Abstract
Purpose
Bloodstream infections (BSIs) are frequent after allogeneic haematopoietic stem cell transplantation (HSCT). The aim of this study was to identify predictors of mortality after BSI in patients who undergo HSCT.
Methods
Patients who underwent HSCT between 1 January 2004 and 31 January 2008 and developed BSI during the first year post-transplantation were included. Variables influencing overall mortality at 7 and 30 days after BSI were analysed.
Results
BSIs developed in 149 patients, within a median of 9 days after undergoing HSCT. Early and late mortality were 15 and 27%, respectively. Of the BSI, 54% were due to Gram-positive microorganisms, 33% were due to Gram-negative microogranisms, 10% were polymicrobial and 3% were fungal. The associated 7-and 30-day mortality was respectively 10 and 24% (Gram positive), 22 and 31% (Gram negative; Pseudomonas aeruginosa mortality 67%, all within 7 days), 13 and 27% (polymicrobial) and 40% (fungal, all within 7 days). Early mortality was higher in relapsed disease at HSCT (25.9%, p = 0.01), but lower in early (i.e. within 20 days of HSCT) BSI (11.7%, p = 0.03) and BSI due to Gram-positive infective agents (10%, p = 0.05). Multivariate analysis confirmed a higher mortality in late BSI [odds ratio (OR) 3.29, p = 0.03] and relapsed disease at HSCT (OR 2.2, p = 0.04). Late mortality was associated with the type of underlying disease (OR 0.44 for diseases other than acute leukaemia, p = 0.05) and its status (OR 6.04 for relapse at HSCT, p = 0.001). Appropriate empirical therapy was associated with lower early and late mortality in single Gram-negative BSI (16 vs. 45% for 7-day mortality, p = 0.09; 21 vs. 64% for 30-day mortality, p = 0.02).
Conclusions
BSIs are frequent during the first year after HSCT and are associated with a high mortality rate. The aetiology influenced early mortality, while the type and phase of the underlying disease played a pivotal role in late mortality. Appropriate empirical therapy is crucial in BSI due to Gram-negative infective agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bloodstream infections (BSIs) are the most frequent infectious complication in patients who have undergone allogeneic haematopoietic stem cell transplantation (HSCT) and affect up to 30% of patients [1–5]. It is likely that during the pre-engraftment phase mucosal damage allows bacteria to enter the bloodstream and the lack of neutrophils hampers their effective clearance, thus leading to BSI. During the post-engraftment phase, the presence of graft versus host disease (GVHD), particularly intestinal, and secondary neutropenia predispose patients to BSIs. Moreover, the presence of central venous catheters (CVC) further increases the risk of introducing bacteria into the bloodstream.
Historically, mortality due to BSIs has been always higher in neutropenic patients than in other subjects. Indeed, the mortality attributable to BSI episodes following HSCT has been reported to be as high as 18–35%, particularly if caused by Gram-negative rods [1, 2, 6]. Traditional studies focus on the relationship between BSI aetiology and mortality; however, others factors might significantly influence early and late mortality after BSI in HSCT patients.
The aim of this study was to identify early and late mortality rates and their predictors in BSIs in patients who underwent HSCT.
Material and methods
This study on mortality in patients with BSI was carried out in 382 consecutive patients who underwent allogeneic HSCT between 1 January 2004 and 31 December 2008 at the HSCT Unit of San Martino Hospital in Genoa. All data were acquired from a prospectively collected computerised database, and a retrospective analysis was performed. The patients were included in the study if they developed bacteraemia in the period between the onset of conditioning to 1 year after HSCT. Some of these BSI episodes were previously included in a study on the aetiology of BSIs in all HSCT recipients from our centre [4].
Only the first episode of BSI was considered. BSI was defined as the isolation of a pathogen from at least one blood culture, but in case of common skin contaminants (coagulase-negative staphylococci, Micrococcus, Corynebacterium, Lactobacillus etc), two consecutive, drawn within 24 h, blood cultures positive for the same pathogen were required to qualify the episode as a BSI [2]. BSI was defined as polymicrobial if two or more pathogens grew in a blood culture or if two different pathogens were recovered from specimens drawn within 48 h.
Transplantation was performed according to institutional protocols using procedures that have been described elsewhere [4, 5]. Surveillance cultures from the pharynx and genital and urinary systems were performed once a week in all inpatients, together with rectal screening for vancomycin-resistant enterococci (VRE) at admission. No methicillin-resistant Staphylococcus aureus (MRSA) screening was performed because the majority of staphylococci recovered from hospitalised patients were resistant to methicillin. All patients received fluoroquinolone (ciprofloxacin or levofloxacin) as prophylaxis from the start of conditioning until neutrophil engraftment. Antifungal prophylaxis with fluconazole was administered from the time of the transplant procedure up to 70 days thereafter, or longer if GVHD was present. In the case of fever (>38°C) or other signs or symptoms of infection, prophylactic antibiotics were stopped and patients were treated with broad-spectrum empirical therapy. The most common regimens included either piperacillin/tazobactam or ceftazidime (usually with amikacin) and in case of severe sepsis or septic shock, meropenem and vancomycin, the choice being at the discretion of the attending physician.
The primary study endpoint was overall cumulative mortality at 7 and 30 days after the onset of BSI (i.e. the day of the first positive blood culture). Groups of patients who were alive or deceased at 7 and 30 days after the development of BSI were compared to identify predictors of mortality. Baseline and post-transplant variables analysed as potential factors influencing mortality included age, sex, type and status of the underlying disease at HSCT, donor type, conditioning regimen, year of BSI, pathogen and the time between HSCT and BSI. The cutoff of 20 days after HSCT infusion was chosen to distinguish early BSI, i.e. that infection usually occurring during the pre-engraftment period, and late BSI, i.e. that infection usually developing during the post-engraftment period (such as during GVHD), relapse of the underlying disease or infection related to the presence of a CVC. Status of the underlying disease at HSCT was classified as follows: (1) first complete remission or inactive disease after the first line of treatment; (2) complete remission or inactive disease after two or more lines of treatment; (3) relapse or active disease at the time of HSCT. Neutropenia was defined as an absolute granulocyte count of <0.5 × 109/l. The pathogens were grouped as single Gram+ versus Gram−, fungi and polymicrobial BSI. Given that an appropriate empirical therapy is of utmost importance for the survival of patients with BSI due to Gram-negative pathogens, the influence of an appropriate (i.e. containing at least one agent active against a given pathogen) antibiotic therapy was analysed for single Gram-negative BSI.
The univariate association between potential risk factors and outcome was assessed by means of χ2 test for heterogeneity or Fisher’s exact test when appropriate. Patients were divided in three groups of age according to tertiles. Multivariate logistic regression was used to assess the independent association with mortality of the various factors considered. The final model was obtained by means of a backward multivariate stepwise procedure, based on the likelihood ratio test. As a measure of the strength of association, the odds ratio (OR) with 95% confidence intervals (95% CI) were computed by exponentiating the coefficient in the logistic regression model. All p values are two-sided, and p values of ≤0.05 were considered to be statistically significant. The analyses were performed using SPSS statistical package, ver. 17.0 for Windows (SPSS, Chicago, IL).
Results
Of 382 patients transplanted during the study period, 149 (39%) developed BSI. Most patients were male (64%) and were affected by acute leukaemia (92, 61.7%). Other underling diseases were multiple myeloma and chronic lymphocytic leukaemia (16 patients, 10.7%), myelodysplastic syndrome and severe aplastic anaemia (14 patients each, 9.4%), followed by chronic myeloid leukaemia and myelofibrosis (13 patients, 8.7%). The donor types were matched related in 47 patients (31.5%), matched unrelated (MUD) in 38 patients (25.5%), cord blood in 29 patients (19.5%), mismatched related in 22 patients (14.8%) and mismatched unrelated in 13 patients (8.7%). The median age was 41 (range 16–65) years. Median follow-up after BSI was 144 days (range 1–1,413) and was more than 30 days for all the survivors. Patient and transplant characteristics are outlined in Table 1.
Median time to bacteraemia was 9 days after transplantion, ranging from 6 days before HSC infusion (during the conditioning regimen) to 322 days therafter. About three-fourth of the episodes occurred early after HSCT, while 25% were classified as late BSI (>20 days after HSCT). A single Gram-positive microorganism was responsible for more than half of the BSIs, followed by infections caused by a single Gram-negative rod and polymicrobial BSIs. Almost all (96%) Staphylococcus infections were resistant to methicillin. Enterococci were the most frequent pathogens, with 51% being susceptible to ampicillin and vancomycin, 37% being resistant to ampicillin and susceptible to vancomycin and 11% being VRE. Among the Gram-negative rods, 73% were resistant to fluoroquinolones and 35% were resistant to ceftazidime. There were important differences in the aetiology between early and late BSIs. Early BSIs were mostly due to enterococci or streptococci (37.8%), followed by Gram-negative rods (29.7%), staphylococci or other skin bacteria (20.7%) and finally polymicrobial or fungal (11.7%). Late infections were predominantly caused by Gram-negative rods (42.1%), followed by staphylococci or other skin bacteria (23.7%), polymicrobial or fungal (18.4%) and enterococci and streptococci (15.8%).
Overall, at 7 and 30 days post-transplantation mortality was 15.4% (23/149) and 26.9% (40/149), respectively. The detailed aetiology with the number of patients deceased 7 and 30 days after BSI (distinguishing between early and late BSI) is shown in Table 2. Among the 40 patients who died within 30 days of developing BSI, ten (25%) died due to a relapse of an underlying disease or primary graft rejection, ten (25%) died from multiorgan toxicity, including haemorrhage, acute respiratory distress syndrome and acute renal failure, two (5%) died due to acute GVHD and 18 died (45%) due to infection. Among the latter 18 patients, ten died within 7 days from the onset of sepsis due to the following pathogens: P. aeruginosa (4 patients: 2 multidrug resistant, 1 coinfection with invasive aspergillosis), E. coli (1 patient), Klebsiella pneumoniae (1 patient), Candida parapsilosis (1 patient), methicillin-resistant Staphylococcus epidermidis (1 patient), enterococci (2 patients: 1 VRE, 1 coinfection with invasive aspergillosis).
The early and late mortality was lower for BSIs caused by a single Gram-positive microorganism and polymicrobial BSIs than for BSIs caused by a single Gram-negative microorganism or fungal BSI. Among the BSIs caused by Gram-positive microorganisms, the highest mortality was due to enterococcal infection, particularly in the case of ampicillin-resistant strains. Early and late mortality was respectively 6 and 22% in ampicillin- and vancomycin- susceptible isolates, 23 and 38% in ampicillin-resistant and vancomycin-susceptible strains, and 25 and 25% in the case of VRE. Four patients who developed candidemia were receiving fluconazole prophylaxis; two patients with infection due to fluconazole-susceptible Candida parapsilosis and one with fluconazole-resistant C. krusei survived, while one patient with fluconazole-susceptible C. parapsilosis and one with fluconazole-resistant C. glabrata died within 7 days after the onset of candidemia.
Among all pathogens, Pseudomonas aeruginosa was associated with the highest mortality (67%), and all of the deaths occurred within 7 days of the development of BSI. In particular, three strains of P. aeruginosa were resistant to all antibiotics except for colistin, and the three patients infected with these strains died with 7 days of developing BSI. On the contrary, all 25 strains of Escherichia coli were susceptible to carbapenems, and the early mortality was 12%. Overall, in 49 cases of BSI due to a single Gram-negative microorganism, an appropriate antimicrobial therapy was administered in 38 patients (78%). The mortality rate was higher in the case of an inappropriate empirical treatment (45 vs. 16% for 7-day mortality, p = 0.09; 64 vs. 21% for 30-day mortality, p = 0.02).
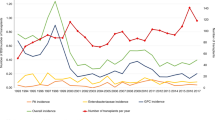
In the univariate analysis (Table 3), relapsed disease at transplantation (p = 0.01) and late BSI (p = 0.03) were significantly associated with a higher early mortality, while BSI due to a single Gram-positive microorganism was associated with lower early mortality (p = 0.05). Thirty-day mortality was significantly associated only with the status of the underlying disease at transplantation (p = 0.004). Multivariate analysis (Table 4) confirmed that predictors of 7-day mortality were late BSI (OR 3.29, 95% CI 1.15–9.38; p = 0.03) and relapsed disease at HSCT (OR 2.20, 95% CI 0.74–6.51; p = 0.04). The 30-day mortality was associated with the type and the status of the underlying disease. Mortality was lower in patients transplanted for diseases other than acute leukaemia (OR 0.44, 95% CI 0.19–1.03; p = 0.05), while patients who received more than one line of chemotherapy before HSCT showed an increased mortality rate that was more than twofold if the patients who were in remission after more than one chemotherapy series and more than sixfold if they had an active disease at HSCT (OR 2.34, 95% CI 0.76–7.2 and OR 6.04, 95% CI 2.18–16.71, respectively; p for trend = 0.001). The overall survival after BSI, stratified according to the status of the underlying, is outlined in Fig. 1.
Overall survival after bloodstream infection according to the status of the underlying disease at time of haematopoietic stem cell transplantation (HSCT). Black line first complete remission or inactive disease after first-line treatment, grey line complete remission or inactive disease after ≥2 lines of treatment, dotted line relapse or active disease at the time of HSCT (p < 0.0001)
Discussion
The aim of this study was to identify predictors of mortality following the development of BSI in HSCT recipients during the first year after transplantation. The overall early (7-day) and late (30-day) mortality was 15 and 27%, respectively. These mortality rates are among the highest reported to date in the literature, possibly because of a restrictive definition used for BSI due to common skin contaminants and a severe coexisting immunosuppression.
Early mortality was as high as 26% in the case of late BSI. Our results are at variance with these reported by Almyroudis and colleagues who found significantly lower mortality rates, particularly for post-engraftment BSI for which they reported a 30-day mortality rate of only 17% [1]. These results might be explained by the fact that in the study of these authors Gram-positive bacteria prevailed and more than 53% of the patients received transplants from a matched related donor. On the contrary, in our study only 40% of cases of late bacteraemia were due to Gram-positive microorganisms and almost 70% transplants were from alternative donors, which are known to be associated with a severe long-lasting immune deficit. Additionally, early mortality was twice as high in patients with uncontrolled underlying disease at HSCT when compared to those who were in remission at HSCT. Such a difference might be due to the fact that patients transplanted in relapse usually have received multiple cycles of intensive chemotherapy, resulting in more severe immunosuppression, longer hospitalisation, higher exposure to antimicrobial treatment and, sometimes, the presence of severe infections before HSCT. Thus, previous antimicrobial exposure and poorer immunity might be responsible for a higher mortality rate. A similar negative influence of pre-transplant intensive chemotherapy was also reported by Scott and colleagues [7]. In their study, the presence of pre-transplant neutropenia was associated with an increased infection-related mortality in patients with myelodysplastic syndrome undergoing HSCT, even though the effect could have been due to an increased incidence of infections [7].
One of the main factors that has been analysed in many studies on BSI-associated mortality is its aetiology. The aetiology of BSI determined in this study was similar to the findings previously reported in our centre [4]. Although the type of pathogen was not a significant independent risk factor in the multivariate analysis, possibly due to an insufficient number of cases, some of our findings deserve to be commented upon. High mortality rates have been found to be associated with BSI due to E. coli, P. aeruginosa and Candida, with the rates varying significantly between studies from 3 to 38% for E. coli, but being consistently high (around 40–50%) for P. aeruginosa and Candida [2, 6]. Also, in our study, the mortality associated with P. aeruginosa remained very high (2/3 patients died), even though the overall incidence of sepsis due to this species was low (6% of all BSIs) [2, 8, 9]. On the contrary, the rate of mortality in the case of E. coli infection was low (12%). Knowing that an inadequate empirical treatment predicts higher mortality in BSIs [10], such an important difference in mortality between P. aeruginosa and E. coli infections might result from the fact that in our centre most of the Enterobacteriaceae remain susceptible to piperacillin/tazobactam or carbapenems that are used in empirical treatments of severe BSI, whereas numerous P. aeruginosa isolates are resistant [4]. Indeed, even in a limited-size sample such as ours, inappropriate empirical therapy resulted in a higher early and late mortality. Overall, the mortality was the lowest in BSI due to Gram-positive pathogens. At our centre, for almost a decade enterococci have been the most frequent Gram-positive pathogens, particularly during the pre-engraftment period [4, 5, 11]. Pharyngeal colonisation and mucositis have been found to be specific risk factors for the development of enterococcal BSI, but the attributable mortality was found to be low [11]. Although early mortality was apparently lower in the case of ampicillin-susceptible strains, there was no difference in outcome in vancomycin-susceptible and VRE isolates. Indeed, the intrinsic virulence of enterococci is considered to be low; thus, it is believed that enterococcal BSI, particularly due to VRE strains, might rather be a marker of the host’s severe disease predisposing to this infection, rather than a result of bacterial pathogenicity [11, 12]. Contrary to data from North American centres [1, 13, 14], the fatality rate, both early and late, for viridans streptococci was remarkably low in our study (0 and 8%, respectively).
In terms of late mortality, all of the groups of pathogens had similar fatality rates, ranging from 24% for Gram-positive microorganisms to 30% for Gram-negative ones and 40% for candidemia, although there were few cases of the latter. Of note, in the case of BSI due to Gram-negative microorganisms, an appropriate empirical therapy was associated with a significantly reduced mortality (21 vs. 64%). The 30-day mortality in our allogeneic HSCT setting seems to be higher than that in a general haematological population. In fact, in a recent multicenter prospective study on BSIs due to P. aeruginosa in adults with haematological malignancies, the reported mortality rate was 32% [13]. On the contrary, we observed 27% mortality for all pathogens, while in nine BSI cases due to P. aeruginosa, the mortality was as high as 67%. In our study, at 30 days after the development of BSI the survival rate was influenced significantly by the underlying disease and was lower in the case of acute leukaemia and an active disease at HSCT. These results indicate that a good control of an underlying haematological disease and an appropriate empirical therapy against Gram-negative microorganisms are crucial for reducing mortality due to infectious complications after allogeneic HSCT.
Several limitations of this study should be acknowledged. First, this was a retrospective analysis of data from a single centre, and it is well known that microbiological aetiology and pattern of resistance may differ significantly across centres. Therefore, these results should only be extrapolated to other settings with due caution. Secondly, overall mortality is influenced by numerous factors that are unrelated to BSI. However, the use of other endpoints, such as attributable mortality, exposes the results to a strong risk of bias. Thus, crude mortality seems to be the most appropriate variable when searching for the difference in outcome after BSI.
In conclusion, early mortality in the case of BSI in HSCT recipients was 15% and closely related to the status of the underlying haematological malignancy and the timing of BSI. Overall, one in four patients who developed BSI during the first year after HSCT died within 30 days of BSI. Gram-negative rods, particularly P. aeruginosa, continue to pose a real threat to this population, and an appropriate empirical therapy is fundamental in BSIs due to Gram-negative microorganisms. Despite preventive measures and broad spectrum empirical antibiotic therapy, reducing the fatality rate of bacteraemia remains a major challenge and will probably become even more difficult if the increase in antibiotic resistance observed worldwide continues.
References
Almyroudis NG, Fuller A, Jakubowski A, Sepkowitz K, Jaffe D, Small TN et al. Pre- and post-engraftment bloodstream infection rates and associated mortality in allogeneic hematopoietic stem cell transplant recipients. Transpl Infect Dis. 2005;7:11–7.
Collin BA, Leather HL, Wingard JR, Ramphal R. Evolution, incidence, and susceptibility of bacterial bloodstream isolates from 519 bone marrow transplant patients. Clin Infect Dis. 2001;33:947–53.
Poutsiaka DD, Price LL, Ucuzian A, Chan GW, Miller KB, Snydman DR. Blood stream infection after hematopoietic stem cell transplantation is associated with increased mortality. Bone Marrow Transplant. 2007;40:63–70.
Mikulska M, Del Bono V, Raiola AM, Bruno B, Gualandi F, Occhini D et al. Blood stream infections in allogeneic hematopoietic stem cell transplant recipients: reemergence of Gram-negative rods and increasing antibiotic resistance. Biol Blood Marrow Transplant. 2009;15:47–53.
Cappellano P, Viscoli C, Bruzzi P, Van Lint MT, Pereira CA, Bacigalupo A. Epidemiology and risk factors for bloodstream infections after allogeneic hematopoietic stem cell transplantion. New Microbiol. 2007;30:89–99.
Wisplinghoff H, Seifert H, Wenzel RP, Edmond MB. Current trends in the epidemiology of nosocomial bloodstream infections in patients with hematological malignancies and solid neoplasms in hospitals in the United States. Clin Infect Dis. 2003;36:1103–10.
Scott BL, Park JY, Deeg HJ, Marr KA, Boeckh M, Chauncey TR et al. Pretransplant neutropenia is associated with poor-risk cytogenetic features and increased infection-related mortality in patients with myelodysplastic syndromes. Biol Blood Marrow Transplant. 2008;14:799–806.
Johnson LE, D’Agata EM, Paterson DL, Clarke L, Qureshi ZA, Potoski BA et al. Pseudomonas aeruginosa bacteremia over a 10-year period: multidrug resistance and outcomes in transplant recipients. Transpl Infect Dis. 2009;11:227–34.
Hakki M, Limaye AP, Kim HW, Kirby KA, Corey L, Boeckh M. Invasive Pseudomonas aeruginosa infections: high rate of recurrence and mortality after hematopoietic cell transplantation. Bone Marrow Transplant. 2007;39:687–93.
Tumbarello M, Spanu T, Caira M, Trecarichi EM, Laurenti L, Montuori E et al. Factors associated with mortality in bacteremic patients with hematologic malignancies. Diagn Microbiol Infect Dis. 2009;64:320–6.
Mikulska M, Del Bono V, Prinapori R, Boni L, Raiola AM, Gualandi F et al. Risk factors for enterococcal bacteremia in allogeneic hematopoietic stem cell transplant recipients. Transpl Infect Dis. 2010;12:505–12.
Dubberke ER, Hollands JM, Georgantopoulos P, Augustin K, DiPersio JF, Mundy LM et al. Vancomycin-resistant enterococcal bloodstream infections on a hematopoietic stem cell transplant unit: are the sick getting sicker? Bone Marrow Transplant. 2006;38:813–9.
Steiner M, Villablanca J, Kersey J, Ramsay N, Haake R, Ferrieri P et al. Viridans streptococcal shock in bone marrow transplantation patients. Am J Hematol. 1993;42:354–8.
Bochud PY, Eggiman P, Calandra T, Van Melle G, Saghafi L, Francioli P. Bacteremia due to viridans streptococcus in neutropenic patients with cancer: clinical spectrum and risk factors. Clin Infect Dis. 1994;18:25–31.
Acknowledgments
This work was partly funded by Associazione Italiana contro il Cancro (AIRC) Milan.
Conflict of interest
All authors nothing to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mikulska, M., Del Bono, V., Bruzzi, P. et al. Mortality after bloodstream infections in allogeneic haematopoietic stem cell transplant (HSCT) recipients. Infection 40, 271–278 (2012). https://doi.org/10.1007/s15010-011-0229-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-011-0229-y