Abstract
Purpose of Review
We explore how a global shift in the food system caused by global economic growth, increase in available food per capita and in food processing is a driver of the obesity epidemic.
Recent Findings
Economic development in most areas of the world has resulted in increased purchasing power and available per capita food. Supermarkets and a growing fast-food industry have transformed our dietary pattern. Ultra-processed food rich on sugars and saturated fat is now the major source of energy in most countries. The shift in food supply is considered a major driver of the obesity epidemic and the increasing prevalence of accompanying complications, such as type 2 diabetes, cardiovascular disease and cancer. However, the global shift might also have direct effects on the increase in type 2 diabetes, cardiovascular disease and cancer, independently of overweight and obesity.
Summary
The shift in the food supply is a major driver of the obesity epidemic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rising prevalence of overweight and obesity is a major global health challenge and concern [1]. For adults, overweight is defined as a body mass index (BMI) ≥25 kg/m2 and obesity as BMI ≥30 kg/m2. The World Health Organization defines overweight and obesity as abnormal or excessive fat accumulation that may impair health. Analysis of the Global Burden of Disease study 2013 revealed that during the last three decades, the prevalence of overweight and obesity rose 27.5 % in adults and 47.1 % in children [2••]. The prevalence of obesity is highest in the developed countries; however, almost two thirds of the obese population live in developing countries [3]. According to the Global Burden of Disease study 2013, the increase in overweight and obesity was highest between 1992 and 2002, and while the rate of increase seems to have slowed down during the past decade in developed countries, a continued increase has been observed in the developing countries [2••].
Weight- and obesity-related complications include type 2 diabetes, cardiovascular disease and cancer [4]. The rise in weight-related health problems has not only cost millions of people their wellbeing but also carries significant costs to the society due to obesity-related illness [5]. In developed countries, treatment of obesity and obesity-related complications has increased the cost of healthcare. Especially type 2 diabetes accounts for a majority of healthcare costs, as 20–30 % of overweight people have type 2 diabetes, while approximately 85 % of diabetic subjects are overweight or obese [6]. Besides the direct costs reflected in healthcare, indirect costs associated with obesity include decreased work productivity, high workers’ compensation claims and lower earnings. Overweight and obesity are not only a burden for the individual and society in general, but also an economic burden for the employer, since the epidemic is associated with lower productivity due to an increase in sick leave and medical claims.
The dominating food source was once local production for local markets. The way from farm to fork involved relatively little processing, whereas the modern food system is characterized by interactions between multiple global players to maximize efficiency, reduce costs and increase production and profit before food reach the household. This change in the food system is considered a major driver of the obesity epidemic, which will be further explored in this review.
Changes in the Food System
Technology, urbanization and shift in income are some of the factors that have profoundly changed the global food system and thereby food consumption [7]. The shift to a global food system started in the USA and other high-income industrialized countries while the system is now rapidly changing in developing countries as well. The major drivers behind the change are development in the technology related to food production and processing. Modern food distribution means global access to a wider variety of foods [8]. With urbanization follows increased consumption of food produced by others [9]. Large regional or local supermarkets replace fresh markets as the major source of food. These supermarkets are often part of multinational or domestic chains and they transform the dietary pattern, together with a growing fast-food industry [10].
Food consumption is increasingly affected by marketing and mass media; the transnational food corporations target potential consumers through marketing campaigns, especially aggressive in the developing countries where increased income means potential new consumers [11].
Assessment of Food Consumption
Dependable means of measuring food consumption are required in order to study how the shift in the food system has changed consumption around the world. In the following, we describe the most applied methods to assess food consumption on the population level.
Individual Dietary Surveys
Detailed monitoring of food consumption patterns can be derived from surveys of dietary intake conducted on national selected representative cohorts of individuals. Methods for assessing dietary intake can be retrospective reporting of intake (recent or remote past) or prospective recording of food consumption [12]. Persons included need to be highly motivated to register complete diet. Many countries do not have resources to perform regular, high-quality person-level dietary surveys of food consumption, and there is variation in the methods used, causing difficulties in the interpretation and comparison of surveys between countries [11].
Household Budget Surveys
Household budget surveys, often conducted by national statistical offices, contain data on food purchased and food from own production. Household budget surveys estimate food available at the household level and are cheaper than person-level surveys. Limitations to these surveys as an estimate of food consumption include lack of information of food consumed outside the home, the distribution of food between household members, food used for other reasons and food waste. As for individual dietary surveys, an important limitation is the variation in the methods applied [13].
Supermarket Sales Data
Most supermarkets use electronic product labels or product codes to identify and track sales items. Supermarket sales data potentially holds information about dietary habits and behaviours at the population level. However, barriers include the link from bought food to food consumed by an individual and the link between sales item codes and nutritional content [14, 15].
Food Balance Sheets
Food balance sheets (FBS) as prepared by the Food and Agriculture Organization of the United Nations provide information of food availability [11]. FBS balance food production, net trade of food and estimates of food fed to animals or in other ways not available for human consumption. These data are available online (http://faostat.fao.org). FBS estimate food available for the consumer. Limitations for using FBS as a proxy for food consumption include lack of information on food waste at the household and retail level and other potential errors discussed elsewhere [13]. When compared to individual dietary surveys, FBS tend to overestimate food consumption [16]. However, FBS are available for all countries and hold long-term trends in food availability why FBS are often used as a proxy for food consumption.
Shift in Food Consumption and the Link to the Overweight and Obesity Epidemic
Increased Energy Intake
Ultimately, obesity reflects energy imbalance. Global estimates, based on FBS, indicate that the available per capita food in developed countries was 3138 kcal/person/day in 1969/1971 and 3360 kcal/person/day between 2005 and 2007. In developing countries, the per capita food available increased from 2055 to 2619 kcal/person/day during the same three and a half decade [3]. Most areas of the world have shown economic development that has resulted in increased purchasing power which is an important factor in explaining the increasing caloric intake [17]. Of note, according to some income projections for 2050, the world will be immensely richer and with less pronounced relative gaps between the per capita incomes of the developed and developing countries [18, 19].
A recent global analysis found that a higher energy intake was sufficient to explain the increasing population body weight especially in high-income countries [20•]. An energy intake body weight model was used to evaluate whether the change in energy intake (estimated from FBS) was sufficient to explain the change in body weight. Body weight was estimated from global databases, national health and nutrition survey reports and peer-reviewed papers with at least 4 years between two observations. Also, studies with more robust weight estimates have previously found similar results in two populations: Swinburn et al. revealed that higher energy intake estimated from the US food supply data was sufficient to explain the increases in body weight in the US population from the 1970s to 2000s [21]. Scarborough et al. reported that higher energy intake, estimated from FBS, explained most of the body weight increase in the UK from 1980s to 2000s [22].
Modern Diet: Energy-Dense, Ultra-Processed Food
While the traditional dietary pattern was based on fresh food, the modern diet is primarily based on processed food most often made and sold by transnational corporations. Food processing is a variety of operations by which raw ingredients are extracted or refined. Processed food is durable, convenient, ready to consume and often cheap compared to fresh food. Food processing is increasingly discussed as an important contributor to the obesity epidemic [23]. Monteiro et al. have proposed a food classification system based on the extent of processing. The system subdivides food into three groups: (1) unprocessed and minimally processed (rice, meat, fruits, etc.) food. This is whole food which is minimally processed in various ways (cleaning, freezing, pasteurization, fermenting, etc.) that do not alter the nutritional properties substantially; (2) processed culinary or industry ingredients (sugar, vegetable oils, pasta, etc.); and (3) ultra-processed products (breads, sweets, ready to eat/heat meals, etc.). Ultra-processed food is a result of group 2 substances with no or little amounts of minimally processed food from group 1 [24]. Ultra-processed food is designed to be convenient, ready to eat, and is most often consumed alone or in combination with other processed food (bread with burger, etc.). Because ultra-processed food is accessible, convenient and portable, it induces unhealthy dietary patterns such as skipping main meals and eating while doing other things [25].
Studies conducted, using the classification system, indicate that ultra-processed foods are replacing traditional diets both in developed and developing countries. A Norwegian study from 2015, using supermarket sales data, found that ultra-processed foods represented 58.8 % of purchases in food retailers and minimally processed foods accounted for 17.2 % [26]. A recent study using the classification system on household budget surveys reported that over 61 % of dietary energy in Canada came from ultra-processed food, and data from Sweden show a dramatical increase in consumption of ultra-processed food [27•, 28]. In developing countries such as Chile and Brazil, studies applying the classification system on household budget surveys data reported consumption of ultra-processed food to replace foods from groups 1 and 2 [29, 30]. With increased purchasing power in the developing countries, ultra-processed food has become more affordable and the convenience of these products becomes important when people have less time. It is cheap compared to traditional diets, and modern food marketing is concentrated on ultra-processed products compared to the less profitable non- or minimally processed food [25].
Traditional diets mainly made from unprocessed and minimally processed food and even when mixed with group 2 substances usually have adequate nutrient and energy density [25]. Compared to traditional diet, ultra-processed products are more energy dense; have more added simple sugars (six times higher than food from groups 1 and 2), sodium and saturated fat and are low in dietary fibre (half compared to food from groups 1 and 2) [27•, 30]. In Canada, dietary patterns dominated by ultra-processed food exceeded World Health Organization recommendations (designed to prevent and control obesity) for fat, sugar and sodium, and are low on dietary fibre [27•]. Evidence from three prospective cohorts including 120.877 American women and men shows that weight gain over a 4-year period is associated with consumption of various processed foods (such as potato chips, French fried potatoes, sugar-sweetened beverages and processed meats) and inversely associated with consumption of unprocessed food (however, not using the classification system mentioned above) [31].
In summary, the global economic growth, increase in available per capita food and ultra-processed food as the dominating source of energy have caused a global shift in the food system. This shift is considered a major driver of the increasing prevalence of overweight and obesity throughout the world.
Overweight- and Obesity-Related Complications
A major concern associated with the increasing prevalence of overweight and obesity is the high risk of accompanying complications, such as type 2 diabetes, cardiovascular disease and cancer. The health-related and economic problems associated with these comorbid disorders are pronounced. In a recently published study including more than 10 million participants from 239 prospective studies across four continents, all-cause mortality was minimal for persons with BMI between 20 and 25 kg/m2. The relationship of BMI to mortality was strong and positive; hazard ratio per 5 kg/m2 units higher BMI was 1.39 (95 % confidence interval 1.34–1.43) in Europe, 1.29 (1.26–1.32) in North America, 1.39 (1.34–1.44) in east Asia and 1.31 (1.27–1.35) in Australia and New Zealand [32••]. Calle et al. showed in a large prospective study involving more than one million men and women that the lowest rates of death from all causes were found at BMI between 23.5 and 24.9 kg/m2 in men and 22.0 and 23.4 kg/m2 in women [33]. Death rates increased throughout the range of overweight and obesity for both men and women in all age groups [33]. Of note, life expectancy of a moderately obese person could be shortened by 2 to 5 years, while morbidly obese men could reduce their life expectancy by almost 13 years [34]. In the Prospective Studies Collaboration, including 900,000 adults, it was demonstrated that for BMI above 25 kg/m2, every 5 kg/m2 higher BMI was associated with 30 % higher overall mortality; 40 % for vascular; 60–120 % for renal, hepatic and diabetic; 10 % for neoplastic and 20 % for respiratory and for all other mortality [35]. A recent pooled analysis of 97 prospective cohorts with 1.8 million participants reported for BMI above 25 kg/m2, every 5 kg/m2 to be associated with 27 % higher risk of coronary heart disease and 18 % higher risk of stroke. Higher blood pressure, cholesterol and glucose were found to mediate half of this excess risk of coronary heart disease and two thirds of the excess risk of stroke, with blood pressure as the most important mediator [36].
The increasing prevalence of obesity and the severe health-related problems are a major global socioeconomic burden.
Food supply, Type 2 Diabetes, Cardiovascular Disease and Cancer
Type 2 Diabetes
The number of people with diagnosed diabetes has risen from 108 million in 1980 to 422 million in 2014, and the rise is expected to continue. The global prevalence of diabetes among adults over 18 years of age has risen from 4.7 % in 1980 to 8.5 % in 2014. Diabetes prevalence has been rising more rapidly in middle- and low-income countries [37].
The global shift in the food system and in particular the excessive caloric intake is a major driving force behind the escalating obesity and type 2 diabetes epidemics worldwide; however, diet quality also has independent effects on the increasing prevalence of type 2 diabetes. In a study using econometric models of repeated cross-sectional data on diabetes and nutritional components of food from 175 countries, a relationship was observed between dietary sugar exposure and diabetes, which was not explained by common variables including obesity [38]. In a systematic review and meta-analysis, Imamura et al. examined the prospective associations between consumption of sugar-sweetened beverages, artificially sweetened beverages and fruit juice with development of type 2 diabetes. The authors concluded that habitual consumption of sugar-sweetened beverages was associated with a higher incidence of type 2 diabetes, independently of adiposity [39]. In a subsequent modelling study, using data from the UK, it was proposed that an incremental reduction in free sugars added to sugar-sweetened beverages without the use of artificial sweeteners could reduce the prevalence of overweight, obesity and type 2 diabetes [40]. Higher intake of saturated fat and trans-fat has also been associated with type 2 diabetes, independently of obesity [41, 42]. Furthermore, in a review seeking to assess current knowledge on the potential epidemiological determinants for development of adipose tissue inflammation causing obesity-related complications (type 2 diabetes, cardiovascular disease, cancer), trans-fatty acid was proposed as a potential determinant contributing to the inflammation in obesity [43].
Cardiovascular Disease
Diet quality also has independent effects on the risk of developing cardiovascular disease. In a recent state-of-the-art review exploring the impact of food consumption on development of cardiovascular disease, higher intake of refined, high-glycaemic carbohydrates, excessive sugar-sweetened beverage consumption, intake of red and processed meats and trans-fatty acids were all associated with higher risk of cardiovascular disease [44].
Cancer
While there is strong evidence that overweight and obesity increase the risk of a number of cancer types including colorectal cancer, oesophageal cancer and endometrial cancer in women [45], evidence is also linking intake of red and processed meat to development of colorectal, pancreatic and prostate cancer [46]. Further, higher consumption of salt, salted food and food containing sugars is associated with an increased risk of stomach and colorectal cancer [47].
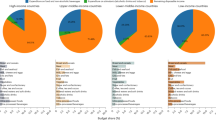
As previously highlighted, the global increase in food consumption, including higher intake of ultra-processed food (rich on sugar and saturated fat) is considered a major driver of the obesity epidemic. However, the global shift in food consumption and supply might have direct effects on the increase in type 2 diabetes, cardiovascular disease and cancer, independently of overweight and obesity (Fig. 1).
The global shift in food supply is considered a driver of the obesity epidemic and the increasing prevalence of accompanying complications, such as type 2 diabetes, cardiovascular disease and cancer. However, the global shift might also have direct effects on the development of type 2 diabetes, cardiovascular disease and cancer, independently of obesity
What are the possible mechanisms explaining a direct link between the shift in food supply and risk of type 2 diabetes, cardiovascular disease and cancer?
Evidence suggests that dietary factors alter intestinal ecology in both rodent models and in humans, and the changed ecology has been associated with clinical consequences [48]. Higher intake of ultra-processed food has been shown to induce dysbiosis (abnormal changes in gut microbiota composition), which has been directly linked to type 2 diabetes, cardiovascular disease and cancer. Type 2 diabetes is a metabolic disorder defined by insulin resistance, endotoxaemia, impaired intestinal permeability and chronic low-grade inflammation, all of which have been linked to diet-induced dysbiosis [49]. With regard to cardiovascular disease, high-fat, high red meat and low-fibre diets (the characteristics of a diet consisting of ultra-processed food) have been associated with reduced microbiota diversity, increased relative abundance of undesirable microorganisms and increased production of toxic compounds including the cardio-toxicant trimethylamine N-oxide (TMAO) [50]. TMAO is a gut microbiota-dependent metabolite shown to be both mechanistically linked to atherosclerosis and whose levels have been strongly linked to cardiovascular disease [51]. Lastly, there is increasing evidence linking the gut microbiota and cancer. As previously stated, diets high in fat and sugar and low in fibre may result in reduced gut microbiota diversity. Combined with the unfavourable effects of these diets that are mediated by dietary components and microbial metabolites, it is likely that these diets increase the risk of colorectal cancer [52].
Taken together, these data indicate changes in the gut microbiota as a potential direct link between the global shift in the food system and risk of developing type 2 diabetes, cardiovascular disease and colorectal cancer; potentially also occurring in normal-weight individuals.
Key Actions to a Healthier Food System
What is the most effective way to slow the obesity epidemic and the rising number of obesity-related complications? In this review, we have addressed how global economic growth, increase in available per capita food and cheap and unhealthy ultra-processed food have caused a global shift in the food system, and how this system is a major driver of the overweight and obesity epidemic.
While the global economic growth has enabled improved healthcare services including treatments, there has been an unexpected rise in the number of diseases and illnesses related to increased prosperity at the same time, with obesity as the major concern [53]. In many developing countries, the economic growth has led to a shift from populations being underweight towards overweight. The cost associated with the burden of overweight is expected to be vast and to affect individuals, families and entire countries. This could potentially lead to a paradoxical reduction in the economic growth of the countries, as a burden of overweight adversely affects various factors of economic growth, including labour supply, productivity, investment and education. It is important to identify strategies for simultaneously controlling the climbing prevalence of overweight while maintaining the decrease in underweight. Appropriate, integrated and cost-effective public health interventions are needed in order to further reduce the prevalence of underweight and to prevent the increase in overweight [54].
The increased general income is a major driver of the rise in available per capita food, which has been directly linked to the higher prevalence of obesity. However, the global shift in the food system has led to a change in which type of food we consume, where ultra-processed food is the major calorie contributor.
Public health interventions, education and information campaigns are warranted to reduce the consumption of ultra-processed food. Dietary guidelines and collaboration with the food industry to label healthier food choices based on processing, added sugar, salt and saturated fat can help people to make healthier food choices [7, 55]. It is important to realize that the global food systems do not aim to deliver optimal human diets; their primary aim is to maximize profits. Ultra-processed food has long shelf life and/or is ready to consume, which is an enormous commercial advantage over fresh food. Therefore, the public health interest in reducing consumption of ultra-processed food conflicts with transnational food corporation’s interest in increasing sales [56]. Cooperation with the food industry is a possible way of reducing consumption of ultra-processed food. The UK salt reduction programme is a successful example of product reformulation in cooperation with the industry to reduce salt intake [57]. Multifactorial systemic changes are needed to slow the obesity epidemic, and it has recently been argued that the only evidence-based approaches to address the disease burden caused by unhealthy commodities are public regulation and market intervention [58].
Conclusion
Global economic growth, increase in available per capita food and low-cost high-energy content ultra-processed food have caused a global shift in the food system and changed the dietary pattern. The shift in food supply is considered a major driver of the obesity epidemic and the increasing prevalence of accompanying complications, such as type 2 diabetes, cardiovascular disease and cancer. However, the global shift might also have direct effects on the increase in type 2 diabetes, cardiovascular disease and cancer, independently of overweight and obesity. Multifactorial systemic changes, especially public regulation and market interventions, are needed to slow the obesity epidemic.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–14.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81. This paper estimates global, regional and national prevalence of overweight and obesity in children and adults from 1980–2013.
Alexandratos N, Bruinsma J. World agriculture towards 2030/2050: the 2012 revision. Rome: FAO; 2012.
Pi-Sunyer X. The medical risks of obesity. Postgrad Med. 2009;121(6):21–33.
Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12(2):131–41.
Daousi C, Casson IF, Gill GV, MacFarlane IA, Wilding JP, Pinkney JH. Prevalence of obesity in type 2 diabetes in secondary care: association with cardiovascular risk factors. Postgrad Med J. 2006;82(966):280–4.
Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21.
Ludwig DS. Technology, diet, and the burden of chronic disease. JAMA. 2011;305(13):1352–3.
Popkin BM. Nutrition transition and the global diabetes epidemic. Curr Diabetes Rep. 2015;15(9):64.
Stuckler D, McKee M, Ebrahim S, Basu S. Manufacturing epidemics: the role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med. 2012;9(6):e1001235.
Kearney J. Food consumption trends and drivers. Philos Trans R Soc Lond B Biol Sci. 2010;365(1554):2793–807.
Barrett-Connor E. Nutrition epidemiology: how do we know what they ate? Am J Clin Nutr. 1991;54(1 Suppl):182S–7.
Hawkesworth S, Dangour AD, Johnston D, Lock K, Poole N, Rushton J, et al. Feeding the world healthily: the challenge of measuring the effects of agriculture on health. Philos Trans R Soc Lond B Biol Sci. 2010;365(1554):3083–97.
Eyles H, Jiang Y, Ni Mhurchu C. Use of household supermarket sales data to estimate nutrient intakes: a comparison with repeat 24-hour dietary recalls. J Am Diet Assoc. 2010;110(1):106–10.
Tin ST, Mhurchu CN, Bullen C. Supermarket sales data: feasibility and applicability in population food and nutrition monitoring. Nutr Rev. 2007;65(1):20–30.
Serra-Majem L, MacLean D, Ribas L, Brule D, Sekula W, Prattala R, et al. Comparative analysis of nutrition data from national, household, and individual levels: results from a WHO-CINDI collaborative project in Canada, Finland, Poland, and Spain. J Epidemiol Community Health. 2003;57(1):74–80.
Gerbens-Leenes PW, Nonhebel S, Krol MS. Food consumption patterns and economic growth. Increasing affluence and the use of natural resources. Appetite. 2010;55(3):597–608.
van der Mensbrugghe D, Osorio-Rodarte I, Burns A, Baffes J. Macroeconomic environment and commodity markets: a longer term outlook, paper for expert meeting on how to feed the world in 2050. In: Conforti P, editor. Rome: FAO, 24–26 June 2009, chapter 5; 2011.
Fontagne L. The world economy in 2050: a tentative picture. CEPII Working paper 2010-27 (http://www.cepii.fr/anglaisgraph/bdd/baseline.htm). 2010.
Vandevijvere S, Chow CC, Hall KD, Umali E, Swinburn BA. Increased food energy supply as a major driver of the obesity epidemic: a global analysis. Bull World Health Organ. 2015;93(7):446–56. This paper investigates the association between changes in national food energy supply and in average population body weight.
Swinburn B, Sacks G, Ravussin E. Increased food energy supply is more than sufficient to explain the US epidemic of obesity. Am J Clin Nutr. 2009;90(6):1453–6.
Scarborough P, Burg MR, Foster C, Swinburn B, Sacks G, Rayner M, et al. Increased energy intake entirely accounts for increase in body weight in women but not in men in the UK between 1986 and 2000. Br J Nutr. 2011;105(9):1399–404.
Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev. 2013;14 Suppl 2:21–8.
Monteiro CA, Levy RB, Claro RM, Castro IR, Cannon G. A new classification of foods based on the extent and purpose of their processing. Cad Saude Publica. 2010;26(11):2039–49.
Monteiro CA. Nutrition and health. The issue is not food, nor nutrients, so much as processing. Public Health Nutr. 2009;12(5):729–31.
Solberg SL, Terragni L, Granheim SI. Ultra-processed food purchases in Norway: a quantitative study on a representative sample of food retailers. Public Health Nutr. 2016;19(11):1990–2001.
Moubarac JC, Martins AP, Claro RM, Levy RB, Cannon G, Monteiro CA. Consumption of ultra-processed foods and likely impact on human health. Evidence from Canada. Public Health Nutr. 2013;16(12):2240–8. This paper investigates the consumption of ultra-processed food in Canada and the dietary quality.
Juul F, Hemmingsson E. Trends in consumption of ultra-processed foods and obesity in Sweden between 1960 and 2010. Public Health Nutr. 2015;18(17):3096–107.
Crovetto MM, Uauy R, Martins AP, Moubarac JC, Monteiro C. Household availability of ready-to-consume food and drink products in Chile: impact on nutritional quality of the diet. Rev Med Chil. 2014;142(7):850–8.
Monteiro CA, Levy RB, Claro RM, de Castro IR, Cannon G. Increasing consumption of ultra-processed foods and likely impact on human health: evidence from Brazil. Public Health Nutr. 2011;14(1):5–13.
Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–404.
Global BMIMC. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;338:776. This paper investigates the association between overweight, obesity and all-cause mortality.
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath Jr CW. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341(15):1097–105.
NIDDK Weight-control Information Center: U.S. Department of Health and Human Services NIoHSRtOaONPN.
Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96.
Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration, Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet. 2014;383(9921):970–83.
Broome ME, Knafl K. Back to the future: building on the past. J Pediatr Nurs. 1994;9(3):208–10.
Basu S, Yoffe P, Hills N, Lustig RH. The relationship of sugar to population-level diabetes prevalence: an econometric analysis of repeated cross-sectional data. PLoS ONE. 2013;8(2):e57873.
Imamura F, O’Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, et al. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ. 2015;351:h3576.
Ma Y, He FJ, Yin Y, Hashem KM, MacGregor GA. Gradual reduction of sugar in soft drinks without substitution as a strategy to reduce overweight, obesity, and type 2 diabetes: a modelling study. Lancet Diabetes Endocrinol. 2016;4(2):105–14.
Hu FB, van Dam RM, Liu S. Diet and risk of type II diabetes: the role of types of fat and carbohydrate. Diabetologia. 2001;44(7):805–17.
Salmeron J, Hu FB, Manson JE, Stampfer MJ, Colditz GA, Rimm EB, et al. Dietary fat intake and risk of type 2 diabetes in women. Am J Clin Nutr. 2001;73(6):1019–26.
von Scholten BJ, Andresen EN, Sorensen TI, Jess T. Aetiological factors behind adipose tissue inflammation: an unexplored research area. Public Health Nutr. 2013;16(1):27–35.
Anand SS, Hawkes C, de Souza RJ, Mente A, Dehghan M, Nugent R, et al. Food consumption and its impact on cardiovascular disease: importance of solutions focused on the globalized food system: a report from the workshop convened by the World Heart Federation. J Am Coll Cardiol. 2015;66(14):1590–614.
Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer. 2004;4(8):579–91.
Bouvard V, Loomis D, Guyton KZ, Grosse Y, Ghissassi FE, Benbrahim-Tallaa L, et al. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015;16(16):1599–600.
Varughese GI, Patel JV, Tomson J, Lip GY. Effects of blood pressure on the prothrombotic risk in 1235 patients with non-valvular atrial fibrillation. Heart. 2007;93(4):495–9.
Chan YK, Estaki M, Gibson DL. Clinical consequences of diet-induced dysbiosis. Ann Nutr Metab. 2013;63 Suppl 2:28–40.
Cani PD, Osto M, Geurts L, Everard A. Involvement of gut microbiota in the development of low-grade inflammation and type 2 diabetes associated with obesity. Gut Microbes. 2012;3(4):279–88.
Tuohy KM, Fava F, Viola R. ‘The way to a man’s heart is through his gut microbiota’—dietary pro- and prebiotics for the management of cardiovascular risk. Proc Nutr Soc. 2014;73(2):172–85.
Tang WH, Hazen SL. The contributory role of gut microbiota in cardiovascular disease. J Clin Invest. 2014;124(10):4204–11.
Louis P, Hold GL, Flint HJ. The gut microbiota, bacterial metabolites and colorectal cancer. Nat Rev Microbiol. 2014;12(10):661–72.
Ezzati M, Vander Hoorn S, Lawes CM, Leach R, James WP, Lopez AD, et al. Rethinking the “diseases of affluence” paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med. 2005;2(5):e133.
Hoque ME, Long KZ, Niessen LW, Al Mamun A. Rapid shift toward overweight from double burden of underweight and overweight among Bangladeshi women: a systematic review and pooled analysis. Nutr Rev. 2015;73(7):438–47.
McGuire S. Institute of Medicine. 2012. Front-of-package nutrition rating systems and symbols: promoting healthier choices. Washington, DC: The National Academies Press. Adv Nutr. 2012;3(3):332–3.
Stuckler D, Nestle M. Big food, food systems, and global health. PLoS Med. 2012;9(6):e1001242.
Wyness LA, Butriss JL, Stanner SA. Reducing the population’s sodium intake: the UK Food Standards Agency’s salt reduction programme. Public Health Nutr. 2012;15(2):254–61.
Moodie R, Stuckler D, Monteiro C, Sheron N, Neal B, Thamarangsi T, et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet. 2013;381(9867):670–9.
Acknowledgments
Steno Diabetes Center, where the authors are employed, receives part of its core funding from unrestricted grants from Novo Nordisk Foundation and Novo Nordisk, and is owned by Novo Nordisk. The authors also have private equity interest in Novo Nordisk.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Emilie H. Zobel, Tine W. Hansen, Peter Rossing and Bernt Johan von Scholten declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Economy and Environment
Rights and permissions
About this article
Cite this article
Zobel, E.H., Hansen, T.W., Rossing, P. et al. Global Changes in Food Supply and the Obesity Epidemic. Curr Obes Rep 5, 449–455 (2016). https://doi.org/10.1007/s13679-016-0233-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-016-0233-8