Abstract
To investigate the effects of miR-98 on TGF-β1-induced cardiac fibrosis in human cardiac fibroblasts (HCFs), and to establish the mechanism underlying these effects, HCFs were transfected with miR-98 inhibitor or mimic, and then treated with or without TGF-β1. The level of miR-98 was determined by qRT-PCR in TGF-β1-induced HCFs. Cell differentiation and collagen accumulation of HCFs were detected by qRT-PCR and Western blot assays, respectively. The mRNA and protein expressions of TGFBR1 were determined by qRT-PCR and Western blotting. In this study, the outcomes showed that TGF-β1 could dramatically decrease the level of miR-98 in a time- and concentration-dependent manner. Upregulation of miR-98 dramatically improved TGF-β1-induced increases in cell differentiation and collagen accumulation of HCFs. Moreover, bioinformatics analysis predicted that the TGFBR1 was a potential target gene of miR-98. Luciferase reporter assay demonstrated that miR-98 could directly target TGFBR1. Inhibition of TGFBR1 had the similar effect as miR-98 overexpression. Downregulation of TGFBR1 in HCFs transfected with miR-98 inhibitor partially reversed the protective effect of miR-98 overexpression on TGF-β1-induced cardiac fibrosis in HCFs. Upregulation of miR-98 ameliorates TGF-β1-induced differentiation and collagen accumulation of HCFs by downregulation of TGFBR1. These results provide further evidence for protective effect of miR-98 overexpression on TGF-β1-induced cardiac fibrosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac fibrosis (CF) represents a fundamental constituent of many cardiac dysfunctions such as ischaemic, dilated and hypertrophic cardiomyopathies, heart failure and myocardial infarction [1, 2]. Moreover, cardiac fibrosis can also be a protopathic disease that is independent of preexisting cardiomyocyte injury [3,4,5,6]. Due to increasing cardiac stiffness, impaired cardiomyocyte contractility and disrupted electrical coupling, cardiac fibrosis has been considered as a major cause of death worldwide [7]. Until now, however, there is no effective strategy for the diagnosis and treatment of cardiac fibrosis. Therefore, it is urgent to find out novel therapeutics for cardiac fibrosis.
MicroRNAs (miRNAs) are endogenous and small (19–25 nucleotide) single-stranded RNAs that repress target gene expressions by inhibition of translation or degradation of mRNA of its target genes [8,9,10]. As important regulators of cardiac biology, miRNAs can regulate the functions of cardiomyocyte such as apoptosis, proliferation, hypertrophy, fibrosis and metabolism [11,12,13]. Aberrant miRNAs have already been related to multiple cardiovascular diseases including cardiac fibrosis [5, 14]. It has been reported that miR-21, miR-503, miR-34a and miR-125b can promote cardiac fibrosis [1, 15,16,17], while miR-let-7i, miR-9, miR-29a and miR-133a attenuate the fibrotic response of heart [18,19,20,21]. These studies indicate that miRNAs are powerful regulators of cardiac fibrosis. A previous study had reported that miR-98 was closely related to myocardial infarction [22], but its precise mechanism remains unclear. In this study, we aim to investigate the precise mechanism and role of miR-98 in TGF-β1-induced cardiac fibrosis.
Cardiac fibroblasts (CFs) are major type of cells responsible for cardiac fibrosis [23]. The proliferation, migration and activation of cardiac fibroblasts play critical roles in the genesis of cardiac fibrosis [6, 23,24,25]. Activated cardiac fibroblasts are featured with myofibroblast differentiation and increased synthesis of protein, including collagen I and III, the predominant extracellular matrix proteins [23]. Recently, more and more studies have demonstrated that transforming growth factor-β1 (TGF-β1) mediates cardiac fibrosis via miRNA-dependent mechanism. In this paper, upregulation of miR-98 had the protective effect on TGF-β1-induced differentiation and collagen accumulation of HCFs. Moreover, we found that transforming growth factor-beta receptor type I (TGFBR1) was the direct target of miR-98 in HCFs. Upregulation of TGFBR1 had the similar effect as downregulation of miR-98. Downregulation of TGFBR1 in HCFs partially reversed the protective effect of miR-98 overexpression on TGF-β1-induced cardiac fibrosis in HCFs. Therefore, our outcomes showed critical roles for miR-98 in the pathogenesis of cardiac fibrosis and suggested its possible application in treatment for TGF-β1-induced cardiac fibrosis.
Materials and methods
Cell culture
Human cardiac fibroblasts (HCFs) were purchased from ScienCell (#6300, USA), and cultured in Fibroblast Medium-2 (#2331) containing 5% fetal bovine serum (#0025), 1% penicillin/streptomycin (#0503), and 1% fibroblast growth supplement-2 (#2382) at 37 °C in 5% CO2 on 0.1% gelatin-coated culture flasks. Passage 3–5 HCFs were used for experiments.
Transient transfection
The miR-98 inhibitor, the miR-98 mimic, miR-negative control of inhibitor (anti-miR-NC), miR-negative control of mimic (miR-NC), siRNA for TGFBR1 (si-TGFBR1), siRNA-negative control (si-NC), pcDNA3.1-TGFBR1 and pcDNA3.1 vector were synthesized and purified by RiboBio (Guangzhou, China). MiR-98 inhibitor (100 nM), mimic (50 nM), anti-miR-NC (100 nM), miR-NC (50 nM), si-NC (100 nM) and si-TGFBR1 (100 nM) were transfected into HCFs using Lipofectamine 3000 reagent (Invitrogen, USA) according to the manufacturer’s protocols.
Construction of plasmids
The 3′-UTR sequences of TGFBR1 gene, containing the putative miR-98 binding site, was amplified by PCR and cloned into the pGL3-control vector (Promega), which was named wild-type 3′-UTR (WT 3′-UTR). Point mutations in the putative miR-98-binding seed regions were carried out using the Quickchange Site-Directed Mutagenesis kit (SBS Genetech, Beijing, China) following the manufacturer’s instruction. The resultant product served as the mutated 3′-UTR (MUT 3′-UTR). Both the wild-type and mutant insert fragments sequences were confirmed by DNA sequencing.
RNA extraction and quantitative reverse transcription polymerase chain reaction (qRT-PCR)
Total RNA of HCFs was extracted by Trizol reagent (Invitrogen, USA) for analyzing miRNA and mRNA levels according to the manufacturer’s protocols. For quantification of miR-98, the TaqMan MicroRNA Reverse Transcription Kit and TaqMan miRNA assay (Applied Biosystems, USA) were used to perform reverse transcription and PCR according to the manufacturer’s instructions. U6 was used as the internal control. The gene expressions of TGFBR1, α-SMA, Collagen I and III were detected using the SYBR Green PCR kits (Qiagen, USA). GAPDH served as an internal control. The following primers were used: TGFBR1 forward, 5′-GTAGCTCTGATGAGTGCAATGAC-3′, reverse, 5′-CAGATATGGCAACTCCCAGTG-3′; α-SMA forward, 5′-CTATGAGGGCTATGCCTTGCC-3′, reverse, 5′-GCTCAGCAGTAGTAACGAAGGA-3′; Collagen I forward, 5′-ACGCATGAGCCGAAGCTAAC-3′, reverse, 5′-AGGGACCCTTAGGCCATTGT-3′; Collagen III forward, 5′-ATAGACCTCAAGGCCCCAAG-3′, reverse, 5′-CCACCCATTCCTCCGACT-3′; GAPDH forward, 5′-ACAACTTTGGTATCGTGGAAGG-3′, reverse, 5′-GCCATCACGCCACAGTTTC-3′.
Western blot analysis
HCFs were lysed using protein lysis buffer with protease inhibitor cocktail. The protein concentration of cell lysates was quantified by BCA Kit, and 50 ng of protein was separated by 10% SDS-PAGE and then transferred onto a PVDF membrane (Millipore, USA). The membranes were blocked in 5% non-fat dry milk diluted with TBST at RT for 1 h and probed overnight at 4 °C with primary antibody as follows: anti-TGFBR1 antibody and anti-α-SMA antibody (Abcam, USA). After that the membranes were wash by TBST and incubated with a goat anti-rabbit or anti-mouse IgG conjugated to horseradish peroxidase (Abcam, USA) for 1 h at RT. Incubation with monoclonal mouse β-actin antibody (1:1000 dilution; CST, USA) was performed as the loading control. The proteins were visualized using ECL Western blotting detection reagents (Millipore, USA). The densitometry of the bands was quantified using the Image J 1.38X software (USA).
Dual-luciferase reporter assay
HCFs were seeded in 6-well plates (2 × 105/well) and incubated overnight before transfection. Then, pGL3-TGFBR1-3′ UTR wild-type or mutant reporter plasmid, miR-98 inhibitor and anti-miR-NC, or miR-98 mimic and miR-NC, and pRL-TK Renilla luciferase reporter (Promega, USA) were cotransfected into cells using Lipofectamine 2000 (Invitrogen). After that luciferase activities were quantified using the Dual-Luciferase reporter system (Promega, USA) following the manufacturer’s protocols, and firefly luciferase activities were normalized to Renilla luciferase activities.
Statistical analysis
Experiments were repeated at least three times. Values are expressed as mean ± standard error of the mean (SEM). Data were evaluated for statistical significance using one-way analysis of variance (ANOVA). P < 0.05 was considered to indicate a statistically significant difference. All statistical analyses were performed using GraphPad Prism 5.0 (GraphPad Software, Inc., USA).
Results
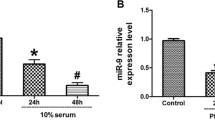
The level of miR-98 in TGF-β1-induced HCFs
To study the level of miR-98 in TGF-β1-induced HCFs, HCFs were treated with TGF-β1 at 10 ng/ml for 0, 6, 12, 24 or 48 h, after which the level of miR-98 was detected. Compared with untreated controls, the outcomes showed that TGF-β1 could dramatically decrease the level of miR-98 in a time-dependent manner (Fig. 1a). Next, HCFs were treated with TGF-β1 at 0, 2.5, 5, 10 and 20 ng/ml for 24 h. As shown in Fig. 1b, the level of miR-98 was evidently reduced by TGF-β1 in HCFs in a concentration-dependent manner. According to the above results, we used 10 ng/ml TGF-β1 to treat HCFs for 24 h in the following experiments.
The level of miR-98 in TGF-β1-induced HCFs. a HCFs were starved in medium containing 0.1% FBS for 24 h, followed by treatment with 10 ng/ml TGF-β1 for 0, 6, 12, 24 or 48 h. Level of miR-98 was analyzed by qRT-PCR. b HCFs were starved in medium containing 0.1% FBS for 24 h, followed by treatment with 0, 2.5, 5, 10 and 20 ng/ml TGF-β1 for 24 h. Level of miR-98 was analyzed by qRT-PCR. The data shown are mean ± SEM (n = 4). *P < 0.05, **P < 0.01, ***P < 0.001 vs. control
Effect of miR-98 on TGF-β1-induced myofibroblasts differentiation of HCFs
To investigate the function of miR-98 in the differentiation of HCFs into myofibroblasts in vitro, we treated HCFs with TGF-β1 (10 ng/ml) for 24 h after transfection with miR-98 mimic or inhibitor. The mRNA and protein levels of α-SMA, a myofibroblast marker, in HCFs were significantly increased by TGF-β1 stimulation as compared with control group (Fig. 2). Upregulation of miR-98 evidently inhibited the increase in TGF-β1-induced α-SMA expression at mRNA and protein levels (Fig. 2a). On the contrary, miR-98 downregulation could promote TGF-β1-stimulated expressions of α-SMA (Fig. 2b). These findings indicated that miR-98 overexpression protected HCFs from TGF-β1-induced differentiation.
Effect of miR-98 on TGF-β1-induced differentiation in HCFs. HCFs were transfected with miR-98 inhibitor or mimic, and then treated with or without TGF-β1 (10 ng/ml) for 24 h. a, b The mRNA and protein levels of α-SMA were determined by qRT-PCR and Western blot, respectively. The data shown are mean ± SEM (n = 4). **P < 0.01, ***P < 0.001 vs. control; ## P < 0.01, ### P < 0.001 vs. vehicle + TGF-β1
Effect of miR-98 on TGF-β1-induced collagen synthesis of HCFs
To demonstrate the effect of miR-98 in collagen synthesis, HCFs transfected with miR-98 mimic were exposed to TGF-β1 for 24 h, and mRNA levels of Collagen I and III were analyzed by qRT-PCR analysis. As expected, mRNA levels of Collagen I and III were significantly decreased in HCFs transfected with miR-98 mimic when compared with TGF-β1-treated HCFs (Fig. 3a). However, miR-98 inhibitor specifically increased TGF-β1-induced collagen synthesis (Fig. 3b), further confirming the effect of miR-98 in collagen synthesis.
Effect of miR-98 on TGF-β1-induced collagen deposition in HCFs. HCFs were transfected with miR-98 inhibitor or mimic, and then treated with or without TGF-β1 (10 ng/ml) for 24 h. The mRNA levels of Collagen I and III were determined by qRT-PCR. The data shown are mean ± SEM (n = 4). **P < 0.01, vs. control; # P < 0.05, ## P < 0.01, ### P < 0.001 vs. vehicle + TGF-β1
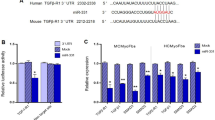
MiR-98 can directly target TGFBR1 in HCFs
The online database (TargetScan 6.2) predicted that TGFBR1 was a binding target of miR-98, we performed qRT-PCR to detect the expression of TGFBR1 on mRNA level in TGF-β1-induced HCFs transfected with miR-98 inhibitor or mimic. We found that mRNA level of TGFBR1 was remarkably decreased after upregulation of miR-98 (Fig. 4a), but was evidently increased after downregulation of miR-98 compared with TGF-β1-treated HCFs (Fig. 4a). To further demonstrate whether TGFBR1 was a direct target of miR-98, TGFBR1 3′-UTR was cloned into a luciferase reporter vector and the putative miR-98 binding site in the TGFBR1 3′-UTR was mutated (Fig. 4b). The effect of miR-98 was determined using luciferase reporter assay. Our results indicated that upregulation or downregulation of miR-98 significantly inhibited or promoted the luciferase activity of pGL3-TGFBR1 3′-UTR WT (Fig. 4c). Mutation of the miR-98-binding site in the TGFBR1 3′-UTR abolished the effect of miR-98, which suggested that TGFBR1 was directly and negatively regulated by miR-98.
TGFBR1 was a direct target of miR-98. HCFs were transfected with miR-98 inhibitor or mimic, and then treated with or without TGF-β1 (10 ng/ml) for 24 h. a The mRNA level of TGFBR1 was determined by qRT-PCR in HCFs. TGFBR1 expression was normalized to GAPDH. b Schematic representation of TGFBR1 3′ UTRs showing putative miRNA target site. c The analysis of the relative luciferase activities of TGFBR1-WT, TGFBR1-MUT in HCFs. All data are presented as mean ± SEM (n = 4). **P < 0.01 vs. control; # P < 0.05, ## P < 0.01 vs. vehicle + TGF-β1 or anti-miR-NC or miR-NC
Downregulation of TGFBR1 had similar effects with miR-98 overexpression
To explore the function of TGFBR1, HCFs were transfected with si-TGFBR1. Western blot analysis showed that the expression of TGFBR1 at protein level was significantly decreased after 24 h in HCFs transfected with si-TGFBR1 (Fig. 5a). The qRT-PCR assay revealed that TGFBR1’s downregulation dramatically decreased differentiation and collagen production of HCFs compared to TGF-β1-only groups (Fig. 5c, d). These results indicated that overexpression of miR-98 downregulated the expression of TGFBR1, thus protecting HCFs from TGF-β1-induced cardiac fibrosis.
The effects of TGFBR1 knockdown on TGF-β1-induced cell differentiation and collagen accumulation in HCFs. HCFs were transfected with si-TGFBR1 or si-NC, and then treated with or without TGF-β1 (10 ng/ml) for 24 h. a The protein expression of TGFBR1 was determined by Western blot. β-Actin was detected as a loading control. b The mRNA level of α-SMA was determined by qRT-PCR. c The mRNA levels of Collagen I and III were determined by qRT-PCR. All data are presented as mean ± SEM (n = 4). **P < 0.01, ***P < 0.001, # P < 0.05, ## P < 0.01 vs. control or TGF-β1 + si-NC
Inhibition of TGFBR1 is essential for protective effect of miR-98 on TGF-β1-induced cardiac fibrosis in HCFs
Next, to determine whether miR-98 overexpression protected HCFs from TGF-β1-induced cardiac fibrosis in a TGFBR1-dependent manner, we cotransfected HCFs with miR-98 mimic and pcDNA-TGFBR1. We found that the expression of TGFBR1 was significantly increased after transfection with miR-98 mimic and pcDNA-TGFBR1 compared with miR-98 mimic and pcDNA3.1 in HCFs (Fig. 6a). Analysis by qRT-PCT assay indicated that upregulating TGFBR1 expression could reverse the protective effect of miR-98 overexpression on TGF-β1-induced cardiac fibrosis in HCFs (Fig. 6b, c). From all above results, we clearly demonstrated that upregulation of miR-98 improved TGF-β1-induced increases in cell differentiation and collagen synthesis of HCFs by downregulation of TGFBR1, and that inhibition of TGFBR1 was essential for the protective effect of miR-98 overexpression TGF-β1-induced cardiac fibrosis in HCFs.
TGFBR1 was involved in the effects of miR-98 on TGF-β1-induced cell proliferation, differentiation and collagen accumulation in HCFs. HCFs were transfected with either miR-98 mimic with pcDNA-TGFBR1 or pcDNA3.1, and then treated with or without TGF-β1 (10 ng/ml) for 24 h. a The protein expression of TGFBR1 was determined by Western blot. β-Actin was detected as a loading control. b The mRNA level of α-SMA was determined by qRT-PCR. c The mRNA levels of Collagen I and III were determined by qRT-PCR. All data are presented as mean ± SEM (n = 4). **P < 0.01, ***P < 0.001 vs. TGF-β1 + miR-98 mimic + pcDNA3.1 or control; ## P < 0.01, ### P < 0.001 vs. vehicle + TGF-β1; & P < 0.05, && P < 0.01 vs. TGF-β1 + miR-98 mimic
Discussion
Cardiac fibrosis plays an important role in the development of other cardiovascular diseases such as heart failure [26, 27]. One of the main factors that influence cardiac fibrosis is excessive deposition of ECM. Cardiac mesenchymal cells including CFs mainly synthesized collagen that is a major ECM component [28]. Therefore, it is important to inhibit cardiac fibrosis by suppression of CFs differentiation and collagen production. In the present study, we studied the effects of miR-98 on differentiation and collagen production of TGF-β1-treated HCFs. The promoted effect on differentiation and collagen production of HCFs induced by TGF-β1 was abolished by upregulation of miR-98, suggesting the protective function of miR-98 overexpression in TGF-β1-induced cardiac fibrosis.
The differentiation of CFs to myofibroblasts that is strongly enhanced in the myocardium of failing hearts is one of the key events in cardiac fibrosis [29]. Cardiac myofibroblasts that mainly produce excessive extracellular collagen in cardiac fibrosis are absent from normal myocardium [30, 31]. The formation of cardiac myofibroblasts is characterized by high expression levels of α-SMA [32, 33]. Our findings showed that miR-98 overexpression could inhibit the TGF-β1-induced differentiation of HCFs by significantly downregulating the expression of α-SMA in TGF-β1-induced HCFs. Furthermore, the ECM mainly consists of many collagens such as types I and III, which form fibrils and provide most of the connective material and other structures in the myocardium [34]. In this study, we found that miR-98 overexpression inhibited TGF-β1-induced synthesis of collagen I and III in HCFs. Taken together, our findings indicated that miR-98 upregulation reversed TGF-β1-induced differentiation and collagen production of HCFs, resulting in protecting from TGF-β1-induced cardiac fibrosis.
Recently, accumulating evidence has reported that miRNA-related mechanisms play critical roles in cardiac fibrosis, and different miRNAs have contrary functions [8, 16, 20, 35,36,37]. For example, Wang et al. [19] found that overexpression of miR-9 inhibited cardiac fibrosis by targeting PDGFR-β. Zhang et al. [38] demonstrated that overexpression of cardiac miR-29b was able to inhibit AngII-induced cardiac fibrosis and improve cardiac dysfunction through the TGF-β/Smad3 pathway. But miRNA-503 promotes angiotensin II-induced cardiac fibrosis by downregulation of Apelin-13 [1]. However, there has been no report on whether miR-98 is differentially expressed in pathological HCFs, or if there are any functional roles of miR-98 in regulating TGF-β1-induced cardiac fibrosis. In this study, we demonstrated that the level of miR-98 was significantly decreased in TGF-β1-induced HCFs. Most importantly, our findings revealed that upregulation of miR-98 inhibited TGF-β1-induced differentiation and collagen production of HCFs. Therefore, this is the first report to show differential expression of miR-98 and the functional role of miR-98 in TGF-β1-induced cardiac fibrosis.
Transforming growth factor-β1 (TGF-β1) directly takes part in the progressive remodeling of cardiac fibrosis in causing heart failure [39,40,41]. The profibrotic effect of TGF-β1 has been shown to be mediated by TGF-β1 receptors (type I and type II) and Smad signaling [42, 43], but the studies concerning TGFBR1 on cardiac fibrosis remain limited. A previous study demonstrated that the application of a TGFBR1 inhibitor reversed differentiation of CF under 3D culture condition [44]. Therefore, suppressing the expression of TGFBR1 to inhibiting the TGF-β signaling pathway may be a promising way to block the differentiation of CFs, resulting in preventing cardiac fibrosis. Zhao et al. reported that miR-101a suppressed cardiac fibrosis induced by hypoxia by downregulation of TGFBR1 on CFs [8]. In this study, we found that TGF-β1-induced cardiac fibrosis was closely related to upregulation of TGFBR1 expression. Moreover, TGF-β1-induced TGFBR1 expression was decreased by miR-98 overexpression. Next, downregulation of TGFBR1 had the similar protective effects as miR-98 overexpression, while the protective effects of miR-98 overexpression were partially abolished by transfection with pcDNA-TGFBR1. Taken together, these outcomes confirmed that upregulation of miR-98 protected HCFs from TGF-β1-induced cardiac fibrosis by targeting TGFBR1.
Our findings showed that overexpression of miR-98 evidently reduces TGF-β1-induced differentiation and collagen accumulation of HCFs by downregulating expression of TGFBR1. These results provide further evidence for protective effect of miR-98 overexpression on TGF-β1-induced cardiac fibrosis. However, there were limitations in this study: all experiments were done in vitro. To further confirm these findings, we will do some animal experiments in a future study.
References
Zhou Y, Deng L, Zhao D, et al. MicroRNA-503 promotes angiotensin II-induced cardiac fibrosis by targeting Apelin-13. J Cell Mol Med. 2016;20(3):495–505.
Zeigler AC, Richardson WJ, Holmes JW, et al. Computational modeling of cardiac fibroblasts and fibrosis. J Mol Cell Cardiol. 2015;93:73–83.
Tao H, Shi KH, Yang JJ, et al. Epigenetic regulation of cardiac fibrosis. Cell Signal. 2013;25(9):1932–8.
Tijsen AJ, van der Made I, van den Hoogenhof MM, et al. The microRNA-15 family inhibits the TGFbeta-pathway in the heart. Cardiovasc Res. 2014;104(1):61–71.
Jiang X, Tsitsiou E, Herrick SE, et al. MicroRNAs and the regulation of fibrosis. FEBS J. 2010;277(9):2015–21.
Dai Y, Khaidakov M, Wang X, et al. MicroRNAs involved in the regulation of postischemic cardiac fibrosis. Hypertension. 2013;61(4):751–6.
van Putten S, Shafieyan Y, Hinz B. Mechanical control of cardiac myofibroblasts. J Mol Cell Cardiol. 2015;93:133–42.
Zhao X, Wang K, Liao Y, et al. MicroRNA-101a inhibits cardiac fibrosis induced by hypoxia via targeting TGFbetaRI on cardiac fibroblasts. Cell Physiol Biochem. 2015;35(1):213–26.
Bei Y, Song Y, Wang F, et al. miR-382 targeting PTEN–Akt axis promotes liver regeneration. Oncotarget. 2016;7(2):1584–97.
Xu T, Zhou Q, Che L, et al. Circulating miR-21, miR-378, and miR-940 increase in response to an acute exhaustive exercise in chronic heart failure patients. Oncotarget. 2016;7(11):12414–25.
Liu X, Xiao J, Zhu H, et al. miR-222 is necessary for exercise-induced cardiac growth and protects against pathological cardiac remodeling. Cell Metab. 2015;21(4):584–95.
Liang D, Xu X, Deng F, et al. miRNA-940 reduction contributes to human tetralogy of fallot development. J Cell Mol Med. 2014;18(9):1830–9.
Xiao J, Liang D, Zhang H, et al. MicroRNA-204 is required for differentiation of human-derived cardiomyocyte progenitor cells. J Mol Cell Cardiol. 2012;53(6):751–9.
Mai L, Xiao L, Huang Y, et al. Novel microRNAs involved in regulation of cardiac fibrosis. Int J Cardiol. 2015;192:14–5.
Gupta SK, Itagaki R, Zheng X, et al. miR-21 promotes fibrosis in an acute cardiac allograft transplantation model. Cardiovasc Res. 2016;110(2):215–26.
Huang Y, Qi Y, Du JQ, et al. MicroRNA-34a regulates cardiac fibrosis after myocardial infarction by targeting Smad4. Expert Opin Ther Targets. 2014;18(12):1355–65.
Nagpal V, Rai R, Place AT, et al. MiR-125b is critical for fibroblast-to-myofibroblast transition and cardiac fibrosis. Circulation. 2016;133(3):291–301.
Wang X, Wang HX, Li YL, et al. MicroRNA Let-7i negatively regulates cardiac inflammation and fibrosis. Hypertension. 2015;66(4):776–85.
Wang L, Ma L, Fan H, et al. MicroRNA-9 regulates cardiac fibrosis by targeting PDGFR-β in rats. J Physiol Biochem. 2016;72(2):213–23.
Tao H, Chen ZW, Yang JJ, et al. MicroRNA-29a suppresses cardiac fibroblasts proliferation via targeting VEGF-A/MAPK signal pathway. Int J Biol Macromol. 2016;88:414–23.
Sang HQ, Jiang ZM, Zhao QP, et al. MicroRNA-133a improves the cardiac function and fibrosis through inhibiting Akt in heart failure rats. Biomed Pharmacother. 2015;71:185–9.
Zhu W, Yang L, Shan H, et al. MicroRNA expression analysis: clinical advantage of propranolol reveals key microRNAs in myocardial infarction. PLoS One. 2011;6:e14736.
Tao H, Yang JJ, Hu W, et al. Noncoding RNA as regulators of cardiac fibrosis: current insight and the road ahead. Pflugers Arch. 2016;468(6):1103–11.
Tao H, Yang JJ, Shi KH, et al. Wnt signaling pathway in cardiac fibrosis: new insights and directions. Metabolism. 2016;65(2):30–40.
Sun M, Yu H, Zhang Y, et al. MicroRNA-214 mediates isoproterenol-induced proliferation and collagen synthesis in cardiac fibroblasts. Sci Rep. 2015;5:18351.
Pellman J, Lyon RC, Sheikh F. Extracellular matrix remodeling in atrial fibrosis: mechanisms and implications in atrial fibrillation. J Mol Cell Cardiol. 2010;48(3):461–7.
Creemers EE, Pinto YM. Molecular mechanisms that control interstitial fibrosis in the pressure-overloaded heart. Cardiovasc Res. 2011;89(2):265–72.
Berk BC, Fujiwara K, Lehoux S. ECM remodeling in hypertensive heart disease. J Clin Invest. 2007;117(3):568–75.
Cucoranu I, Clempus R, Dikalova A, et al. NAD(P)H oxidase 4 mediates transforming growth factor-beta1-induced differentiation of cardiac fibroblasts into myofibroblasts. Circ Res. 2005;987(9):9800–7.
Porter KE, Turner NA. Cardiac fibroblasts: at the heart of myocardial remodeling. Pharmacol Ther. 2009;123(2):255–78.
van den Borne SW, Diez J, Blankesteijn WM, et al. Myocardial remodeling after infarction: the role of myofibroblasts. Nat Rev Cardiol. 2010;7(1):30–7.
Rohr S. Myofibroblasts in diseased hearts: new players in cardiac arrhythmias? Heart Rhythm. 2009;6(6):848–56.
Leask A. Potential therapeutic targets for cardiac fibrosis TGFβ, angiotensin, endothelin, CCN2 and PDGF, partners in fibroblast activation. Circ Res. 2010;106(11):1675–80.
Pelouch V, Dixon IM, Golfman L, et al. Role of extracellular matrix proteins in heart function. Mol Cell Biochem. 1993; 129(2): 101–20.
Zhong C, Wang K, Liu Y, et al. miR-198b controls cardiac fibroblast proliferation and migration. J Cell Mol Med. 2016;20(6):11981–7.
Zhou Y, Deng L, Zhao D, et al. MicroRNA-503 promotes angiotensin II-induced cardiac fibrosis by targeting Apelin-13. J Cell Mol Med. 2016;20(3):4985–5505.
Nagpal V, Rai R, Place AT, et al. MiR-125b is critical for fibroblast-to-myofibroblast transition and cardiac fibrosis. Circulation. 2016;133(3):2981–3301.
Zhang Y, Huang XR, Wei LH, et al. miR-29b as a therapeutic agent for angiotensin II-induced cardiac fibrosis by targeting TGF-β/Smad3 signaling. Mol Ther. 2014;22(5):974–85.
Lijnen PJ, Petrov VV, Fagard RH. Induction of cardiac fibrosis by transforming growth factor-beta(1). Mol Genetic Metabol. 2000;71(1–2):418–35.
Kuwahara F, Kai H, Tokuda K, et al. Transforming growth factor-β function blocking prevents myocardial fibrosis and diastolic dysfunction in pressure-overloaded rats. Circulation. 2002;106(1):130–5.
Lim H, Zhu YZ. Role of transforming growth factor-beta in the progression of heart failure. Cell Mol Life Sci. 2006;63(22):2584–96.
Chen J, Mehta JL. Angiotensin II-mediated oxidative stress and procollagen-I expression in cardiac fibroblasts: blockade by pravastatin and pioglitazone. Am J Physiol Heart Circ Physiol. 2006;291(4):H1738–45.
Liu X, Sun SQ, Hassid A, et al. cAMP inhibits transforming growth factor-beta-stimulated collagen synthesis via inhibition of extracellular signal-regulated kinase 1/2 and Smad signaling in cardiac fibroblasts. Mol Pharmacol. 2006;70(6):1992–2003.
Driesen RB, Nagaraju CK, Abi-Char J, et al. Reversible and irreversible differentiation of cardiac fibroblasts. Cardiovasc Res. 2014;101(3):411–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Cheng, R., Dang, R., Zhou, Y. et al. MicroRNA-98 inhibits TGF-β1-induced differentiation and collagen production of cardiac fibroblasts by targeting TGFBR1. Human Cell 30, 192–200 (2017). https://doi.org/10.1007/s13577-017-0163-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13577-017-0163-0