Abstract
Purpose of Review
Systemic photoprotection is an attractive concept; however, its use has been limited by a lack of robust evidence. We performed a review to evaluate the evidence for systemic photoprotection and skin cancer prevention in humans by vitamins C, D and E, carotenoids, nicotinamide, retinoids, polyphenols, Polypodium leucotomos extract, NSAIDs and afamelanotide.
Recent Findings
In a randomized controlled trial, compared with placebo, a 13% reduction in actinic keratoses and a 23% reduction in keratinocyte carcinoma were found with continued nicotinamide use over 12 months, although the result should be interpreted with caution. A synthetic melanotropin, Nle4-D-Phe7-a-MSH, showed promising results in photoprotection but was limited by its side effect profile.
Summary
Various photoprotective agents have shown promise in the reduction of the acute response to UV radiation, but there is insufficient evidence for their mainstream use presently. There is evidence for keratinocyte skin cancer prevention with the use of retinoids and nicotinamide in certain populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The deleterious effects of ultraviolet (UV) radiation on skin are mediated by a number of mechanisms that can ultimately lead to skin cancer. These include the production of reactive oxygen species leading to oxidative damage to tissues, UV-induced DNA mutations and immunosuppression [1,2,3,4,5,6].
Photoprotection aims to limit these effects and encompasses prevention of acute responses such as erythema and tanning, as well as chronic effects such as wrinkling, photoageing and skin cancer. Systemic photoprotection refers to compounds taken internally that offer protection against the effects of UV radiation [1, 2, 6] and represents an attractive concept owing to the potential ease of use compared with topical modalities. However, the use of systemic photoprotection has thus far been limited by a lack of robust evidence demonstrating protection. Much of the literature on this topic focuses on a reduction of the Minimal Erythema Dose (MED) as a marker of photoprotection, while other studies assessed cellular changes or clinical outcomes, i.e. incidence of skin cancer, to investigate this concept. Herein, we review the data on systemic protection in humans in vivo.
Vitamins
The main source of vitamins and minerals is through our diet, particularly fruits and vegetables [2, 6]. In addition, both individual vitamins and vitamin mixtures are sold over the counter.
Although the photoprotection gained through individual dietary components, such as particular vitamins, is significantly lower than that achieved by using topical sunscreen; some have been shown to possibly contribute to the skin’s defence against UV radiation [1].
Vitamins C and E
On their own, neither ascorbic acid (vitamin C) nor d-α-tocopherol (vitamin E) has demonstrated a photoprotective effect. However, several controlled studies show a statistically significant modest increase in median MED (range 16.5–80 mJ/cm2) when the combination is taken orally [7,8,9], and it is thought that the regeneration of vitamin E in the presence of ascorbic acid is responsible for this effect [7].
Vitamin D
Vitamin D is converted to its active form in the epidermis following exposure to UVB radiation [10]. Studies examining the photoprotective effect of vitamin D in humans are few, and evidence from randomized controlled trials (RCTs) are lacking.
In a double-blind, placebo-controlled intervention trial, 20 participants were administered a single high dose of cholecalciferol (200,000 international units) 1 h following experimental sunburn. This was found to mitigate local inflammatory responses, defined as diminished oedema and epidermal vesiculation, and to decrease expression of inflammatory mediators in the skin in a dose-dependent manner compared with placebo [11].
The Women’s Health Initiative, a prospective trial, assessed > 36,000 post-menopausal women over a 5-year period assigned to either calcium plus vitamin D or placebo. They found no difference in the incidence of keratinocyte cancer or melanoma between the study arms. In a subgroup analysis, women in the calcium/vitamin D group with a history of keratinocyte cancer had 57% fewer melanomas at the end of the trial period (HR, 0.43; 95% CI 0.21–0.90; P = 0.026); however, there were several limitations with the study. The trial objective was to assess the effect of supplementation on hip fracture and colon cancer, not skin cancer. In addition, the absolute numbers of melanoma cases overall were small in both arms, raising the possibility of a chance effect.
Epidemiologic studies have reported inconsistent results on the association between supplementation of various vitamins and skin cancer risk. Several meta-analyses of RCTs looking at the association, however, do not support the use of vitamins in skin cancer prevention [12, 13]. A meta-analysis of various vitamins and vitamin combinations found no association between supplementation and skin cancer risk overall, including in subgroup analyses by type of vitamin, type of skin cancer and population type [14].
Carotenoids
Carotenoids are pigments synthesized by plants; thus, the main source in the human diet is vegetables. The most common carotenoids are lutein, zeaxanthin and lycopene as well as provitamin A carotenoids α-carotene, β-carotene and β-cryptoxanthin [6]. They concentrate in skin in an unequal distribution across the body [1]. Carotenoids are thought to exert their main photoprotective role in the skin by acting as singlet oxygen ‘quenchers’, absorbing reactive oxygen species, thereby preventing their damaging effects on the skin. In addition, they are reported to have both anti-proliferative effects via the formation of retinoic acid and anti-inflammatory effects [1].
Beta-Carotene
Multiple studies on dietary and supplement forms of β-carotene have been conducted with scarce or conflicting evidence as to its photoprotective effect. Beginning in the 1970s, β-carotene was shown to improve photosensitivity in patients with erythropoietic protoporphyria [15, 16]. More recently, studies assessing its effect on photoprotection and skin cancer incidence have yielded varying results.
A modest reduction in UV-induced erythema, as measured by increase in MED, has been found in studies with relatively small numbers [5, 17]. The effect was only seen after at least 6 weeks of taking β-carotene supplements, and continuous treatment was required for it to be sustained [5]. Effective doses were generally > 10 mg/day. Importantly, concern has been raised over the risk of lung cancer with β-carotene supplementation in high-risk populations. Two large RCTs with doses of β-carotene 20-30 mg/day showed an increased risk of lung cancer among men at high risk of lung cancer at baseline taking this supplement. This risk reduced once the supplement was stopped [18, 19].
Similarly, the evidence for β-carotene does not as yet support supplementation in terms of skin cancer prevention [5]. An RCT in Nambour, Australia, in 1999 of > 1500 patients looked at keratinocyte cancer incidence over 4.5 years with interventions including β-carotene supplementation. No significant difference between the incidences of basal cell carcinoma (BCC) or cutaneous squamous cell carcinoma (SCC) was found between oral β-carotene and placebo groups [20]. Results from two other RCTs supported this finding [21, 22].
Lycopene
Lycopene is another carotenoid with high antioxidant activity found principally in tomatoes, some red fruits and vegetables [6]. Several small studies assessing the effect of dietary sources (e.g. tomato paste, tomato extract) show less pronounced UV-induced erythema, albeit with a small effect size [23, 24].
A case-control study involving 22 participants administered either tomato paste containing 16 mg lycopene along with a small dose of β-carotene and lutein or olive oil for 10 weeks. An increase in serum lycopene was reported in the treatment group, but no significant increase in skin lycopene levels was found. The lycopene group was found to have a 40% relative reduction in UVB-induced erythema of the dorsal hand (P = 0.02) [23].
Another study randomized 36 participants to one of three different lycopene supplements taken twice daily for 12 weeks. These were synthetic lycopene capsules (5.1 mg lycopene/capsule), tomato extract capsules (4.9 mg lycopene/capsule) or a lycopene drink (4.1 mg lycopene). A small but significant increase in skin lycopene levels was found in all groups at 12 weeks (P < 0.05) [24]. A 38% and 48% reduction in UVB-induced erythema was found in the tomato extract capsule and lycopene drink groups, respectively, at 12 weeks (P < 0.001) [24].
From both of these studies, it is difficult to ascertain the clinical significance of the reported reduction in erythema. Furthermore, there were a number of limitations with the studies including small sample sizes and lack of standardization of potential confounding factors such as diet and UV exposure.
Xanthophylls
Xanthophylls are oxygenated carotenoids. They include lutein, astaxanthin and zeaxanthin and are found in green leafy vegetables, legumes, seafood and eggs [25, 26]. While antioxidant activity has been attributed to their use [27], little evidence in humans exists currently. A double-blind, placebo-controlled study administered a daily paprika-xanthophyll preparation containing 9 mg total xanthophylls to 43 Japanese participants for 5 weeks. A significant increase in MED in the group treated with supplementation was demonstrated at 4 weeks (P < 0.05) [26].
While many of these studies may suggest a photoprotective role of carotenoids with regard to UV-induced erythema, the evidence is limited by relatively small numbers and heterogeneous methodology. Moreover, optimal dose and duration to achieve these effects remain unknown.
Nicotinamide
Nicotinamide is an amide form of vitamin B3 that is well tolerated with a favourable safety profile. It is readily available as a supplement and is ubiquitous in the human diet found in meat, nuts, legumes and vegetables. It is a precursor to NAD+, a cofactor in ATP production that is depleted by UV radiation. ATP is essential for cellular function and repair as well as the immune response following damage by UV radiation [6].
Phase II and III trials looking at the efficacy of nicotinamide in the prevention of skin cancer have shown positive results, although more robust studies are required to confirm the findings. A double-blind, placebo-controlled RCT including > 300 participants assigned oral nicotinamide 500 mg twice-daily or placebo for 12 months [28]. A 23% reduction in pooled keratinocyte carcinomas (mean 1.8 vs. 2.4 (P = 0.02) in the nicotinamide group was found, although the result should perhaps be interpreted with caution given the relatively wide confidence intervals (95% CI = 4–38). In addition, an estimated three to five fewer actinic keratoses (AK) from baseline were found in the intervention group, as well as a non-significant trend toward reduced incidence of BCC (mainly superficial) and a negligible reduction in SCC. The chemopreventive benefits were not evident once the nicotinamide was stopped, suggesting that continued use is necessary to maintain the effect [28]. A Bayesian analysis of the findings of this trial concluded that there was insufficient evidence to establish nicotinamide’s efficacy in skin cancer prevention [29].
Studies of nicotinamide in the organ transplant population have shown conflicting results.
A phase II RCT of 22 immunosuppressed renal transplant patients administered 500 mg nicotinamide or placebo twice daily over 6 months [30]. There was a non-significant trend toward fewer BCCs in the treatment group compared with the control group, but no difference in the rate of SCC was found between the study groups. There was a 16% non-significant reduction in actinic keratoses in the treatment group.
Conversely, a case-control study administered oral nicotinamide 250 mg three times daily or placebo to 38 organ transplant recipients over the same time period and reported a reduction in size of AK in 88% of the treatment group (P = 0.01), with complete remission in almost half of these [31]. An increase in size or development of new AK was observed in 91% of the controls with seven AK progressing to SCC [31].
For photoprotection, a placebo-controlled, randomized cross-over trial of 61 healthy volunteers found nicotinamide up to 1500 mg PO daily had no effect on UV-induced erythema. However, a significant reduction in UV-induced immunosuppression was reported in the nicotinamide arm, compared with placebo by measuring tuberculin purified protein derivative (Mantoux) results of UV irradiated and non-irradiated skin, before and after supplementation with nicotinamide [32].
Retinoids
Retinoids are vitamin A derivatives and are the most studied preventative agents for skin cancer [33]. The exact mechanism by which they exert their effects is unknown but is thought to be related to their modulatory effects on cell proliferation, differentiation and apoptosis. Acitretin, a synthetic second generation aromatic retinoid, is generally considered the first choice for skin cancer prevention and is the most studied for this purpose [33, 34].
The evidence for the use of retinoids for the prevention of keratinocyte cancer comes largely from the renal transplant population. A cross-over, placebo-controlled trial randomized 23 renal transplant patients to acitretin 25 mg daily for 12 months, titrated against patient tolerance. An estimated 42% increase in SCC during the non-treatment period was observed compared with the acitretin period; the effect was estimated to be significantly higher with the exclusion of one outlier. In addition, there was evidence of regression of actinic keratoses during the treatment period. There was insufficient evidence to show a benefit in BCC prevention [33].
A double-blind, placebo-controlled trial randomized 38 renal transplant recipients to 30 mg of acitretin per day for 6 months. There was a significant reduction in the number of patients with new keratinocytic skin cancers (χ2 = 6.27, P = 0.01) and in the cumulative number of new skin cancers (Mann-Whitney U test, P = 0.009) for acitretin compared with placebo. In addition, there was a reduction in keratotic lesions [35].
An open-label RCT looked at the preventative effect of two doses of acitretin on skin cancer in 26 renal transplant patients. Participants were treated with 0.4 mg/kg/day for 3 months, and then half the participants were reduced to half dose for a further 9 months, although many patients required a dose reduction owing to side effects, most commonly mucocutaneous effects such as cheilitis and excessive peeling of the skin. In contrast to other studies, while there was a rapid decrease in the number of actinic keratoses by nearly 50% in both arms, there was no significant difference in the number of malignant lesions developing in either group [36]. The exact number of tumours developing in the groups was not provided. The results of this study are limited by the lack of a placebo group.
The results of a prospective, randomized, double-blind, placebo-controlled trial assessing the effect of acitretin on keratinocyte skin cancer in 70 non-transplant patients were less promising. Participants had a history of skin cancer and were administered acitretin 25 mg or placebo for 5 days per week for 2 years. While there was a trend toward lower numbers of keratinocyte cancer in the acitretin arm during the study period, the result was not statistically significant [37].
While clinical trials are few, the evidence overall supports a positive effect of acitretin in skin cancer prevention. The effect is seen mainly in the prevention of SCC and actinic keratoses in renal transplant recipients with a history of skin cancer. The mechanism of this beneficial effect is unclear, as is the optimum long-term dose of acitretin for skin cancer prevention.
One of the major limiting factors across all the studies is the significant side effects that led to dose reduction or withdrawal in many participants. It is worth noting that no deterioration in renal or liver function was noted in any of the trials.
Dietary Botanicals
Polyphenols
Polyphenols are a broad group of plant products whose photoprotective properties are largely due to their antioxidant activity. They are ubiquitous in the human diet and are found in fruits, vegetables, nuts, seeds and red wine [2]. The main classes are flavonoids, stilbenes, lignans, hydroxybenzoic acid and hydroxycinnamic acids. The most well-known polyphenols include resveratrol, caffeic and ferulic acid as well as the catechins [6].
Of the polyphenols, flavonoids are reported to have the most significant antioxidant activity, although most of the data from experimental studies comes from green tea catechins. Flavonoids include flavanols, isoflavones and anthocyanidins and foods high in their content include onions, cacao, citrus fruits, berries, cherries, pomegranate juice and green tea extract [6]. Although small intervention studies have reported a reduction in UV-induced erythema with cacao extract containing high dose flavanol [38] and with an oral supplement containing citrus and rosemary extract (high in both polyphenols and diterpenes) [39], controlled trials do not support these results.
Green tea (Camellia sinensis) contains a mixture of catechins (in particular, epigallocatechin-3-gallate (EGCG)), which have antioxidant effects as well as immune-modulating effects [6].
Two randomized, double-blind, placebo-controlled trials each assigned 50 patients to a supplement of green tea catechins plus vitamin C 1080 mg/100 mg per day or placebo for 3 months. Both studies failed to show any statistically significant difference in MED or cellular markers of UV-induced damage between the groups [40, 41]. In addition, there are several limitations to the use of EGCG in a practical sense, as it has a short half-life, is poorly soluble and sensitive to oxidation [6].
Resveratrol is found in grape skin, seeds and wine. Although preclinical findings are encouraging, to our knowledge, there are no human intervention studies assessing its systemic photoprotective properties.
Polypodium leucotomos
Polypodium leucotomos extract (PLE) comes from a fern found in Central and South America and has been used in traditional medicine for years to treat inflammation. It is rich in polyphenols, particularly ferulic and caffeic acids; thus, its efficacy in skin disease is attributed mainly to its antioxidant effect [6]. It is available over the counter in many countries as a dietary supplement [42].
A small case-control study investigating the photoprotective effects of topical and oral PLE exposed 21 participants to ‘moderate’ daily natural UV radiation. MED and skin biopsy specimens were assessed. A single dose of 1080 mg of PLE resulted in a statistically significant increase in mean MED (34 to 98 mJ/cm2, P < 0.001). In addition, skin biopsies from patients who took PLE showed slight preservation of dendritic morphology compared with the control group; however, no quantitative difference in sunburn cells between the groups was noted. These apparent protective changes were more pronounced in participants who were photosensitized prior to UV exposure with oral 8-methoxypsoralen or 5-methoxypsoralen [3], thus not indicative of protection from solar UV.
In a prospective study, 22 participants with Fitzpatrick skin types I-III were administered 480 mg of PLE 1 to 2 h prior to radiation of half the back with artificial UVA, UVB radiation and visible light. The other half of the back was irradiated prior to PLE administration and thus acted as a control site. A statistically significant decrease in erythema as assessed by Investigator Global Assessment or colorimetry was found in 77% of participants following PLE administration (P < 0.05). Other participants exhibited no change or a decrease in MED following treatment.
A significant reduction in biomarkers associated with UV damage, such as keratinocyte apoptosis and cyclobutane pyrimidine dimers, was found in the treatment arm [43].
Similarly, a prospective study with nine healthy subjects administered 7.5 mg/kg of oral PLE also assessed MED and skin biopsy results. There was significantly less erythema in the PLE-treated group, although the effect was lost at 3 h post-administration of PLE. Skin biopsies taken 24–72 h after ingesting PLE demonstrated less epidermal damage, significantly reduced sunburn cells and cyclobutane pyrimidine dimer production, and a trend toward preservation of Langerhans cells [4].
Similar studies [44, 45] supported an increased MED following administration of oral PLE in most, but not all, participants.
Overall, studies examining the photoprotective effect of PLE have shown a protective effect against UV-induced erythema that appears to extend to UV damage at the cellular level. That being said, the protective effect, at least in terms of erythema, was of short duration. Larger randomized controlled studies with a focus on clinical outcomes are required to confirm a protective benefit.
NSAIDs
Non-steroidal anti-inflammatory drugs (NSAIDs) have been studied for their preventative effects on keratinocyte cancer owing to their inhibition of COX-2, a pro-inflammatory cytokine [46]. Clinical studies examining the effects of NSAIDs on the prevention of keratinocyte skin cancer have shown conflicting results.
A systematic review of the association between NSAIDs and BCC found a 10% risk reduction in BCC with any NSAID use in the pooled estimate, RR 0.90 (95% CI 0.84–0.97) [46]. The effect was modest and only seen in those deemed at high risk of BCC (defined in this study as a history of > 10 actinic keratosis or prior skin cancer). There was significant inter-study heterogeneity.
A meta-analysis found that a daily dose of aspirin was significantly associated with a reduced risk of skin cancer (OR 0.94, CI 0.90–0.99, P = 0.05) [47], although the effect size was small and the studies showed significant heterogeneity. Conversely, another meta-analysis found no chemo-preventative effect of NSAIDs on either SCC or BCC [48].
The preventative effect of 200 mg celecoxib twice daily was evaluated in a randomized double-blind, placebo-controlled trial in 240 high-risk patients [49]. High risk in this case was defined as individuals with a Fitzpatrick skin type of I, II or III plus 10–40 actinic keratoses and a previous diagnosis of either actinic keratosis or keratinocyte cancer. Celecoxib was continued for 9 months followed by a 2-month post-intervention follow-up period. There was no significant difference between the groups in terms of the stated primary outcome of new actinic keratoses. An exploratory analysis of the data, however, showed a significant reduction in the mean number of both BCC and SCC in the celecoxib group compared with placebo (RR 0.43; 95% CI 0.24–0.75, P = 0.03). The association was evident from 3 to 6 months after initiation of the intervention. The follow-up period was too short to allow for assessment of the effect of treatment cessation.
A case-control study looked at > 1000 patients with keratinocyte cancer. Information was collected on demographics, sun exposure, sun sensitivity and analgesic use (including NSAIDs), and the histology of the keratinocyte cancers was examined. A minimal reduction in the odds of BCC and a moderate reduction in the odds of SCC and actinic keratoses were seen with both NSAIDs overall and aspirin; however, the confidence intervals of these associations crossed 1, raising the possibility there may be no difference between the two groups. None of these results was significant at a P level < 0.05 [50].
When the cases were stratified by the presence of molecular alteration, however, statistically significant benefits were found. Aspirin use was associated with a moderate-high risk reduction of developing tumours with altered p53 or PTCH (P < 0.05), albeit with wide confidence intervals. Overall NSAID use was associated with a reduction in P53 mutated SCC detected by immunohistochemistry (OR = 0.32 (0.14–0.73), P < 0.05). This reduction was mirrored in TP53 mutation analysis but was not statistically significant [50].
A large cohort study assessed NSAID use in > 34,000 patients at high risk of skin cancer for the development of BCC and SCC over a median follow-up period of 3 years [51]. While there was a statistically significant benefit in terms of hazard ratio with non-aspirin NSAID use and BCC, the effect size was weak and reduced with analysis using multiply imputed data for completion of the data set. There was no statistically significant association between aspirin and BCC or between NSAID use and SCC.
Limitations included potential recall bias as assessment of exposure was self-reported and confounding. In particular, frequent NSAID users were more likely to have higher cumulative sun exposure. Mention was made of adjustment during statistical analysis; however, no further details were given [51].
Overall, the evidence for the protective effects of NSAIDs is conflicting. There are a small number of (mostly observational) studies with significant heterogeneity that show no or modest reduction in keratinocyte cancer, and there remains a lack of robust evidence for a significant effect. Moreover, a number of important side effects have been associated with NSAIDs including gastrointestinal bleeding, renal impairment and increase in cardiovascular risk that likely outweigh any potential clinical benefit in this situation [52].
Afamelanotide
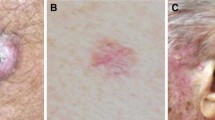
Afamelanotide (Nle4-D-Phe7-a-MSH) is a synthetic analogue of α-melanocyte stimulating hormone (MSH), a naturally occurring hormone that stimulates the production of eumelanin in the skin. Eumelanin is one of the skin’s natural defences against UV radiation, and abundant epidemiological data supports its protective role against UV-induced skin cancer [53]. Afamelanotide is currently approved in Europe and the USA for the prevention of phototoxicity in people with erythropoietic protoporphyria.
A randomized, double-blind placebo-controlled study of 79 participants was conducted to look at the safety, tolerability and photoprotective effect of Nle4-D-Phe7-a-MSH. The medication was administered subcutaneously over a 3-month period. The trial showed promising results with significantly increased melanin density in all treated participants. The largest increase was seen in those at highest risk of UV damage (those with lowest baseline skin melanin levels), who had an approximate increase of 61% in melanin from baseline over the treatment period. There was significantly reduced DNA damage and a decrease in histological evidence of UV damage after exposure to 3× the participant’s MED. One significant limiting factor is the side effect profile of the synthetic melanotropin, which includes nausea, vomiting, facial flushing and fatigue and was the main reason for withdrawal from this study in 20% of participants in the intervention arm [53].
Conclusion
The ease of taking an oral supplement or dietary component makes this an attractive option for photoprotection. While oral agents such as β-carotene and Polypodium leucotomos extract have shown promise in reduction of the acute response to UV radiation, there is insufficient evidence currently that this translates to convincing clinical benefit. Research assessing the mechanism of their effects and whether a reduction in erythema translates to a reduction in persistent UV damage and risk of malignancy would strengthen the notion of systemic photoprotection by these agents.
There is evidence for keratinocyte skin cancer prevention with the use of retinoids and nicotinamide. Larger studies to confirm the protective effects, particularly of nicotinamide, would be useful to support these findings.
Fundamentally, optimal sun protection involves a combination of shade-seeking, protective clothing, sunglasses and sunscreen use. While there may be an adjunctive role for oral agents in systemic photoprotection, the potential benefit of individual dietary components is much lower than that achieved by topical sunscreen use [5].
Evidence from larger, controlled studies assessing clinical outcomes in terms of prevention of immediate sun-induced changes and ultimately a decreased risk of skin cancer, as well as the optimal dose and duration of therapy, is needed before systemic photoprotection can be advocated in mainstream practice.
Change history
17 September 2020
The original version of this article did not include the results from articles showing a more favorable side effect profile with a controlled-release subcutaneous implant of afamelanotide.
References
Stahl W, Sies H. β-Carotene and other carotenoids in protection from sunlight. Am J Clin Nutr. 2012;96(5):1179S–84S.
Fernández-García E. Skin protection against UV light by dietary antioxidants. Food Funct. 2014;5(9):1994–2003.
González S, Pathak M, Cuevas J, Villarrubia V, Fitzpatrick T. Topical or oral administration with an extract of Polypodium leucotomos prevents acute sunburn and psoralen-induced phototoxic reactions as well as depletion of Langerhans cells in human skin. Photodermatol Photoimmunol Photomed. 1997;13(1–2):50–60.
Middelkamp-Hup MAPM, Parrado C, Goukassian D, Rius-Diaz F, Mihm MC, et al. Oral Polypodium leucotomos extract decreases ultraviolet-induced damage of human skin. J Am Acad Dermatol. 2004;51(6):910–8.
Stahl WSH. Photoprotection by dietary carotenoids: concept, mechanisms, evidence and future development. Mol Nutr Food Res. 2012;56(2):287–95.
Parrado CPN, Gilaberte Y, Juarranz A, Gonzalez S. Oral photoprotection: effective agents and potential candidates. Front Med. 2018;5:188.
Mireles-Rocha HGI, Huerta M, Trujilloherna B, Elizalde A, Cortes-Franco R. UVB photoprotection with antioxidants: effects of oral therapy with d-a-tocopherol and ascorbic acid on the minimal erythema dose. Acta Derm Venereol. 2002;82:21–4.
Eberlein-König BPM, Przybilla B. Protective effect against sunburn of combined systemic ascorbic acid (vitamin C) and d-a-tocopherol (vitamin E). J Am Acad Dermatol. 1998;38(1):45–8.
Fuchs JKH. Modulation of UV-light-induced skin inflammation by d-alpha-tocopherol and l-ascorbic acid: a clinical study using solar simulated radiation. Free Radic Biol Med. 1998;25(9):1006–12.
Mason RSRJ. Sunlight vitamin D and skin cancer. Anti Cancer Agents Med Chem. 2013;13(1):83–97.
Scott JF, Das LM, Ahsanuddin S, Qiu Y, Binko AM, Traylor ZP, et al. Oral vitamin D rapidly attenuates inflammation from sunburn: an interventional study. J Invest Dermatol. 2017;137(10):2078–86.
Chang YJ, Myung SK, Chung ST, Kim Y, Lee EH, Jeon YJ, et al. Effects of vitamin treatment or supplements with purported antioxidant properties on skin cancer prevention: a meta-analysis of randomized controlled trials. Dermatology. 2011;223(1):36–44.
Bardia A, Tleyjeh IM, Cerhan JR, Sood AK, Limburg PJ, Erwin PJ, et al. Efficacy of antioxidant supplementation in reducing primary cancer incidence and mortality: systematic review and meta-analysis. Mayo Clin Proc. 2008;83(1):23–34.
Chang YJMS, Chung ST, Kim Y, Lee EH, Jeon YJ, et al. Effects of vitamin treatment or supplements with purported antioxidant properties on skin cancer prevention: a meta-analysis of randomized controlled trials. Dermatology. 2011;223(1):36–44.
Balwani M, Desnick RJ. The porphyrias: advances in diagnosis and treatment. Blood. 2012;120(23):4496–504.
Mathews-Roth MM, Pathak MA, Parrish J, Fitzpatrick TB, Kass EH, Toda K, et al. A clinical trial of the effects of oral beta-carotene on the responses of human skin to solar radiation. J Invest Dermatol. 1972;59(4):349–53.
Carrascosa JM, Floriach N, Sala E, Aguilera J. Increase in minimal erythemal dose following oral administration of an antioxidant complex based on a mix of carotenoids: double-blind, placebo-controlled trial. Photodermatol Photoimmunol Photomed. 2017;33(5):284–6.
Omenn GSGG, Thornquist MD, Balmes J, Cullen MR, Glass A, et al. Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med. 1996;334(18):1150–5.
Heinonen OPHJ, Albanes D, Haapakoski J, Palmgren J, Pietinen P. The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N Engl J Med. 1994;330(15):1029–35.
Green AWG, Nèale R, Hart V, Leslie D, Parsons P, et al. Daily sunscreen application and betacarotene supplementation in prevention of basal-cell and squamous-cell carcinomas of the skin: a randomised controlled trial. Lancet. 1999;354(9180):723–9.
Frieling UMSD, Kupper TS, Muntwyler J, Hennekens CH. A randomized, 12-year primary-prevention trial of beta carotene supplementation for nonmelanoma skin cancer in the physician’s health study. Arch Dermatol. 2000;2:179–84.
Greenberg ERBJ, Stukel TA, Stevens MM, Mandel JS, Spencer SK, et al. A clinical trial of beta carotene to prevent basal-cell and squamous-cell cancers of the skin. The Skin Cancer Prevention Study Group. N Engl J Med. 1991;323(12):789–95.
Stahl WHU, Wiseman S, Eichler O, Sies H, Tronnier H. Dietary tomato paste protects against ultraviolet light–induced erythema in humans. J Nutr. 2001;131(5):1449–51.
Aust O, Stahl W, Sies H, Tronnier H, Heinrich U. Supplementation with tomato-based products increases lycopene, phytofluene, and phytoene levels in human serum and protects against UV-light-induced erythema. Int J Vitam Nutr Res. 2005;75(1):54–60.
Juturu V, Bowman JP, Deshpande J. Overall skin tone and skin-lightening-improving effects with oral supplementation of lutein and zeaxanthin isomers: a double-blind, placebo-controlled clinical trial. Clin Cosmet Investig Dermatol. 2016;9:325–32.
Nishino A, Sugimoto K, Sambe H, Ichihara T, Takaha T, Kuriki T. Effects of dietary paprika xanthophylls on ultraviolet light-induced skin damage: a double-blind placebo-controlled study. J Oleo Sci. 2018;67(7):863–9.
Roberts RL, Green J, Lewis B. Lutein and zeaxanthin in eye and skin health. Clin Dermatol. 2009;27(2):195–201.
Chen AC, Martin AJ, Choy B, Fernandez-Penas P, Dalziell RA, McKenzie CA, et al. A phase 3 randomized trial of nicotinamide for skin-cancer chemoprevention. N Engl J Med. 2015;373(17):1618–26.
Gilmore SJ. Nicotinamide and skin cancer chemoprevention: the jury is still out. Australas J Dermatol. 2018;59(1):6–9.
Chen AC, Martin AJ, Dalziell RA, McKenzie CA, Lowe PM, Eris JM, et al. A phase II randomized controlled trial of nicotinamide for skin cancer chemoprevention in renal transplant recipients. Br J Dermatol. 2016;175(5):1073–5.
Drago F, Ciccarese G, Cogorno L, Calvi C, Marsano LA, Parodi A. Prevention of non-melanoma skin cancers with nicotinamide in transplant recipients: a case-control study. Eur J Dermatol. 2017;27(4):382–5.
Yiasemides E, Sivapirabu G, Halliday GM, Park J, Damian DL. Oral nicotinamide protects against ultraviolet radiation-induced immunosuppression in humans. Carcinogenesis. 2009;30(1):101–5.
George RWW, Russ G, Bannister K, Mathew T. Acitretin for chemoprevention of non-melanoma skin cancers in renal transplant recipients. Australas J Dermatol. 2002;43:269–73.
Chen AC, Damian DL, Halliday GM. Oral and systemic photoprotection. Photodermatol Photoimmunol Photomed. 2014;30(2–3):102–11.
Bavinck JNTL, Van Der Woude FJ, Tegzess AM, Hermans J, ter Schegget J, et al. Prevention of skin cancer and reduction of keratotic skin lesions during acitretin therapy in renal transplant recipients: a double-blind. Placebo-Controlled Study J Clin Oncol. 1995;13(8):1933–8.
De Sévaux RGSJ, De Jong EM, Van de Kerkhof PC, Hoitsma AJ. Acitretin treatment of premalignant and malignant skin disorders in renal transplant recipients: clinical effects of a randomized trial comparing two doses of acitretin. J Am Acad Dermatol. 2003;49(3):407–12.
Kadakia KC, Barton DL, Loprinzi CL, Sloan JA, Otley CC, Diekmann BB, et al. Randomized controlled trial of acitretin versus placebo in patients at high-risk for basal cell or squamous cell carcinoma of the skin (North Central Cancer Treatment Group Study 969251). Cancer. 2012;118(8):2128–37.
Heinrich UNK, Tronnier H, Sies H, Stahl W. Long-term ingestion of high flavanol cocoa provides photoprotection against UV-induced erythema and improves skin condition in women. J Nutr. 2006;136(6):1565–9.
Perez-Sanchez A, Barrajon-Catalan E, Caturla N, Castillo J, Benavente-Garcia O, Alcaraz M, et al. Protective effects of citrus and rosemary extracts on UV-induced damage in skin cell model and human volunteers. J Photochem Photobiol B. 2014;136:12–8.
Farrar MD, Nicolaou A, Clarke KA, Mason S, Massey KA, Dew TP, et al. A randomized controlled trial of green tea catechins in protection against ultraviolet radiation-induced cutaneous inflammation. Am J Clin Nutr. 2015;102(3):608–15.
Farrar MD, Huq R, Mason S, Nicolaou A, Clarke KA, Dew TP, et al. Oral green tea catechins do not provide photoprotection from direct DNA damage induced by higher dose solar simulated radiation: a randomized controlled trial. J Am Acad Dermatol. 2018;78(2):414–6.
Lim HW A-MM, Stengel F. Current challenges in photoprotection. J Am Acad Dermatol. 2017;76(3S1):S91-S9.
Kohli I, Shafi R, Isedeh P, Griffith JL, Al-Jamal MS, Silpa-Archa N, et al. The impact of oral Polypodium leucotomos extract on ultraviolet B response: a human clinical study. J Am Acad Dermatol. 2017;77(1):33–41 e1.
Aguilera PCC, Puig-Butille JA, Badenas C, Lecha M, Gonzalez S, et al. Benefits of oral Polypodium Leucotomos extract in MM high-risk patients. J Eur Acad Dermatol Venereol. 2013;27(9):1095–100.
Nestor MBB, Swenson N. Safety and efficacy of oral Polypodium leucotomos extract in healthy adult subjects. J Clin Aesthet Dermatol. 2015;8(2):19–23.
Muranushi COC, Green AC, Pandeya N. Can oral nonsteroidal antiinflammatory drugs play a role in the prevention of basal cell carcinoma? A systematic review and metaanalysis. J Am Acad Dermatol. 2016;74(1):108–19.
Zhu Y, Cheng Y, Luo RC, Li AM. Aspirin for the primary prevention of skin cancer: a meta-analysis. Oncol Lett. 2015;9(3):1073–80.
Zhang BLX, Ye L, Wang Y. No chemopreventive effect of nonsteroidal anti-inflammatory drugs on nonmelanoma skin cancer: evidence from meta-analysis. PLoS One. 2014;9(5):e96887.
Elmets CA, Viner JL, Pentland AP, Cantrell W, Lin HY, Bailey H, et al. Chemoprevention of nonmelanoma skin cancer with celecoxib: a randomized, double-blind, placebo-controlled trial. J Natl Cancer Inst. 2010;102(24):1835–44.
Torti DCCB, Storm CA, Fortuny J, Perry AE, Zens MS, et al. Analgesic and nonsteroidal anti-inflammatory use in relation to nonmelanoma skin cancer: a population-based case-control study. J Am Acad Dermatol. 2011;65(2):304–12.
Pandeya N, Olsen CM, Thompson BS, Dusingize JC, Neale RE, Green AC, et al. Aspirin and nonsteroidal anti-inflammatory drug use and keratinocyte cancers: a large population-based cohort study of skin cancer in Australia. Br J Dermatol. 2019;181(4):749–60.
Szeto CC, Sugano K, Wang JG, Fujimoto K, Whittle S, Modi GK, et al. Non-steroidal anti-inflammatory drug (NSAID) therapy in patients with hypertension, cardiovascular, renal or gastrointestinal comorbidities: joint APAGE/APLAR/APSDE/APSH/APSN/PoA recommendations. Gut. 2020;69:617–29.
Barnetson RS, Ooi TK, Zhuang L, Halliday GM, Reid CM, Walker PC, et al. [Nle4-D-Phe7]-alpha-melanocyte-stimulating hormone significantly increased pigmentation and decreased UV damage in fair-skinned Caucasian volunteers. J Invest Dermatol. 2006;126(8):1869–78.
Acknowledgements
Jennifer Taylor is supported by the Krembil Foundation, Canada.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Photodermatology
Rights and permissions
About this article
Cite this article
Taylor, J.H., Rosen, C.F. Systemic Photoprotection. Curr Derm Rep 9, 181–188 (2020). https://doi.org/10.1007/s13671-020-00306-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13671-020-00306-1