Abstract
Purpose of Review
Previous literature reviews summarized the associations between individual foods or food groups and lung cancer risk, but the relationship between dietary patterns and lung cancer risk has received less attention. We conducted a systematic review and meta-analyses of observational studies on the associations between dietary patterns and lung cancer risk.
Recent Findings
PubMed, Embase, and Web of Science were systematically searched from inception to February 2023. Random-effects models were used to pool relative risks (RR) on associations with at least two studies. Twelve studies reported on data-driven dietary patterns, and 17 studies reported on a priori dietary patterns. A prudent dietary pattern (high in vegetables, fruit, fish, and white meat) tended to be associated with a lower risk of lung cancer (RR = 0.81, 95% confidence interval [CI] = 0.66–1.01, n = 5). In contrast, Western dietary patterns, characterized by higher intakes of refined grains and red and processed meat, were significantly positively associated with lung cancer (RR = 1.32, 95% CI = 1.08–1.60, n = 6). Healthy dietary scores were consistently associated with a lower risk of lung cancer (Healthy Eating Index [HEI]: RR = 0.87, 95% CI = 0.80–0.95, n = 4; Alternate HEI: RR = 0.88, 95% CI = 0.81–0.95, n = 4; Dietary Approaches to Stop Hypertension: RR = 0.87, 95% CI = 0.77–0.98, n = 4; Mediterranean diet: RR = 0.87, 95% CI = 0.81–0.93, n = 10) while the dietary inflammatory index was associated with a higher risk of lung cancer (RR = 1.14, 95% CI = 1.07–1.22, n = 6).
Summary
Our systematic review indicates dietary patterns characterized by a higher intake of vegetables and fruits, a lower intake of animal products, and anti-inflammation may be associated with a reduced risk of lung cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer was the most common cancer among men and the third most common cancer among women (following breast and colorectal cancers) globally in 2020 [1]. In the USA, lung cancer incidence has been decreasing dramatically from 64.4 (1992) to 41.6 (2019) per 100,000 in the last three decades [2]. However, it is still the second leading incident cancer among both men and women and the leading cause of cancer death in the USA. [3]. The most well-established risk factor for lung cancer is tobacco smoking, which is attributed to 80–90% of lung cancer deaths among US men and women [4]. However, over 15% of men and over 50% of women with lung cancer are nonsmokers [5]. Therefore, identification of other lifestyle factors besides smoking that are associated with lung cancer is critical for informing prevention efforts.
The World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) summarized the evidence on dietary factors and lung cancer risk, concluding with limited suggestive evidence that red meat and processed meat might increase the risk of lung cancer and higher intake of fruits/vegetables might decrease the risk of lung cancer [6]. However, individual foods or food groups can be highly correlated or have components which interact biologically which cannot be captured by studying them in isolation.
Rather than focusing on a single food or nutrient, dietary pattern analysis captures the quality of the overall diet [7••, 8, 9]. Generally, two types of dietary patterns are commonly used in nutritional studies: a priori (literature-, guideline-, or index-based methods) and data-driven methods (also called a posteriori). A priori dietary patterns use scoring methods based on existing dietary guidelines or literature and include the commonly studied Healthy Eating Index (HEI) [10], alternate HEI (AHEI), Dietary Approaches to Stop Hypertension (DASH) [11], Mediterranean diet [12], and dietary inflammatory index (DII) [13]. Data-driven dietary patterns are derived from statistical analyses such as factor analysis and cluster analysis based on dietary intake data from a specific study. Other methods combine a priori knowledge and the data itself using reduced rank regression, such as used in the creation of the empirical dietary inflammation pattern (EDIP) [14].
To our knowledge, only two systematic reviews have focused on associations between dietary patterns and lung cancer risk. One review, published in 2016, involved only eight observational studies [15]. Another recently published review summarized the associations between the Mediterranean diet and lung cancer with eight cohort and one case–control studies [16•]. Several additional prospective cohort studies have investigated the association between a priori dietary patterns and lung cancer risk [17,18,19, 20•, 21]. Therefore, we aimed to conduct a systematic review and meta-analysis to summarize the available evidence on associations between dietary patterns and lung cancer risk.
Methods
The current review was conducted and reported in accordance with standard criteria (Preferred Reporting Items for Systematic Reviews and Meta-Analyses, PRISMA) [22]. The protocol was registered in PROSPERO (CRD42021242842).
Search Strategy
We searched PubMed, Embase, and Web of Science up to February 2, 2023. Generally, the search terms included the following components: cohort or case–control study, lung cancer, and dietary patterns. Details about the search terms could be found in the Supplemental Table 1. We only included studies written in English and did not restrict on year of publication. The references of the retrieved studies also were searched for any additional studies.
Study Selection and Inclusion Criteria
The study selection was performed with the following steps. First, authors (LZ and BK) scanned the title and abstract to obtain the relevant literature for further full-text review. Second, the authors downloaded the identified literature and read the full text carefully to ascertain eligibility based on our inclusion criteria. The inclusion criteria included as follows: (1) participants who were free of lung cancer at baseline for cohort studies and controls without lung diseases for case–control studies; and (2) the exposure of interest was any dietary patterns or scores including Western diet, prudent diet, HEI, AHEI, DASH, Mediterranean diet, DII, or other dietary patterns derived from data-driven methods including factor analysis or cluster analysis; and (3) the outcome of interest was the incidence of lung cancer; and (4) the study design was cohort design or case–control design; and (5) the study reported adjusted relative risk (RR) including odds ratio (OR) or hazard ratio (HR) and 95% confidence intervals (CI).
The exclusion criteria included: (1) studies that focused on children or adolescents (age ≤ 18 years); or (2) the exposures were food items, or food groups, or glycemic index/load; or (3) the outcome was lung cancer death or mortality, or recurrence or metastasis of lung cancer; or (4) the study design was experiments, ecological studies, or meta-analysis; or (5) studies lacked information on RR or OR or HR and their 95% CIs. An exclusion list of full-text review was provided in Supplemental Table 2.
Data Extraction and Quality Assessment
We used an a priori abstract table to obtain the following information: last name of the first author, publication year, study location or cohort name, study design, study duration or follow-up period, total number of cases, cohort size or number of controls, study population, median age, sex, exposure assessment method, deriving methods of dietary patterns and scoring details, outcome and outcome assessment method, contrast groups, main results for adjusted models, confounders included in analyses, and results stratified by sex and smoking status. We used the Newcastle–Ottawa scale (NOS) to assess the study quality of the included studies based on selection bias, comparability, and outcome assessment [23]. In questions for comparability of the NOS, the most important confounders are age and smoking. The second most important confounders are energy intake and family history of lung cancer. We considered studies with 0–3, 4–6, and 7–9 points to represent low-, medium-, and high-quality studies, respectively (Supplemental Table 3).
Statistical Analyses
All data were shown as abstracted and displayed according to the study design and exposure types (data-driven and a priori dietary patterns). We conducted meta-analyses to combine the available evidence on associations with at least two studies using random-effects models [24] and in sensitivity analyses combined results for prospective cohort studies only. We evaluated heterogeneity by estimating the variance between studies using Cochran’s Q test and the I-squared (I2) statistic [25]. We did not assess small study effects and perform meta-regression because of the limited number of studies for each association. We used command “metan” in STATA (version 15, StataCorp) to perform the meta-analyses. A 2-sided P value < 0.05 was considered statistically significant.
Results
Study Characteristics
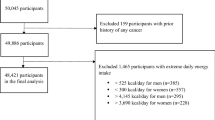
After removing the duplicates, we identified 573 records by searching PubMed, Embase, and Web of Science (Fig. 1). Another two papers were added from the manual reference review [26]. We identified 47 articles for further full-text review, of which 19 articles were excluded (Supplemental Table 2). Finally, we included 28 studies in the current review [17,18,19, 20•, 21, 26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48]. Characteristics of each of the studies, including covariates adjusted for in multivariable models, are shown in Table 1. There were 17 cohort studies [17, 19, 20•, 21, 26, 28, 34,35,36,37, 40, 42,43,44,45, 47, 48], nine case–control studies [27, 30,31,32,33, 38, 39, 41, 46], and two case-cohort studies [17, 28]. The publication years ranged from 2003 to 2022. Two case-cohort studies were performed in the Netherlands [17, 28]. Only five case–control studies [30,31,32, 39, 46] and five cohort studies [19, 20•, 36, 42, 48] were conducted outside the USA or European countries. The median follow-up years of prospective studies was 12 years, ranging from 4.3 to 20.3 years. Most of these studies (26 out of 28) used food frequency questionnaires (FFQs) to collect the diet information.
We obtained 12 studies on data-driven dietary patterns and 17 studies on a priori dietary patterns (one study reported two types of dietary patterns). Eleven studies focused on factor analysis [28, 30,31,32,33,34, 38, 39, 41, 47, 48], and one focused on cluster analysis [27]. Four studies reported on HEI [20•, 21, 35, 45], four on AHEI [20•, 21, 35, 45], and four on DASH [20•, 21, 35, 45]. Nine studies evaluated the associations between the Mediterranean diet and lung cancer [17, 18, 20•, 21, 26, 35,36,37, 45]. Six articles assessed the associations between DII and lung cancer [18, 19, 21, 36, 37, 46]. We classified over 80% of studies (23/28) as high-quality studies with the NOS ≥ 7 (Supplemental Table 3).
Dietary Patterns and Lung Cancer Among Case–Control Studies
Associations between dietary patterns and lung cancer among case–control studies were summarized in Fig. 2. Three of four studies indicated an inverse association between prudent diet and lung cancer [31, 32, 41] and two of them were statistically significant [32, 41]. Three studies focusing on a vegetable dietary pattern found significant inverse associations with lung cancer (all P values for trend < 0.01) [32, 38, 39]. Two studies showed that high meat or high quality protein-based dietary patterns were significantly associated with a higher risk of lung cancer [30, 39]. Similarly, four of five studies showed the Western diet was associated with higher lung cancer risk [31, 32, 38, 41]. One study reported associations between a priori dietary patterns and lung cancer using a case–control design (Fig. 2) [41]. The study suggested conformity to the Polish-adapted Mediterranean diet was associated with a lower risk of lung cancer [41]. One case–control study showed positive association between DII and lung cancer risk [46].
Associations between dietary patterns and lung cancer risk among case–control studies. CI confidence intervals, F female, M male, Q4 vs Q1 Quartile 4 vs. Quartile 1, Q5 vs Q1 Quintile 5 vs. Quintile 1, RR relative risk, T3 vs T1 Tertile 3 vs. Tertile 1.a Tex-Mex pattern is characterized by its heavy use of legumes, spices, and shredded cheese. b Principal component 1: High in vegetables and low in animal products. Principal component 2: High in other plant food except for vegetables. c Except for these two studies, all others are data-driven dietary patterns
Dietary Patterns and Lung Cancer Among Prospective Studies
Figure 3 showed associations between data-driven dietary patterns and lung cancer using a prospective design. Prudent dietary patterns (two studies) [47, 48] and dietary patterns high in vegetables (two studies) [28] and fiber (two studies) [34, 48] showed significant inverse associations with lung cancer. In contrast, dietary patterns high in animal products [34], fructose [48], and meat [28], as well as a Western diet [47, 48] were associated with a higher risk of lung cancer.
Associations between a priori dietary patterns and lung cancer risk among cohort studies were shown in Fig. 4. Four studies reported associations for HEI [20•, 21, 35, 45] and four reported on AHEI [20•, 21, 35, 45]. Except for the Women’s Health Initiative (WHI) [45], the other three studies indicated inverse associations of HEI with lung cancer risk with RRs for the highest category compared with the lowest category ranging from 0.79 to 0.86 [20•, 21, 35]. The findings from the WHI observational study with 86,090 postmenopausal women suggested null associations between HEI or AHEI and lung cancer risk [45]. A lower risk of lung cancer was found among higher DASH scores in three out of four studies [20•, 21, 35, 45]. Mediterranean diet was associated with a reduced lung cancer risk in six out of nine studies [17, 18, 20•, 26, 35,36,37, 45]. Among five studies on DII [18, 19, 21, 36, 37], all were positively associated with lung cancer risk but only two of them were statistically significant [18, 21]. Three other studies reported that conformity to the Recommended Food Score [29] or a plant-based diet [40] or diabetes risk reduction diet [43] were related to a lower risk of lung cancer.
Associations between a priori dietary patterns and lung cancer risk among prospective studies. AHEI Alternate Healthy Eating Index-2010, aMED alternate Mediterranean diet, CI confidence intervals, DASH Dietary Approaches to Stop Hypertension, DII Dietary inflammatory index, FSAm-NPS the Nutrient Profiling System of the British Food Standards Agency (modified version), F female, HEI-2010 Healthy Eating Index-2010, HEI-2015 Healthy Eating Index-2015, M male, mMED modified alternate Mediterranean diet, MDS adapted Mediterranean diet score, Q4 vs Q1 Quartile 4 vs. Quartile 1, Q5 vs Q1 Quintile 5 vs. Quintile 1, RR relative risk, T3 vs T1 Tertile 3 vs. Tertile 1
Dietary Patterns and Lung Cancer Stratified by Sex or Smoking Status
Among studies that evaluated results stratified by sex, similar results for males and females were reported (Supplemental Table 4). Considering the impact of smoking on associations between dietary patterns and lung cancer, we further summarized the evidence stratified by smoking status (Supplemental Table 5). For data-driven dietary patterns, the proportion of studies reporting statistically significant findings (approximately 43–55%) were similar between smoking subgroups, with 11 out of 20 studies for former smokers, eight out of 16 studies among current smokers, and six out of 14 studies for never smokers. For the a priori dietary patterns, there were more statistically significant associations observed among former smokers (nine out of 17 studies) and current smokers (seven of 16 studies) than never smokers (four out of 18 studies).
Meta-Analyses on Associations of Dietary Patterns with Lung Cancer
Table 2 shows the pooled results between dietary patterns and lung cancer risk when there were at least two studies reporting associations. Fruits/vegetables patterns (RR = 0.56, 95% CI = 0.36–0.87) were inversely associated with lung cancer risk, while high meat/protein patterns (RR = 1.58, 95% CI = 1.10–2.26) and Western dietary patterns (RR = 1.32, 95% CI = 1.08–1.60) were positively associated with lung cancer. Higher dietary quality measured by HEI (RR = 0.87, 95% CI = 0.80–0.95), AHEI (RR = 0.88, 95% CI = 0.81–0.95), DASH (RR = 0.87, 95% CI = 0.77–0.98), and Mediterranean Diet Score (MDS; RR = 0.87, 95% CI = 0.81–0.93) were significantly associated with lower risk of lung cancer, while higher DII (i.e., more pro-inflammatory diet) was associated with a higher risk of lung cancer (RR = 1.14, 95% CI = 1.07–1.22). The forest plots were shown in Supplemental Fig. 1. We found a high heterogeneity between studies for fruit/vegetables patterns (I2 = 91, P < 0.001) and high meat/protein patterns (I2 = 75, P = 0.007). After we excluded the He et al. study and De Stefani et al. 2008 study, the I2 decreased, and results were similar with our main estimates (fruit/vegetables patterns: RR = 0.71, 95% CI = 0.62–0.82, I2 = 0, P for Q = 0.46; high meat/protein patterns: RR = 1.31, 95% CI = 1.09–1.58, I2 = 0, P for Q = 0.83). These observed associations were similar when we restricted the analyses to prospective studies (Supplemental Table 6).
We further pooled studies stratified by sex (Supplemental Table 7) or smoking status (Supplemental Table 8). Consistent with our summary results, the associations between dietary patterns and lung cancer did not differ much across sex. However, significant associations were more likely to be found among former and current smokers than among never smokers.
Discussion
Summary of Results
Based on this systematic review of the evidence on associations between dietary patterns and lung cancer risk, we found that dietary patterns characterized by high intake of fruits or vegetables and low intake of animal-based foods were associated with a lower risk of lung cancer. Conformity of diet to a healthy dietary pattern including HEI, AHEI, DASH, and Mediterranean diet was associated with a lower risk of lung cancer, while a more pro-inflammatory diet (i.e., higher DII) was associated with a higher risk of lung cancer in the majority of studies reported to date.
Explanations and Comparison
Our review indicates dietary patterns with higher fruits and vegetables and lower animal products are associated with a lower risk of lung cancer, which is generally consistent with previous evidence on these individual food groups [49]. Recently, an umbrella review summarized the associations between fruit and vegetable intake and health outcomes [50]. The study found higher fruit intake or vegetable intake is associated with a lower risk of lung cancer. Another umbrella review that focused on the associations between red meat and cancer risk found higher intake of red meat was associated with a higher risk of lung cancer [51]. A prudent diet and HEI, AHEI, DASH, and Mediterranean diet scores are all characterized by higher intakes of fruits and vegetables, and lower intakes of red/processed meat, and the consistent lower risk of lung cancer with these dietary patterns in our review supports the previous reviews of the individual food groups.
Our findings on the Mediterranean diet and lung cancer corroborate the conclusions of a review published in 2022 which included nine studies (eight cohort and one case–control studies) [16•]. Our review included an additional cohort study published in 2021 [20•]. Besides Mediterranean diet, in the current systematic review, conformity to a healthy diet as assessed by the HEI, AHEI, and DASH is consistently associated with a lower risk of lung cancer. These dietary patterns give higher scores for plant-based foods, such as whole grains, vegetables, fruits, and nuts [52] and emphasize moderation of red and processed meat intake. The DASH diet also emphasizes reduced intake of sugar-sweetened beverages and sodium. Chronic inflammation plays a critical role in carcinogenesis [53]. Recently, an umbrella review suggested compelling evidence on the link between DII and respiratory (including lung) cancers [54]. A meta-analyses of multiple cancer types reported a positive association between DII and lung cancer in three cohorts (pooled RR = 1.30, 95% CI = 1.13–1.50) [55]. In our systematic review, six studies indicate positive associations between DII and lung cancer risk with three of them statistically significant (pooled RR = 1.14, 95% CI = 1.07–1.22).
We found that among studies that reported on a priori dietary patterns, more statistically significant associations were observed among former and current smokers than never smokers, which was somewhat consistent with a previous systematic review on the Mediterranean diet and lung cancer that identified inverse associations among former smokers but not among never smokers or current smokers [16•]. However, among previous studies, only one study reported a statistically significant interaction between HEI and smoking on lung cancer (Pinteraction = 0.03) [20•]. For data-driven dietary patterns, results were similar between smoking subgroups. Thus, more studies are needed that stratify results by smoking status to determine whether associations may differ by tobacco exposure. Studies evaluating the effect modification role of sex on the associations between dietary patterns and lung cancer reported similar results between males and females without significant interactions [19, 21, 47].
The inverse associations of diets high in plant-based foods and low in red meat or animal products with lung cancer risk are biologically plausible. A diet high in fruits, vegetables, and whole grains is higher in bioactive compounds like carotenoids, flavonoids, and polyphenols, which display anticarcinogenic properties in animal studies [56]. In addition, dietary components like fiber may affect inflammation which is a hallmark of cancer and is implicated in the etiology of lung cancer [57, 58]. Potential biological mechanisms have been proposed to support the positive association between diets high in red or processed meat and lung cancer risk. Multiple carcinogens like heme iron, heterocyclic amines, and N-nitroso compounds were found in red and processed meat [59]. Epidemiological studies also showed heme iron from red or processed meat was positively associated with a higher risk of lung cancer [60].
Limitations
Several limitations of the review and of the individual studies should be noted. First, due to the observational study designs of the included studies, we cannot rule out residual confounding of healthy lifestyles. Previous studies reported cigarette smoking is significantly associated with unhealthy diet [61,62,63]. Even though most of the included studies have adjusted for important confounders, such as smoking, physical activity, body mass index, and family history of cancer, the observed association could still be biased by unmeasured confounders or residual confounding. Second, we observed an inverse association between some dietary patterns and lung cancer with a limited number of studies, such as the pro plant-based dietary score which calculates the relative contribution of plant foods versus animal products in the diet and the Recommended Food Score. We cannot draw definitive conclusions based on only one or two studies, and more research is needed among different populations. Third, we did not have enough information to further explore the association between dietary patterns and subtypes of lung cancer. Lung cancer is a complex disease including small cell lung cancer (accounts for 15–17%) and non-small cell lung cancer (> 85%) like adenocarcinoma, squamous cell carcinoma, and large cell carcinoma [64]. Those histologic subtypes may have different etiology. Only five studies in our review reported results stratified by histologic subtypes [19, 39, 43, 45, 47], and none of them observed significant differences in these subgroup analyses, which may be due to the limited numbers in each subgroup. More studies with larger sample sizes are needed to examine whether associations differ by histologic subtype. Finally, we did not have enough information to address the role of race and ethnicity in the associations between dietary patterns and lung cancer risk. Among those studies in our systematic review, none of case–control studies reported information on race and ethnicity and only six of 17 cohorts further controlled for race and ethnicity in multivariable models [20•, 21, 35, 43, 45, 47]. Of these six studies, four studies [21, 43, 45, 47] examined the interaction between dietary patterns and race and ethnicity with only one study reporting a significant interaction between Western dietary pattern and ethnicity [47]. Further research is needed to evaluate the role of race and ethnicity in associations between diet and lung cancer risk.
Conclusion
Our systematic review indicated healthy dietary patterns characterized by high fruits and vegetables and low in red meat and animal products are associated with a lower risk of lung cancer.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- AHEI:
-
Alternate Healthy Eating Index
- CI:
-
Confidence intervals
- DASH:
-
Dietary Approaches to Stop Hypertension
- DII:
-
Dietary Inflammatory Index
- EDIP:
-
Empirical Dietary Inflammation Pattern
- HEI:
-
Healthy Eating Index
- NOS:
-
Newcastle-Ottawa scale
- RR:
-
Relative risk
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Howlader N NA, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z,. SEER cancer statistics review, 1975–2018. site. Available at https://seer.cancer.gov/csr/1975_2018/.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30. https://doi.org/10.3322/caac.21590.
U.S. Department of Health and Human Services. The health consequences of smoking: a report of the surgeon general. In.; 2004.
Parkin DM, Bray F, Ferlay J, et al. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55(2):74–108. https://doi.org/10.3322/canjclin.55.2.74.
World Cancer Research Fund International. Diet, nutrition, physical activity and cancer: a global perspective: a summary of the Third Expert Report. In.: World Cancer Research Fund International; 2018.
•• Steck SE, Murphy EA. Dietary patterns and cancer risk. Nat Rev Cancer. 2020;20(2):125–38. https://doi.org/10.1038/s41568-019-0227-4. The review summarized the evidence on associations between dietary patterns and cancer risk and pointed out directions for future research.
Krebs-Smith SM, Subar AF, Reedy J. Examining dietary patterns in relation to chronic disease: matching measures and methods to questions of interest. Circulation. 2015;132(9):790–3. https://doi.org/10.1161/CIRCULATIONAHA.115.018010.
Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13(1):3–9. https://doi.org/10.1097/00041433-200202000-00002.
Guenther PM, Casavale KO, Reedy J, et al. Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet. 2013;113(4):569–80. https://doi.org/10.1016/j.jand.2012.12.016.
Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10. https://doi.org/10.1056/NEJM200101043440101
Trichopoulou A, Costacou T, Bamia C, et al. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599–608. https://doi.org/10.1056/NEJMoa025039.
Shivappa N, Steck SE, Hurley TG, et al. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17(8):1689–96. https://doi.org/10.1017/S1368980013002115.
Tabung FK, Smith-Warner SA, Chavarro JE, et al. Development and validation of an empirical dietary inflammatory index. J Nutr. 2016;146(8):1560–70. https://doi.org/10.3945/jn.115.228718.
Sun Y, Li Z, Li J, et al. A healthy dietary pattern reduces lung cancer risk: a systematic review and meta-analysis. Nutrients. 2016;8(3):134. https://doi.org/10.3390/nu8030134.
• Bahrami A, Khalesi S, Makiabadi E, et al. Adherence to the Mediterranean diet and the risk of lung cancer: a systematic review and dose-response meta-analysis of observational studies. Nutr Rev. 2022;80(5):1118–28. https://doi.org/10.1093/nutrit/nuab117. The study reviewed the evidence on Mediterranean diet and risk of lung cancer, and results were consistent with our main findings.
Schulpen M, van den Brandt PA. Adherence to the Mediterranean diet and risk of lung cancer in the Netherlands Cohort Study. Br J Nutr. 2018;119(6):674–84. https://doi.org/10.1017/S0007114517003737.
Boden S, Myte R, Wennberg M, et al. The inflammatory potential of diet in determining cancer risk; a prospective investigation of two dietary pattern scores. PLoS One. 2019;14(4):e0214551. https://doi.org/10.1371/journal.pone.0214551
Shivappa N, Wang R, Hebert JR, et al. Association between inflammatory potential of diet and risk of lung cancer among smokers in a prospective study in Singapore. Eur J Nutr. 2019;58(7):2755–66. https://doi.org/10.1007/s00394-018-1825-8.
• Wang Q, Hashemian M, Sepanlou SG, et al. Dietary quality using four dietary indices and lung cancer risk: the Golestan Cohort Study (GCS). Cancer Causes Control. 2021;32(5):493–503. https://doi.org/10.1007/s10552-021-01400-w. This is the latest study examaining the association between different dietary quality indices and lung cancer risk using a prospective cohort design.
Park SY, Boushey CJ, Shvetsov YB, et al. Diet quality and risk of lung cancer in the multiethnic cohort study. Nutrients. 2021;13(5):1614. https://doi.org/10.3390/nu13051614.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. https://doi.org/10.1016/j.ijsu.2010.02.007.
Wells GA, Shea B, O’Connell Da, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. In.: Oxford; 2000.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88. https://doi.org/10.1016/0197-2456(86)90046-2.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. https://doi.org/10.1002/sim.1186.
Gnagnarella P, Maisonneuve P, Bellomi M, et al. Red meat, Mediterranean diet and lung cancer risk among heavy smokers in the COSMOS screening study. Ann Oncol. 2013;24(10):2606–11. https://doi.org/10.1093/annonc/mdt302.
Tsai YY, McGlynn KA, Hu Y, et al. Genetic susceptibility and dietary patterns in lung cancer. Lung Cancer. 2003;41(3):269–81. https://doi.org/10.1016/s0169-5002(03)00238-1.
Balder HF, Goldbohm RA, van den Brandt PA. Dietary patterns associated with male lung cancer risk in the Netherlands Cohort Study. Cancer Epidemiol Biomarkers Prev. 2005;14(2):483–90. https://doi.org/10.1158/1055-9965.EPI-04-0353.
Mai V, Kant AK, Flood A, et al. Diet quality and subsequent cancer incidence and mortality in a prospective cohort of women. Int J Epidemiol. 2005;34(1):54–60. https://doi.org/10.1093/ije/dyh388.
De Stefani E, Boffetta P, Ronco AL, et al. Nutrient patterns and risk of lung cancer: a factor analysis in Uruguayan men. Lung Cancer. 2008;61(3):283–91. https://doi.org/10.1016/j.lungcan.2008.01.004.
De Stefani E, Deneo-Pellegrini H, Boffetta P, et al. Dietary patterns and risk of cancer: a factor analysis in Uruguay. Int J Cancer. 2009;124(6):1391–7. https://doi.org/10.1002/ijc.24035.
De Stefani E, Ronco AL, Deneo-Pellegrini H, et al. Dietary patterns and risk of adenocarcinoma of the lung in males: a factor analysis in Uruguay. Nutr Cancer. 2011;63(5):699–706. https://doi.org/10.1080/01635581.2011.563033.
Gorlova OY, Weng SF, Hernandez L, et al. Dietary patterns affect lung cancer risk in never smokers. Nutr Cancer. 2011;63(6):842–9. https://doi.org/10.1080/01635581.2011.589958.
Gnagnarella P, Maisonneuve P, Bellomi M, et al. Nutrient intake and nutrient patterns and risk of lung cancer among heavy smokers: results from the COSMOS screening study with annual low-dose CT. Eur J Epidemiol. 2013;28(6):503–11. https://doi.org/10.1007/s10654-013-9803-1.
Anic GM, Park Y, Subar AF, et al. Index-based dietary patterns and risk of lung cancer in the NIH-AARP diet and health study. Eur J Clin Nutr. 2016;70(1):123–9. https://doi.org/10.1038/ejcn.2015.122.
Hodge AM, Bassett JK, Shivappa N, et al. Dietary inflammatory index, Mediterranean diet score, and lung cancer: a prospective study. Cancer Causes Control. 2016;27(7):907–17. https://doi.org/10.1007/s10552-016-0770-1.
Maisonneuve P, Shivappa N, Hebert JR, et al. Dietary inflammatory index and risk of lung cancer and other respiratory conditions among heavy smokers in the COSMOS screening study. Eur J Nutr. 2016;55(3):1069–79. https://doi.org/10.1007/s00394-015-0920-3.
Tu H, Heymach JV, Wen CP, et al. Different dietary patterns and reduction of lung cancer risk: a large case-control study in the U.S. Sci Rep. 2016;6:26760. https://doi.org/10.1038/srep26760
He F, Xiao RD, Lin T, et al. Dietary patterns, BCMO1 polymorphisms, and primary lung cancer risk in a Han Chinese population: a case-control study in Southeast China. BMC Cancer. 2018;18(1):445. https://doi.org/10.1186/s12885-018-4361-2.
Kane-Diallo A, Srour B, Sellem L, et al. Association between a pro plant-based dietary score and cancer risk in the prospective NutriNet-sante cohort. Int J Cancer. 2018;143(9):2168–76. https://doi.org/10.1002/ijc.31593.
Hawrysz I, Wadolowska L, Slowinska MA, et al. Adherence to prudent and mediterranean dietary patterns is inversely associated with lung cancer in moderate but not heavy male polish smokers: a case-control study. Nutrients. 2020;12(12). https://doi.org/10.3390/nu12123788
Cai H, Sobue T, Kitamura T, et al. Low-carbohydrate diet and risk of cancer incidence: the Japan Public Health Center-based prospective study. Cancer Sci. 2022;113(2):744–55. https://doi.org/10.1111/cas.15215.
Zhang Y, Zhong G, Zhu M, et al. Association between diabetes risk reduction diet and lung cancer risk in 98,159 participants: results from a prospective study. Front Oncol. 2022;12:855101. https://doi.org/10.3389/fonc.2022.855101
Deschasaux M, Huybrechts I, Murphy N, et al. Nutritional quality of food as represented by the FSAm-NPS nutrient profiling system underlying the Nutri-Score label and cancer risk in Europe: Results from the EPIC prospective cohort study. PLoS Med. 2018;15(9):e1002651. https://doi.org/10.1371/journal.pmed.1002651
Myneni AA, Giovino GA, Millen AE, et al. Indices of diet quality and risk of lung cancer in the women’s health initiative observational study. J Nutr. 2021;151(6):1618–27. https://doi.org/10.1093/jn/nxab033.
Sadeghi A, Parastouei K, Seifi S, et al. Inflammatory potential of diet and odds of lung cancer: a case-control study. Nutr Cancer. 2022;74(8):2859–67. https://doi.org/10.1080/01635581.2022.2036770.
Wei X, Zhu C, Ji M, et al. Diet and risk of incident lung cancer: a large prospective cohort study in UK biobank. Am J Clin Nutr. 2021;114(6):2043–51. https://doi.org/10.1093/ajcn/nqab298.
Willemsen RF, McNeil J, Heer E, et al. Dietary patterns with combined and site-specific cancer incidence in Alberta’s Tomorrow Project cohort. Eur J Clin Nutr. 2022;76(3):360–72. https://doi.org/10.1038/s41430-021-00958-7.
Vieira AR, Abar L, Vingeliene S, et al. Fruits, vegetables and lung cancer risk: a systematic review and meta-analysis. Ann Oncol. 2016;27(1):81–96. https://doi.org/10.1093/annonc/mdv381.
Angelino D, Godos J, Ghelfi F, et al. Fruit and vegetable consumption and health outcomes: an umbrella review of observational studies. Int J Food Sci Nutr. 2019;70(6):652–67. https://doi.org/10.1080/09637486.2019.1571021.
Huang Y, Cao D, Chen Z, et al. Red and processed meat consumption and cancer outcomes: umbrella review. Food Chem. 2021;356:129697. https://doi.org/10.1016/j.foodchem.2021.129697
Miller V, Webb P, Micha R, et al. Defining diet quality: a synthesis of dietary quality metrics and their validity for the double burden of malnutrition. Lancet Planet Health. 2020;4(8):e352–70. https://doi.org/10.1016/s2542-5196(20)30162-5.
Greten FR, Grivennikov SI. Inflammation and cancer: triggers, mechanisms, and consequences. Immunity. 2019;51(1):27–41. https://doi.org/10.1016/j.immuni.2019.06.025.
Marx W, Veronese N, Kelly JT, et al. The dietary inflammatory index and human health: an umbrella review of meta-analyses of observational studies. Adv Nutr. 2021;12(5):1681–90. https://doi.org/10.1093/advances/nmab037.
Fowler ME, Akinyemiju TF. Meta-analysis of the association between dietary inflammatory index (DII) and cancer outcomes. Int J Cancer. 2017;141(11):2215–27. https://doi.org/10.1002/ijc.30922.
Subramaniam S, Selvaduray KR, Radhakrishnan AK. Bioactive compounds: natural defense against cancer? Biomolecules. 2019;9(12):758. https://doi.org/10.3390/biom9120758.
Yang JJ, Yu D, Xiang YB, et al. Association of dietary fiber and yogurt consumption with lung cancer risk: a pooled analysis. JAMA Oncol. 2020;6(2):e194107. https://doi.org/10.1001/jamaoncol.2019.4107
Gomes M, Teixeira AL, Coelho A, et al. The role of inflammation in lung cancer. Adv Exp Med Biol. 2014;816:1–23. https://doi.org/10.1007/978-3-0348-0837-8_1.
Abid Z, Cross AJ, Sinha R. Meat, dairy, and cancer. Am J Clin Nutr. 2014;100(Suppl 1):386S-393S. https://doi.org/10.3945/ajcn.113.071597.
Ward HA, Whitman J, Muller DC, et al. Haem iron intake and risk of lung cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Eur J Clin Nutr. 2019;73(8):1122–32. https://doi.org/10.1038/s41430-018-0271-2.
Heydari G, Heidari F, Yousefifard M, et al. Smoking and diet in healthy adults: a cross-sectional study in tehran, iran, 2010. Iran J Public Health. 2014;43(4):485–91.
Alkerwi A, Baydarlioglu B, Sauvageot N, et al. Smoking status is inversely associated with overall diet quality: Findings from the ORISCAV-LUX study. Clin Nutr. 2017;36(5):1275–82. https://doi.org/10.1016/j.clnu.2016.08.013.
MacLean RR, Cowan A, Vernarelli JA. More to gain: dietary energy density is related to smoking status in US adults. BMC Public Health. 2018;18(1):365. https://doi.org/10.1186/s12889-018-5248-5.
Polanski J, Chabowski M, Jankowska-Polanska B, et al. Histological subtype of lung cancer affects acceptance of illness, severity of pain, and quality of life. J Pain Res. 2018;11:727–33. https://doi.org/10.2147/JPR.S155121.
Acknowledgements
We acknowledge authors of the original studies that included in our systematic review and meta-analyses.
Author information
Authors and Affiliations
Contributions
Study conception and design: LZ and SS; study protocol: LZ and SS; literature research and data extraction: LZ and BK; data analyses: LZ and BK; results interpretation: LZ, BK, JZ, and SS; draft: LZ; review and critical revision: LZ, BK, JZ, and SS; read and approved the version of the manuscript being submitted: LZ, BK, JZ, and SS.
Corresponding author
Ethics declarations
Conflict of Interest
All authors have no conflict of interest to declare.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, L., Kase, B., Zheng, J. et al. Dietary Patterns and Risk of Lung Cancer: A Systematic Review and Meta-Analyses of Observational Studies. Curr Nutr Rep 12, 338–357 (2023). https://doi.org/10.1007/s13668-023-00469-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-023-00469-w