Abstract
We investigated the genetic background of early-onset epileptic encephalopathy (EE) using targeted next generation sequencing analysis. Thirty sporadic or familial cases associated with early-onset EE were included. An early-onset EE gene panel including sixteen genes (ARX, CDKL5, CNTNAP2, FOLR1, FOXG1, LAMC3, MBD5, MECP2, NTNG1, PCDH19, PNKP, SCN1A, SCN1B, SCN2A, STXBP1, KCNQ2) was constituted. Nine definite and three potential causal mutations in 30 cases (40 %) were identified. All mutations presented heterozygously except one. Five mutations had been previously detected (SCN1A c.842C > T (p.P281L), SCN1A c.4907G > C (p.A1636P), PCDH19 c.1091dupC (p.Y366LfsX10), CNTNAP2 c.416A > G (p.N139S), MBD5 c.3595G > A(p.Y1199R) while other seven were novel (SCN1A c.4907G > C (p.A1636P), SCN2A c.4633A > G (p.M1545 V), CDKL5 c.197_198delCT (p.L67QfsX23), FOXG1 c.*6C > T, KCNQ2 c.560c > A (p.S187Y), KCNQ2 c.835G > A (p.G279S), STXBP1 c.1105G > T (p.E369X)). Eight of 12 mutations were de novo. While the overall mutation detection rate was found 40 %, this ratio was 55.5 % (10 out of 18) and 16.6 % (2 out of 12) in patients born to nonconsanguineous parents and consanguineous parents, respectively. In conclusion, a selected gene panel approach including mainly de novo and channel-encoding genes will result in the detection of variants in isolated patients and support the channelopathy theory underlying epilepsy, while consanguineous families will remain less diagnosed. Targeted next generation sequencing approach is an efficient diagnostic tool in the detection of the genetic basis of early-onset EE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term epileptic encephalopathy (EE) was first used in ILAE 2001 classification; it was described as being “epileptiform abnormalities which may contribute to progressive dysfunction” [1]. A more detailed description of EE was given in an ILAE 2009 classification [2]. Epileptic encephalopathy embodies the notion that the epileptic activity itself may contribute to severe cognitive and behavioral impairments above and beyond what might be expected from the underlying pathology alone (e.g. cortical malformation), and that these can worsen over time.
EEs have produced a group of pharmacoresistant epileptic disorders which occurred at a critical period of brain development, and are characterized by cognitive dysfunction or decline with abnormal electroencephalography (EEG) findings. The persistent epileptic activity interferes with the natural development and function of the immature brain. EEs can appear at any time from the neonatal period through the adolescence but usually occur during the early infantile period.
The number of studies relating to the genetic background of EE has been increasing rapidly. As a direct result, several responsible genes playing important roles in brain development, neurotransmitter synthesis and release, structure or functions of membrane receptors and transporters have been identified [3, 4]. These studies have greatly improved our knowledge on the etiologies and pathophysiological mechanisms of EEs, but at the same time, have presented an increasingly complex picture.
In this study, we aimed to investigate the genetic background of early-onset EE by using targeted Next Generation Sequencing (NGS) analysis.
Participants and methods
Participants
Thirty-five cases having early-onset refractory seizures with global developmental delay and cognitive dysfunction and regularly followed at Child Neurology Division, Pediatrics Department of Ege University Faculty of Medicine were included in this study. Inclusion criteria were as follows: (1) Normal metabolic screening (blood for lactate, pyruvate, aminoacid and acyl carnitine, biotinidase, ammonia, urine for organic acid, cerebrospinal fluid for glucose, lactate, aminoacid), (2) Normal karyotype, (3) No mutation in antiquitin (ALDH7A1) gene analysis, (4) No known dysmorphologic syndromes, (5) Normal or nonspecific cranial magnetic resonance imaging (MRI) findings and normal cranial magnetic resonance spectroscopy (MRS).
Physical and neurological examinations were performed in all cases. Developmental states were evaluated by the Ankara Development Screening Test (adapted from the Denver Test for Turkish children) for the patients up to 72 months of age and the Wechsler Intelligence Scale for Children–Revised (WISC-R) who are over 6 years-old [5, 6]. The former test is appropriate for ages 0–72 months and evaluates fine motor, gross motor, language, and adaptive personal/social skills. Scores are given for these four skills and total development. Scores between age-normative values and 20 % of those values are taken as near normal and refers to IQ scores over 80. Scores between 20 and 30 % of age-normative values are recorded as being borderline and refer to IQ scores of 70–79. Scores less than 30 % of age normative values are scored as having significant delay. Total scores for general development are also recorded. Scores between 40 and 60 are appropriate for age, 21–39 shows mild-to-moderate delay, and ≤20 signifies severe delay [5].
The clinical data of the cases who were regularly followed up at Ege University Child Neurology outpatient and inpatient services were collected retrospectively. Their clinical and laboratory findings were reevaluated by the authors. All cases were then referred to an experienced geneticist, and their pedigrees constructed. From the 35 cases originally included in this study between September 2013 and October 2014, five cases were excluded. One case due to a mutation in antiquitin gene analysis, one case had a mutation in CDKL5 gene analysis (her blood sample was previously sent to another laboratory), two cases were diagnosed with static encephalopathy, and one case was found to have Pitt-Hopkins syndrome, clinically.
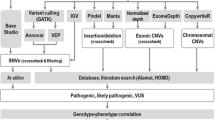
Genetic analysis
Sixteen early-onset EE related genes (ARX, CDKL5, CNTNAP2, FOLR1, FOXG1, LAMC3, MBD5, MECP2, NTNG1, PCDH19, PNKP, SCN1A, SCN1B, SCN2A, STXBP1, KCNQ2) which were previously reported in different studies were analyzed in 30 cases with early-onset EE [7–10]. These genes were analyzed on Illumina MiSeq platform using the targeted NGS approach. All variants found in this analysis were filtered out based on minor allele frequency (MAF) >1 % as in dbSNP(version 137), 1000 Genomes Poject, ESP 6500 Exome Project (https://esp.gs.washington.edu/drupal/), and ExAC v0.2 (http://exac.broadinstitude.org/) databases. Variants were filtered based on the presumed inheritance pattern. Afterwards, all variants were visually validated by an experienced researcher using Integrative Genomics Viewer (IGV) and clearly false positives were excluded. Variants found in the patients were then compared to the variants listed in various databases including Human Gene Mutation Database (HGMD) [11], as well as Ensembl and National Center for Biotechnology Information (NCBI) database. The pathogenicity of novel variants was predicted using in silico tools, SIFT [12], MutationTaster [13] and PolyPhen-2 [14]. Conservation of residues across species was evaluated by PhyloP algorithm and GERP [15, 16]. The Sanger sequencing method was used to confirm pathogenic variants found via NGS and to perform segregation analysis.
Local ethical committee approval was obtained, and a written informed consent was provided by all participants.
Results
Clinical features
Clinical and laboratory findings of the study group are outlined in Table 1. Thirty early-onset EE cases were included in this study. Ages ranged between 7 months-17 years (mean ± SD: 64 ± 52 months). Seventeen of thirty cases were female. All except two cases were born at term. Birth-weights varied between 2200 and 4000 (mean ± SD: 3231 ± 454) grams. Perinatal asphyxia was reported in eight of our group (27 %). Parental consanguinity was found in 12 cases (40 %). In five cases (Case 16, 17, 18, 21, 30), similar clinical findings were described in siblings. Family history also revealed either epilepsy or mental retardation (MR) in first/second degree relatives in five cases (Case 1, 2, 13, 14, 20). Sixteen cases were microcephalic. Neurological examination results were abnormal in 25 cases (83.3 %). Spastic tetraparesis, hypotonia, and optic atrophy were found in 11, 10 and, 8 cases, respectively. Movement disorders such as dyskinesia and ataxia were also found in four and two cases, respectively. Autistic features and hand stereotypies were observed in five cases (Case 9, 11, 12, 20, 24). All cases had developmental delay with varying severity.
Age at seizure onset varied between 1 day and 9 months (93 ± 85 days). Seizures began during the neonatal period in one-third of cases; six suffered seizures on the first day of life. Most cases (23/30) displayed more than one seizure type. The most frequent seizure type was infantile spasm (60 %). Six cases had solely infantile spasms. Generalized tonic/clonic/tonic–clonic seizures were seen in 18 of 30 cases. Myoclonic seizures, either generalized or focal, were observed in 6 cases, and 12 cases had partial seizures with or without generalization. Atypical absences were observed in only one case. Moreover, fever induced partial or generalized motor seizures were noted in five cases and four of them had recurrent febrile status.
Initial EEGs showed focal/multifocal epileptiform discharges in 21 (70 %), hypsarrhythmia in 4 (13 %), generalized spike and wave discharges in 2 (7 %), and suppression-burst in 2 (7 %) cases. Epileptiform activity was not observed in one case (Case 27). Five cases also had slowing of background activity.
Cranial MRI was found to be normal in about half of cases (13/30). Cranial MRI revealed cortical atrophy in 14 cases, cerebellar atrophy in two cases, and periventricular hyperintensity on T2 weighted/FLAIR images in two cases. One case had T2 hyperintense signal changes in the basal ganglia. In all cases, magnetic resonance spectroscopy (MRS) examination yielded negative results.
Sequencing results
Targeted gene sequencing revealed nine disease-causing variants (7 point mutations, 2 frameshift mutations) in 6 genes in 9 of 30 early-onset EE cases. One novel and two previously reported de novo variants, one of which are defined as disease-causing mutations in HGMD [11], were found in SCN1A gene in three different cases [17]. Five de novo novel variants were found in SCN2A, CDKL5, KCNQ2, and STXBP1 genes of five cases. Case 5 carried a previously defined damaging mutation in PCDH19 gene [18]. The mother of this patient was not available for segregation analysis. Potential causal variants identified in this study were found in three genes (FOXG1, CNTNAP2, and MBD5). Molecular results of the patients are outlined in Table 2. Novel mutations defined in this study were not found in 100 ethnically matched healthy controls and all were predicted to be pathogenic using in silico tools.
Clinical features of nine cases (Cases 1–9) having definite disease-causing variants in SCN1A, SCN2A, PCDH19, CDKL5, KCNQ2, and STXBP1 genes were in accordance with presumed clinical syndromes. All those cases were heterozygous for the variants detected.
The clinical findings and molecular results of the cases with potential causal variants (case 10, case 11, and case 12) are outlined below:
Case 10 was homozygous for a novel variation [c.*6C > T (g.28768755C > T)] in FOXG1 gene. Both parents were carried the novel variant heterozygously. This case has been followed up since 6 month-old as atypical Rett Syndrome. The heterozygous FOXG1 gene defects were defined in similar cases previously [19].
In case 11, a rare variant [c.416A > G (p.N139S)], which was previously reported as probably damaging was detected in the CNTNAP2 gene [20]. Segregation analysis showed that it was inherited from the unaffected father. Interestingly this case has displayed clinical findings compatible with Dravet syndrome.
Case 12, carried a very rare variation in MBD5 [c.3595G > A (p.Y1199R)] gene, which was inherited from unaffected father. Clinical features of this case were similar to the previously reported patients with MBD5 defects [21]. Family history revealed that three male siblings of her father had died due to unknown reasons during the neonatal period. She also had prominent dysmorphic features; these include thick/arched eyebrow, midface hypoplasia, thin and tented upper lip, open mouth, widely spaced teeth, prominent upper incisors and small hands (Fig. 1).
The overall mutation detection rate was 40 % in this study. This ratio was 55.5 % (10 out of 18) and 16.6 % (2 out of 12) in patients born to nonconsanguineous parents and consanguineous parents, respectively.
Discussion
Early-onset EEs are debilitating syndromes, which cause permanent developmental regression and intractable epilepsy. Although varying early-onset EEs are recognized by ILAE, many infants displaying similar clinical findings cannot be strictly categorized within the parameters of these syndromes. Genetic etiology is considered the principal factor responsible for these devastating epileptic disorders.
It has been reported that multiple genetic mutations can be responsible for the same EE, and specific gene mutations can also cause multiple syndromes. These findings indicate that differing underlying abnormalities using a common pathophysiologic pathway often result in a broad spectrum of clinical phenotypes.
In 30 cases with early-onset EE, we isolated twelve definite or potential causal variants. Kodera et al. [7] studied 53 patients with early-onset EE, using a panel of 35 known and potential candidate genes and NGS, and 12 pathogenic mutations were found. Kwong et al. [8] performed NGS analysis using a panel of 7 genes (ARX, CDKL5, KCNQ2, PCDH19, SCN1A, and STXBP1) in 26 patients with infantile EE and identified 10 mutations. Lemke et al. [9] evaluated 33 cases with epilepsy by targeted NGS using 265 monogenic epilepsy-associated genes and found that 48 % of cases had disease-causing mutations. In a recent study conducted by Mercimek-Mahmutoglu et al., 110 patients with intractable epilepsy, global developmental delay, and cognitive dysfunction were retrospectively evaluated [10]. Genetic causes were identified in 28 % of these patients; 7 % had inherited metabolic disorders, and 21 % had other genetic causes including genetic syndromes, pathogenic copy number variants on array comparative genomic hybridization, and epileptic encephalopathy related to mutations in SCN1A, SCN2A, SCN8A, KCNQ2, STXBP1, PCDH19, and SLC9A6 genes. The authors also reported that, using prepared EE panel in conjunction with targeted NGS, a genetic diagnosis was obtained in 45 % of patients.
Channelopathy genes are the most commonly involved genes in almost all epilepsy forms similar to the present study. It has been reported that mutations in SCN1A gene may be associated with different phenotypes changing from generalized epilepsy with febrile seizures plus (GEFS+) to Dravet syndrome. KCNQ2 mutations usually cause more severe clinical phenotype such as early-onset EE while KCNQ3 mutations are associated with milder phenotypes. Multiple mechanisms besides channelopathies in the pathogenesis of early-onset EE have been identified. Defects in DNA transcription, cell synaptic function, and metabolic pathway enzymes may lead to early-onset EE. Because of overlapping clinical features and lacking of phenotype genotype correlations in early-onset EEs, multiple gene panels or whole exome sequencing (WES) have been strongly suggested to identify genetic etiology [22].
Among the variants detected in our cases, three previously defined variants (rs112767060, rs370517200, rs201334086) in SCN1A, CNTNAP2, and MBD5 genes and seven novel mutations in SCN1A, SCN2A, CDKL5, KCNQ2, STXBP1, and FOXG1 genes were considered to be causative variants, because they were de novo, nonsynonim variants, and predicted to alter protein function using in silico prediction programs (SIFT, PolyPhen2 and MutationTaster). However, further cases and functional studies are needed to clarify their effect.
Case 10, presenting with atypical Rett Syndrome, carried FOXG1 mutation (c.*6C > T) homozygously. Up to date all previously reported cases with FOXG1 mutations were heterozygous, and it has been suggested that haploinsufficiency is responsible for clinical findings [19]. We have considered that the effects of c.*6C > T mutation could be milder since it is placed at 3′ untranslated region, and only homozygosity could cause clinical findings. Further studies are needed to confirm this hypothesis.
The CNTNAP2 variant detected in Case 11 has been inherited from the father and it has been described as a probably damaging mutation by Murdoch et al. [20]. Since CNTNAP2 gene defects have not been defined in Dravet syndrome, molecular analysis of all known causative genes for Dravet syndrome or whole exome sequencing analysis should be performed to clarify the exact relationship between the molecular and clinical findings. Strauss et al. [23] reported a homozygous mutation CNTNAP2 in nine children with cortical dysplasia, focal epilepsy, relative macrocephaly, and diminished deep tendon reflexes. Our case having missense mutation in CNTNAP2 gene, displayed partial seizures from two years of age and had a normal cranial MRI.
Studies conducted on 2q23.1 microdeletion syndrome have shown MBD5 to be the major causative gene in the development of this syndrome [21, 24]. Point mutations in MBD5 gene can also present a similar clinical picture to microdeletion syndrome [25]. Recently, the same deletion has been found in children with infantile spasms [26]. Segregation analysis showed that the MBD5 mutation found in case 12 was inherited from the father. Three siblings of the father had died from unknown conditions during the neonatal period. Since this genomic region is highly conserved, it is considered that this variation might be the causative mutation. The phenotypical variability in this family can be explained by a possible incomplete penetrance or variable expressivity which can be seen in autosomal dominantly inherited diseases.
In the literature, the mutation detection rate among the outbreed epileptic encephalopathy cases varies between 22.6 and 44.8 % [7–10]. The overall mutation detection rate (40 %) found in the present study is compatible with the earlier reports. The higher percentage of mutation detection rate among the patients born to nonconsanguineous parents compared to those born to consanguineous parents (55.5 versus 16.6 %) can be attributed to the selected genes mostly known for their de novo inheritance pattern. These data also indicate that different candidate gene/genes responsible for early-onset EE with autosomal recessive inheritance should be considered in our cases, and whole exome sequencing might be a more rational tool to discover novel genes.
In conclusion, targeted NGS approach allows parallel sequencing of as many genes as required and is therefore an effective diagnostic tool for mapping the genetic background of early-onset EEs.
References
Engel J Jr (2001) A proposed diagnostic scheme for people with epileptic seizures and with epilepsy: report of the ILAE Task Force on Classification and Terminology. Epilepsia 42:796–803
Berg AT, Berkovic SF, Brodie MJ, Buchhalter J, Helen Cross J, van Emde Boas W et al (2010) Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia 51:676–685
Mastrangelo M, Leuzzi V (2012) Genes of early-onset epileptic encephalopathies: from genotype to phenotype. Pediatr Neurol 46:24–31
Gursoy S, Ercal D (2016) Diagnostic approach to genetic causes of early-onset epileptic encephalopathy. J Child Neurol 31(4):523–532
Yalaz K, Epir S (1983) The Denver Developmental Screening Test: normative data for Ankara children. Turk J Pediatr 25:245–248
Wechsler D (1991) Wechsler Intelligence Scale for Children III. Psychological Corporation, New York
Kodera H, Kato M, Nord AS, Walsh T, Lee M, Yamanaka G et al (2013) Targeted capture and sequencing for detection of mutations causing early onset epileptic encephalopathy. Epilepsia 54:1262–1269
Kwong AK, Ho AC, Fung CW, Wong VC (2015) Analysis of mutations in 7 genes associated with neuronal excitability and synaptic transmission in a cohort of children with non-syndromic infantile epileptic encephalopathy. PLoS One 10:e0126446
Lemke JR, Riesch E, Scheurenbrand T, Schubach M, Wilhelm C, Steiner I et al (2012) Targeted next generation sequencing as a diagnostic tool in epileptic disorders. Epilepsia 53:1387–1398
Mercimek-Mahmutoglu S, Patel J, Cordeiro D, Hewson S, Callen D, Donner EJ et al (2015) Diagnostic yield of genetic testing in epileptic encephalopathy in childhood. Epilepsia 56:707–716
Stenson PD, Ball EV, Mort M, Phillips AD, Shiel JA, Thomas NS et al (2003) Human gene mutation database (HGMD): 2003 update. Hum Mutat 21:577–581
Kumar P, Henikoff S, Ng PC (2009) Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc 4:1073–1081
Schwarz JM, Rodelsperger C, Schuelke M, Seelow D (2010) MutationTaster evaluates disease-causing potential of sequence alterations. Nat Methods 7:575–576
Adzhubei IA, Schmidt S, Peshkin L, Ramensky VE, Gerasimova A, Bork P et al (2010) A method and server for predicting damaging missense mutations. Nat Methods 7:248–249
Pollard KS, Hubisz MJ, Rosenbloom KR, Siepel A (2010) Detection of nonneutral substitution rates on mammalian phylogenies. Genome Res 20:110–121
Davydov EV, Goode DL, Sirota M, Cooper GM, Sidow A et al (2010) Identifying a high fraction of the human genome to be under selective constraint using GERP++. PLoS Comput Biol 6:e1001025
Depienne C, Trouillard O, Saint-Martin C, Gourfinkel-An I, Bouteiller D, Carpentier W et al (2009) Spectrum of SCN1A gene mutations associated with Dravet syndrome: analysis of 333 patients. J Med Genet 46:183–191
Dibbens LM, Tarpey PS, Hynes K, Bayly MA, Scheffer IE, Smith R et al (2008) X-linked protocadherin 19 mutations cause female-limited epilepsy and cognitive impairment. Nat Genet 40:776–781
Terrone G, Bienvenu T, Germanaud D, Barthez-Carpentier MA, Diebold B, Delanoe C et al (2014) A case of Lennox-Gastaut syndrome in a patient with FOXG1-related disorder. Epilepsia 55:e116–e119
Murdoch JD, Gupta AR, Sanders SJ, Walker MF, Keaney J, Fernandez TV et al (2015) No evidence for association of autism with rare heterozygous point mutations in contactin-associated protein-like 2 (CNTNAP2), or in other contactin-associated proteins or contactins. PLoS Genet 11:e1004852
Williams SR, Mullegama SV, Rosenfeld JA, Dagli AI, Hatchwell E, Allen WP et al (2010) Haploinsufficiency of MBD5 associated with a syndrome involving microcephaly, intellectual disabilities, severe speech impairment, and seizures. Eur J Hum Genet 18:436–441
El Achkar CM, Olson HE, Poduri A, Pearl PL (2015) The genetics of the epilepsies. Curr Neurol Neurosci Rep 15:39. doi:10.1007/s11910-015-0559-8
Strauss KA, Puffenberger EG, Huentelman MJ, Gottlieb S, Dobrin SE, Parod JM et al (2006) Recessive symptomatic focal epilepsy and mutant contactin-associated protein-like 2. N Engl J Med 354:1370–1377
Talkowski ME, Mullegama SV, Rosenfeld JA, van Bon BW, Shen Y, Repnikova EA et al (2011) Assessment of 2q23.1 microdeletion syndrome implicates MBD5 as a single causal locus of intellectual disability, epilepsy, and autism spectrum disorder. Am J Hum Genet 89:551–563
Bonnet C, Ali Khan A, Bresso E, Vigouroux C, Béri M, Lejczak S et al (2013) Extended spectrum of MBD5 mutations in neurodevelopmental disorders. Eur J Hum Genet 21:1457–1461
Du X, An Y, Yu L, Liu R, Qin Y, Guo X et al (2014) A genomic copy number variant analysis implicates the MBD5 and HNRNPU genes in Chinese children with infantile spasms and expands the clinical spectrum of 2q23.1 deletion. BMC Med Genet 15:62
Acknowledgments
This project was supported by Ege University Scientific Research Projects (EGEBAP) with grant number 14-TIP-033.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
This study was approved by the local ethical committee (13-9/15).
Informed consent
Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Rights and permissions
About this article
Cite this article
Gokben, S., Onay, H., Yilmaz, S. et al. Targeted next generation sequencing: the diagnostic value in early-onset epileptic encephalopathy. Acta Neurol Belg 117, 131–138 (2017). https://doi.org/10.1007/s13760-016-0709-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-016-0709-z