Abstract
Polysaccharide-based hydrogel scaffolds have emerged as promising candidates for skin regeneration. However, for restoring the integrity of the injured tissue, an appropriate balance of moisture and bioactivity needs to be maintained at the wound surface. Though several researchers have designed hydrogels from synthetic or natural resources, their applicability is restricted due to availability, cost and restricted properties suitable to specific wound types. In this study, a novel hydrogel composed of polysaccharide polymer from Moringa oleifera seeds and polyvinyl alcohol (MSP/PVA) was synthesized as a wound dressing material. The hydrogel was characterized using FTIR and XRD and evaluated for its fluid handling properties. It could absorb 5.7 g H2O g−1 dry weight with 20–30 % moisture being retained even after 24 h. Its good water absorption and donation ability make it appropriate for dry, necrotic and slightly exuding wounds. Its breathability and water vapor transmission rate extend it applicability to management of burns. The hydrogel exhibited hemocompatibility, antibacterial activity, bacterial impermeability, antioxidant activity and iron chelation that might help healing chronic wounds as well. It was biodegradable. In vivo wound healing showed that the rate of wound reduction and closure was accelerated with rapid re-epithelialization of partial thickness wounds in 6 days without scar formation. In vitro povidone–iodine loading and release studies showed that the iodine release followed Fickian diffusion process. The MSP/PVA hydrogel holds promise for management of dry, necrotic, slightly exuding, chronic wounds, burns and thus appears to be an economical alternative worth industrial exploitation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Traditional nursing practices for wound care aimed at keeping the wound dry. Wound, however, heals in a physiological environment conducive to tissue repair and regeneration. With the advent of Winter’s concept [1] of moist wound healing the purpose of dressing evolved from passive hemostasis and protection to an active role in facilitation of natural debridement, stimulation of proliferation and re-epithelialization and thus healing the wound in the shortest possible time with minimal pain, discomfort and scarring to the patient. A variety of active dressings composed of natural and synthetic polymers with sophisticated additional therapies have been developed for the purpose. The demand for natural polymers like bacterial celluloses, silk fibroin, carrageenan, carboxy methyl cellulose, pectin, collagen, gelatin, hyaluronic acid, chitosan and alginates and their blends is rising owing to their biocompatibility, renewability, non-toxicity and biodegradability in treatment of both acute and chronic wounds [2, 3]. A variety of formulations like hydrogels, semipermeable membranes, foams, hydrocolloids and hydrogels have been developed by such biomaterials that maintain the delicate moisture balance at the wound interface. However, products of animal origin raise issues related to adverse immune reactions in many patients and cultural sensitivities of societies. Availability, scalability, cost and ease of production are other limitations.
Plants and their extracts have also been used traditionally for wound management. They provide cheap and easily available sources of biopolymers and active ingredients. Antibacterial, anti-inflammatory, and wound healing activity of various plants have been extensively reported. Phytoactive ingredients include various chemical families like alkaloids, essential oils, flavonoids, tannins, terpenoids, saponins, and phenolic compounds [4]. Moringa oleifera, the ‘miracle tree’, has long been considered as a medicinal cabinet and used in traditional medicine to treat a variety of diseases. Leaf extracts of this plant have been studied for their wound healing potential [5] while the gum exudates from the stem have been studied for the film forming and gelling ability [6]. Muhammad et al. [7] reported that the aqueous fraction of M. oleifera leaves enhanced proliferation and viability as well as migration of human dermal fibroblast cells. They reported the presence of vicenin-2 in these extracts that may be responsible for the healing process. Seed extracts of this plant have been used variously as coagulant for water purification, analgesic, antipyretic and anti-asthmatic purposes [8, 9]. In an earlier communication of this laboratory [10], we reported in vitro wound healing potential of the biopolymer where the polymer powder was proposed as dressing for hemorrhagic wounds. The biopolymer was 56.4 % carbohydrate and 32.5 % protein. Its polysaccharide component had neutral sugars present comprising xylose (36 %), arabinose (22 %) and glucose, galactose and mannose (14 % each). We also observed that the biopolymer extracted from the pods had antioxidant and iron chelation activity [11]. Antimicrobial activity against Scenedesmus obliquus (green alga), Escherichia coli, Pseudomonas aeruginosa, Staphylococcus aureus, Bacillus sterothermophilus, Bacillus licheniformis and Herpes simplex virus type 1 and Polio virus type 1 has also been reported in Moringa sp. [8–10]. Satish et al. [12] suggested the role of fibrinogenolytic proteases in Moringa leaf and bark extracts for the procoagulant activity observed in these extracts. Though a number of exploratory studies on wound healing potential of Moringa extracts have been done; however, a wound dressing of commercial value is still not available.
Hydrogels are three-dimensional hydrophilic networks that carry high water content of >70 % which successfully promote rehydration. They help in immediate pain control, are easy to replace, absorb and prevent loss of body fluids, act as a barrier to invading microbes, permit gaseous exchange and may be used for controlled drug delivery. They have been successfully used for the rehydration of dry necrotic, sloughy, granulating, and epithelializing wounds. Considering this we aimed at synthesizing composite hydrogels using Moringa seed polymer (MSP) and polyvinyl alcohol (PVA) to determine its applicability in wet wound care. These hydrogels were evaluated for antioxidant activity, iron chelation, antibacterial activity, hemocompatibility, breathability, fluid handling capacity, bacterial penetration and in vivo wound healing ability. Povidone–iodine loading, release and antibiosis against common pathogenic bacteria were also studied and the gels were characterized using FTIR and XRD spectroscopy.
Experimental
Extraction of polymer and hydrogel synthesis
Pods of M. oleifera were collected locally and dried. Seeds and the dried mucilaginous part around it were ground to a fine powder followed by polymer extraction [10]. For hydrogel synthesis, 50 mL of 10 % (w/v) PVA solution was mixed with 50 mL solution of MSP (3, 5 and 7 %). To this mixture, 10.6 mL glutaraldehyde reagent (0.5 mL glutaraldehyde, 0.1 mL concentrated HCl and 10 mL absolute alcohol) was added as a cross-linker with constant stirring. Hydrogels were obtained by the conventional solution casting method. After drying at 40 °C the prepared hydrogels were washed thoroughly with distilled water to remove any unreacted chemicals, re-dried and stored at room temperature for further use. PVA hydrogels prepared similarly without MSP were used as control. All experiments were conducted in triplicate and analyzed statistically using Microsoft Excel 2007 statistical tool (Microsoft, Redmond, Washington, USA).
FTIR and XRD analyses
The major functional groups in the hydrogels were detected using Fourier transformed infrared (FTIR) spectroscopy (FTLA 2000, ABB Bomem, Canada) using KBr pellet [13]. The PVA powder and dry MSP/PVA hydrogels were subjected to X-ray diffraction (XRD-PW 1700, Philips, USA) using CuKα radiation generated at 40 kV and 40 mA. The range of diffraction angle was 10.00–70.00° of 2θ. The crystallinity of the PVA and the dry hydrogel was expressed as crystallinity index (CI) by Segal et al. [14], using the height of the peak I (2θ = 19.4°) and minimum height of the peak I′ (2θ = 40.0°) by the following equation:
Wet integrity and swelling ability
The dispersion characteristic/wet integrity of the hydrogel was examined by the modified method of Mishra et al. [15]. Hydrogels (2 × 2 cm) of different MSP concentrations (3, 5 and 7 %) were placed in 50 mL of simulated wound fluid (SWF), which consisted of 2.298 g L−1 sodium chloride and 0.368 g L−1 dehydrated calcium chloride in water [16]. The flask was gently swirled for 60 s without causing a vortex, and the integrity of the hydrogel was visually established.
To observe the water absorbing ability of the hydrogels composed of different MSP concentrations (3, 5 and 7 %), samples of 2 × 2 × 0.08 cm size were immersed in 50 mL distilled water at pH 7 for 120 min at room temperature. Swelling index and water absorption capacity (%) were calculated at 20 min intervals using the following equations:
where W h and W d are the weights (g) of swollen and dry hydrogel, respectively.The hydrogel having maximum water absorbing ability was further tested for its water absorption ability at different pH (3, 7 and 12), temperature (10 to 60 °C) and in SWF. Free swell capacity of the hydrogel was expressed as swelling index per 100 cm2.
Moisture retention capacity
To determine the moisture retention capacity (R h), swollen hydrogels were incubated at 37 °C with 70–75 % relative humidity [17]. The samples were weighed before incubation (W 0) and at different time intervals (W t). Moisture retention ability (R h) was measured using Eq. 4:
Fluid affinity
Fluid affinity of the hydrogel was determined by SMTL test method TM-238 based upon British Standard Specification [18]. Accordingly, 2 × 2 cm pre-weighed samples of the test material were placed onto the surface of gelatine (35 % in SWF) and agar (2 % in SWF) containing Petri plates. The plates were sealed to inhibit evaporative loss and were incubated for 48 h at 28 ± 1 °C. After incubation, the hydrogels were gently removed and re-weighed. On the basis of change in weight (%) of each sample, they were categorised as fluid absorbing or fluid donating, according to Table 1.
Water vapor transmission rate (WVTR)
WVTR was measured using the modified Water Cup Method [19]. For each WVTR determination a circular piece of the hydrogel (2 cm diameter, 1 mm thickness) was first equilibrated in air for 24 h and placed on a glass vial containing 10 mL distilled water. The edges of the sample were sealed with glue. Another circular piece of the same hydrogel was fixed on another vial without water as a reference. The complete assembly was then weighed accurately and placed in an incubator at 37 ± 1 °C with a relative humidity of 70-85 %. Weight measurements were made after every 60 min for 8 h. The amount of water vapor transmitted through the hydrogels was measured using the following equation:
where WVTR = water vapor transmission rate (g h−1 m−2), G = weight loss (g), t = time (h), and A = test area (vial mouth area) = 3.14 × 10−4 m−2
Oxygen permeability and hemocompatibility
Oxygen permeability through the hydrogel was performed after the method of Lu et al. [16]. The prepared hydrogel was placed on the top of an open 100 mL glass bottle containing 50 mL of de-ionized water and held in place with a screw lid (30 mm diameter). The negative control was a closed bottle with an airtight cap preventing oxygen from entering the flask whereas the positive control was an open flask allowing oxygen to enter the flask and dissolve in water as a recipient. The test flasks were placed in an open environment under constant agitation for 24 h. The water samples collected were then analyzed directly for their dissolved oxygen content using Oximeter 91 (WTW GmbH, Germany).
Thrombogenicity of the hydrogel surface was evaluated by the blood clot formation test after Imai et al. [20] using acid citrate dextrose (ACD) human whole blood obtained from the J.L.N. hospital, Ajmer.
Hemolytic activity was tested by the direct contact method according to ASTM F 756-00 [21] using 1 cm2 hydrogels equilibrated in phosphate buffer saline (PBS) for 24 h at 37 °C. Hemolysis (%) was calculated according to Eq. 6
where OD s , ODnc, and ODpc are optical densities of sample, negative control and positive control, respectively.
Povidone–iodine (PVP-I) loading and release
Iodine release kinetics was studied after Mishra et al. [15]. PVP-I was loaded on the hydrogels by immersing pre-weighed hydrogel pieces (W d) in an aqueous solution (1 mg mL−1) of the antimicrobial compound at 30 °C for 24 h in dark. The pieces (1 × 1 cm) were then dried at 40 °C for 24 h to remove residual water and reweighed (W0). The percentage of drug loading efficiency was calculated according to Eq. 7
For iodine release experiments, the PVP-I-loaded hydrogels were placed in 5-mL PBS at 30 °C with intermittent shaking and transferred to fresh PBS at predetermined time intervals. The amount of released iodine was assayed spectrophotometrically at 515 nm and the released content was calculated using a standard calibration curve.
To determine if the iodine release follows Fickian or non-Fickian diffusion, the data were analyzed using the Korsmeyer-Peppas equation [22] represented as:
and \( \log \left( {{{M_{\text{t}} } \mathord{\left/ {\vphantom {{M_{\text{t}} } {M_{\alpha } }}} \right. \kern-0pt} {M_{\alpha } }}} \right) = \log k\, + n\,\,\log \,\,t \), where \( {{M_{\text{t}} } \mathord{\left/ {\vphantom {{M_{\text{t}} } {M_{\alpha } }}} \right. \kern-0pt} {M_{\alpha } }} \) is the fraction of drug release at time t. A plot of \( \log \left( {{{M_{\text{t}} } \mathord{\left/ {\vphantom {{M_{\text{t}} } {M_{\alpha } }}} \right. \kern-0pt} {M_{\alpha } }}} \right) \) vs. log t yields a straight line and n, the diffusion exponent can be read from the slope of the line plot. The value of n is indicative of the mechanism of transport of the drug through the gel, k is the release rate constant incorporating structural and geometric characteristics of the delivery system. For Korsmeyer-Peppas model, the release exponent n ≤ 0.5 from thin films denotes Fickian diffusion while n values more than 0.5 but less than 1 represent anomalous (non-Fickian) transport and n = 1 is for case II transport.
Evaluation of antibacterial activity
Antibacterial activity of PVP-I-loaded hydrogels was determined by the disk (10-mm diameter) diffusion method [10] against common wound pathogenic bacteria Pseudomonas aeruginosa (ATCC 27853), Escherichia coli (ATCC 25922), Bacillus licheniformis (ATCC 12759) and Staphylococcus aureus (ATCC 25923). Unloaded hydrogels and PVA hydrogels were used as control. After incubation at 37 °C for 24 h, the anti-bacterial activity was evaluated on the basis of zone of inhibition formed.
Bacterial penetration test
Bacterial inoculum was prepared by adding 1 mL of 105 dilution of garden soil suspension in peptone broth with incubation at 37 °C for 24 h. Subsequently a 2 × 2 cm hydrogel was placed on the surface of nutrient agar plates and inoculated with 0.02 mL of culture inoculum (108 CFU mL−1 adjusted with 0.5 McFarland) in the centre. The plates were incubated at 37 °C for 24 h. After incubation, the hydrogels were removed and examined for bacterial growth under the surface where the hydrogels were placed [23]. Slides were prepared from the agar surface and Gram stained to confirm the presence/absence of bacterial growth under the hydrogel surface.
Antioxidant activity, iron chelation and reducing power
The antioxidant activity of the hydrogel based on scavenging of the stable 1,1-diphenyl-2-picrylhydrazyl (DPPH) free radical was assayed after Esa et al. [24] and calculated as below:
where A 0 is the absorbance of 0.06 mM methanolic DPPH only whereas A S is the absorbance of the reaction mixture.
Iron chelation was measured according to the modified method of Dinis et al. [25]. The inhibition of ferrozine-Fe2+ complex formation was calculated using Eq. 10
where A c and A s are absorbance of control and sample, respectively. Both the tests were performed on 1 × 1 cm pieces of hydrogel.
Total reducing power of the hydrogels was determined after Oyaizu [26]. Hydrogels (1 × 1 cm) were placed in a test tube with 2.5 mL of phosphate buffer (0.2 M, pH 6.6) and 2.5 mL of 1 % potassium ferricyanide. The mixture was incubated at 50 °C for 20 min. Then, 2.5 mL of 10 % trichloroacetic acid was added and centrifuged at 3000 g for 10 min. The supernatant (2.5 mL) was mixed with distilled water (5 mL) and 0.02 mL FeCl3 (0.1 %). After proper mixing, absorbance was measured at 700 nm against phosphate buffer (pH 6.6) as a blank. Ascorbic acid (1 mg mL−1) was used as reference material.
Evaluation of skin irritability and in vivo wound healing ability
The skin irritation test was carried out on Swiss albino mice following the norms of the International Organisation for Standardization (ISO). Commercial pellet diet (Lipton India) and drinking water were provided ad libitum. Animal experiments were carried out after obtaining the clearance from the institutional animal ethical committee. Animals were kept in individual cages under 25 ± 2 °C, 55 ± 10 % relative humidity, natural illumination, conventional diet and water. A single exposure test was performed after shaving the fur from the back of the test mice. UV sterilized, PVP-I-loaded hydrogels (2 × 2 cm) were applied on the shaved skin on the test group. Gauze moistened with 0.5-mL distilled water (negative control) was applied to the mice of control group. The hydrogel was secured in place by semi-occlusive bandages and left for 4 h. Thereafter, the application sites were observed at 1, 24, 48 and 72 h by removing patches. The skin reactions for erythema and oedema were described and evaluated according to the ISO norms [27] of classification system for skin reactions. The preliminary irritation index (PII) was determined using the primary irritation scores (PIS) for each animal at each time interval of observation and classified as follows: 0, non-irritating; >0–2.0, slightly irritating; 2.1–5.0, moderately irritating; >5.0, severely irritating. The PIS for both erythema and oedema at each specified time were added and divided by the total number of observations. The animals were observed for signs of gross toxicity and behavioral changes at least once daily during the test period.
For in vivo wound healing experiments Swiss albino mice weighing between 25 and 40 g were selected for the study and divided into three groups of three animals each. On the 0th day, the fur on the back of the mice was shaved. Before creating the wound, the back skin was locally anesthetized with lignocaine hydrochloride gel (Xylocaine® jelly). The skin of the anesthetized area was excised to partial thickness to obtain a wound of about 1 cm. Wounds of the animals in the control group were kept open without any treatment while those in standard group were applied with Ovidine® (5 % w/w povidone–iodine ointment).Animals in the test group were applied with PVP-I-loaded hydrogels secured in place using secondary gauze dressing. All the wounds were digitally photographed and the physical attributes of healing which mainly contributes for wound closure were studied by tracing the wound size at 0th, 3rd, and 6th day or till complete epithelialization occurred with standard reference ruler.
Biodegradability assessment
Biodegradability of the hydrogel was investigated by the modified method of Sedlarik et al. [28]. For this purpose, 1 g of garden soil was suspended in distilled water and after proper vortexing 10 mL of this suspension was inoculated in 90 mL of nutrient broth and incubated at 37 °C for 48 h for enrichment of microbes present in the soil. Thereafter, 2 × 2 cm dried and pre-weighed hydrogels were kept in 40 mL of nutrient broth and further inoculated with 10 mL of enriched culture. Simultaneously hydrogels were also kept in sterile nutrient broth without inoculum that served as a control. All the flasks were incubated at 37 °C for 28 days. Their morphologies were evaluated periodically every 7th day by visual observations. The hydrogels were dried in a desiccator and after complete drying the weight loss was measured by Eq. 11
where W 0 and W t are initial and final dry weights of the hydrogels after 4 weeks.
Results and discussion
Structural analysis of hydrogel
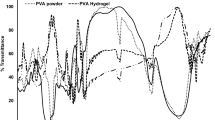
Infrared spectroscopy is a valuable tool to characterize the chemical structure and crystallinity of polymers. Figure 1 shows the FTIR spectra of MSP, PVA powder, MSP/PVA hydrogel and PVA hydrogel for comparison. The large bands between 3000 and 3500 cm−1 in PVA and MSP powder are linked to the stretching vibration of O–H bond from inter to intra-molecular hydrogen bonding. A strong reduction in the O–H peaks in the hydrogels was observed, perhaps due to formation of acetal bridges among the pendant hydroxyl groups of the polymer chains due to cross-linking of MSP with PVA via glutaraldehyde. The vibrational bands observed between 2800 and 3000 cm−1 refer to the stretching of C–H from alkyl groups. Peaks at 1708 and 1735 cm−1 in the hydrogels are due to C=O and C–O from acetate groups in PVA [13]. Two distinct strong absorption bands at 1645 cm−1 and 1540 cm−1represent α-helices of proteins present in the Moringa seed polymer. Reduction in the peak at 1645 cm−1 is indicative of involvement of C=O bonds in hydrogel formation [29]. The 1506 cm−1 peak in hydrogel corresponds to C=C stretching, while methylene scissor deformation typical of PVA can be seen at 1456 cm−1. A distinct peak at 1141 cm−1 is present in PVA powder which is absent in the hydrogel. The intensity of this peak is influenced by the crystalline portion of the polymeric chains. It is related to the symmetric C–C stretching mode or stretch of C–O of a portion of chain where an intra-molecular hydrogen bond is formed between two neighboring OH groups that are on the same side of the chain [13]. The absence of this peak in the hydrogel indicates breaking of the C–O–C and OH bonds and the formation of new cross-links with MSP. In MSP/PVA hydrogel asymmetric vibrations of S–O (sulfo) groups formed bands around 1265 cm−1 while that between 800 and 830 cm−1 in the polysaccharide region was due to C–O–S of sulphate esters of hexoses. The broad peak in the region 1200–900 cm−1 is characterized by –C–O, C–CH stretching and C–O, C–O–C bending of glycosidic rings in the saccharide groups of MSP [30]. Strong reduction of peaks in this region is indicative of involvement of the saccharide skeleton in bond formation.
The X-ray diffraction (XRD) analysis of MSP/PVA hydrogel was performed to investigate the crystalline behavior of the composite hydrogel. The diffractogram of pure PVA powder (Fig. 2) shows the characteristic peak for an orthothrombic lattice centred at 19.2º and 40.0° of 2θ indicating the presence of semi-crystalline phase [31]. Crystallinity is a measure of regularity in arrangement of structural elements. PVA is characterized by strong inter and intra hydrogen bonding between the chain. The MSP/PVA hydrogel showed a peak at 2θ of 19.4° indicating that crystallinity in the hydrogel was due to PVA. The peak intensity was, however, lesser in the MSP/PVA hydrogel than PVA powder with broadening of the peak at 2θ of 40.0º which suggests increase in amorphous nature of the hydrogel confirming association between MSP and PVA chains during hydrogel formation. The crystallinity as measured from the peak height method at 2θ of 19.4° and 40.0°, decreased from 75 % in PVA to 60 % in the composite hydrogel.
Wet integrity and swelling ability
Maintenance of integrity is important during application of a dressing, as a product with no dispersion will retain its original structure and therefore it is easier to remove. Wet integrity/dispersion indicates how the physical characteristics of a dressing will change when it interacts with wound fluid. Specifically, it determines whether it will form an amorphous gel or retain its original structure. Hydrogels immersed in SWF were visually evaluated for their integrity. An increase in the overall size and flexibility of the dressing was observed on swelling. The gels maintained their integrity in both water as well as SWF.
Before determining the water absorption capacity of MSP/PVA hydrogels as a function of MSP concentration and time at pH 7.0, the hydrogel sheets were conditioned by allowing them to equilibrate in air at room temperature for at least 24 h. Thus, the initial water content at time t = 0 prior to immersion in the de-ionized water was, in essence, the equilibrium water content in air. Each sample moved from the same equilibrium state in air to that in water. This ensured that the differences in osmotic driving force for water absorption between the samples could be related to their differences in composition and microstructure for the same osmotic shift in equilibrium.
The water absorption capacity increased with the increase in the concentration of MSP (Fig. 3). Maximum swelling index was observed with 7 % MSP. Concentrations higher than this led to formation of brittle and hard gels while concentration below 3 % formed soft and tacky gels that were difficult to remove from molds and were thus not considered for further studies. Swelling kinetics at all the three MSP concentrations showed fast rate of absorption in the first 80 min followed by a slow increase by 7.6 % to 13 % in the next 40 min (120 min stage). The MSP/PVA hydrogels absorbed a maximum of 4.8, 5.0 and 5.7 g H2O g−1 dry weight at 3, 5 and 7 % MSP concentration, respectively, as against PVA which absorbed 3.3 g H2O g−1 dry weight. The swelling ability of the gels remained unaltered in SWF. This can be ascribed to the cationic nature of MSP and/or due to the low cross-linking degree of the hydrogel [32].
Fluid handling properties of a dressing are important in determining the applicability of the product. While a product showing good water absorption and donation ability can be used as a hydrogel for hydration of dry and necrotic wounds, the one with an appropriate absorption and water vapor permeability can be used as a dry dressing for exuding wounds. The free swell capacity of the MSP/PVA hydrogels was 144.4 g 100 cm−2 which is better than the commercially available Kerramax® powder, a supersorbent dressing containing milled cross-linked polyacrylate with a mean free swell capacity of 74.14 g 100 cm−2. The product appears to be superior to some other synthetic dressings recommended for exuding wounds as Mesorb® (methylcelluose) and Eclypse® polyacrylate crystals that have been reported to have a mean free swell capacity of 76.16 and 52.29 g 100 cm−2 [33]. Thus, the MSP/PVA hydrogel can be used for exuding wounds.
Water absorption of MSP/PVA hydrogel was pH sensitive. It exhibited maximum absorption capacity of 5.64 g H2O g−1 dry weight at pH 7 which decreased by 75.7 and 21.8 % at pH 3 and 12, respectively (Fig. 4). The water absorption capacity of the hydrogel is attributed to the presence of ionisable groups viz. amines, carbonyl and hydroxyl in the polymer chain that can either accept or release proton in response to change in environmental pH. Presence of these groups is verified by the FTIR spectrum of the gel. In acidic media most carboxylic groups are protonated so decreased repulsion of anionic groups leads to decreased swelling ratio. At pH 12, charge screening effect of excess Na+ ions in medium is expected to shield the COO− group that prevents effective anion–anion repulsion. Carboxylate groups get ionized at pH 7.0 and the resultant electrostatic repulsion enhances the swelling capacity [34]. The pH sensitivity has been reported in other hydrogel systems and such pH sensitive hydrogels are suitable candidates for controlled drug release.
In the swollen state, water molecules form hydrogen bonds with polar groups of polymer backbone within the hydrogel and organize around hydrophobic groups causing gradual increase in volume and absorption capacity of hydrogels [35]. Temperature responsive swelling character was observed in the PVA and MSP/PVA hydrogels (Fig. 5). As the temperature of the hydrogel in the swelling state increased, the water content of the hydrogel also increased perhaps due to the association/dissociation of hydrogen bonds within hydrogels. The PVA gel lost physical integrity at 60 °C. The MSP/PVA hydrogel was more stable showing increase in the swelling index from 196 to 518 % when temperature increased from 10 to 50 °C translating into a water content of 1.96 to 5.18 g g−1 H2O, respectively. The volume of the hydrogel changed from 156 to 525 % with increase in temperature. Hydrophobic associations and hydrogen bonds play a vital role in the process. It has been postulated that temperature rise increases pore space of hydrogels by breaking cross-links and increasing kinetic energy of water molecules. However, at temperatures beyond 50 °C the MSP/PVA network collapses leading to an abrupt decrease in swelling index. This type of swelling behavior is called inverse (or negative) temperature dependence. Such behavior is shown by hydrogels containing moderately hydrophobic groups or a mixture of hydrophilic and hydrophobic groups. At lower temperatures, hydrogen bonding between hydrophilic groups and water dominates while at higher temperatures shrinking occurs due to strengthening of inter-polymer chain association through hydrophobic interactions [36]. A similar de-swelling at high temperature has also been reported by Kumari et al. [37] and Sadeghi et al. [38] in Psyllium polyacrylic acid hydrogel and starch-poly(sodium acrylate-co-acrylamide) hydrogel, respectively.
Moisture retention ability of hydrogels
Dehydration rate is an important feature to determine the applicability of a dressing. Moisture retention is especially crucial in burn injuries where heavy water loss from the wound bed by exudation and evaporation may lead to a fall in body temperature and increase in the metabolic rate [39]. On the other hand, excess moisture build up exacerbates infection and bad odor. Thus, optimal moisture content needs to be maintained at the wound surface to promote epithelial migration and autolytic debridement [2].
Both PVA and MSP/PVA hydrogels showed decrease in moisture content (Rh) with time (Fig. 6). A faster decrease was observed with PVA gels than the MSP/PVA gels. The results show that the two kinds of hydrogels lose water at rates of 0.04 g h−1 and 0.025 g h−1, respectively. After 24 h the total loss was approximately 70–80 %. Commercially available dressing like Geliperm (Geistlich, Switzerland) used mainly for burns and superficial pressure sores has been reported to show similar behavior losing about 50 % of its bound water after 12 h, and retaining about 30 % water after 24 h [17]. Lu et al. [16] reported that photocross-linked chitosan derivative hydrogels retained about 36.69 % water after 6 days of exposure to air and were suggested to be good for moderate exuding and skin burn wounds. Moisture retention capability of PVP/PEG/agar based wound dressing was about 40 % at 37 °C in 5 h [40] while oxidized alginate/gelatine blended hydrogels lost 30–40 % water in 1 day of air exposure increasing to 80 % over 4 days and were recommended for moderately exuding wounds [17].
Fluid affinity of hydrogels
The principle purpose of a hydrogel in a wound is to donate fluid to the wound. Available hydrogels vary in their water content ranging from 70 to 95 % [2]. The ability of hydrogel dressings to donate moisture helps in facilitating the rehydration of dry necrotic or devitalized tissue to promote autolytic debridement [41]. In addition, high fluid affinity will help to absorb excess wound exudate and liquefied tissue debris once autolytic debridement has taken place [2].The MSP/PVA hydrogel showed ability to absorb fluid with an increase in weight by 23 % on 2 % agar while donation to 35 % gelatin lead to a decrease in hydrogel weight by 17 % and thus can be considered as Type 3 days hydrogel dressing. Commercially available Carrasyn gel, Carrasyn V, Duo Derm gel and Solo Site have been reported to be fluid donors and better suited to dry, necrotic wounds. According to Jary et al. [42] moisturizing hydrogels (types d or e) are more effective on dry, necrotic wounds, while absorbent gels (types 3, 4 or 5) are useful on moist, fibrinous wounds. The MSP/PVA hydrogel with both fluid absorption and donation ability like DuoDerm gel [43] can find applicability on both dry and exuding wounds.
WVTR
Water loss from wounds needs to be controlled to maintain an optimal level of moisture to accelerate the healing process. A high WVTR for a wound dressing may lead to faster drying of the wound while a lower level will lead to accumulation of exudates thereby decreasing the healing process and open up the risk of infection [2].
Evaporative water loss for normal skin is 204 ± 12 g m−2 day−1 and for first, second and third degree burn it is 279 ± 26, 4272 ± 50.5, and 3432 ± 40 g m−2 day−1, respectively. For granulating wounds a high evaporative loss of 5138 ± 202 g m−2 day−1 is reported. It has been recommended that a rate of 2000–2500 g m−2 day would provide adequate level of moisture without risking wound dehydration [17]. The MSP/PVA hydrogel developed here had a WVTR of 2828 g m−2 day−1; equivalent to 117 g m−2 h−1 and is comparable to Biabrone and Omiderm which have been reported to have a WVTR of 154 and 208 g m−2 h−1 respectively and are used in burn wounds [44]. Lu et al. [16] recommended that photocross-linked chitosan derivative hydrogels with a WVTR of 2934–2561 g m−2 day−1 for skin burns while Balakrishnan et al. [17] developed hydrogel of oxidized alginate/gelatin with a WVTR of 2686 g m−2 day−1 for moderate to heavily exuding wound. Silver sulfadiazine-loaded PVA/chitosan blends with a WVTR of 2508 g m−2 day−1 showed applicability in the treatment of burn wounds in vivo [45]. Thus, the MSP/PVA hydrogel may be useful for the treatment of exuding wounds and burns.
Oxygen permeability
Adequate oxygenation is vital for all steps involved in wound healing as it plays a fundamental role in angiogenesis, fibroblast function, epithelialization and bacterial infection management [46]. Low oxygen concentration decreases the regeneration of tissue and slows down the healing process [16]. The solutions from the airtight negative control and the open flask (positive control) had dissolved oxygen values of 6.4 and 9.4 mg L−1, respectively, whereas those from flasks covered with MSP/PVA hydrogel had dissolved oxygen value of 8.3 mg L−1. This suggests that the prepared hydrogel will allow sufficient oxygen diffusion towards the wound.
Hemocompatibility of hydrogels
Blood compatibility of biomaterials designed for wound management is significant where dressing comes in contact with blood and damages the erythrocytes or leads to thrombus formation. MSP/PVA hydrogel was evaluated for blood compatibility and thrombogenic behavior. The hydrogel was found to be anti-thrombogenic with 33.33 % decrease in the weight of blood clot over control. While the positive control formed a clot weighing 0.81 g, the hydrogel formed 0.54 g clot. Earlier studies on MSP polymer showed that the polymer is thrombogenic; however, in hydrogel the property is reversed perhaps due to the reduction of surface charges by cross-linking with PVA that enhances the hydrophilicity [10, 47]. Further the hydrogels could be classified as non-hemolytic as they showed a hemolytic index of 1.8 % [21]. The studied hydrogel is although hemocompatible but it cannot be used for bleeding wounds for being anti-thrombogenic. They may prove to be of importance particularly in treatment of venous leg ulcers where complications occur as a result of thromboembolism [48].
Drug loading and releasing efficiency of hydrogels
Apart from maintaining a moist environment at the wound site, hydrogels also act as reservoir of drugs for localized delivery to prevent bacterial infection. In the present study, PVP-I a broad spectrum antimicrobial compound was used. MSP/PVA hydrogels showed 18, 20 and 23 % loading efficiency at 3, 5 and 7 % MSP concentrations, respectively. Thus, increasing the MSP concentration increased the PVP-I loading efficiency perhaps due to increase in pore volume of the gel. The swelling ability of the hydrogel decreased by 57.36 % in PVP-I solution as compared to swelling in water or SWF.
PVP-I acts as a reservoir of active iodine which is slowly released from the PVP-I complex. A number of studies have established its highly effective, broad spectrum antimicrobial action. Though contradictions do occur, however, numerous in vivo studies demonstrated that use of PVP-I is effective for the chronic wound environment [49]. Iodine released from the complex of PVP-I is rendered inactive following its use in destruction of microbial species and an equilibrium is maintained with further release of iodine until the iodine reservoir is exhausted. The amount of iodine released and the rate of release is important in determining the effectiveness of PVP-I-loaded wound dressings. Besides reducing the bacterial load of wounds, PVP-I has also been reported to help reduce excessive protease levels which inhibit the wound healing process [50].
Figure 7 shows the dependence of drug release on MSP/PVA mass ratio used. The release of the iodine increased with the increase in the MSP concentration. The MSP/PVA hydrogels released 25, 32 and 40 µg mL−1 iodine after 60 min with 3, 5 and 7 % MSP concentration equivalent to an increase of 25–60 %. Hydrogel samples with high PVP-I loadings show large initial bursts due to more drug clusters connected to the hydrogel surface [51]. This explanation is supported by the fact that this immediate release depends largely on the weight percent of the PVP-I-loaded in the hydrogel.
All the three types of hydrogels irrespective of their biopolymer content showed 50–70 % release of iodine in the first 20 min with a maximum release of 97–99 % in 60 min. The higher the weight percent of the PVP-I, the higher the percent of the iodine immediately released. The iodine release kinetics was analyzed by the Korsmeyer-Peppas equation. The values of diffusional exponent ‘n’ were 0.59, 0.50 and 0.49 for hydrogels of 3, 5 and 7 % MSP concentrations, respectively. For thin film ‘n’ values close to 0.5 indicate Fickian diffusion referring to a situation where water penetration rate in the gel is less than the polymer chain relaxation rate [22]. Kumar et al. [52] reviewed effective PVP-I concentrations for in vitro biocidal activity against bacteria, yeast, molds, actinomycetes and rickettsia along with the time required for the biocidal activity. Concentration of PVP-I in the range of 3.75–2500 µg mL−1 effectively kills Candida within 10–120 s whereas its 1000 µg mL−1concentration is effective for the Clostridium in 30–60 s. MSP/PVA hydrogels released 52 and 40 µg mL−1iodine after 60 min that may effectively control Staphylococcus, Bacillus, Candida and Actinomycetes.
Antibacterial activity
Infection delays the healing process, causes wound breakdown, prolonged hospital stay, increased trauma care and thus treatment costs [2]. Many bacterial agents are known to cause infections. Staphylococcus aureus followed by E. Coli and Pseudomonas aeruginosa are reported to be the most prevalent wound infection causing bacterial agents [53]. Antimicrobial dressings reduce the bacterial load and prevent bacterial by-products from damaging the wound bed.
Antibacterial activity of the MSP/PVA and their PVP-I-loaded hydrogels were investigated against four pathogenic bacteria that are commonly found in wound infections and cause delayed wound healing. As displayed in Table 2 the MSP/PVA hydrogel had inherent antibacterial activity against E. coli and B. licheniformis. Loading of PVP-I increased the antibacterial effect by increasing the zone size from 4 to 6 mm and 4 to 12 mm against E. coli and B. licheniformis, respectively with additional activity against S. aureus forming a 10 mm zone of inhibition.
Microbe penetration ability
Besides decontaminating wounds the dressing material should also act as a bacterial barrier to new invaders and possible hospital acquired infections. The MSP/PVA hydrogel was found to be impermeable to mixed microbial inoculum. No bacterial growth could be observed on the nutrient agar surface masked by the hydrogel film after 24 h of incubation though the lawn did grow beside the immobilized hydrogel. Thus the bulk network structure of the prepared hydrogel serves as a barrier for bacterial penetration.
DPPH, reducing power and iron chelation activity of hydrogel
Reactive oxygen species (ROS) play a vital role in the healing process. They restrict microbial invasions and promote healing by acting as messengers. They promote fibrosis leading to scar formation and in certain cases excess ROS cause extensive tissue damage by stimulating expression of matrix metalloproteases (MMPs), serine proteases and inflammatory cytokines rendering a non-healing state [54]. Therefore, control of oxidants in the wound for faster and scar-less wound healing is of importance. Antioxidants generally reduce the adverse effects of oxidants by scavenging radicals. The presence of reducing ability in the hydrogel, thus, improves its future potential healing ability. The MSP/PVA hydrogels exhibited 55.6 % DPPH activity as compared to ascorbic acid (72.5 %). The gel had a strong reducing ability displaying an absorbance of 0.125 which is comparable to ascorbic acid that showed an absorbance of 0.123 at 700 nm at a concentration of 1 mg mL−1.
Iron plays an important role in wound pathogenesis. It not only causes damage via ROS formation by the Fenton reaction but also increases the risk of wound infections like those caused by the opportunistic pathogen Vibrio vulnificus [55]. Thus chelation of iron from the wound site is an important issue for fast healing of wounds. Iron chelation has been known to reduce mortality in mice infected with Trypanosoma cruzi and pathogenesis by Pythium insidiosum [56]. The hydrogel used in the present study was capable of chelating 63 % iron which is comparable to ascorbic acid. Iron chelation perhaps reduces the redox potential of the hydrogel thereby stabilizing the oxidized form of the metal ions, suggesting their action as an antioxidant which may also be related to their iron binding capacity. This property of the hydrogel is particularly advantageous in chronic wounds where iron content shows a 20-fold rise via the attack of ROS and proteolytic enzymes occurring in non-healing wounds [57].
Skin sensitivity and in vivo wound healing potential of hydrogel
Skin irritation is a locally arising inflammatory reaction, which appears shortly after stimulation. Its main characteristics are the development of transient inflammatory reactions as evident by clinical signs of irritation viz. erythema (redness), oedema (swelling), itching, and pain. Skin irritation and sensitization response of the hydrogel and its wound healing potential was tested on Swiss albino mice. As per primary dermal irritation index there was no appearance of erythema or oedema in the presence of PVP-I-loaded MSP/PVA hydrogel that could be observed even after 72 h of application. No other signs of gross toxicity, adverse pharmacologic effects or abnormal behavior were observed.
Wound contraction plays a significant role in healing of excision wounds. The pro-healing activity of hydrogels containing M.oleifera seed biopolymer was observed macroscopically on incision wounds in Swiss albino mice and is presented in Fig. 8. After 3 days PVP-I-loaded MSP/PVA hydrogel-treated wounds showed 56.3 ± 3.2 % closure as against 43.3 ± 4.8 % and 33.3 ± 5.7 % closure by PVP-I ointment (Ovidine®)-treated and -untreated wounds, respectively. After 6 days, the hydrogel-treated wounds showed complete scar-less regeneration with restoration of hair growth while the untreated and PVP-I ointment-treated wounds healed in 10–12 days. Flavonoids, polyphenols and other important phytocomponents present in Moringa seed that are bioactive and have antioxidant and antibacterial action may be responsible for accelerated wound healing [10, 11].
Biodegradability assessment of hydrogels
Health care waste management is becoming a challenging problem for developing countries. Thus there is an increasing demand to develop new materials that are biodegradable and so environmental friendly. Biodegradable materials that can be easily degraded by in vivo enzymatic action are biocompatible and non-toxic are gaining attention in tissue engineering and controlled drug delivery.
Biodegradability of the hydrogels was studied under artificial composting like environment. Periodical examination of hydrogels showed transparent, smooth and flexible morphology of the hydrogels which served as control whereas hydrogels inoculated with soil microflora showed irregularities and roughness on the surface, with depositions, that could be the microflora that has entered into the polymer network. Their color became dark brown and flexibility increased upon stretching which indicated that the internal structure of the hydrogels was collapsing. The MSP/PVA hydrogel showed 27 % weight loss whereas PVA hydrogel showed only 11 % weight loss after 4 weeks of incubation. PVA is a slow biodegradable synthetic polymer. Bastioli et al. [58]. reported that an amylase-PVA composite (PVA-starch blend) was very slowly biodegraded and that 75 % weight loss required 300 days in a degradation test with activated sludge. Though the hydrogel showed better degradability, however, biodegradability cannot be accurately assessed as the weight of microbial biomass present inside the network which could not be accounted for. However weight loss of 27 % in the composite hydrogel against 11 % of PVA-based hydrogel signifies its importance in medical applications.
Conclusion
A novel biodegradable MSP/PVA hydrogel has been designed that may be potentially useful in wound management. The dressing exhibited good fluid handling capacity, biocompatibility, hemocompatibility, oxygen penetration and is recommended for dry, necrotic and low exuding wounds. The hydrogel also possessed antibacterial activity and was impermeable to bacteria. In vivo studies showed that the hydrogel accelerated the healing process without scar formation.
References
Winter GD (1962) Formation of the scab and the rate of epithelisation of superficial wounds in the skin of the young domestic pig. Nature 193:293–294
Boateng JS, Matthews KH, Stevens HNE, Eccleston GM (2008) Wound healing dressings and drug delivery systems: a review. J Pharm Sci 97:2892–2923
Boateng J, Catanzano O (2015) Advanced therapeutic dressings for effective wound healing—a review. J Pharm Sci 104:3653–3680
Thakur R, Jain N, Pathak R, Sandhu SS (2011) Practices in wound healing studies of plants. Evid Based Complement Alternat Med 2011:438056
Hukkeri VI, Nagathan CV, Karadi RV, Patil SV (2006) Antipyretic and wound healing activities of Moringa oleifera Lam in rats. Indian J Pharm Sci 1:124–126
Panda DS, Swain SS, Kanungo KS, Gupta R (2006) Preparation and evaluation of gels from gum of Moringa oleifera. Indian J Pharm Sci 68:777–780
Amali Muhammad A, Pauzi NAS, Aruselvan P, Abas F, Fakurazi S (2013) In vitro wound healing potential and identification of bioactive compounds from Moringa oleifera Lam. BioMed Res Int 2013:1–10
Bhargave A, Pandey I, Nama KS, Pandey M (2015) Moringa oleifera Lam.—Sanjana (horseradish tree)—a miracle food plant with multipurpose uses in Rajasthan-India-an overview. Int J Pure Appl Biosci 3:237–248
Ali GH, El-Taweel GE, Ali MA (2004) The cytotoxicity and antimicrobial efficiency of Moringa oleifera seeds extracts. Int J Environ Stud 61:699–708
Bhatnagar M, Parwani L, Sharma V, Ganguli J, Bhatnagar A (2013) Hemostatic, antibacterial biopolymers from Acacia arabica (Lam.) Willd. and Moringa oleifera (Lam.) as potential wound dressing materials. Indian JExp Biol 51:804–810
Parwani L, Bhatnagar M, Bhatnagar A, Sharma V (2012) Reactive oxygen species control by plant biopolymers intended to be used in wound dressings. Int J Pharm Pharm Sci 4:506–510
Satish A, Sairam S, Ahmed F, Urooj A (2012) Moringa oleifera Lam.: protease activity against blood coagulation cascade. Pharmacognosy Res 4:44–49
Mansur HS, Sadahira CM, Souza AN, Mansur AAP (2008) FTIR spectroscopy characterization of poly(vinyl alcohol) hydrogel with different hydrolysis degree and chemically crosslinked with glutaraldehyde. Mater Sci Eng C28:539–548
Segal L, Creely JJ, Martin AE Jr, Conrad CM (1962) An empirical method for estimating the degree of crystallinity of native cellulose using the X-ray diffractometer. Text Res J 29:786–794
Mishra A, Chaudhary N (2010) Study of povidone iodine loaded hydrogels as wound dressing material. Trends Biomater Artif Organ 23:122–128
Lu G, Ling K, Zhao P, Xu Z, Deng C, Zheng H, Huang J, Chen J (2010) A novel in situ-formed hydrogel wound dressing by the photocross-linking of a chitosan derivative. Wound Repair Regen 18:70–79
Balakrishnan B, Mohanty M, Umashankar PR, Jayakrishnan A (2005) Evaluation of an in situ forming hydrogel wound dressing based on oxidized alginate and gelatin. Biomaterials 26:6335–6342
Surgical Materials Testing Laboratory SMTL TM 238 (2005) Test method for fluid affinity of hydrogels. Report, Wales
American Society for Testing and Materials ASTM E (1996) Standard test methods for water vapour transmission of materials ASTM E 96-93. American Society for Testing and Materials, Philadelphia
Imai Y, Nose YJ (1972) New method for evaluation of antithrombogenicity of materials. J Biomed Mater Res 6:165–172
American Society for Testing and Materials ASTM F (2000) Standard practices for assessment of haemolytic properties of materials. American Society for Testing and Materials, Philadelphia
Chime Salome A, Onunkwo Godswill C, Onyishi Ikechukwu I (2013) Kinetics and mechanisms of drug release from swellable and non swellable matrices: a review. Res J Pharm Biol Chem Sci 4:97–103
Tomic SL, Micic MM, Dobic SN, Filipovic JM, Suljovrujic EH (2010) Smart poly(2-hydroxyethyl methacrylate/itaconic acid) hydrogels for biomedical application. Radiat Phys Chem 79:643–649
Esa NM, Hern FS, Ismail A, Yee CL (2010) Antioxidant activity in different parts of roselle (Hibiscus sabdariffa L.) extracts and potential exploitation of the seeds. Food Chem 122:1055–1060
Dinis TCP, Madeira VMC, Almeida LM (1994) Action of phenolic derivatives (acetaminophen, salicylate, and 5-aminosalicylate) as inhibitors of membrane lipid peroxidation and as peroxyl radical scavengers. Arch Biochem Biophys 315:161–169
Oyaizu M (1986) Studies on products of browning reaction: antioxidative activities of products of browning reaction prepared from glucosamine. Jpn J Nutr 44:307–315
International Organization for Standardization ISO 10993-10 (2003) Biological evaluation of medical devices-Part 10: tests for irritation and delayed-type hypersensitivity
Sedlarik V, Saha N, Sedlarikova J, Saha P (2008) Biodegradation of blown films based on poly(lactic acid) under natural conditions. Macromol Symp 272:100–103
El-Bahy GS, El-Sayed ESM, Mahmoud AA, Gweily NM (2012) Preparation and characterization of poly vinyl alcohol/gelatin blends. J Appl Sci Res 8:3544–3551
Bhatnagar M, Parwani L, Sharma V, Ganguly J, Bhatnagar A (2014) Exopolymers from Tolypothrix tenuis and three Anabaena sp. (Cyanobacteriaceae) as novel blood clotting agents for wound management. Carb Polym 99:692–699
Liu K, Li Y, Xu F, Zuo Y, Zhang L, Wang H, Liao J (2009) Graphite/poly(vinyl alcohol) hydrogel composite as porous ringy skirt for artificial cornea. Mater Sci Eng C 21:261–266
Matricardi P, Cencetti C, Ria R, Alhaique F, Coviello T (2009) Preparation and characterization of novel gellan gum hydrogels suitable for modified drug release. Molecules 14:3376–3391
Hampton S (2011) KerraMax®: managing highly exuding wounds. J Community Nurs 25:4–8
Sadeghi M, Ghasemi N, Kazemi M, Soleimani F (2012) Synthesis, swelling behavior, salt and pH sensitivity of cross linked carrageenan-graft-poly(acrylamide-co-itaconic acid) superabsorbent hydrogel. Middle-East Sci Res 11:311–317
Ruel-Gariepy E, Leroux J (2004) In situ-forming hydrogels- review of temperature sensitive systems. Eur J Pharm Biopharm 58:409–426
Du Toit LC, Kumar P, Choonara YE, Pillay V (2016) Electroactive polymers and coatings. In: Hosseini M, Makhlouf ASH (eds) Industrial applications for intelligent polymers and coatings. Springer, Switzerland
Kumari A, Kaith BS, Singha AS, Kalia S (2010) Synthesis, characterization and salt resistance swelling behaviour of psy-g-poly(AA) hydrogel. Adv Mater Lett 1:123–128
Sadeghi M, Hosseinzadeh H (2008) Synthesis and swelling behavior of starch-poly (sodium acrylate-co-acrylamide) superabsorbent hydrogel. Turk J Chem 32:375–388
Hoffman AS (2002) Hydrogels for biomedical applications. Adv Drug Deliv Rev 54:3–12
Soler DM, Rodriguez Y, Correa H, Moreno A, Carrizales L (2012) Pilot scale-up and shelf stability of hydrogel wound dressings obtained by gamma radiation. Radiat Phys Chem 81:1249–1253
Thomas S, Hughes G, Fram P, Hallett A (2005) An in vitro comparison of the physical characteristics of hydrocolloids, hydrogels, foams and alginate/cmc fibrous dressings. SMTL Rep 1–24
Jary A, Lurton Y, Gicquel V, Abault Y, Basle B (2007) Evaluation of the fluid affinities of amorphous hydrogel dressings. Le Journal des Plaies et Cica 58:97–100
Lay-Flurrie K (2004) The properties of hydrogel dressings and their impact on wound healing. Prof Nurs 19:269–273
Bruin P, Jonkman MF, Meijer HJ, Permings AJ (1990) A new porous polyether urethane wound covering. J Biomed Mater Res 24:217–226
Chakavala SR, Patel NG, Pate NV, Thakkar VT, Patel KV, Gandhi TR (2012) Development and in vivo evaluation of silver sulfadiazine loaded hydrogel consisting polyvinyl alcohol and chitosan for severe burns. J Pharm Bioallied Sci 4:S54–S56
Albert M (2008) The role of hyperbaric oxygen therapy in wound healing. Wound Care Canada 6:60–62
Leitão AF, Gupta S, Silva JP, Reviakine I, Gama M (2013) Hemocompatibility study of a bacterial cellulose/polyvinyl alcohol nanocomposite. Colloid Surf B 111:493–502
Simon DA, Dix FP, McCollum CN (2004) Management of venous leg ulcers. Brit Med J 328:1358–1362
Angel DE, Morey P, Storer JG, Mwipatayi BP (2008) The great debate over iodine in wound care continues: a review of the literature. Wound Pract Res 16:6–21
Eming SA, Smola-Hess S, Kurschat P, Hirche D, Krieg T, Smola HA (2006) Novel property of povidon-iodine: inhibition of excessive protease levels in chronic non-healing wounds. J Invest Dermatol 126:2731–2733
Huang X, Brazel CS (2001) On the importance and mechanisms of burst release in matrix-controlled drug delivery systems. J Control Rel 7:121–136
Kumar JK, Hemanth Kumar Reddy C, Gunashakaran V, Ramesh Y (2009) Application of broad spectrum antiseptic povidone iodine as powerful action: a review. J Pharm Sci Technol 1:48–58
Shrestha B, Basnet RB (2009) Wound infection and antibiotic sensitivity pattern of bacterial isolates. Postgrad Med J N 9:1–6
Wilgus TA, Bergdall VK, Dipietrol LA, Oberyszyn AM (2005) Hydrogen peroxide disrupts scarless foetal wound repair. Wound Rep Regen 13:513–519
Litwin CM, Rayback TW, Skinner J (1996) Role of catechol siderophore synthesis in Vibrio vulnificus virulence. Infect Immun 64:2834–2838
Zanette RA, Bitencourt PE, Alves SH, Fighera RA, Flores MM, Wolkmer P, Hecktheuer PA, Thomas LR, Pereira PL, Loreto ES, Santurio JM (2013) Insights into the pathophysiology of iron metabolism in Pythium insidiosum infections. Vet Microbiol 162:826–830
Halliwell B (1989) Protection against tissue damage in vivo by desferrioxamine: what is its mechanism of action? Free Radical Bio Med 7:645–651
Bastioli C, Bellotti V, Giudice LD, Gilli G (2009) Microstructure and biodegradability of mater-bi products. In: Vert M, Feijen J, Albertsson A, Scott G, Chiellini E (eds) Biodegradable polymers and plastics. The Royal Society of Chemistry, Cambridge
Acknowledgments
The authors are indebted to Department of Biotechnology (DBT), Govt. of India for providing financial support to Laxmi Parwani in terms of fellowship. For ACD human whole blood, authors are grateful to the Jawaharlal Nehru Hospital, Ajmer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Parwani, L., Bhatnagar, M., Bhatnagar, A. et al. Evaluation of Moringa oleifera seed biopolymer-PVA composite hydrogel in wound healing dressing. Iran Polym J 25, 919–931 (2016). https://doi.org/10.1007/s13726-016-0479-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13726-016-0479-8