Abstract
Background
Strongyloides stercoralis may lead to overwhelming infestation [Strongyloides hyperinfection syndrome (SHS)]. We aimed at describing a case series of patients admitted in intensive care unit (ICU) with SHS and report a literature review of such cases.
Patients and methods
Retrospective multicenter study of 11 patients admitted to the ICU of tertiary hospitals with SHS between 2000 and 2013. Literature review with Pubmed retrieved 122 cases. Logistic regression analysis was performed to identify predictive factors of ICU mortality and shock occurrence.
Results
133 patients [median age 53 (39, 64), 72.2 % males] were included. Underlying immunosuppression was present in 127 patients, mostly long-term corticosteroid treatment in 111 (83.5 %) patients. Fever (80.8 %), respiratory (88.6 %), and gastrointestinal (71.2 %) symptoms were common clinical manifestations. Shock occurred in 75 (57.3 %) patients and mechanical ventilation was required in 89 (67.9 %) patients. Hypereosinophilia and a concomitant bacterial infection were observed in 34 (34.3 %) and 51 (38.4 %) patients, respectively. The in-ICU mortality rate was 60.3 %. Predictive factors of ICU mortality were shock occurrence [Odds ratio (OR) 18.1, 95 % confidence interval (95 % CI) 3.03–107.6, p < 0.01] and mechanical ventilation (OR 28.1, 95 % CI 3.6–217, p < 0.01). Hypereosinophilia (OR 0.21, 95 % CI 0.06–0.7, p = 0.01) and a concomitant bacterial infection (OR 4.68, 95 % CI 1.3–16.8, p = 0.02) were independent predictors of shock occurrence.
Conclusion
SHS remains associated with a poor outcome, especially when associated with shock and mechanical ventilation. Deterioration to shock is often related to concomitant bacterial infection. The poor outcome of established SHS pleads for a large application of antiparasitic primary prophylaxis in at-risk patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Strongyloidiasis encompasses various disorders caused by a soil dwelling nematode helminth, Strongyloides stercoralis. It occurs in about 30 million people in 70 countries worldwide [1–3]. It is more frequently observed in endemic tropical and subtropical zones including the southern United States of America, but it can be observed as well in non-endemic areas such as European countries. Besides the common gastrointestinal presentation with diarrhea, two characteristic clinical syndromes of acute infection and hyperinfection syndrome have been described. Acute infection, also known as Loeffler’s syndrome, is caused by larval invasion and migration and is characterized by cutaneous manifestations such as serpiginous urticarial rash, cough, dyspnea, and gastrointestinal symptoms. Strongyloides hyperinfection syndrome (SHS) [4–7] was first described in 1970 and is related to disseminated infection with multiple organ involvement [8]. SHS is caused by massive intestinal invasion by a high load of parasites, which reach pulmonary circulation and perforate alveolar membrane leading to alveolar damage and acute respiratory failure [4]. The incidence of SHS may reach 2 % among patients with strongyloidiasis [9]. It typically occurs in immunocompromised patients with underlying illnesses such as advanced HIV infection. However, it is noteworthy that it is also frequently related to immunosuppressive treatments such as corticosteroids, most especially at the time of initiation or dosing increase [4]. Respiratory, gastrointestinal, cutaneous, and neurologic symptoms are observed in variable frequencies, but a hallmark of SHS is the severity of organ failures requiring ICU admission.
To date, single case reports stand for the most part of literature in the field of SHS. In this study, we aimed at describing the clinical and biological characteristics and the outcome of critically ill patients with SHS requiring ICU admission. We performed a retrospective multicenter study in order to maintain a high level of suspicion toward diagnosis and prevention. In addition, we performed a review of literature to identify the previously published cases and series of SHS.
Patients and methods
Study design and definitions
We performed a retrospective study in order to address the features and the outcomes of patients admitted to the intensive care unit for SHS. To this aim, we gathered a cohort of original cases (unpublished cases) of SHS from the ICUs involved in the Grrr-OH (Groupe de Recherche sur la Réanimation Respiratoire chez le patient d’Onco-Hématologie) research network within a 14-year period (2000–2013). To this aim, we performed searches both through medical files in the ICU and records from the parasitology laboratories. In addition we performed an exhaustive review of the literature in order to collect the previously published cases of SHS.
SHS was defined as disseminated strongyloidiasis implying the presence or exacerbation of gastrointestinal and/or respiratory symptoms attributable to increased larval migration [5]. Parasitologic detection was performed on available samples: stools, gastrointestinal biopsies, respiratory samples analysis, cerebrospinal fluid, skin biopsy, and other histologic or necropsic examinations. Hypereosinophilia was defined as an eosinophil count higher than 500/mm3. Endemic areas were defined as zones with Strongyloides stercoralis infection prevalence and was higher than 10 % as previously described [3].
Literature review
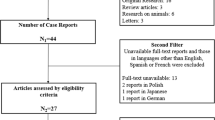
The published cases were retrieved in the National Library of Medicine’s MEDLINE using the keywords Strongyloidiasis and immunocompromized, Strongyloides hyperinfection, malignant Strongyloidiasis, Strongyloides superinfection. Papers in English and in French were included in the review. Two investigators (GG and FP) independently reviewed the case reports. The search period ranged from January 1970 to June 2010. The references of all articles were also checked for additional relevant reports. Only reports including the main clinical and biological data and the survival status were taken into account.
Data collection
We collected the following data for the unpublished and literature cases: demographic data (age, gender, geographic origin), underlying immunosuppressive disease [HIV infection, hematologic malignancy, cancer, autoimmune disease, Human T-lymphotropic virus 1 (HTLV1) infection], treatment with corticosteroids (presence of corticosteroids treated as a binary variable, daily dose, and time from corticosteroids initiation and identification of Strongyloides infection), chemotherapy or other immunosuppressive drugs, clinical features including respiratory failure requiring mechanical ventilation, and shock defined by a circulatory failure with persistent hypotension despite fluid loading and requiring vasopressors, eosinophil count, parasitologic investigations (serology, stools’ material, gastrointestinal tract biopsies, respiratory samples, cerebrospinal fluid). Standard stool microscopy and Baermann concentration technique were routinely used. Serological testing consisted of an enzyme-linked immunosorbent assay to detect IgG to a filariform larval antigen. The type of antiparasitic treatment (albendazole, thiabendazole, and/or ivermectin) was collected as well and the outcome was ICU survival.
Statistical analysis
Descriptive statistics were reported as medians (with interquartile range) and as numbers (percentage) for continuous and categorical variables, respectively. The characteristics of patients from the unpublished series and from the literature review were compared using Student or Mann–Whitney–Wilcoxon’s rank sum test, and Pearson χ 2 test or the Fisher’s exact test, as appropriate. Variables associated with ICU mortality and shock occurrence in univariate analysis (p value <0.10) were then entered in a multivariate logistic regression analysis using a backward stepwise procedure. The calibration of the model was evaluated by the Hosmer–Lemeshow test in which a p value >0.20 indicated adequate calibration. Clinically relevant interactions were tested two by two using the Wald test (p for interaction <0.10).
Results
Baseline characteristics of patients
One hundred and thirty-three patients including 11 unpublished cases and 122 previously published cases that met eligibility criteria were included in the study. The flow diagram of the literature review and the complete list of references are available in the supplementary file. The patients’ baseline characteristics are presented in Table 1. Patients were mostly males, with a median age of 53 (39–64) years. Two-thirds of patients originated from Strongyloides endemic area.
An underlying immunosuppression was reported in 127 patients (95.5 %), 33 of them (25.8 %) had autoimmune disorders, 27 (21.1 %) had hematologic malignancies, 20 (15.6 %) had obstructive airway disorders, 16 (12.5 %) had solid organ transplantation, 14 (10.9 %) had HIV infection, and 12 (9.4 %) had miscellaneous disorders. In HIV-infected patients, the median CD4 lymphocyte count was 34 (14–48) per mm3 and the median viral load was 50157 [6-430000] copies/mL. 111 (83.5 %) patients were treated with corticosteroids at a median dose of 40 mg per day. Of note, the corticosteroid dosing had been recently increased prior to SHS in 34 patients (46.6 % of available data). The median time from corticosteroid treatment initiation to the occurrence of SHS symptoms was 42 days. Adjunctive immunosuppressant or chemotherapy was reported in 33 (24.8 %) and 24 (18.1 %) patients, respectively.
Features of Strongyloides hyperinfection syndrome
Clinical and biological characteristics of SHS, treatment modalities, and outcome are presented in Table 2. Fever was observed in most patients (n = 105, 80.8 %). Gastrointestinal and respiratory symptoms were very frequent as well (n = 94, 71.2 % and n = 117, 88.6 %, respectively). A majority of patients exhibited organ failures such as shock (n = 75, 57.3 %) and acute respiratory failure requiring mechanical ventilation (n = 89, 70.0 %). Of note, shock and mechanical ventilation were more frequent in the unpublished case series.
Biologic explorations evidenced hypereosinophilia in 34 (34.3 %) patients for whom the median count was 1638 (747–3000) per mm3. Human T-lymphotropic virus 1 (HTLV1) serology was positive in seven out of 16 patients. Strongyloides larvae were retrieved in stools in 98 (93.3 %) cases. Respiratory samples including sputum, tracheal aspirates, or bronchoalveolar fluid evidenced parasitic infection in 93 (93.9 %) patients. SHS diagnosis was made post-mortem in 10 (7.5 %) cases in which necropsy evidenced multi-organ parasitic invasion. Serological diagnosis was reported in 14 cases and was positive in 12 of them. Anti-helminthic treatment was distributed between thiabendazole in 45 (35.3 %) patients, albendazole in 37 (28.9 %) patients, and ivermectin in 52 (40.6 %) patients. Ivermectin was administered by enteral route in most cases (n = 46, 95.8 %), but parenteral administration was occasionally required in 13 (26.5 %) cases.
Interestingly, a concomitant bacterial infection was observed in 51 (38.4 %) patients. Thirty-four had bacteremia, 23 had pneumonias, and 14 had meningitis. Bacteremia were due to Enterobacteriaceae in 29 cases, Enterococcus species in four cases, Pseudomonas aeruginosa in two cases, and were polymicrobial in seven cases. In addition, two cases of Candida albicans fungemia have been reported. Bacterial meningitis was mostly related to Enterobacteriaceae (n = 10), while Enterococcus faecium and Streptococcus viridans were documented in three and one cases, respectively. The overall outcome of SHS patients was poor with an in-ICU mortality rate of 60.3 %.
Prognostic factors
We performed univariate and multivariate analysis in order to identify the factors predictive of ICU mortality (Table 3 ). In univariate analysis, fever, concomitant bacterial infection, shock, and mechanical ventilation were associated with ICU mortality whereas the endemic zone origin and hypereosinophilia were negatively associated with ICU mortality. All these variables were entered into a multivariate logistic regression model. Not surprisingly, organ failures such as shock (Odds ratio (OR) 18.1, 95 % confidence interval (95 % CI) 3.03–107.6, p < 0.01) and mechanical ventilation (OR 28.1, 95 % CI 3.6–217, p < 0.01) were independently associated with ICU mortality. Furthermore, we performed an additional analysis with shock as the dependent variable (Table 4 ). A concomitant bacterial infection (OR 4.68, 95 % CI 1.3–16.8, p = 0.02) was an independent predictor of shock while hypereosinophilia (OR 0.21, 95 % CI 0.06–0.7, p = 0.01) was protective.
Discussion
This study combining original and previously published cases of SHS highlights five striking messages: (1) SHS is a rare disorder in France since we only identified 11 cases from about 20 ICUs over a 14-year period; (2) SHS is usually associated with immunosuppressive conditions but may be observed without any comorbidities; (3) a concomitant bacterial infection is commonly encountered, most especially in patients with shock; (4) SHS is associated with a poor outcome owing to the frequency of organ failures; (5) Hypereosinophilia may carry a protective role toward deterioration to shock.
The immune response against Strongyloides stercoralis is complex and relies both on polymorphonuclear eosinophils and on a potent Th-2 adaptive immune response. The particular susceptibility of HTLV1-infected patients to SHS emphasizes the importance of T cell response in the host defense against Strongyloides. HTLV-1 induces both a Th-1 response and the expansion of regulatory T cells that result in decreased production of IL-5 and eosinophil depletion [10, 11]. Accordingly, expansion of regulatory T cells has been associated with impaired immune response against Strongyloides infection in mouse models, whereas their depletion decreased the worm burden [12]. The polymorphonuclear eosinophil is the cornerstone of anti-helminthic host defense, acting as an antigen-presenting cell to induce Th2 adaptive immunity in an IL-5-dependent manner [13–18]. Several experimental data have demonstrated the critical role of eosinophils against helminths by modulating their numbers or their antigen-presenting functions in mice [13, 17, 19–21]. Hypereosinophilia is encountered in about 70 % of patients with Strongyloides infection but only 20 % of SHS patients [22, 23]. The involvement of eosinophils was suggested in the present study by the association between hypereosinophilia and protection from shock. This finding is consistent with previous reports suggesting that eosinopenia was associated with a worse outcome in SHS [24, 25]. Whether eosinophilia is directly involved in the pathophysiology of organ failures or is just a bystander of appropriate antiparasitic immune response remains unclear.
A number of immunosuppressive medications are likely to alter the antiparasitic immune response. Our study highlights the major role of corticosteroid treatment as a risk factor of SHS [7, 8, 26]. Indeed, corticosteroids promote apoptosis of eosinophils and have potent effects on their main functions. In the present report, 83.5 % of patients were receiving corticosteroid treatment at a median dose of 40 mg per day. The main indications for corticosteroids were autoimmune disorders or hematological malignancies in combination with chemotherapy [8, 27]. Of note, chronic airway disorders were also quite frequent indications of corticosteroid treatment (15 % of patients). The very high prevalence of corticosteroid treatment probably accounted for the absence of impact on ICU mortality or shock. Considering the lack of specificity of gastrointestinal and respiratory symptoms or fever in such immunocompromised patients, physicians should remain aware that any increase in immunosuppression may result in SHS in patients with chronic Strongyloides infection.
Multiple organ involvement is a hallmark of SHS. Accordingly, organ failures were frequently observed both in our case series and in the literature cases. Thus shock developed in 60 % of the whole cohort, and in 90 % of unpublished cases. Organ failures might be explained by not only overwhelming parasitic invasion, but also by concomitant bacterial infections that were present in 38.4 % of patients and that were identified as an independent predictor of shock. Such bacterial infections are mostly related to Enterobacteriaceae, thereby suggesting a digestive origin. Several mechanisms linking helminthic migration and bacterial infections have been proposed, including gastrointestinal mucous damage [28–30], small bowel bacterial overgrowth [31], and bacterial carriage onto the parasite’s surface. Furthermore, the release of a Macrophage Migration Inhibitory Factor-like protein by the parasite itself may promote an anti-inflammatory cytokine pattern likely to favor bacterial superinfections [32, 33]. Thus, patients with SHS carry a high risk of bacterial infections that should prompt early empirical antibiotic treatment in case of organ failures.
The rarity of SHS precluded a comprehensive assessment of treatment in critically ill patients, and the indications of antiparasitic drugs in SHS remain largely based on their efficacy in chronic strongyloidiasis. Thus, ivermectin currently represents the gold standard treatment of SHS since it has been shown to be more efficient than high-dose albendazole in chronic strongyloidiasis [34, 35]. However, the lack of parenteral formulation of ivermectin approved for humans represents a major limit for administration to critically ill SHS patients who often evidence occlusive syndrome and malabsorption. For this reason, a veterinary parenteral formulation of ivermectin has successfully been used subcutaneously in some case reports, although the compound’s efficacy remains difficult to establish in such biased publications [36–39]. Most importantly, the high mortality rate of established SHS strongly pleads for a large implementation of antiparasitic primary prophylaxis in patients who stayed in Strongyloides endemic zones and who have risk factors of SHS, such as initiation or intensification of immunosuppression. As of today, a single-dose treatment with ivermectin represents a simple, efficient, and cheap preventive intervention against hyperinfection syndrome [40].
The present study has several limitations. First, we may have missed some cases due to the retrospective design of the study. Second, our original cases were obtained from a non-endemic zone. Third, the literature review of SHS cases was obviously dependent on publication biases, making it impossible to address the real prevalence and incidence of SHS. Fourth, HIV infection might have been underestimated since detection was not available before 1985. Last, some relevant data were not exhaustively recorded in published cases. However most cases were very detailed, making it possible performing a reliable statistical analysis.
In conclusion, we here report a comprehensive analysis of original and previously published cases of SHS. The deterioration to shock may evoke a concomitant bacterial infection. The poor outcome of established SHS strongly supports the large application of antiparasitic eradication prophylaxis in at-risk patients, particularly in case of initiation or intensification of immunosuppression.
References
Siddiqui AA, Berk SL. Diagnosis of Strongyloides stercoralis infection. Clin Infect Dis Off Publ Infect Dis Soc Am. 2001;33:1040–7.
Vadlamudi RS, Chi DS, Krishnaswamy G. Intestinal strongyloidiasis and hyperinfection syndrome. Clin Mol Allergy CMA. 2006;4:8.
Schär F, Trostdorf U, Giardina F, Khieu V, Muth S, Marti H, et al. Strongyloides stercoralis: global Distribution and Risk Factors. Plos Negl Trop Dis. 2013;7:e2288.
Ramanathan R, Nutman T. Strongyloides stercoralis infection in the immunocompromised host. Curr Infect Dis Rep. 2008;10:105–10.
Keiser PB, Nutman TB. Strongyloides stercoralis in the immunocompromised population. Clin Microbiol Rev. 2004;17:208–17.
Concha R, Harrington W Jr, Rogers AI. Intestinal strongyloidiasis: recognition, management, and determinants of outcome. J Clin Gastroenterol. 2005;39:203–11.
Debussche X, Toublanc M, Camillieri JP, Assan R. Overwhelming strongyloidiasis in a diabetic patient following ACTH treatment and keto-acidosis. Diabète Métabolisme. 1988;14:294–8.
Rivera E, Maldonado N, Vélez-García E, Grillo AJ, Malaret G. Hyperinfection syndrome with Strongyloides stercoralis. Ann Intern Med. 1970;72:199–204.
Milder JE, Walzer PD, Kilgore G, Rutherford I, Klein M. Clinical features of Strongyloides stercoralis infection in an endemic area of the United States. Gastroenterology. 1981;80:1481–8.
Montes M, Sanchez C, Verdonck K, Lake JE, Gonzalez E, Lopez G, et al. Regulatory T cell expansion in HTLV-1 and strongyloidiasis co-infection is associated with reduced IL-5 responses to Strongyloides stercoralis antigen. Plos Negl Trop Dis. 2009;3:e456.
Porto AF, Neva FA, Bittencourt H, Lisboa W, Thompson R, Alcântara L, et al. HTLV-1 decreases Th2 type of immune response in patients with strongyloidiasis. Parasite Immunol. 2001;23:503–7.
Blankenhaus B, Klemm U, Eschbach M-L, Sparwasser T, Huehn J, Kühl AA, et al. Strongyloides ratti infection induces expansion of Foxp3+ regulatory T cells that interfere with immune response and parasite clearance in BALB/c mice. J Immunol Baltim Md. 1950;2011(186):4295–305.
Galioto AM, Hess JA, Nolan TJ, Schad GA, Lee JJ, Abraham D. Role of eosinophils and neutrophils in innate and adaptive protective immunity to larval strongyloides stercoralis in mice. Infect Immun. 2006;74:5730–8.
Herbert DR, Lee JJ, Lee NA, Nolan TJ, Schad GA, Abraham D. Role of IL-5 in innate and adaptive immunity to larval Strongyloides stercoralis in mice. J Immunol Baltim Md. 1950;2000(165):4544–51.
Kerepesi LA, Hess JA, Nolan TJ, Schad GA, Abraham D. Complement component C3 is required for protective innate and adaptive immunity to larval strongyloides stercoralis in mice. J Immunol Baltim Md. 1950;2006(176):4315–22.
Rotman HL, Yutanawiboonchai W, Brigandi RA, Leon O, Gleich GJ, Nolan TJ, et al. Strongyloides stercoralis: eosinophil-dependent immune-mediated killing of third stage larvae in BALB/cByJ mice. Exp Parasitol. 1996;82:267–78.
Padigel UM, Hess JA, Lee JJ, Lok JB, Nolan TJ, Schad GA, et al. Eosinophils act as antigen-presenting cells to induce immunity to Strongyloides stercoralis in mice. J Infect Dis. 2007;196:1844–51.
Padigel UM, Lee JJ, Nolan TJ, Schad GA, Abraham D. Eosinophils can function as antigen-presenting cells to induce primary and secondary immune responses to Strongyloides stercoralis. Infect Immun. 2006;74:3232–8.
Coffman RL, Seymour BW, Hudak S, Jackson J, Rennick D. Antibody to interleukin-5 inhibits helminth-induced eosinophilia in mice. Science. 1989;245:308–10.
Grimaldi JC, Yu NX, Grunig G, Seymour BW, Cottrez F, Robinson DS, et al. Depletion of eosinophils in mice through the use of antibodies specific for C-C chemokine receptor 3 (CCR3). J Leukoc Biol. 1999;65:846–53.
Gurish MF, Humbles A, Tao H, Finkelstein S, Boyce JA, Gerard C, et al. CCR3 is required for tissue eosinophilia and larval cytotoxicity after infection with Trichinella spiralis. J Immunol Baltim Md. 1950;2002(168):5730–6.
Liu H-C, Hsu J-Y, Chang K-M. Strongyloides stercoralis hyperinfection presenting with symptoms mimicking acute exacerbation of chronic obstructive pulmonary disease. J Chin Med Assoc. 2009;72:442–5.
Lagacé-Wiens PRS, Harding GKM. A Canadian immigrant with coinfection of Strongyloides stercoralis and human T-lymphotropic virus 1. Can Med Assoc J . 2007;177:451–3.
Igra-Siegman Y, Kapila R, Sen P, Kaminski ZC, Louria DB. Syndrome of hyperinfection with Strongyloides stercoralis. Rev Infect Dis. 1981;3:397–407.
Adedayo O, Grell G, Bellot P. Hyperinfective strongyloidiasis in the medical ward: review of 27 cases in 5 years. South Med J. 2002;95:711–6.
Fardet L, Généreau T, Poirot J-L, Guidet B, Kettaneh A, Cabane J. Severe strongyloidiasis in corticosteroid-treated patients: case series and literature review. J Infect. 2007;54:18–27.
Coulter C, Walker DG, Günsberg M, Brown IG, Bligh JF, Prociv P. Successful treatment of disseminated strongyloidiasis. Med J Aust. 1992;157:331–2.
Ghoshal UC, Ghoshal U, Jain M, Kumar A, Aggarwal R, Misra A, et al. Strongyloides stercoralis infestation associated with septicemia due to intestinal transmural migration of bacteria. J Gastroenterol Hepatol. 2002;17:1331–3.
Kakati B, Dang S, Heif M, Caradine K, McKnight W, Aduli F. Strongyloides duodenitis: case report and review of literature. J Natl Med Assoc. 2011;103:60–3.
Gutierrez Y, Bhatia P, Garbadawala ST, Dobson JR, Wallace TM, Carey TE. Strongyloides stercoralis eosinophilic granulomatous enterocolitis. Am J Surg Pathol. 1996;20:603–12.
Sipahi AM, Damião AO, Simionato CS, Bonini N, Santos MA, de Moraes-Filho JP, et al. Small bowel bacterial overgrowth in strongyloidiasis. Digestion. 1991;49:120–4.
Younis AE, Soblik H, Ajonina-Ekoti I, Erttmann KD, Luersen K, Liebau E, et al. Characterization of a secreted macrophage migration inhibitory factor homologue of the parasitic nematode Strongyloides acting at the parasite-host cell interface. Microbes Infect Inst Pasteur. 2012;14:279–89.
Pastrana DV, Raghavan N, FitzGerald P, Eisinger SW, Metz C, Bucala R, et al. Filarial nematode parasites secrete a homologue of the human cytokine macrophage migration inhibitory factor. Infect Immun. 1998;66:5955–63.
Suputtamongkol Y, Premasathian N, Bhumimuang K, Waywa D, Nilganuwong S, Karuphong E, et al. Efficacy and safety of single and double doses of ivermectin versus 7-day high dose albendazole for chronic strongyloidiasis. Plos Negl Trop Dis. 2011;5:e1044.
Muennig P, Pallin D, Challah C, Khan K. The cost-effectiveness of ivermectin vs. albendazole in the presumptive treatment of strongyloidiasis in immigrants to the United States. Epidemiol Infect. 2004;132:1055–63.
Hauber HP, Galle J, Chiodini PL, Rupp J, Birke R, Vollmer E, et al. Fatal outcome of a hyperinfection syndrome despite successful eradication of Strongyloides with subcutaneous ivermectin. Infection. 2005;33:383–6.
Leung V, Al-Rawahi GN, Grant J, Fleckenstein L, Bowie W. Case report: failure of subcutaneous ivermectin in treating Strongyloides hyperinfection. Am J Trop Med Hyg. 2008;79:853–5.
Lichtenberger P, Rosa-Cunha I, Morris M, Nishida S, Akpinar E, Gaitan J, et al. Hyperinfection strongyloidiasis in a liver transplant recipient treated with parenteral ivermectin. Transpl Infect Dis Off J Transplant Soc. 2009;11:137–42.
Pacanowski J, Santos MD, Roux A, Maignan CLE, Guillot J, Lavarde V, et al. Subcutaneous ivermectin as a safe salvage therapy in Strongyloides stercoralis hyperinfection syndrome: a case report. Am J Trop Med Hyg. 2005;73:122–4.
Santiago M, Leitão B. Prevention of strongyloides hyperinfection syndrome: a rheumatological point of view. Eur J Intern Med. 2009;20:744–8.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the Groupe de Recherche sur la Réanimation Respiratoire en Onco-Hématologie (Grrr-OH).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Geri, G., Rabbat, A., Mayaux, J. et al. Strongyloides stercoralis hyperinfection syndrome: a case series and a review of the literature. Infection 43, 691–698 (2015). https://doi.org/10.1007/s15010-015-0799-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-015-0799-1