Abstract
Multiple sclerosis (MS) is a common autoimmune disease of central nervous system in which neurodegenerative and inflammatory mechanisms cause alternate neurological impairments. Many inflammatory and anti-inflammatory cytokines were suggested as contributor in MS pathogenesis, and the balance between these opposing cytokines can regulate MS severity. IL-37, an anti-inflammatory cytokine, is the most recently identified member of IL-1 family, which acts as a natural inhibitor of innate immunity. However, the role of IL-37 in MS has not investigated so far. Therefore, in this study, we aimed to measure serum level of IL-37 in patients with relapsing remitting multiple sclerosis (RRMS) and neuromyelitis optica (NMO). In a case–control study, plasma was collected from healthy controls (n = 49) and also patients with RRMS (n = 122) and NMO (n = 31). Serum level measurement of IL-37 was performed using enzyme-linked immunoassay (ELISA) method. The serum levels of IL-37 were 247.46 ± 74.02 and 312.00 ± 86.72 and 114.63 ± 20.58 in RRMS and NMO patients and healthy controls, respectively, showing statistically significant difference between them (P = 0.00). Furthermore, we found a positive correlation between the serum levels of IL-37 and EDSS of patients (r = +0.31 and P = 0.00). In summary, the serum level of IL-37 was found to be significantly increased in MS patients compared to healthy controls. Furthermore, the mean serum level of IL-37 was correlated with disease severity. This suggests that IL-37 may be part of a feed-back loop to control underlying inflammation in MS pathogenesis. However, further studies will be required to indicate exact role of IL-37 in the MS pathomechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is a complex T cell-mediated autoimmune demyelinating disease of the central nervous system that normally conduces to alternate neurological impairments followed by disability progression in young people and middle-aged adults [1]. Although the causes underlying this disease remain obscure, it is well known that there are both genetic and environmental contributions [2]. An increasing body of evidence clearly indicates that alterations of immune system activity including increased Th1, Th2, and Th17 cell-derived cytokines, and decreased regulatory T (Treg) cells play a critical role in the pathogenesis of MS [3–5]. In addition to role of cytokines in progression and regulation of experimental allergic encephalitis (EAE), implication of them in the MS pathomechanisms has been also demonstrated based on examination of post-mortem MS tissue and transgenic mice [6, 7]. IL-37, an inhibitory member of IL-1 family of cytokines, participates in a wide variety of immunological mechanisms in response to the inflammation and autoimmune diseases [8]. IL-37 as the most recently identified member of IL-1 family of cytokines was discovered in silico in 2000 by several independent groups [9]. IL-1 family consists of 11 members including 3 receptors (IL-1Ra, IL-36Ra, and IL-38) and 8 cytokines (IL-1α, IL-1β, IL-18, IL-33, IL-36α, IL-36β, IL-36γ, and IL-37) [10, 11]. It has become increasingly clear in the several past years that production of IL-37 in peripheral blood monocytes can be induced by pro-inflammatory cytokines such as TNF-α, IFN-γ, and IL-18 or anti-inflammatory cytokines such as IL-10 and TGF-β [12, 13]. IL-37 is mostly produced by NK, monocytes, stimulated B cells which are also important in the etiopathogenesis of MS [14]. Although the role of IL-37 in adaptive immunity is still unclear, it is well known that can regulate innate immunity as also previous studies tend to imply that IL-37 suppress inflammation through negative feedback mechanisms. Secretion of IL-37 in different types of cells such as macrophages, monocytes, and epithelial cells can suppress production of pro-inflammatory cytokines [14]. More recently, abundant studies have illuminated increased IL-37 expression in many chronic inflammatory and autoimmune diseases such as arthritis, in patients with Mycobacterium avium infections, atherosclerotic coronary, and carotid artery plaques, in psoriatic plaques, Crohn’s disease, systemic lupus erythematosus, and Guillain-barr´e syndrome [15–17]. However, the role of IL-37 in MS has not investigated so far.
It has become increasingly clear in the past several years that adaptive immune responses play a pivotal role in the pathogenesis of MS, but it should also be mentioned that adaptive immunity is not acting in isolation but rather in conjunction with components of the innate immune system, and innate immune responses can involve and affect the nature of adaptive immune responses especially in multiple sclerosis [18]. It is well known that IL-37 regulates innate immune responses, thereby regulate adaptive immunity by modulating the production of cytokines and affecting the function of DCs which are main contributors of MS pathogenesis.
Therefore, in our present study, we sought to determine serum level of IL-37 in patients with relapsing remitting multiple sclerosis (RRMS) and neuromyelitis optica (NMO) and also correlation between the mean serum concentration of IL-37 with other clinical characteristics of patients.
Methods and materials
This case–control study was carried out in Isfahan, one of the most populated province of Iran, and all participants of study were also resident of this province. We recruited 122 RRMS (40 men and 82 women) and 31 NMO (13 men and 18 women) patients from Iranian MS and Neuroimmunology Researches Center who and then they were underwent diagnosis according to the McDonald’s and Wingerchuk criteria, respectively. We also chose 59 healthy subjects from Iranian Blood Transfusion Organization (IBTO) who was matched well with the patients regarding to the age and sex. Degree of disability was assessed using the Kurtzke Disability Score, and other medical history and examination findings including spinal MRI, brain MRI, duration of disease, and relapse number during last year were collected. We excluded cases with other autoimmune disorder, infection disease, and systemic blood abnormalities. The protocol of study was approved by Ethical Committee on Human Research, Isfahan University of Medical Sciences. Informed written consent was achieved from patients.
Blood samples (3–5 ml) were collected from peripheral veins according to the routine puncture method and then plasma was recruited using centrifuge and stored at −80 °C. Serum level measurement of IL-37 was performed using enzyme-linked immunoassay (ELISA) according to the manufacturer’s instructions (eBioscience, San Diego, CA, USA).
Statistical analysis was performed using SPSS for hardware (Ver. 19). The Kolmogrov-Smirnov Z test was used to verify the normality of the data. The difference between the groups was analyzed by Mann–Whitney U test and Wilcoxon signed-rank test. The correlation between variables was assessed using the Spearman rank correlation test. Data were expressed as mean ± standard deviation (SD). All tests were two tailed, and P ≤ 0.05 was considered as a significant threshold.
Results
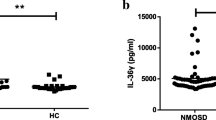
The mean age of RRMS and NMO patients was 37.96 ± 9.87 and 37.91 ± 9.26, respectively. The mean age of healthy controls was 35.26 ± 7.97 which did not show significant difference with those of patients, and they were well matched regarding to the age and sex as shown in Table 1 (P = 0.14). Other clinical and paraclinical characteristics of patients and healthy controls including duration of disease, EDSS, relapse number, brain MRI, and spinal MRI are summarized in Table 1. The mean concentration of IL-37 in the serum of patients with RRMS and NMO was 247.46 ± 74.02 and 312.00 ± 86.72, respectively, which were significantly higher than healthy controls (114.63 ± 20.58, P = 0.00) (Fig. 1). Furthermore, the mean serum level of IL-37 was significantly higher in NMO patients compared to RRMS patients (P = 0.00). There was no significant difference between men and women regarding to the mean serum level of IL-37 (P = 0.67). We found a positive correlation between serum level of IL-37 and EDSS of patients (r = +0.31, P = 0.00) (Fig. 2). In addition, there was a significant association between serum level of IL-37 and duration of disease (r = +0.17, P = 0.03). However, we could not show significant correlation between relapse number of patients during last year and serum level of IL-37 (P = 0.24).
Discussion
MS is a common autoimmune disease of disease of CNS in which neurodegenerative and inflammatory mechanisms cause alternate neurological impairments. Many inflammatory and anti-inflammatory cytokines were suggested as contributor in MS pathogenesis, and the balance between these opposing cytokines can regulate MS severity [19]. IL-37, an anti-inflammatory cytokine, is the most recently identified member of IL-1 family, which acts as a natural inhibitor of innate immunity. However, the role of IL-37 in MS has not investigated so far. In this study, we assessed the serum level of IL-37 in patients with RRMS and NMO compared to healthy controls. We found increased serum level of IL-37 in the patients with RRMS and NMO compared to healthy controls suggesting activation by pro-inflammatory cytokines or other unknown factors in MS patients. More importantly, there was also a positive correlation between serum level of IL-37 and EDSS and duration of disease. We could not find any association between serum level of IL-37 and other factors such as age and sex.
There is a lot of evidence that different responses of adaptive immune, especially those of CD4+ and CD8+ subpopulations, have a key role in the MS pathogenesis [20]. In addition, recent studies have shown that other types of immune cells such as B cells are also important, in particular in the pathogenesis of NMO. Nevertheless, presence of autoreactive T cells and autoantibodies in healthy controls suggests that other mechanisms and immune cells may also be involved in the pathogenesis of MS and NMO [21]. Indeed, we can consider innate immunity as one of the most important part of immune responses to the autoimmune stimulations. Furthermore, innate immunity responses influence adaptive responses, and they share many molecules and transcription factors in their signaling pathway.
Semi-mature dendritic cells (DCs) play a pivotal role in maintaining tolerance in many types of self-antigen-enriched environments through mediating T cell tolergenecity. It has been shown that IL-37 as an anti-inflammatory cytokine also participates in peripheral tolerance through induction of DCs generations [22].
Recently, it has been revealed that DCs expressing IL-37 favor the development of regulatory T cells, although they have decreased ability to activate naïve T cells that are important for suppression of autoimmune reactions in MS [22].
It has been demonstrated that IL-37 can decrease expression of some pro-inflammatory cytokines in immune cells, in particular PMNCs, and also TNF-a as a pro-inflammatory cytokine induces production of IL-37 in PMNCs [12]. Therefore, the increased serum level of IL-37 in our MS and NMO patients may be due to increased serum level of pro-inflammatory cytokines in them.
Increased serum level of IL-37 in RRMS and NMO patients is consistent with previous studies that reported elevated level of this cytokine in patients with other autoimmune diseases such as Crohn’s disease, systemic lupus erythematosus, and Guillain-barr´e syndrome (GBS) [17, 23] suggesting role of IL-37 in suppressing excessive inflammation. However, we cannot completely exclude possible role of this cytokine in pathomechanisms of MS. In a study, in this regard, Li et al. [15] investigated plasma and CSF levels of IL-37, IL-17A, IFN-γ, and TNF-α in patients with acute GBS and healthy controls using ELISA method. They showed increases plasma IL-37, IL-17A, IFN-γ, and TNF-α and CSF IL-37 and IL-17A in GBS patients in compared with healthy controls. Since increased inflammatory cytokines and IL-37 were shown in this study, we can conclude previous notion that IL-37 increases in response to the inflammation. In addition to autoimmune diseases, due to ability of IL-37 to reducing inflammation by inhibiting production of inflammatory cytokines and chemokines, its protective role was investigated in other disorders such septic shock, concanavalin A-induced hepatitis, and experimental model of ischemia/reperfusion [14, 24, 25]. Furthermore, Li et al. [26] evaluated both serum and expressions of IL-37, TNF-a, IL-6, and IL-17 mRNA in peripheral blood mononuclear cells of patients with grave’s disease using real-time reverse transcription–polymerase chain reaction (RT-PCR) and ELISA, respectively. They reported increased serum level and expression of IL-37 in grave’s patients compared to the healthy controls. In addition, they found positive correlation between IL-37 with disease activity and other cytokines. In a similar study, increased serum level of IL-37 was reported in rheumatoid arthritis patients compared to healthy controls [27]. They also showed decreased serum level of IL-37 in patients who were drug responsive after treatment with disease modifying anti-rheumatoid arthritis drugs.
Conclusion
In summary, the serum level of IL-37 was found to be significantly increased in MS patients compared to healthy controls. Furthermore, serum level of IL-37 was correlated with disease severity. This suggests that IL-37 may be part of a feed-back loop to control underlying inflammation in MS pathogenesis. However, further studies will be required to indicate exact role of IL-37 in MS pathomechanisms.
References
Compston A, Coles A (2008) Multiple sclerosis. Lancet 372(9648):1502–1517. doi:10.1016/S0140-6736(08)61620-7
Miller E (2012) Multiple sclerosis. Adv Exp Med Biol 724:222–238. doi:10.1007/978-1-4614-0653-2_17
Martins TB, Rose JW, Jaskowski TD, Wilson AR, Husebye D, Seraj HS, Hill HR (2011) Analysis of proinflammatory and anti-inflammatory cytokine serum concentrations in patients with multiple sclerosis by using a multiplexed immunoassay. Am J Clin Pathol 136(5):696–704. doi:10.1309/AJCP7UBK8IBVMVNR
Venken K, Hellings N, Liblau R, Stinissen P (2010) Disturbed regulatory T cell homeostasis in multiple sclerosis. Trends Mol Med 16(2):58–68. doi:10.1016/j.molmed.2009.12.003
Jadidi-Niaragh F, Mirshafiey A (2011) Th17 cell, the new player of neuroinflammatory process in multiple sclerosis. Scand J Immunol 74(1):1–13. doi:10.1111/j.1365-3083.2011.02536.x
Hauser SL, Bhan AK, Gilles F, Kemp M, Kerr C, Weiner HL (1986) Immunohistochemical analysis of the cellular infiltrate in multiple sclerosis lesions. Ann Neurol 19(6):578–587. doi:10.1002/ana.410190610
Ferber IA, Brocke S, Taylor-Edwards C, Ridgway W, Dinisco C, Steinman L, Dalton D, Fathman CG (1996) Mice with a disrupted IFN-gamma gene are susceptible to the induction of experimental autoimmune encephalomyelitis (EAE). J Immunol 156(1):5–7
Akdis M, Burgler S, Crameri R, Eiwegger T, Fujita H, Gomez E, Klunker S, Meyer N, O’Mahony L, Palomares O, Rhyner C, Ouaked N, Schaffartzik A, Van De Veen W, Zeller S, Zimmermann M, Akdis CA (2011) Interleukins, from 1 to 37, and interferon-gamma: receptors, functions, and roles in diseases. J Allergy Clin Immunol 127(3):701–721. doi:10.1016/j.jaci.2010.11.050 (e701–770)
Dinarello CA, Bufler P (2013) Interleukin-37. Semin Immunol 25(6):466–468. doi:10.1016/j.smim.2013.10.004
Garlanda C, Dinarello CA, Mantovani A (2013) The interleukin-1 family: back to the future. Immunity 39(6):1003–1018. doi:10.1016/j.immuni.2013.11.010
Dinarello C, Arend W, Sims J, Smith D, Blumberg H, O’Neill L, Goldbach-Mansky R, Pizarro T, Hoffman H, Bufler P, Nold M, Ghezzi P, Mantovani A, Garlanda C, Boraschi D, Rubartelli A, Netea M, van der Meer J, Joosten L, Mandrup-Poulsen T, Donath M, Lewis E, Pfeilschifter J, Martin M, Kracht M, Muehl H, Novick D, Lukic M, Conti B, Solinger A, Kelk P, van de Veerdonk F, Gabel C (2010) IL-1 family nomenclature. Nat Immunol 11(11):973. doi:10.1038/ni1110-973
Nold MF, Nold-Petry CA, Zepp JA, Palmer BE, Bufler P, Dinarello CA (2010) IL-37 is a fundamental inhibitor of innate immunity. Nat Immunol 11(11):1014–1022. doi:10.1038/ni.1944
Bufler P, Gamboni-Robertson F, Azam T, Kim SH, Dinarello CA (2004) Interleukin-1 homologues IL-1F7b and IL-18 contain functional mRNA instability elements within the coding region responsive to lipopolysaccharide. Biochem J 381(Pt 2):503–510. doi:10.1042/BJ20040217
Boraschi D, Lucchesi D, Hainzl S, Leitner M, Maier E, Mangelberger D, Oostingh GJ, Pfaller T, Pixner C, Posselt G, Italiani P, Nold MF, Nold-Petry CA, Bufler P, Dinarello CA (2011) IL-37: a new anti-inflammatory cytokine of the IL-1 family. Eur Cytokine Netw 22(3):127–147. doi:10.1684/ecn.2011.0288
Li C, Zhao P, Sun X, Che Y, Jiang Y (2013) Elevated levels of cerebrospinal fluid and plasma interleukin-37 in patients with Guillain-Barre syndrome. Mediators Inflamm 2013:639712. doi:10.1155/2013/639712
Song L, Qiu F, Fan Y, Ding F, Liu H, Shu Q, Liu W, Li X (2013) Glucocorticoid regulates interleukin-37 in systemic lupus erythematosus. J Clin Immunol 33(1):111–117. doi:10.1007/s10875-012-9791-z
Sharma S, Kulk N, Nold MF, Graf R, Kim SH, Reinhardt D, Dinarello CA, Bufler P (2008) The IL-1 family member 7b translocates to the nucleus and down-regulates proinflammatory cytokines. J Immunol 180(8):5477–5482
Fernandez M, Montalban X, Comabella M (2010) Orchestrating innate immune responses in multiple sclerosis: molecular players. J Neuroimmunol 225(1–2):5–12. doi:10.1016/j.jneuroim.2010.05.014
Petek-Balci B, Coban A, Shugaiv E, Turkoglu R, Ulusoy C, Icoz S, Pehlivan M, Tuzun E, Akman-Demir G, Kurtuncu M, Eraksoy M (2014) Predictive value of early serum cytokine changes on long-term interferon beta-1a efficacy in multiple sclerosis. Int J Neurosci. doi:10.3109/00207454.2014.939747
Goverman J (2009) Autoimmune T cell responses in the central nervous system. Nat Rev Immunol 9(6):393–407. doi:10.1038/nri2550
Sospedra M, Martin R (2005) Immunology of multiple sclerosis. Annu Rev Immunol 23:683–747. doi:10.1146/annurev.immunol.23.021704.115707
Chen HM, Fujita M (2015) IL-37: a new player in immune tolerance. Cytokine 72(1):113–114. doi:10.1016/j.cyto.2014.11.025
McNamee EN, Masterson JC, Jedlicka P, McManus M, Grenz A, Collins CB, Nold MF, Nold-Petry C, Bufler P, Dinarello CA, Rivera-Nieves J (2011) Interleukin 37 expression protects mice from colitis. Proc Natl Acad Sci USA 108(40):16711–16716. doi:10.1073/pnas.1111982108
Sakai N, Van Sweringen HL, Belizaire RM, Quillin RC, Schuster R, Blanchard J, Burns JM, Tevar AD, Edwards MJ, Lentsch AB (2012) Interleukin-37 reduces liver inflammatory injury via effects on hepatocytes and non-parenchymal cells. J Gastroenterol Hepatol 27(10):1609–1616. doi:10.1111/j.1440-1746.2012.07187.x
Bulau AM, Fink M, Maucksch C, Kappler R, Mayr D, Wagner K, Bufler P (2011) In vivo expression of interleukin-37 reduces local and systemic inflammation in concanavalin A-induced hepatitis. Sci World J 11:2480–2490. doi:10.1100/2011/968479
Li Y, Wang Z, Yu T, Chen B, Zhang J, Huang K, Huang Z (2014) Increased expression of IL-37 in patients with Graves’ disease and its contribution to suppression of proinflammatory cytokines production in peripheral blood mononuclear cells. PLoS One 9(9):e107183. doi:10.1371/journal.pone.0107183
Zhao PW, Jiang WG, Wang L, Jiang ZY, Shan YX, Jiang YF (2014) Plasma levels of IL-37 and correlation with TNF-alpha, IL-17A, and disease activity during DMARD treatment of rheumatoid arthritis. PLoS One 9(5):e95346. doi:10.1371/journal.pone.0095346
Conflict of interest
The authors declare that no conflict of interest exists.
Ethical standard
The protocol of study was approved by Ethical Committee on Human Research, Isfahan University of Medical Sciences.
Informed consent
Informed written consent was achieved from patients.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Farrokhi, M., Rezaei, A., Amani-Beni, A. et al. Increased serum level of IL-37 in patients with multiple sclerosis and neuromyelitis optica. Acta Neurol Belg 115, 609–614 (2015). https://doi.org/10.1007/s13760-015-0491-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-015-0491-3