Abstract
The aim of this study is to investigate the frequency of unilateral cranial autonomic symptoms during migraine attacks, and to compare the clinical characteristics of migraine patients with and without unilateral cranial autonomic symptoms. One hundred and eighty-six consecutive patients with episodic migraine attacks were prospectively included. Cranial autonomic symptoms of the patients occurred during headache, frequency, duration, severity and character of headache, disease duration, presence of aura, laterality of headache, accompanying symptoms, relation of migraine attacks with menstruation, lesions detected on magnetic resonance images, and family history of migraine were recorded. The patients with and without unilateral cranial autonomic symptoms during headache were compared in terms of above-mentioned parameters. Seventy-seven (41.4 %) patients were observed to develop unilateral cranial autonomic symptoms during migraine attack. Disease duration was longer in the patients with unilateral cranial autonomic symptoms than in those without (p = 0.045). Headache was unilateral in 83.1 % of the patients with unilateral cranial autonomic symptoms (p = 0.001). Pure menstrual or menstrually related migraine attacks were more common in the patients with unilateral cranial autonomic symptoms (p = 0.043) and is thought that menstruation-related hormonal factors might have a triggering role on the trigeminal-autonomic reflex pathway. The longer disease duration in patients with unilateral cranial autonomic symptoms might be associated with the activation of pathophysiological mechanisms that cause cranial autonomic symptoms in time. Frequent unilateral pain in migraine patients with unilateral cranial autonomic symptoms is likely to indicate that the development of autonomic symptoms may share common mechanisms with the pathogenesis of trigeminal autonomic cephalalgias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cranial autonomic symptoms (CAS) such as lacrimation, conjunctival injection, eyelid edema, and nasal congestion as well as miosis, ptosis, forehead or facial sweating and facial flushing are characteristic signs of trigeminal autonomic cephalalgias (TACs). However, they can also be encountered in migraine patients during headache attacks, besides the systemic autonomic symptoms like nausea, vomiting and diarrhea, and represent the activation of the parasympathetic system. Although it is thought that CAS occur during migraine attacks due to increased activity of trigeminal-autonomic reflex that consists of brainstem connections between the trigeminal nerve and facial parasympathetic outflow, pathophysiology of the CAS remains unclear.
Although, brainstem in migraine and hypothalamic gray matter in TACs are considered to be responsible for headache as shown in functional neuroimaging studies [1, 2], migraine and TACs may share common pathophysiological pathways and common symptoms. While CAS have been reported in patients with migraine [3–9], migrainous symptoms such as photophobia, phonophobia, nausea, and vomiting have been reported in patients with cluster headache [10]. It has been suggested that the presence of CAS in migraine patients may be important regarding treatment approaches and may predict a better response to triptans [13].
The present study aimed to investigate the frequency of unilateral CAS (UCAS) during migraine attacks, and to compare the clinical features of migraine patients with and without UCAS.
Materials and methods
One hundred and eighty-six consecutive patients, who had episodic migraine attacks, were prospectively included in the study. They were diagnosed as having migraine with and without aura according to the International Classification of Headache Disorders-II (ICHD-II) criteria [14]. Patients with chronic migraine, with primary headaches other than migraine and with secondary headaches were excluded from the study. Data regarding frequency, duration, severity, character, localization and laterality of headache, as well as disease duration, presence of aura, and aggravation of headache with physical activity were obtained. In addition, symptoms including nausea, vomiting, photophobia, and phonophobia that accompanied headache, relation of migraine attacks with menstruation, family history of migraine and cranial magnetic resonance (MR) imaging findings were recorded. Severity of headache was scored on a headache severity scale from 1 to 3 (1 = mild, 2 = moderate, 3 = severe). Patients who had migraine attacks associated with menstruation were classified as those with pure menstrual migraine or menstrually related migraine according to the ICHD-II criteria and these two groups were evaluated together. Small hyperintense lesions located in the periventricular area or in the deep white matter and clinically silent infarct-like lesions, which were detected on the cranial MR images (n = 105) were recorded.
According to the laterality of headache, patients were divided into three groups as follows: those with unilateral headache, those with bilateral headache, and those with both unilateral and bilateral headache (unilateral + bilateral). The patients with unilateral headache were divided into the following categories: left-sided headache, right-sided headache, headache more frequent on the left side than on the right side (left > right), headache more frequent on the right side than on the left side (right > left), and headache with equal frequency on the left and right sides (left = right). The patients with unilateral + bilateral headache were also divided into the above-mentioned categories based on their unilateral headache. Furthermore, left-sided headache alone and headache being left > right were evaluated together as headache with left-side predominance, whereas right-sided headache alone and headache being right > left were evaluated together as headache with right-side predominance.
All patients were questioned with respect to the presence of reddening of the eye, lacrimation, eyelid edema, and nasal congestion during headache attacks, as well as laterality of these signs and their association with laterality of headache. CAS was considered positive in the presence of at least one autonomic symptom, and only those patients with unilateral CAS were evaluated. Although many of the patients indicated that they had experienced these symptoms in approximately more than half of their headache attacks, they could not specify the exact frequency of the symptoms.
Patients suffering from migraine headache were consulted in the headache center of our clinic and were informed about the aim of the study. Patient data including headache history and autonomic symptoms were obtained by two neurologists (H.G., A.E.Ç.) via direct interview. Detailed analyses of the records and data collection were done by three (authors) neurologists.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS, Inc., Chicago, IL, USA) version 11.5. The Shapiro–Wilk test was used to test the normality of continuous variables. Continuous variables were expressed as mean ± standard deviation or median (minimum–maximum), where applicable, whereas nominal data were expressed as number and percentages. While the mean differences were evaluated by the Student’s t test, the Mann–Whitney U test was used to compare the median values. Nominal data were analyzed by the Pearson Chi-square or Fisher’s Exact tests, where appropriate. A p value < 0.05 was considered statistically significant.
Results
One hundred and eighty-six patients (167 females and 19 males) were included in the study. During migraine attacks, UCAS occurred in 77 (41.4 %) patients. No significant differences were found between the patients with and without UCAS in terms of mean age and gender distribution (p > 0.05). There was also no significant difference between these patient groups with respect to the frequency and character of headache attacks, the rate of attacks with and without aura, and the rate of patients who experienced aggravation of headache with physical activity (p > 0.05). Although, we observed that patients with UCAS had more severe headaches and longer attack durations as compared to those without UCAS, statistically significant differences were not found concerning these symptoms (p = 0.055 and p = 0.089, respectively). Moreover, no significant differences were observed between the patients with and without UCAS in the frequency of accompanying symptoms including nausea, vomiting, photophobia and phonophobia, family history of migraine, and the frequency of lesions on MR images (p > 0.05). Duration of migraine disease was found to be longer in the patients with UCAS (p = 0.045). There was a significant difference between the patients with and without UCAS in the laterality of headache (unilateral versus bilateral) (p = 0.001). Headache was always unilateral in 83.1 % of the patients with UCAS and in 59.6 % of those without UCAS. Pure menstrual or menstrually related migraine attacks were more common in the patient group with UCAS (p = 0.043). Demographic and clinical characteristics of the patients with and without UCAS during migraine attacks are presented in Table 1.
As mentioned in the “Materials and Methods” section, the patients with unilateral and unilateral + bilateral headaches were further classified into subgroups based on the side of headache. Statistical analysis results for these subgroups revealed no significant difference between the patients with and without UCAS.
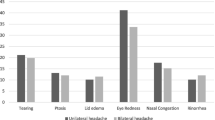
In the patients with UCAS, eyelid edema alone or in association with other symptoms was the most common symptom (51 patients, 66.2 %). Lacrimation in 43 patients (55.8 %), reddening of the eye in 40 patients (51.9 %) and nasal congestion in 20 patients (26.0 %) were found. The prevalence of UCAS in migraine patients is listed in Table 2.
Of these 77 patients with UCAS, 27 (35.1 %) had only one UCAS, 27 (35.1 %) had two UCAS, 19 (24.7 %) had three UCAS and 4 (5.2 %) had four UCAS during migraine attacks. No significant correlation was observed between the number of UCAS and the individual characteristics of migraine attacks except for vomiting (p = 0.009) as shown in Table 3.
Discussion
In the present study, UCAS were detected during headache in 41.4 % of the patients with migraine. In the previous studies, UCAS had been reported to accompany headache in 27–46 % of migraine patients [3–5]. The frequency of CAS had been reported to be 52–73 % in the studies evaluating CAS during migraine attacks [5–7].
In our study, it was demonstrated that duration of disease was significantly longer in the patients with UCAS as compared to those without UCAS. Duration of headache attacks was also longer in patients with UCAS; however, a statistically significant difference was not found between these two groups of patients. Although we clinically observed that the patients with UCAS had more severe headaches as compared to those without UCAS, a statistically significant difference between the severity of the pain and the presence of UCAS could not be obtained. It should be emphasized, however, that p value (p = 0.055) of the related statistical analysis was found only slightly over the threshold. It may be expected to observe lacrimation, a type of CAS, when even a healthy person is exposed to a very strong pain. Similarly, the severity of pain during the migraine attacks might be expected to be related to such cranial autonomic symptoms. A positive association between the presence of UCAS and severity of pain had also been determined [3, 4]. The development of CAS during headache attacks had been reported to be associated with long-lasting disease, length of headache episodes, and accompanying phonophobia [5]. It had been proposed that longer pain periods and long-lasting disease with frequent attacks may induce central sensitization of the trigeminal nucleus, and consequently may facilitate the trigeminal-autonomic reflex [5]. Moreover, it had been stated that, over a certain threshold of pain, the trigeminal-autonomic reflex can be activated and CAS may occur [15].
The present study demonstrated that headache was usually unilateral (83.1 %) in the patients with UCAS. Headache was bilateral only in 3.9 % of the patients in this group. Association between presence of UCAS and unilateral pain had also been reported in the previous studies [3, 4, 9]. Frequent unilateral pain in migraine patients with UCAS is likely to indicate that the development of autonomic symptoms may share common mechanisms with the pathogenesis of TACs.
It had been suggested that autonomic control of the cardiovascular system by the cerebral hemispheres is asymmetric; the left hemisphere dominantly affects parasympathetic function, whereas the right hemisphere dominantly affects sympathetic function [16, 17]. In a study evaluating autonomic reactivity during pain-free periods in migraine patients, increased parasympathetic activity had been reported in response to headache in left-sided migraineurs as compared to right-sided migraineurs [18]. However, we did not demonstrate a significant difference between the patients with and without UCAS in terms of frequency of right-sided or left-sided headache. Similarly, in another study, the side of headache was not found to be related with the prevalence of CAS [5].
To the best of our knowledge, association of menstruation with the presence of CAS has not been established well in migraine patients yet. On the other hand, based on a limited amount of data concerning the association between TACs and menstruation, it was found that menstruation has no significant effect on cluster headache [19–22]. However, it is also known that ovarian hormones influence the autonomic nervous system [23]. Indeed, as revealed in our study, pure menstrual or menstrually related migraine attacks were more common in the patients with UCAS supporting the thought that menstruation-related hormonal factors might have a triggering role on the trigeminal-autonomic reflex pathway.
Presence of CAS during migraine attacks reflects the involvement of the cranial parasympathetic system. It had been suggested that increased activity of the trigeminal-autonomic reflex pathway is responsible for the parasympathetic autonomic signs in TACs. This reflex pathway consists of brainstem connections between the trigeminal nerve and facial parasympathetic outflow. While the afferent arm of the reflex is composed of trigeminocaudal nucleus fibers, to which nociceptive input reaches, the efferent arm is composed of vasomotor and secretomotor fibers, which arise from the superior salivatory nucleus via the facial nerve. The afferent arm is active in migraine, whereas the efferent arm is active in cluster headache [15, 24]. In addition to the afferent arm of the reflex, hyperactivity of parasympathetic efferent arm might be responsible for autonomic symptoms in patients with migraine.
Common autonomic symptoms and unilateral pain are observed both in patients with migraine and in patients with cluster headache; and they all benefit from the same pain relieving treatments. All these observations indicate that migraine and TACs may share a common pathophysiological pathway. However, functional neuroimaging studies showing brainstem activation during migraine and hypothalamic gray matter activation during TACs do not corroborate this hypothesis and indicate that migraine and TACs have different pathogenesis [1, 2]. Nonetheless, in a recent positron emission tomography (PET) study, hypothalamic activity in addition to brainstem activation had been reported during spontaneous attacks in migraine patients without aura [25]. This finding, together with neuroendocrine studies and certain features of clinical presentation of migraine, indicates that hypothalamus also plays a role in the pathophysiology of migraine. The development of CAS during migraine attack also supports the hypothalamic effect [26]. Functional neuroimaging studies to be performed on migraine patients with CAS might be beneficial in terms of illuminating the pathophysiology of this type of migraine.
The reason for the development of CAS only in certain migraine patients, causes for the activation of the trigeminal-autonomic reflex, or factors changing the threshold that is necessary for activation of this reflex have not been clarified yet. It was demonstrated in our study that UCAS was rather frequent in migraine patients and that clinical characteristics of migraine were not so different in migraine patients with UCAS as compared to those without UCAS. However, migraine patients with UCAS had longer disease duration; and their headache was mostly unilateral and influenced by menstruation.
References
May A (2009) New insights into headache: an update on functional and structural imaging findings. Nat Rev Neurol 5(4):199–209
Sprenger T, Goadsby PJ (2010) What has functional neuroimaging done for primary headache and for the clinical neurologist? J Clin Neurosci 17(5):547–553
Obermann M, Yoon MS, Dommes P, Kuznetsova J, Maschke M, Weimar C, Limmroth V, Diener HC, Katsarava Z (2007) Prevalence of trigeminal autonomic symptoms in migraine: a population-based study. Cephalalgia 27(6):504–509
Barbanti P, Fabbrini G, Pesare M, Vanacore N, Cerbo R (2002) Unilateral cranial autonomic symptoms in migraine. Cephalalgia 22(4):256–259
Gupta R, Bhatia MS (2007) A report of cranial autonomic symptoms in migraineurs. Cephalalgia 27(1):22–28
Lai TH, Fuh JL, Wang SJ (2009) Cranial autonomic symptoms in migraine: characteristics and comparison with cluster headache. J Neurol Neurosurg Psychiatry 80(10):1116–1119
Rozen TD (2011) A history of cigarette smoking is associated with the development of cranial autonomic symptoms with migraine headaches. Headache 51(1):85–91
Kelman L, Tanis D (2006) The relationship between migraine pain and other associated symptoms. Cephalalgia 26(5):548–553
Kaup AO, Mathew NT, Levyman C, Kailasam J, Meadors LA, Villarreal SS (2003) ‘Side locked’ migraine and trigeminal autonomic cephalgias: evidence for clinical overlap. Cephalalgia 23(1):43–49
Rozen TD, Niknam RM, Shechter AL, Young WB, Silberstein SD (2001) Cluster headache in women: clinical characteristics and comparison with cluster headache in men. J Neurol Neurosurg Psychiatry 70(5):613–617
Vingen JV, Pareja JA, Stovner LJ (1998) Quantitative evaluation of photophobia and phonophobia in cluster headache. Cephalalgia 18(5):250–256
Goadsby PJ, Cittadini E, Cohen AS (2010) Trigeminal autonomic cephalalgias: paroxysmal hemicrania, SUNCT/SUNA, and hemicrania continua. Semin Neurol 30(2):186–191
Barbanti P, Fabbrini G, Vanacore N, Pesare M, Buzzi MG (2003) Sumatriptan in migraine with unilateral cranial autonomic symptoms: an open study. Headache 43(4):400–403
Headache Classification Subcommittee of the International Headache Society (2004) The International Classification of Headache Disorders, 2nd edn. Cephalalgia 24(Suppl 1):9–160
Goadsby PJ, Lipton RB (1997) A review of paroxysmal hemicranias, SUNCT syndrome and other short-lasting headaches with autonomic feature, including new cases. Brain 120(Pt 1):193–209
Oppenheimer SM, Kedem G, Martin WM (1996) Left-insular cortex lesions perturb cardiac autonomic tone in humans. Clin Auton Res 6(3):131–140
Hilz MJ, Dütsch M, Perrine K, Nelson PK, Rauhut U, Devinsky O (2001) Hemispheric influence on autonomic modulation and baroreflex sensitivity. Ann Neurol 49(5):575–584
Avnon Y, Nitzan M, Sprecher E, Rogowski Z, Yarnitsky D (2004) Autonomic asymmetry in migraine: augmented parasympathetic activation in left unilateral migraineurs. Brain 127(Pt 9):2099–2108
Lieba-Samal D, Wöber C (2011) Sex hormones and primary headaches other than migraine. Curr Pain Headache Rep 15(5):407–414
van Vliet JA, Favier I, Helmerhorst FM, Haan J, Ferrari MD (2006) Cluster headache in women: relation with menstruation, use of oral contraceptives, pregnancy, and menopause. J Neurol Neurosurg Psychiatry 77(5):690–692
Manzoni GC, Micieli G, Granella F, Martignoni E, Farina S, Nappi G (1988) Cluster headache in women: clinical findings and relationship with reproductive life. Cephalalgia 8(1):37–44
Ekbom K, Waldenlind E (1981) Cluster headache in women: evidence of hypofertility(?) Headaches in relation to menstruation and pregnancy. Cephalalgia 1(3):167–174
Martin VT, Behbehani M (2006) Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis–part I. Headache 46(1):3–23
Dodick DW, Rozen TD, Goadsby PJ, Silberstein SD (2000) Cluster headache. Cephalalgia 20(9):787–803
Denuelle M, Fabre N, Payoux P, Chollet F, Geraud G (2007) Hypothalamic activation in spontaneous migraine attacks. Headache 47(10):1418–1426
Holle D, Katsarava Z, Obermann M (2011) The hypothalamus: specific or nonspecific role in the pathophysiology of trigeminal autonomic cephalalgias? Curr Pain Headache Rep 15(2):101–107
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guven, H., Çilliler, A.E. & Çomoğlu, S.S. Unilateral cranial autonomic symptoms in patients with migraine. Acta Neurol Belg 113, 237–242 (2013). https://doi.org/10.1007/s13760-012-0164-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-012-0164-4