. Common primary sources of infection include vascular catheters, skin and soft tissue, pleuropulmonary, osteoarticular and endocarditis [7].
Mortality of SAB is reported to have either plateaued over the past few decades [7] or (in most reports) declined [4, 8, 9]. Explanations given to the possible plateau in mortality rates in a recent review include the larger numbers of older and sicker patients among SAB patients and the relative plateau in antibiotic efficacy [7]. Mejer et al. demonstrated increase in Charlson comorbidity score and the proportion of older patients among SAB patients during a 14 years period [4].
We aimed to describe time trends in SAB cases in our hospital in a cohort of hospitalized patients starting 1988 and up to end of 2010. We planned to explore the impact of recent years’ improved medical care on one hand, along with ageing of the population, increasing rate of invasive procedures, accumulation of comorbidities and increased health care/hospital acquired infections, on outcomes of SAB.
Methods
Data collection
The study was conducted at Rabin Medical Center, Beilinson Hospital, a 900-bed primary and tertiary care university hospital. The hospital has four main intensive care units (ICUs) and six small ICUs in which patients undergo mechanical ventilation within the six internal medicine and two surgical departments.
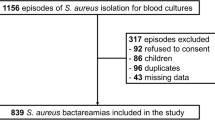
All consecutive adult patients who had been diagnosed with S. aureus bacteremia were identified. Data were collected retrospectively between January 1, 1999, and December 31, 2010, by reviewing patients’ medical records and were merged with data prospectively collected between April 1, 1988, and September 30, 1994. Results from earlier years collected in these databases have been previously described [10, 11]. The study was approved by the local research ethics committee.
Contaminants (S. aureus isolated in a single set of blood cultures with no evidence of systemic inflammatory response syndrome within 48 h of blood culture, in which the patient was not treated and did not die within 30 days) were excluded. Patients were included only once, for the first episode of S. aureus bacteremia. Patients were included up until October 2010.
Microbiology
Two separate sets of blood cultures were obtained routinely (up to six sets if endocarditis was suspected), with 10 mL of blood collected in one aerobic and one anaerobic bottle. The Bactec 460 was used between 1988 and 1992 and the Bactec 9240 microbial system (Becton–Dickinson, Franklin Lakes, NJ) after 1992. Isolates were identified on the basis of morphologic features and API system. Susceptibility to antibiotics was tested by the disk diffusion method on Mueller–Hinton agar, according to Clinical and Laboratory Standards Institute (CLSI) procedures. Repeated blood cultures were obtained until results were negative.
Definitions
Health care associated infections were defined as any of the followings: previous hospitalization of ≥2 days during previous 90 days; clinic visit during previous 30 days; Home IV therapy or chemotherapy or wound treatment during previous 30 days; or patients arriving from long term care facilities. Hospital acquired infections were defined as presentation of infection after >48 h of hospitalization. Other infections were considered community acquired. Central line associated infections were defined as any SAB without an obvious source other than the catheter and if catheter was removed—positive culture of the catheter tip. An infectious diseases expert determined the source of infection per each episode. Appropriate empirical antibiotic treatment was defined as matching in vitro susceptibility of the S. aureus isolate and given within 48 h after obtaining blood culture, except for single use of aminoglycoside or rifampicin treatment.
Statistical analysis
Categorical variables were compared using the Chi-square test for trends, including the Chi square for linear trends where appropriate; continuous variables by the t test (for normal distribution) or the Mann–Whitney U test (for other distributions). Analyses were performed using the Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA).
We compared three periods: 1988–1994; 1998–2004; 2005–2010. Data concerning management of infection are missing for the first time period.
Results
We included in the analysis 1692 patients: 342 patients during 1988–1994; 597 patients during 1998–2004 and 753 patients during 2005–2010. In the first period, 122 (35.7 %) patients died within 30 days, in the second period—229 (38.4 %) and in the third period—523 (42.9 %), P = 0.016.
Differences between patients’ characteristics, infection characteristics, management and outcomes in the various time periods are presented in Table 1.
Median age was significantly lower in the first time period. Although no significant difference in median age was demonstrated between second and third periods, percentages of patients aged 80 years and older significantly increased with time (21.6 % of patients in 1988–1994; 30.3 % in 1998–2004 and 35.1 % in 2005–2010). Percentage of patients with renal failure, liver disease, congestive heart failure, dementia and bedridden state significantly increased with time. Patients in the third period were significantly more likely to be ventilated, carry a urinary catheter, present with septic shock and have pneumonia or endocarditis as the source of infection. MRSA infection but also inappropriate empiric therapy were significantly less common in the first time period, but there were no significant differences between the second and the third periods. Full management data were not available for first time period. In the third period, patients were significantly more likely to get infectious diseases consultation and be hospitalized in intensive care unit (ICU) (Table 1).
Resistance patterns of isolates during the years (Table 2)
Among all S. aureus isolates and among MRSA isolates specifically, resistance to rifampin and gentamicin declined significantly in the third period and resistance to tetracycline decreased significantly with time. Resistance to trimethoprim-sulfamethoxazole declined significantly between first period and later periods and resistance to ofloxacin increased at the same time. Among MRSA isolates, resistance to clindamycin increased non-significantly with time.
30 days mortality among young patients (Tables 3, 4)
We examined mortality in four age groups: age <50 years, 50–64, 65–79, ≥80. In each group, mortality was non-significantly higher in the third time period (Table 3). Patients’ and infection characteristics of patients aged <50 over time are presented in Table 4. In the third period these younger patients had higher McCabe score, were more likely to be ventilated and carry a urinary catheter at presentation, more likely to present with septic shock and be hospitalized in ICU, and have as a source pneumonia or endocarditis (Table 4). No significant increase was demonstrated in MRSA rates with time in this group of young patients and rates of appropriate treatment did not decline with time.
Mortality in other age groups was above 25 % in all time periods, reaching 60 % among 264 patients ≥80 years in the third time period (Table 3).
30 days mortality among patients with independent functional capacity (Table 5)
Patients with independent functional capacity were similarly to young patients “sicker” in the third period—with higher comorbidity score, higher rates of urinary catheter at presentation, septic shock and higher rates of pneumonia or endocarditis and as a source (Table 5).
No significant increase was demonstrated in MRSA rates among patients with independent functional capacity with time and rates of appropriate treatment did not decline with time.
Discussion
In our cohort of 1692 patients with SAB, we found significant increase in 30 days mortality during 2005–2010 compared with 1998–2004 and previous years. This increased mortality is probably explained by the characteristics of patients during 2005–2010. Patients in this period were “sicker”—they had higher comorbidity rates, lower functional capacity and were more likely to be ventilated and carry a urinary catheter at infection presentation. They had more severe infection—higher rates of presentation with septic shock and higher rates of pneumonia or endocarditis as the source of the infection. These differences were also demonstrated in patients aged <50 years and patients with independent functional capacity, similar to the entire cohort. The increase in mortality with time was not explained by MRSA rates or inappropriate empiric therapy. No significant difference was demonstrated in neither MRSA rates not inappropriate therapy rates between the second and third periods. Such differences were also not demonstrated among younger and patients with independent functional capacity. We did not find other differences in patients’ management that could explain the mortality difference.
Our results concerning mortality are in contrast to recent studies reporting decreased mortality in recent years among patients with SAB. These include Allard et al., reporting decrease in 30 days mortality from 29 % in 1997–1999 to 18 % in 2003–2005 in Canada [12]; Asgeirsson et al., reporting a decrease from 25 % in 1995–1996 to 8.2 % in 2007–2008 in Iceland [8]; Benfield et al., reporting a decrease from 34.5 to 21.7 % from 1981 to 2000 in Denmark [9]; and Mejer et al., reporting a significant decrease in 30 days mortality, mainly in hospital acquired SAB from 1995 to 2008 in Denmark [4]. It should be noted that most of these cohorts are from Scandinavian countries, known for their low rates of MRSA infections. Asgeirsson et al. described only four cases of MRSA during 1995–2008. Similarly, Benfield et al. reported MRSA in 0.3 % of bacteremias and Mejer et al. in less than 1 % [4, 8, 9].
The reduction in mortality over time in previous studies was largest in the youngest age group [8, 9]. In our study, non-significantly increased mortality with time was demonstrated in patients younger than 50 years. In addition, rates of patients aged 80 and older were higher over time and compared to other studies [9].
In contrast to the non-significant difference in rates of MRSA bacteremia during 2005–2010 vs. 1998–2004 in our cohort, Allard et al. demonstrated a significant increase in MRSA from few cases in 1991–1999 to 10 % in 2000–2002 and 20 % in 2003–2005 [12]. Other studies demonstrated a decline in bacteremias of hospital onset MRSA in the last few years. Community acquired MRSA rates varied dramatically across diverse geographical areas [5, 6].
In accordance to our findings, Mejer et al. demonstrated an increase in Charlson comorbidity score among SAB patients during a 14-year period [4]. Allard et al. reported that between 1991–1993 and 2003–2005, the proportion of cases attributed to endocarditis and pneumonia increased significantly, while that attributed to catheter infections decreased [12].
The vast majority of the bacteremias (>88 %) in our cohort were hospital or health care associated. The rates of these infections increased significantly since the first time period, but not from the second to the third period. Asgeirsson et al. reported a significant increase in community-acquired (CA) SAB from 1995–1999 to 2005–2008, with rates of above 35 %, much higher than in our cohort [8]. Benfield et al. also demonstrated increased annual rates of community-acquired SAB from 1981 to 2000, with overall 28 % of cases acquired in the community [9]. The differences in rates of CA SAB between our cohort and others may stem from variability in the definitions of hospital, health care associated or community acquired infection [13].
Risk factors for mortality in our cohort were similar over time and compared to previous studies [8, 9, 12].
We demonstrated changes in antibiotic susceptibility with time. These changes were previously reported, including increase in susceptibility to trimethoprim–sulfamethoxazole [14], tetracycline [15], gentamicin and rifampin [16]. The increase in susceptibility has previously been explained by reduced usage of the relevant antibiotics [14] and spread of susceptible strains [15, 16].
This study has several limitations. First, it is a single center retrospective study. Second, during the study we did not perform routine molecular tests on SAB isolates, thus, we do not have data on SCC type, spa typing, MecA positivity or other specific features of S. aureus.
In conclusion, in our cohort, patients with SAB in recent compared to previous years were older and sicker, had higher rates of pneumonia and septic shock at presentation and consequently had higher 30 days mortality. Nowadays patients with SAB in our institution are a different population than 20 years ago. Epidemiology and outcomes of SAB vary in time and according to the geographical location, and external validity of studies should be taken into consideration.
References
Holland TL, Arnold C, Fowler VG Jr. Clinical management of Staphylococcus aureus bacteremia: a review. JAMA. 2014;312:1330–41.
van Hal SJ, Jensen SO, Vaska VL, Espedido BA, Paterson DL, Gosbell IB. Predictors of mortality in Staphylococcus aureus bacteremia. Clin Microbiol Rev. 2012;25:362–86.
Frimodt-Moller N, Espersen F, Skinhoj P, Rosdahl VT. Epidemiology of Staphylococcus aureus bacteremia in Denmark from 1957 to 1990. Clin Microbiol Infect. 1997;3:297–305.
Mejer N, Westh H, Schonheyder HC, Jensen AG, Larsen AR, Skov R, et al. Stable incidence and continued improvement in short term mortality of Staphylococcus aureus bacteraemia between 1995 and 2008. BMC Infect Dis. 2012;12:260.
David MZ, Daum RS, Bayer AS, Chambers HF, Fowler VG Jr, Miller LG, et al. Staphylococcus aureus bacteremia at 5 US academic medical centers, 2008–2011: significant geographic variation in community-onset infections. Clin Infect Dis. 2014;59:798–807.
Rhee Y, Aroutcheva A, Hota B, Weinstein RA, Popovich KJ. Evolving epidemiology of Staphylococcus aureus bacteremia. Infect Control Hosp Epidemiol. 2015;36:1417–22.
Tong SY, Davis JS, Eichenberger E, Holland TL, Fowler VG Jr. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev. 2015;28:603–61.
Asgeirsson H, Gudlaugsson O, Kristinsson KG, Heiddal S, Kristjansson M. Staphylococcus aureus bacteraemia in Iceland, 1995–2008: changing incidence and mortality. Clin Microbiol Infect. 2011;17:513–8.
Benfield T, Espersen F, Frimodt-Moller N, Jensen AG, Larsen AR, Pallesen LV, et al. Increasing incidence but decreasing in-hospital mortality of adult Staphylococcus aureus bacteraemia between 1981 and 2000. Clin Microbiol Infect. 2007;13:257–63.
Paul M, Kariv G, Goldberg E, Raskin M, Shaked H, Hazzan R, et al. Importance of appropriate empirical antibiotic therapy for methicillin-resistant Staphylococcus aureus bacteraemia. J Antimicrob Chemother. 2010;65:2658–65.
Paul M, Zemer-Wassercug N, Talker O, Lishtzinsky Y, Lev B, Samra Z, et al. Are all beta-lactams similarly effective in the treatment of methicillin-sensitive Staphylococcus aureus bacteraemia? Clin Microbiol Infect. 2011;17:1581–6.
Allard C, Carignan A, Bergevin M, Boulais I, Tremblay V, Robichaud P, et al. Secular changes in incidence and mortality associated with Staphylococcus aureus bacteraemia in Quebec, Canada, 1991–2005. Clin Microbiol Infect. 2008;14:421–8.
Smit J, Sogaard M, Schonheyder HC, Nielsen H, Thomsen RW. Classification of healthcare-associated Staphylococcus aureus bacteremia: influence of different definitions on prevalence, patient characteristics, and outcome. Infect Control Hosp Epidemiol. 2016;37(2):208–11.
Bishara J, Pitlik S, Samra Z, Levy I, Paul M, Leibovici L. Co-trimoxazole-sensitive, methicillin-resistant Staphylococcus aureus, Israel, 1988–1997. Emerg Infect Dis. 2003;9:1168–9.
Trzcinski K, Cooper BS, Hryniewicz W, Dowson CG. Expression of resistance to tetracyclines in strains of methicillin-resistant Staphylococcus aureus. J Antimicrob Chemother. 2000;45:763–70.
Aubry-Damon H, Legrand P, Brun-Buisson C, Astier A, Soussy CJ, Leclercq R. Reemergence of gentamicin-susceptible strains of methicillin-resistant Staphylococcus aureus: roles of an infection control program and changes in aminoglycoside use. Clin Infect Dis. 1997;25:647–53.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
None.
Conflict of interest
All authors declare none.
Rights and permissions
About this article
Cite this article
Yahav, D., Shaked, H., Goldberg, E. et al. Time trends in Staphylococcus aureus bacteremia, 1988–2010, in a tertiary center with high methicillin resistance rates. Infection 45, 51–57 (2017). https://doi.org/10.1007/s15010-016-0919-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-016-0919-6