Abstract
Background and aim
Surgical site infections (SSIs) are associated with a high morbidity, mortality and healthcare costs. The prevention of SSIs is based on a combination of preoperative preparation, surgical techniques, perioperative antibiotic prophylaxis (PAP) and postoperative wound care. Despite an abundance of evidence demonstrating the effectiveness of antimicrobials to prevent SSIs, the use of antimicrobial prophylaxis in this clinical setting is associated with inappropriate timing and selection and excessive duration of administration. To date, pharmacy interns (PIs) have not been involved in this process. The aim of this study was to evaluate feasibility of involving PIs in monitoring adherence to the guidelines for antibiotic prophylaxis in surgery patients.
Methods
The study was conducted in seven hospitals in Germany within the framework of the project “Pharmacy interns on the ward” (P-STAT2). Twenty-seven PIs participated, either from either May to October 2008 or from November 2008 to April 2009. Each patient admitted to the participating wards was consecutively monitored. PIs documented the antibiotic prophylaxis and checked the adherence with the hospital ward’s PAP guidelines taking both the choice of antibiotic drug and the duration of PAP into account. The costs of antibiotics, personnel and material were calculated in cases of non-adherence with guidelines.
Results
This is the first time that PIs were involved in monitoring antibiotic prophylaxis guidelines. A total of 6,167 patients were enrolled (mean age 58.3 ± 19.6 years; 47.1% male); of these, 5,064 patients underwent surgery and were ultimately available for evaluation. Guidelines for antibiotic prophylaxis were followed in 70.7% of the cases.
Conclusions
The study revealed that many patients do not receive the appropriate antibiotic prophylaxis despite the fact that guidelines are in place. Based on these results, we conclude that PIs may play an important role in antibiotic prophylaxis management.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Surgical site infection (SSI) is a common complication of surgery, with reported incidence rates of 2–20% [1]. They are the second most common cause of nosocomial infections and are associated with high morbidity, mortality and healthcare costs [2–4]. It has been estimated that there were between 400,000 and 600,000 nosocomial infections in Germany in 2006, of which 22,5000 were SSIs [5].
The risk of SSI depends on many patient-related factors, including existing infections, low serum albumin concentration, older age, obesity and diabetes, as well as surgical factors, such as duration of procedure and how clean the surgical procedure is (clean, clean–contaminated, contaminated or dirty–infected) [4, 6]. Optimal antibiotic prophylaxis ensures that an adequate concentration of an appropriate antimicrobial agent is present in the serum, tissue and wound during the entire time that the incision is open. The antimicrobial agent should be active against those bacteria that are likely to be encountered during the operation and should be safe for the patient and an economical option for the hospital. Antibiotic prophylaxis is not only clearly indicated for contaminated and dirty–infected surgical procedures, but also for most clean–contaminated surgical wounds and many clean procedures, such as orthopaedic implants. The prevention of SSI is very important, and its success depends on a combination of preoperative preparation, surgical technique, perioperative antibiotic prophylaxis (PAP) and postoperative wound care [7]. The evidence for the effectiveness of antimicrobials in preventing SSIs is well established, with previous studies demonstrating the importance of timing, selection, and duration of the prophylaxis. The prolonged use of prophylactic antibiotics is associated with the prevalence of antimicrobial resistance on surgical wards and the emergence of toxicity, as well as with costs [3, 8–11].
The feasibility of training and employing pharmacy interns (PIs) on hospital wards in Germany and the high acceptance of PIs by physicians and nurses were demonstrated in a pivotal study in 2002 [12]. To the best of our knowledge, however, PIs have not been involved in monitoring the adherence to guidelines for antibiotic prophylaxis in surgery patients on hospital wards. PIs are highly qualified, but lack practical experience and, therefore, require supervision by an experienced clinical pharmacist. Involving PIs in the adherence to antibiotic prophylaxis gives them a chance to gain this practical experience. Furthermore, both overall productivity in the hospital ward and the quality of an essential process can be improved; hereby, personnel expenditure for PIs is low.
The analysis presented here was part of the German multicentre evaluation “Pharmacy interns on the ward” (P-STAT 2). In this evaluation, PIs were also involved in medication reconciliation, the identification, resolution and prevention of drug-related problems, and the evaluation of the adherence to guidelines for antithrombotic prophylaxis in surgery patients [13].
The overall aim of this study was to evaluate the feasibility of involving PIs in monitoring PAP. Further objectives were to evaluate the involvement of PIs in various aspects of the management of antibiotic prophylaxis in surgery patients in German hospitals:
-
1.
perioperative and prolonged (postoperative) antibiotic prophylaxis, including antibiotics used and duration of antibiotic prophylaxis;
-
2.
adherence of PAP in surgery patients according to current guidelines;
-
3.
calculation of the cost of antibiotics in cases of non-adherence with the guidelines.
Methods
Setting
The study was conducted in 14 different hospital wards of seven hospitals in Germany (5 community hospitals and 2 university hospitals). The clinics of the participating wards were general and visceral surgery (n = 5), gynaecology (n = 1), orthopaedic and accident surgery (n = 6), otolaryngology (n = 1), and urology (n = 1).
Each participating hospital ward was required to provide its own PAP guideline according to the evidence-based guidelines [14];
for example,
-
1.
Cefuroxime 1,500 mg intravenous (IV) (hospital ward A) and cefazoline 2,000 mg IV (hospital ward B) in patients with total joint replacement, or
-
2.
amoxicillin/clavulanic acid 2.2 g IV (hospital ward C) or ceftriaxone 2 g IV (hospital ward D) in patients with cholecystectomy.
In generally, the guideline was defined by each clinic—in some cases involving clinical pharmacists and/or microbiologists. Before initiation of the study the guideline was checked by the study coordinator.
Pharmacy interns
Twenty-seven PIs spent 6 months of a 12-month mandatory internship working on a hospital ward—either from May to October 2008 or from November 2008 to April 2009—within the framework of the project “Pharmacy interns on the ward” [13]. The hypothesis was that their work would result in improvements in the quality and safety of the medication use process. One part of the study was the evaluation of the PAP and adherence to PAP guidelines.
Each hospital pharmacy (n = 5) or community pharmacy supplying a hospital (n = 2) provided internships for four PIs (2 PIs every half-year). One of the participating PIs dropped out before the internship started. Prior to the initiation of the study, both PIs and attending pharmacists received a 2-day training course in pharmaceutical care, medication reconciliation, antithrombotic guidelines, PAP, and antibiotic therapy. The PIs were supervised by pharmacists with experience in clinical pharmacy practice.
Patients
All patients admitted to the hospital wards between June 2008 and April 2009 were evaluated irrespective of the main diagnosis. The following aspects were documented from the patients’ medical records in the pre- and postoperative period: demographic data, main diagnosis/indication for surgery, duration of surgery, co-morbidities, renal function, antibiotic agent(s) received, dosage, route of administration and number of antibiotic applications during the surgery, and the duration of antibiotic prophylaxis postsurgery. Patients who did not receive any antibiotic prophylaxis during the hospital visit (no antibiotic prophylaxis was prescribed by the attending physician) were also included in the study cohort.
Adherence to the PAP guidelines was checked for both type of antibiotic drug and duration of PAP [14, 15]. Adherence to the guideline was defined as a correspondence between the prescribed antibiotic drug and duration of treatment and the guideline implemented by the respective hospital ward. Each deviation from the prescribed antibiotic and/or duration of PAP was defined as non-adherence. In cases of non-adherence, no pharmaceutical intervention by the PIs was undertaken because the study was planned only as an “as–is” analysis. Prolonged use of an antibiotic prophylaxis was considered to be a deviation in the duration of PAP as defined in the guideline—especially with respect to the use of antibiotics for more than 24 h after surgery.
The potential cost savings related to antibiotic use, personnel and material was calculated in cases where the actual duration of the antibiotic prophylaxis exceeded the duration set down in the guidelines. For calculating antibiotic costs, average prices of the syndicate from one of the participating hospitals were used. Data collection took place from May 2008 to April 2009; accordingly, average prices from the fourth quarter 2008 were used. Personnel and material costs were also included for cases of unnecessary IV administration (personnel costs 4.30 euro, calculated for an average lead time for preparing the IV infusion of 12.9 min, as measured on 7 hospital wards [16]; material costs: 0.70 euro, as calculated for infusion line, canula, syringe, resolvent).
All data were checked independently for face validity by two experienced clinical pharmacists on the basis of the available documented patient data, primary diagnosis, or operative indication, duration of surgery, and antibiotic regimen.
Patient anonymity was ensured so that no patient-specific data were recorded. Therefore, institutional review board approval was not required.
Statistical analyses
Statistical analyses were performed using PASW ver. 18 software (Predictive Analytics Software; SPSS, Chicago, IL). Data are presented as the mean and standard deviation (SD) or as the median and interquartile range (IQR).
Results
Study population
From June 2008 to April 2009, a total of 6,167 patients in 14 hospital wards were enrolled for the evaluation of antibiotic prophylaxis. The patients’ characteristics are given in Table 1. The mean age of the patients was 58.3 ± 19.6 years; 47.1% were male.
The distribution of the patients who underwent surgery, the duration of surgery, the patients who received peri- and/or postoperative antibiotic prophylaxis, and the adherence to guidelines are shown in Fig. 1.
Antibiotic prophylaxis
Data from 3,730 patients were available for evaluating peri- and/or postoperative antibiotic prophylaxis; in 14 patients it was unclear whether an antibiotic prophylaxis had been given (see Fig. 1).
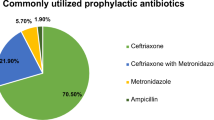
Twenty-nine different antibiotics were used for peri- and post-operative prophylaxis. The five most commonly used antibiotics were, beginning with the most frequently used, (1) cefuroxime (-axetil) IV or oral; (2) cefazoline IV; (3) amoxicillin/clavulanic acid IV or oral; (4) ciprofloxacin IV or oral; (5) ceftriaxone IV.
Of the 3,730 patients, 1,227 (32.9%) received prolonged (postoperative) antibiotic prophylaxis. On the different hospital wards participating in the study, the mean percentage of patients receiving a prolonged antibiotic prophylaxis was 29.9% (range 0.3–94.9%). On average, these patients received an antibiotic prophylaxis for 4.2 ± 2.8 days (minimum 1, maximum 21 days; see Table 2).
Adherence of PAP in surgery patients to current guidelines
Of the 6,167 patients enrolled, 5,064 patients underwent surgery and were available for evaluation. The results are summarized in Fig. 2. Guidelines for antibiotic prophylaxis were followed in 70.7% (IQR 47.4–78.3%, minimum 4.5%, maximum 84.9%) of the patients.
Potential cost savings in cases of non-adherence with guidelines
Potential cost savings were calculated for all 758 patients receiving an antibiotic prophylaxis for a longer duration than that defined by the implemented guidelines. Average potential cost savings for each of these antibiotic prophylaxis were calculated to be 43.84 ± 21.74 euro per patient in cases of non-adherence (see Fig. 3).
Discussion
To the best of our knowledge, this is the first evaluation of the adherence to guidelines for antibiotic prophylaxis in surgery patients in which PIs were involved in the monitoring process.
The results of our study show that PIs, under the supervision of a clinical pharmacist, may contribute substantially towards collecting data for a quality-assured PAP management. PIs can be integrated in the procedure of PAP by documenting the main diagnosis or the indication for surgery, the duration of surgery, and the antibiotic drug, including dosage, route of application and duration of antibiotic use. Accordingly, they can evaluate the antibiotic prophylaxis on the basis of the guideline to assess the adherence in daily practice. Furthermore, PIs may even initiate a pharmaceutical intervention after consultation with a clinical pharmacist.
The evidence for efficacy of PAP is well established. The results of this multicentre evaluation show that more than 70% of the patients received an antimicrobial prophylaxis. However, there is still considerable room for improvement, especially in the process around the discontinuation of the antimicrobial prophylaxis. The majority of published evidence demonstrates that the use of antimicrobial prophylaxis after wound closure is unnecessary, and most studies comparing single-dose prophylaxis with multidose prophylaxis have not shown benefit of additional doses [17]. Furthermore, the application of single-dose prophylaxis results in a decreased total antibiotic use [DDD (defined daily doses) per 1,000 patient days] [18].
Prolonged use of prophylactic antibiotics is associated with the emergence of resistant bacterial strains [17]. On average, 30% of the patients in our study received prolonged antibiotic prophylaxis. Many studies have demonstrated deviations in PAP guidelines in the treatment of up to 87.7% of patients [3, 9–11, 19]. Prolonged prophylaxis may be caused by the surgeon’s fear of SSIs [3] and the great uncertainty on the duration of PAP [20].
A wide spectrum of antibiotics are available for use as peri- and postoperative prophylaxis. The two most commonly used antibiotics in our evaluation, cefuroxime and cefazoline, meet the criteria for an optimal antibiotic for perioperative antibiotic prophylaxis, such as good tissue penetration, activity against Staphylococcus spp. and Streptococcus spp, lack of toxicity, and low costs [21].
On the wards participating in our study, the adherence to the respective guideline for antibiotic prophylaxis ranged from 4.5 to 84.9%. Adherence rates of >80% on three hospital wards may suggest that the treating physicians were familiar with the guidelines and aware of multidrug resistant bacteria selection in cases of prolonged prophylaxis. However, there were five wards with adherence rates of <50%, with one ward showing an adherence rate of only 4.5%. We did not ask the surgeons for the reasons for the non-adherence; known potential reasons are the fear of SSIs, the complexity of the operation, the extended duration of the operation and the insertion of catheters. Data from large and cohort studies have shown that the adherence to PAP guidelines is suboptimal in many hospitals [17, 22, 23]. A questionnaire-based analysis by Pan et al., conducted in 24 Italian cardiac surgical units, revealed that the adherence to strongly evidence-based recommendations, grade IA, was also sub-optimal and that the scientific evidence of recommendation did not directly correlate with its implementation on the wards [24]. In a German study investigating the practice of PAP, Dettenkofer et al. observed that none of the eight participating hospitals had written standards that guided the use of PAP [20, 25]. Several strategies are feasible to increase adherence and reduce the number of prolonged antibiotic prophylaxis, such as written standards according to evidence-based guidelines, education, training, simplification of the guidelines, implementation of checklists which cover the entire surgical pathway, especially the administration of antibiotic prophylaxis and/or the use of pre-printed stickers naming the drug, dosage, route of administration and time-period of application [26, 27].
Published data on the unnecessary costs associated with the administration of prolonged antibiotic prophylaxis are limited. To the best of our knowledge, there are no data available on the calculation of unnecessary costs including personnel and material costs. Our data show that if the guidelines were followed, an average of about 44 euro may be saved for each patient.
The results of antibiotic prophylaxis in daily practice are useful for physicians, clinical pharmacists as well as for the entire clinic: it is essential to discuss these results in surgical teams. Efforts should be made to improve each ward’s adherence to its respective guideline.
Involving PIs in monitoring adherence to guidelines for antibiotic prophylaxis is feasible, and PIs may play an important role in the quality control of the management of antibiotic prophylaxis. Furthermore, involving PIs in a multidisciplinary team on a hospital ward gives them the opportunity to gain valuable clinical experience. Due to the fact that monitoring antibiotic prophylaxis was only a part of the main study, the burden of work for the PIs involved in this study was very high. Therefore, some issues were not evaluated, such as the timing of the first dose of antibiotic and the number, severity and duration of SSIs, although it would have been interesting to do so.
Limitations
There were no data available on the timing of the first dose of antibiotic before incision and the number of SSIs. In addition, information on PI interventions in cases of prolonged antibiotic prophylaxis was not available. However, as mentioned, the evaluation of adherence to guidelines for antibiotic prophylaxis was only one aspect of the P-STAT 2 project.
In conclusion, this prospective evaluation revealed that many patients do not receive appropriate antibiotic prophylaxis despite the fact that guidelines are available. PIs may play an important role in the management of antibiotic prophylaxis by monitoring the status of the wards’ adherence with existing guidelines. However, a variety of challenges has eventually to be considered in order to achieve a quality-assured process.
Abbreviations
- IV:
-
Intravenous
- n/a:
-
Not available
- PAP:
-
Perioperative antibiotic prophylaxis
- PI:
-
Pharmacy intern
- SSI:
-
Surgical site infection(s)
References
Auerbach, AD. Prevention of Surgical Site Infections. In: Shojania KG, Duncan BW, McDonald KM, et al. eds. Making health care safer: A critical analysis of patient safety practices. Evidence Report/Technology Assessment No. 43 (prepared by the University of California at San Francisco, Stanford Evidence-based Practice Center under Contract No. 290-97-0013). AHRQ Publication No 01-E058. Agency for Healthcare Research and Quality, Rockville. 2001; pp 221–44.
Burke JP. Infection control—a problem for patient safety. N Eng J Med. 2003;348:651–6.
Tourmousoglou CE, Yiannakopoulou EC, Kalapothaki V, Bramis J, Papadopoulos JS. Adherence to guidelines for antibiotic prophylaxis in general surgery: a critical appraisal. J Antimicrob Chemother. 2008; doi:10.1093/jac/dkm406.
Gaynes RP, Culver DH, Horan TC, Edwards JR, Richards C, Tolson JS. Surgical Site Infection (SSI) rates in the United States, 1992–1998: The National Nosocomial Infections Surveillance System Basic SSI Risk Index. Clin Infect Dis. 2001; doi:10.1086/321860.
Gastmeier P, Geffers C. Nosokomiale Infektionen in Deutschland: Wie viele gibt es wirklich? [Nosocomial infections in Germany: What are the numbers, based on the estimates for 2006?]. Dtsch Med Wochenschr. 2008;133:1111–5.
Cheadle WG. Risk factors for surgical site infection. Surg Infect. 2006;7:s7–11.
Akalin HE. Surgical prophylaxis: the evolution of guidelines in an era of cost containment. J Hosp Infect. 2002; doi:10.1053/jhin.2001.1121.
Hecker MT, Aron DC, Patel NP, Lehmann MK, Donskey CJ. Unnecessary use of antimicrobials in hospitalized patients: current patterns of misuse with an emphasis on the antianaerobic spectrum of activity. Arch Intern Med. 2003;163:972–8.
Miliani K, L’Heriteau F, Astagneau P, on behalf of the INCISO Network Study Group. Non-compliance with recommendations for the practice of antibiotic prophylaxis and risk of surgical site infection: results of a multilevel analysis from the INCISO Surveillance Network. J Antimicrob Chemother. 2009; doi:10.1093/jac/dkp367.
Yalcin AN, Serin S, Gurses E, Zencir M. Surgical antibiotic prophylaxis in a turkish university hospital. J Chemother. 2002;14:373–7.
Al-Momany NH, Al-Bakri AG, Makahleh ZM, Wazaify MMB. Adherence to international antimicrobial prophylaxis guidelines in cardiac surgery: a Jordanian study demonstrates need for quality improvement. J Manag Care Pharm. 2009;15:262–71.
Gerdemann A, Griese N, Schulz M. Pharmacy interns on the ward—a pilot study. Pham World Sci. 2007; doi:10.1007/s11096-005-5044-z.
Hohmann C, Radziwill R, Eickhoff C, Schulz M. Evaluation der Tätigkeit von Pharmaziepraktikanten auf Station (P-STAT 2) [Pharmacy interns on the ward (P-STAT 2)]. Krankenhauspharmazie. 2008;29:393–6.
Working Group “Hygiene in Hospital and Practice” of AWMF. Perioperative antibiotic prophylaxis. 2009. http://www.uni-duesseldorf.de/AWMF/ll/029-022.htm. Accessed: 07 March 2011.
Wacha H, Hoyme U, Isenmann R, Kujath P, Lebert C, Naber K, Salzberger B. Perioperative Antbiotika-Prophylaxe [Perioperative antibiotic prophylaxis. Evidence based guidelines by an expert panel of the Paul Ehrlich Gesellschaft]. Chemother J. 2010;19:70–84.
Optifastprogramm-Kalkulation der Kosten. 2006.
Bratzler DW, Houck PM, for the Surgical Infection Prevention Guidelines Writers Workgroup. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Clin Infect Dis. 2004;38:1706–15.
Meyer E, Schwab F, Pollitt A, Bettolo W, Schroeren-Boersch B, Trautmann M. Impact of a change in antibiotic prophylaxis on total antibiotic use in a surgical intensive care unit. Infection. 2010; doi:10.1007/s15010-009-9115-2.
Lallemand S, Thouverez M, Bailly P, Bertrand X, Talon D. Non-observance of guidelines for surgical antimicrobial prophylaxis and surgical-site infections. Pharm World Sci. 2002;24:95–9.
Dettenkofer M, Forster DH, Ebner W, Gastmeier P, Rüden H, Daschner FD. The practice of perioperative antibiotic prophylaxis in eight German hospitals. Infection. 2002; doi:10.1007/s15010-002-2170-6.
Marculescu CE, Osmon DR. Antibiotic prophylaxis in orthopedic prosthetic surgery. Infect Dis Clin N Am. 2005; doi:10.1016/j.idc.2005.07.002.
Bratzler DW, Houck PM, Richards C, Steele L, Dellinger EP, Fry DE, Wright C, Ma A, Carr K, Red L. Use of antimicrobial prophylaxis for major surgery: baseline results from the National Surgical Infection Prevention Project. Arch Surg. 2005;140:174–82.
Silver A, Eichorn A, Kral J, Pickett G, Barie P, Pryor V, Dearie MB. Timeliness and use of antibiotic prophylaxis in selected inpatient surgical procedures. Am J Surg. 1996;171:548–52.
Pan A, Ambrosini L, Patroni A, Soavi L, Signorini L, Carosi G, Santini, C. Adherence to surgical site infection guidelines in Italian cardiac surgery units. Infection. 2009; doi:10.1007/s15010-008-7474-8.
Ruef C. Perioperative antibiotic prophylaxis—Still room for improvement. Infection. 2002; doi:10.1007/s15010-002-7302-5.
de Vries E, Dijkstra L, Smorenburg S, Meijer RP, Boermeester M. The SURgical PAtient Safety System (SURPASS) checklist optimizes timing of antibiotic prophylaxis. Patient Saf Surg. 2010; doi:10.1186/1754-9493-4-6.
Ritchie S, Scanlon N, Lewis M, Black PN. Use of a preprinted sticker to improve the prescribing of prophylactic antibiotics for hip fracture surgery. Qual Saf Health Care 2004; doi:10.1136/qshc.2003.009696.
Acknowledgments
We thank all participating pharmacies: Dom-Apotheke, Essen; Asklepios Kliniken Hamburg GmbH; Waisenhaus-Apotheke, Halle; Universitätsklinikum Heidelberg; Klinikum Fulda gAG; Klinikum rechts der Isar der TU München; and Dr.-Horst-Schmidt-Kliniken GmbH, Wiesbaden (Germany) and all pharmacy interns for their valuable contributions. We thank Christiane Sauerwein (ZAPP, ABDA, Berlin) for generating the database and her contribution in the analysis process and Susanne vom Scheidt (ZAPP, ABDA, Berlin) for her support in running the study. The main sponsor of this study was the Federal Union of German Associations of Pharmacists (ABDA), Berlin, Germany; the co-sponsor was Dr. August und Dr. Anni Lesmüller-Foundation, Munich, Germany.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hohmann, C., Eickhoff, C., Radziwill, R. et al. Adherence to guidelines for antibiotic prophylaxis in surgery patients in German hospitals: a multicentre evaluation involving pharmacy interns. Infection 40, 131–137 (2012). https://doi.org/10.1007/s15010-011-0204-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-011-0204-7