Abstract
Multiple sclerosis (MS) is the most common inflammatory demyelinating disease in the central nervous system. It is one of the major causes of disability in young adults. Early diagnosis and treatment of this disease could decrease later disability and additional costs. In this cross-sectional analytical study, a total of 351 patients were selected from among the multiple sclerosis patients that went to MS clinic or neurologic clinic in 1990–2016. Data were collected and analysed by SPSS v16. This study was conducted on 82.6% females and 17.4% males. Family history of MS was positive in 12.8% of cases. Mean time of onset of symptoms till first medical visit was 3.25 months. Mean time from first medical visit to diagnosis was 14.98 months. Mean time from onset of symptoms till diagnosis was 18.01 months and the mean time from onset of symptoms till initiation of treatment was 18.73 months. Also, 29.3% of cases had delay in first medical visit and 42.2% of cases had delay in diagnosis of MS more than 6 weeks from first medical visit. Overall, delay in first medical visit and diagnosis of MS has decreased over the years. However, there is still delay in diagnosis of MS. Factors associated with delay are low education, male gender, living in rural areas, primary progressive MS, age at MS diagnosis and first clinical symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is a disease of the cranial–spinal system, usually manifested in relapsing attacks by a variety of symptoms. The most common symptoms include motor disturbances (paresis, tremor, and spasms), sensory changes, optic neuritis, other cranial disorders like diplopia, and disequilibrium [1, 2]. It may be associated with less common symptoms like urinary disturbances. MS symptoms begin to manifest at the age of 20–45 years [3]. The mean age of symptoms manifestation is 5 years earlier in women compared to men. In five present of patients, the condition begins before the age of 18 years. The female-to-male proportion of affliction with MS is 1.77.
The incidence and prevalence of MS is increasing in Iran [4]. According to some studies on MS, the prevalence rate is 54.51 present and the incidence rate is 5.87 per 100,000 individuals [5]. There were 1100 MS patients in Hamadan province, Iran in 2013. The prevalence rate of MS in Hamadan is 62.56 per 100,000 individuals [4], being one of the main causes of disability among the youth [6]. Besides, 50 present of the patients need help to walk after 15 years of the onset of symptoms [7]. Although MS patients will rarely experience few symptoms, they mostly will suffer from disability in the course of time due to incomplete recovery induced by relapsing attacks and conversion of the disease to the progressive MS [3]. It is associated with significant economical load. The national annual costs of MS are estimated at 6.8–11.9 million USD (almost 34,000 USD per patient) [8]. The MS drugs are among the most expensive commercially available medicines imposing high costs on patients and healthcare system [9,10,11,12].
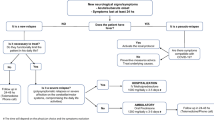
Many studies have indicated that the early diagnosis and prompt treatment of the condition can prevent its rapid progression and hinder disability [13,14,15,16]. There is inflammation and demyelization in the early stages of the disease; however, neuro-degeneration is dominant in the later course of the disorder, thus reducing greatly chances of remyelination [17]. Moreover, slowing down the speed of MS progression diminishes the costs imposed on patients and healthcare system [10]. Some evidence suggests that all available drugs produce a better response to MS in the initial stages of the condition [18, 19]. All clinical trials on clinically isolated syndrome (CIS) have demonstrated that prompt treatment decreases chances of progression of the disease to the definite form of MS, and reduces its progression on the basis of MRI evidence [15, 16 , 20,21,22]. The National Institute of Clinical Excellence (NICE) recommends a delay of 6 weeks between the first manifestation of symptoms and the first neurological assessment and a delay of 6 weeks between the neurological assessment and diagnosis.
The early diagnosis and treatment of MS is of utmost significance. Therefore, this study provided a better analysis of the diagnostic process in MS patients to reduce their disability and diminish the imposed costs.
Subjects and methods
A total of 351 MS patients presenting to MS Clinic and Neurology Clinic at Sina Hospital in Hamadan, Iran during 1990–2016 participated in this observational, cross-sectional and analytical study. They were selected using convenient sampling strategy. All patients were diagnosed with MS between 1990 and 2016, and the available data were evaluated. MS was diagnosed with clinical examination, magnetic resonance imaging (MRI), lumbar puncture (LP), and visual evoked potential (VEP) using McDonald criteria. The required data were collected through Expanded Disability Status Scale (EDSS). EDSS data of patients previously diagnosed with MS were extracted from their clinical record by a neurologist. Written informed consent was obtained from patients before making use of the information given in the questionnaires including age, gender, date of birth, place of residence, occupation, date of onset of symptoms, type of primary symptoms, date of first visit to physician, physician of the first visit (neurologist or non-neurologist), date of diagnosis, date of initiation of treatment, and family history of affliction with MS.
The patients were examined by a neurologist and the EDSS of each patient was estimated. This is a criterion for measuring the level of disability in MS patients that investigates the rate of changes in sensory–motor disability in the course of time using a score ranging from 0 to 10. The inclusion criteria were: all MS patients with definite diagnosis of the disorder on the basis of clinical examination and MRI, and inclination for voluntary participation. Also, the exclusion criteria were: lack of inclination for participation, impossibility of patient follow-up, and deficient patient records and questionnaires. On the basis of a study conducted by Adamec et al. [24] entitled “Delay in the Diagnosis of Multiple Sclerosis in Croatia”, the sample volume was estimated at 351 patients using sample volume proportions formula.
Statistical analysis
The data were analysed using SPSS v16. The level of statistical significance was set at p < 0.05. The quantitative variables with normal distribution were reported with mean and SD, and those without normal distribution were described using median and range of mid-quartiles. The qualitative variables were described with ratio and percentage. In analytical statistics, the length of delay in clinic presentation, delay in diagnosis of MS and delay in treatment were explored in both groups using independent-sample t test (for data with normal distribution) and Mann–Whitney test (for data with non-normal distribution). To compare these values among multiple groups like occupational groups, education levels and types of diseases, analysis of variance (ANOVA) and Kruskal–Wallis were run for normally distributed data and non-normally distributed data, respectively.
Results
In this cross-sectional analytical study, 61 (17.4%) patients were male and 290 (82.6%) were female. The female-to-male proportion was 4.75. The mean age of onset of MS was 30.70 ± 10.17 years in males and 28.92 ± 8.15 years in females. Additionally, the highest prevalence of the disease occurred in 20–29 years of age with 46.8 percent frequency. The family history for MS was positive in 45 cases (12.8%) of which 30 cases (66.67%) pertained to first-degree relatives and 15 cases (33.33%) to second-degree relatives. Besides, 26.8 percent (94) of patients were single, 68.9 percent (242) were married, and 4.3 percent (15) were divorced.
Regarding place of residence, 15.4 percent (54) of patients lived in rural and 84.6 percent (297) in urban regions. Regarding education level, 257 patients (72.3%) held high school diploma or higher and 94 patients (27.7%) had education less than diploma (elementary or middle school). As for occupational status, 89 patients (25.4%) were employed, 179 patients (51.1%) were housekeepers, 3 patients (0.6%) were unemployed, and 79 patients (22%) had changed their job or left it due to disease. Moreover, clinical symptoms of MS were first initiated in 41 percent of patients during 2012–2016. In other patients, the symptoms were first manifested in 2011 or before.
The most prevalent primary symptoms of MS among the patients were sensory symptoms with 53.3 percent and optic neuritis with 30.5 percent rate of prevalence. Regarding type of disease, “relapsing–remitting” was the most common type of MS, followed by “secondary-progressive” with 26.8 percent rate of prevalence ranking the second, and “primary-progressive” with 5.4 percent rate of prevalence ranking the third. At the onset of disease, the patients presented most frequently to neurologists (63.2%), general practitioners (GP) (15.4%) and ophthalmologists (13.1%).
The mean delay between onset of clinical symptoms and visiting the physician was 3.25 months, between physician visit and MS diagnosis was 14.98 months, between onset of symptoms and diagnosis was 18.01 months, and between onset of MS and onset of treatment was 18.73 months. Moreover, 70.7 percent of patients visited the physician during 6 weeks after the onset of symptoms, 29.3 percent delayed visit to the physician, 57.8 percent achieved diagnosis during 6 weeks after visiting the physician, 42.2 percent had more than 6 weeks of delay in diagnosis, and 55.8 percent achieved diagnosis during 3 months after the onset of symptoms.
As the Kolmogorov–Smirnov test indicated non-normal distribution of data (p = 0.000), non-parametric Kruskal–Wallis test was used to compare the mean delay between onset of symptoms and diagnosis in various years, the results of which showed that the mean delay between the onset of symptoms and diagnosis was significantly reduced with the passage of time (p = 0.000) (Table 1).
The patients’ EDSS mean at diagnosis was 0.86 with standard deviation of 1.10, median of 0.00, maximum of 5.0 and minimum of 0.00. As the Kolmogorov–Smirnov test showed the mean delay between onset of symptoms and diagnosis and the EDSS mean at diagnosis were not normally distributed (p = 0.00), Mann–Whitney test was used in this regard, the results of which revealed that the EDSS mean at diagnosis in females was significantly lower, compared to males (p = 0.023). According to the Kolmogorov–Smirnov test revealing the mean delay between onset of symptoms and diagnosis and the EDSS mean at diagnosis was non-normally distributed (p = 0.000), the results of Kruskal–Wallis test indicated a significant difference between mean delay between onset of symptoms and diagnosis among different education levels (p = 0.000).
Based on the results of Mann–Whitney test, the EDSS mean at diagnosis was significantly smaller in city, compared to villages (p = 0.017). The results of Kruskal–Wallis test also indicated that the EDSS mean between onset of symptoms and diagnosis was significantly greater in individuals aged 40 + years (p = 0.004).
As the Kolmogorov–Smirnov test showed the EDSS mean at diagnosis was not normally distributed (p = 0.000), Kruskal–Wallis test was run to compare the EDSS mean at diagnosis among different types of MS, which indicated a significant difference in this regard (p = 0.000). Furthermore, Kruskal–Wallis test revealed a significant difference in the EDSS mean at diagnosis and between mean onset of symptoms and diagnosis among various types of MS (p = 0.000) (Table 2).
Based on Kruskal–Wallis test, the mean delay between onset of symptoms and diagnosis and the EDSS mean at diagnosis were significantly smaller in optic neuritis, compared to other symptoms (p = 0.000). Also, the EDSS mean at diagnosis and the mean delay between onset of symptoms and diagnosis were significantly greater in motor symptoms than in other symptoms (Table 3).
It should be noted that some patients manifested more than one symptom at the onset of disease. Regarding the non-normal distribution of mean delay between onset of symptoms and diagnosis and the EDSS mean at diagnosis based on Kolmogorov–Smirnov test (p = 0.000), Spearman correlation was conducted to investigate the association between mean delay between onset of symptoms and diagnosis and EDSS mean at diagnosis indicating a direct positive correlation (p = 0.000, r = 0.2). In other words, as the delay between onset of symptom and diagnosis increases, the EDSS mean at diagnosis also goes up. Finally, with increasing age of onset of MS, the EDSS mean at diagnosis significantly increased indicating a direct correlation between the two using Spearman correlation (p = 0.006, r = 0.14).
Discussion
This study investigated the delay in visiting doctors and diagnosis of MS patients. Considering the increasing prevalence and incidence of MS in recent years and the necessity of early diagnosis and treatment of the disorder to decrease patients’ disability and the imposed costs on them, investigating the delay in MS diagnosis is of utmost importance.
In this study, the mean delay between onset of symptoms and diagnosis was 18.01 months and the median was 2.0 months. The EDSS mean of patients at diagnosis was 0.86 ± 1.10, whereas in the study of Fernandez et al. (2010) conducted in Spain, the delay between onset of symptoms and diagnosis was 24.9 months and EDSS mean at diagnosis was 1.91 ± 1.32 [23]. The difference may be attributed to the possibility of directly visiting neurologists in Iran and the use of different diagnostic criteria like Poser in Spain. In a study conducted by Adamec et al. (2013) in Croatia, 61.5 percent of patients presented to neurologists during six weeks and 64.1 percent of patients achieved diagnosis during 6 weeks on the basis of NICE guideline [24].
In the present study, 70.7 percent of patients visited the physician during 6 weeks after onset of symptoms and 57.8 percent of patients achieved diagnosis during 6 weeks of presenting to doctor. In a study done by Kelly et al. (2011) in Ireland, 78 percent of patients visited the neurologists during 6 weeks and 53 percent of patients achieved diagnosis during 6 weeks [25]. In this study, 69.2 percent of the patients (243 cases) achieved diagnosis in the first year of onset of disease, whereas in a study by Osama Al Wutayd (2015) in Saudi Arabia, only 14 percent of patients achieved diagnosis in the first year, indicating the more appropriate status of the diagnostic process in Hamadan province [26].
Generally, the present study showed some delay between onset of symptoms and MS diagnosis on the basis of NICE guideline, which might be attributed to insufficient awareness of people about MS, late presentation to clinic, visiting non-neurologists, non-neurologist physicians’ insufficient awareness about MS, numerous misleading signs and symptoms of the disease, the use of different diagnostic criteria, and insufficient continuity of visiting the doctor.
The mean delay between onset of symptoms and diagnosis has significantly decreased over time. The mean age of patients at the time of onset of disease was 29.35 years in the present study, whereas it was 33.7 years in a study carried out by Kingwell et al. (2010) [27]. In a study conducted by Fernandez et al. (2010) in Spain, the mean age of patients at the onset of disease was 31.2 years [23]. In a study carried out by E’temadifar et al. (2010) in Iran, this value was 28.2 years [4]. In a study conducted by Majidi Nasab et al. during 2005–2011, this value was 27.6 years.
Considering the lower age of onset of MS in Iran and its increasing prevalence in recent years, it is recommended that some preventive measures be taken to reduce the controllable risk factors of MS, like enrichment of foods with nutrients and vitamin D. The mean delay between onset of symptoms and diagnosis was greater in men than in women (21.95–16.97 months). With regard to the statistical significance of EDSS mean at diagnosis in men compared to women, it is recommended to increase men’s awareness of the importance of early presentation to the physician after onset of symptoms.
The mean delay between onset of symptoms and diagnosis was greater in villagers compared to citizens. I was also found the EDSS mean was significantly greater in villagers than in citizens. Thus, early referral of patients by general practitioners in villages and the necessity of holding MS re-education courses are highly important. The delay rate in visiting physicians after onset of symptoms is considerably higher in illiterate than in literate patients, indicating the importance of people’s awareness of early presentation to the doctor. On the other hand, the EDSS mean at diagnosis was greater in illiterate patients. In the present study, the rate of “primary progressive MS” was 5.4 percent, while this rate was 9.6 percent and 12.3 percent in two regions in a study done by Kingwell et al. [27] in Canada.
The mean delay between onset of symptoms and diagnosis was greater in “primary-progressive MS” compared to other types, being is line with the findings of Kingwell et al. [27]. The mean delay between onset of symptoms and diagnosis was significantly smaller in patients whose symptoms began with optic neuritis, compared to other symptoms. Finally, in the study of Fernandez et al. (2010) in Spain, onset of MS with optic neuritis led to early presentation to neurologists [23].
Conclusion
Totally, delay in visiting the doctor and late diagnosis after onset of symptoms of MS decreased over time, which might be due to the easier MS diagnostic procedures in more recent McDonald criteria, compared to previous criteria; however, there is still some delay in diagnosis. Factors affecting delay in MS diagnosis include low literacy level or illiteracy, the male gender, living in village, primary-progressive MS, and initial clinical signs and symptoms of MS. Regarding the fact that patients turn to various physicians and specialists in their first visit to treatment centers after the onset of symptoms of MS, physicians’ development programs and MS re-education courses may aid in the early diagnosis of the disorder and the subsequent disabilities and crippling. People’s increasing awareness about MS can greatly enhance early presentation to doctors after onset of symptoms. It is also suggested that this study be replicated in other regions of Iran to estimate the rate of MS attacks and subsequent disabilities in patients.
Limitations of the study
The limitations of the present study include errors in patient reminding, deficiencies in patients’ records, impossibility of investigation into primary MRIs, and impossibility of following up all the patients.
References
Ropper AH (2005) Adams and Victor’s principles of neurology: McGraw-Hill Medical Pub. Division New York
Daroff RB, Jankovic J, Mazziotta JC, Pomeroy SL (2015) Bradley’s Neurology in Clinical Practice E-Book: Elsevier Health Sciences
Merritt HH (2010) Merritt’s neurology: Lippincott Williams & Wilkins
Etemadifar M, Sajjadi S, Nasr Z, Firoozeei TS, Abtahi S-H, Akbari M et al (2013) Epidemiology of multiple sclerosis in Iran: a systematic review. Eur Neurol 70(5–6):356–363
Etemadifar M, Izadi S, Nikseresht A, Sharifian M, Sahraian MA, Nasr Z (2014) Estimated prevalence and incidence of multiple sclerosis in Iran. Eur Neurol 72(5–6):370–374
Noseworthy JH, Lucchinetti C, Rodriguez M, Weinshenker BG (2000) Multiple sclerosis. N Engl J Med 343(13):938–952
Weinshenker BG, Bass B, Rice G, Noseworthy J, Carriere W, Baskerville J et al (1989) The natural history of multiple sclerosis: a geographically based study: I. Clinical course and disability. Brain 112(1):133–146
Whetten-Goldstein K, Sloan FA, Goldstein LB, Kulas ED (1998) A comprehensive assessment of the cost of multiple sclerosis in the United States. Mult Scler 4(5):419–425
Campbell JD, Ghushchyan V, McQueen RB, Cahoon-Metzger S, Livingston T, Vollmer T et al (2014) Burden of multiple sclerosis on direct, indirect costs and quality of life: National US estimates. Mult Scler Relat Disord 3(2):227–236
Grima D, Torrance G, Francis G, Rice G, Rosner A, Lafortune L (2000) Cost and health related quality of life consequences of multiple sclerosis. Mult Scler 6(2):91–98
Kobelt G, Berg J, Lindgren P, Fredrikson S, Jönsson B (2006) Costs and quality of life of patients with multiple sclerosis in Europe. J Neurol Neurosurg Psychiatry 77(8):918–926
Sobocki P, Pugliatti M, Lauer K, Kobelt G (2007) Estimation of the cost of MS in Europe: extrapolations from a multinational cost study. Mult Scler 13(8):1054–1064
Beck RW, Chandler DL, Cole SR, Simon JH, Jacobs LD, Kinkel RP et al (2002) Interferon β-1a for early multiple sclerosis: CHAMPS trial subgroup analyses. Ann Neurol 51(4):481–490
Jacobs LD, Beck RW, Simon JH, Kinkel RP, Brownscheidle CM, Murray TJ et al (2000) Intramuscular interferon beta-1a therapy initiated during a first demyelinating event in multiple sclerosis. N Engl J Med 343(13):898–904
Kappos L, Freedman MS, Polman CH, Edan G, Hartung H-P, Miller DH et al (2007) Effect of early versus delayed interferon beta-1b treatment on disability after a first clinical event suggestive of multiple sclerosis: a 3-year follow-up analysis of the BENEFIT study. Lancet 370(9585):389–397
Kappos L, Polman C, Freedman M, Edan G, Hartung H, Miller D et al (2006) Treatment with interferon beta-1b delays conversion to clinically definite and McDonald MS in patients with clinically isolated syndromes. Neurology 67(7):1242–1249
Franciotta D, Salvetti M, Lolli F, Serafini B, Aloisi F (2008) B cells and multiple sclerosis. Lancet Neurol 7(9):852–858
Comi G (2009) Shifting the paradigm toward earlier treatment of multiple sclerosis with interferon beta. Clin Ther 31(6):1142–1157
Goodin D, Bates D (2009) Treatment of early multiple sclerosis: the value of treatment initiation after a first clinical episode. Mult Scler 15(10):1175–1182
Edan G, Kappos L, Montalbán X, Polman C, Freedman M, Hartung H-P et al (2013) Long-term impact of interferon beta-1b in patients with CIS: 8-year follow-up of BENEFIT. J Neurol Neurosurg Psychiatry 85(11):1183–1189
Kennedy P (2013) Impact of delayed diagnosis and treatment in clinically isolated syndrome and multiple sclerosis. J Neurosci Nurs 45(6):S3–S13
Noyes K, Weinstock-Guttman B (2013) Impact of diagnosis and early treatment on the course of multiple sclerosis. Am J Manag Care 19(17 Suppl):s321–s331
Fernández O, Fernández V, Arbizu T, Izquierdo G, Bosca I, Arroyo R et al (2010) Characteristics of multiple sclerosis at onset and delay of diagnosis and treatment in Spain (the Novo Study). J Neurol 257(9):1500–1507
Adamec I, Barun B, Gabelić T, Zadro I, Habek M (2013) Delay in the diagnosis of multiple sclerosis in Croatia. Clin Neurol Neurosurg 115:S70–S72
Kelly S, Chaila E, Kinsella K, Duggan M, McGuigan C, Tubridy N et al (2011) Multiple sclerosis, from referral to confirmed diagnosis: an audit of clinical practice. Mult Scler 17(8):1017–1021
Wutayd OA (2016) Delay in the diagnosis of multiple sclerosis. Int J Healthcare Sci 4(2):427–428
Kingwell E, Leung AL, Roger E, Duquette P, Rieckmann P, Tremlett H (2010) Factors associated with delay to medical recognition in two Canadian multiple sclerosis cohorts. J Neurol Sci 292(1):57–62
Acknowledgements
The authors give their special thanks to the members of Committee of Ethics at Hamadan University of Medical Sciences for approving the research proposal. We also extend our thanks to Deputy in Research at the university.
Funding
The study was funded by Research and Technology Vice-President, Hamadan University of Medical Sciences (No. 9512107703).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The research proposal was approved by Committee of Ethics in Human Research at Hamadan University of Medical Sciences under ethics code no.: IR.UMSHA.REC.1395.586.
Informed consent
The participants were oriented with research goals and procedures and the patients took part in the study voluntarily after signing written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ghiasian, M., Faryadras, M., Mansour, M. et al. Assessment of delayed diagnosis and treatment in multiple sclerosis patients during 1990–2016. Acta Neurol Belg 121, 199–204 (2021). https://doi.org/10.1007/s13760-020-01528-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-020-01528-7