Abstract
Researchers and policymakers often rely on the infant mortality rate as an indicator of a country’s health. Despite arguments about its relevance, uniform measurement of infant mortality is necessary to guarantee its use as a valid measure of population health. Using important socioeconomic indicators, we develop a novel method to adjust country-specific reported infant mortality figures. We conclude that an augmented measure of mortality that includes both infant and late fetal deaths should be considered when assessing levels of social welfare in a country. In addition, mortality statistics that exhibit a substantially high ratio of late fetal to early neonatal deaths should be more closely scrutinized.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The infant mortality rate (IMR) is often regarded as a barometer for overall welfare of a community or country. As such, the IMR has been used by researchers as an outcome to be explained or as an explanatory variable to capture the socioeconomic development of a country.Footnote 1 Subsequent findings serve as policy conclusions or recommendations. As an example of policy dependence on a measured association between IMR and economic development, at least two of the eight Millennium Development Goals (MDG) directly reference this metric (United Nations 2013).Footnote 2
This article provides evidence that country-specific mortality rates may be reported with error even in countries with comprehensive coverage of mortality statistics and improved birthing characteristics (e.g., skilled antenatal obstetric care, hospital vs. in-home delivery, skilled birth attendant during childbirth). Moreover, we develop a method to correct these measurements so that cross-country comparisons may be made by exploring a potential exception to the inverse relationship between IMR and development: namely, Cuba. Between 2001 and 2011, the average gross domestic product (GDP) per capita of Organisation for Economic Co-operation and Development (OECD) countries exceeded Cuba’s average eightfold. Yet, during that same period, the IMR differed by only about 1 death per 1,000 live births. Perhaps more striking, for that same period, Cuba recorded an average IMR 18 % lower than the U.S. average, while GDP per capita in the United States surpassed that of Cuba by a factor of 10.Footnote 3
Cuba’s apparent IMR success has not gone unnoticed in the general media and academia. In fact, Cuba is often cited as the example of a poor country that has reached health standards comparable with those of rich nations, with this opinion based highly on its IMR.Footnote 4 We examine whether this observed contrast is due to systematic undercounting of infant deaths or actual improvements in infant health care. We show that Cuban official statistics severely undercount infant deaths. Careful analysis suggests that after the reported measures are adjusted, the corrected IMR is close to twice what is reported. Similarly, early neonatal deaths are as many as three times higher than figures reported officially.
Underreporting can be the result of improperly classifying late fetal deaths as early neonatal deaths.Footnote 5 Our findings suggest that 33 % to 50 % of all late fetal deaths may be classified instead as early neonatal deaths. On comparative terms, using the adjusted measures suggests that Cuba’s adjusted IMR is slightly lower, on average, relative to countries with similar economic and social development. When compared with more developed nations, however, Cuba’s adjusted IMR is not at the same level as previously held.
We obtain these results by exploring a significant discrepancy between the late fetal and early neonatal mortality rates reported by Cuba. More specifically, Cuba reports a late fetal mortality rate (LFMR) that is close to six times the reported early neonatal mortality rate (ENMR). As pointed out in previous literature (e.g., Velkoff and Miller 1995), such disparity suggests substantial undercounting of infant deaths that, in turn, leads to artificially low levels of IMR. Using these two indicators, we develop a simple three-stage method that builds on the existing IMR correction literature.
The first stage of our method estimates a more plausible late fetal to early neonatal deaths ratio given that this ratio seems to be substantially higher in Cuba relative to other countries. We estimate the corrected ratio using key socioeconomic determinants of maternal, prenatal, and infant health. Using the estimated ratio, the second stage proceeds to adjust the late fetal and early neonatal deaths. Finally, in the last stage, we use the corrected early neonatal deaths to adjust the reported infant deaths. The method relies on relatively weak assumptions and can be readily applied to any country or region exhibiting reporting disparities similar to those observed in Cuba.
It is important to highlight that corrected IMR figures not only provide a better assessment of a country’s socioeconomic development but also have relevant policy implications. National and foreign aid funds are typically allocated based on the priorities assessed by the state or the funding organizations. Understated mortality statistics might lead to an improper allocation of funds. This misallocation of funds, in turn, may result in less than necessary resources for infant and prenatal health care. Last, policies that try to aggressively reduce infant deaths (such as those pursued by Cuba after the 1959 socialist revolution) may distort incentives among health professionals. For instance, physicians may feel compelled to underreport infant death statistics if they are pressured to reach statistical targets. In the case of Cuba, for example, Hirschfeld (2007a, b) documented such instances of underreporting.
This study proposes two key policy recommendations. First, to reduce the incentives to misclassify infant deaths, an augmented mortality measure that includes both infant and late fetal deaths should be considered when assessing levels of economic development and social welfare in a country. Alternatively, more attention should be given to mortality measures that take fetal deaths into account (i.e., perinatal mortality rate, LFMR, and so on). Second, mortality statistics that exhibit a substantially high number of late fetal deaths (LFDs) relative to early neonatal deaths (ENDs) should be more closely scrutinized because this is typically a sign of misclassification.
Last, an overwhelming concern in comparative studies on infant mortality is the lack of comparable indicators given that definitions of live births and infant deaths vary significantly by country (e.g., European Commission 2003; McFarlane et al. 2003). A key advantage of our study is the use of a unique data set, from the EURO-PERISTAT project (PERISTAT hereafter), which allows for valid comparisons across countries—a feat that is unachievable with other existing data sets. It is important to also highlight that previous treatments of this question in the context of Cuba, albeit very detailed and informative, relied heavily on personal accounts and anecdotal evidence (e.g., Stusser 2012). As a result, quantitative evidence of IMR misreporting is mostly missing in the economics, demography, and development literatures. This article tries to fill the gap by presenting the first data-driven evidence of misreporting using Cuban infant mortality information.
Data and Definitions
To evaluate a country’s reported aggregate health outcome as a metric of improved development, it is important to understand the construction of that health measure—in this case, infant mortality—as well as possible avenues through which discrepancies and difficulties in measurement may arise. In this section, we define discrete time periods on the gestational and infant timeline, and we describe the data available for measurement of infant mortality and its components.
Definitions
Figure 1 depicts periods of fetal and infant development from conception to birth and through the first year of life as classified by the ICD-10 (World Health Organization, WHO 1993). Four of these subperiods are relevant for defining fetal and infant mortality rates. The late fetal period begins at 22 completed weeks of gestation (or at a weight of the fetus of 500g) and ends at birth.Footnote 6 The early neonatal period begins at birth of the fetus and covers the first seven days after birth. The perinatal period encompasses both the late fetal and early neonatal periods. The infant period spans the first year after birth. Mortality rates are defined as the number of deaths occurring in a particular period per 1,000 live births.Footnote 7
Data
Given the inherent difficulties in recording very early deaths, data on early neonatal and late fetal deaths are scarce. A notable exception is a World Health Organization (WHO) study that compiled late fetal and early neonatal deaths for almost every country worldwide for the year 2000 (World Health Organization, WHO 2006).Footnote 8 The depth and scope of these data are tainted by one caveat: rather than using standardized measures to define deaths and live births, the WHO data rely on country-specific definitions.Footnote 9 The variation in these definitions—and, hence, reporting criteria—are a key obstacle for any comparative study. To overcome this limitation, we use a unique data set on perinatal outcomes collected by the EURO-PERISTAT (2008) project that allows for comparable measures of LFMR, ENMR, and IFM.
The PERISTAT project was created in 1999 as part of the European Union’s Health Monitoring Programme in order to “develop valid and reliable indicators that can be used for monitoring and evaluating perinatal health in Europe” (EURO-PERISTAT 2008:19).Footnote 10 The main advantage of this data set is that fetal and infant deaths are consistently recorded across countries by weight (in the case of fetal deaths) and by days since birth (in the case of infant deaths).Footnote 11 This, in turn, allows for measures of late fetal and early neonatal deaths that are comparable across all PERISTAT countries, a feat that was impossible using the WHO study or other available data sets containing birth and death data.
The PERISTAT report provides information on late fetal and early neonatal deaths for 26 European countries for the year 2004.Footnote 12 To compare Cuba’s 2004 infant mortality statistics with those of PERISTAT countries, we obtain data on reported late fetal, early neonatal, and infant deaths from the Cuban Anuario Estadístico de Salud (Dirección Nacional de Registros Médicos y de Salud 2010). The Anuario Estadístico de Salud reports fetal and neonatal deaths following the WHO ICD-10 definitions on fetus weight and days since birth, respectively.Footnote 13 This reporting definition allows for a comparable measure of late fetal and early neonatal deaths between Cuba and the developed countries of the PERISTAT sample. The complete data set is presented in Online Resource 1.
Evidence of Concern
Based on their reported values, Cuba’s IMR (5.79) is statistically the same as the average among PERISTAT countries (mean = 5.06; SD = 3.2). In this section, we compare mortality rates of PERISTAT countries and Cuba along other dimensions. We demonstrate a clear discrepancy that suggests further investigation.
Country Comparisons Using the PERISTAT Sample
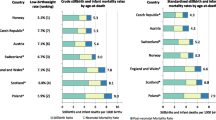
Panel a of Fig. 2 presents LFMRs and ENMRs for PERISTAT countries and Cuba ranked by their perinatal mortality rates (PMRs). For ease of comparison, we show both indicators in the same graph with the ENMR depicted below the horizontal axis. Among PERISTAT countries, the LFMR ranges between 2.52 to 6.53 deaths per 1,000 live births, with an average of 4.19. The values for the ENMR tend to be lower, with an average of 2.36 deaths per 1,000 live births and values ranging between 0.92 deaths in Spain and 3.78 deaths in Latvia. A key takeaway from this graph is that the reported levels of LFMR and ENMR are positively related. This positive association is also depicted in panel b of Fig. 2, which presents a scatter plot of the LFMRs and the ENMRs along with a linear fit for the sample of PERISTAT countries. Although the LFMR tends to be slightly higher than the ENMR, higher levels of ENMR are clearly associated with higher levels of LFMR, and vice versa. Additionally, the correlation coefficient between END and LFD in the PERISTAT sample is approximately .97.
LFMR and ENMR in PERISTAT countries and Cuba, 2004. Panel a shows the LFMR (above vertical axis at 0) and ENMR (below axis) for PERISTAT countries and Cuba. The ENMRs and LFMRs are calculated using reported neonatal and fetal deaths. To allow for comparability between ENMR and LFMR, we use live births (rather than total births for LFMR) in the denominator. Dashed lines depict the average ENMR and LFMR. Panel b presents a scatterplot of LFMR and ENMR with the corresponding linear fit (excluding Cuba)
This similarity is not surprising; in fact, findings from the medical literature and previous cross-country studies support the positive correlation. For example, the 2000 WHO study stated that “stillbirths should equal, or more likely exceed, early neonatal deaths, as shown by data from developed countries, historical datasets and hospital data” (World Health Organization, WHO 2006:8).Footnote 14 According to this report, such behavior is the result of neonatal and fetal deaths having many common causes and determinants.Footnote 15 A study of various Soviet republics comes to a similar conclusion (Velkoff and Miller 1995).
PERISTAT Countries and Cuba Comparisons
We draw the reader’s attention to two findings in Fig. 2a. First, with a reported ENMR of approximately 2.13 deaths per 1,000 live births, Cuba is below the sample average and outperforms countries such as Germany, England, and the Netherlands. Second, the reported indicators for Cuba sharply contradict themselves: although Cuba equaled and even bettered the ENMR of many countries in the PERISTAT sample, the same is not true for the LFMR. In fact, the LFMR level for Cuba is higher than that of all countries in PERISTAT, and the difference is quite substantial. With a reported LFMR of nearly 13 deaths per 1,000 live births, Cuba’s LFMR is almost three times the average LFMR of the PERISTAT countries and two times higher than that of Latvia, which has the highest LFMR in the PERISTAT sample. The discrepancy is further corroborated in panel b of Fig. 2, which shows that Cuba is clearly an outlier relative to the PERISTAT sample.
This finding is unexpected given the correlation in the two measures in the PERISTAT sample and in previous studies. To further clarify this point, Fig. 3 depicts the ratio of LFDs to ENDs. Based on the aforementioned arguments, this ratio should be slightly higher than 1.Footnote 16 For the PERISTAT countries, this expectation holds: these countries exhibit an average ratio of about 1.84 (illustrated by the solid horizontal line), with all observations ranging between 1.04 (Denmark) and slightly more than 3.00 (Spain). Cuba, on the other hand, exhibits a ratio of more than six, or 230 %, higher than the PERISTAT average (panel b, Fig. 3).
Ratio of late fetal deaths (LFD) to early neonatal deaths (END), 2004. In panel a, each spike represents the ratio of late fetal to early neonatal deaths for each country. The solid horizontal line represents the average ratio excluding Cuba (i.e., the PERISTAT average ratio). In panel b, each spike represents the percentage difference between the LFD-END ratios and the PERISTAT average ratio
Velkoff and Miller (1995:255) pointed out (and showed that it is the case for various Soviet republics) that “if early neonatal deaths are being systematically misclassified as late fetal deaths, then the ratio of late fetal to early neonatal mortality will be high compared to its expected value.” With this in mind, the disparity in the LFMR and ENMR might be the result of improperly classifying ENDs as LFDs. This misclassification, in turn, leads to a disproportionate ratio of these two measures as illustrated in Fig. 3.
The similar pattern of very high LFDs relative to ENDs observed in Cuba may be the result of authorities purposely misclassifying ENDs as LFDs in order to present a lower IMR. The incentive for this type of misreporting lies in the technicality that the ENDs are counted in the IMR while LFDs are not. Therefore, this differential treatment of LFDs allows for the possibility that deaths that should be rightly classified as ENDs might, instead, be classified as LFDs. However, the exact reasons for the discrepancy cannot be readily identified from available data. Therefore, the purpose of this article is to report and adjust reporting discrepancies. Nonetheless, we discuss the plausibility of several alternative explanations for the high LFD-END ratio observed in Cuba.
One possible explanation may be that this high ratio resulted from a coding error or a particular shock in Cuba in 2004, the year for which the PERISTAT data are available and hence the year of study in this article. However, the ratios for Cuba from 1996 to 2012 (the latest year for which data are available) have been consistently above 4.0 every year.Footnote 17 An additional possibility may be that Cuba may count late-term abortions (LTAs) as part of LFDs, which would lead to substantially higher levels of LFDs given Cuba’s high abortion rates.Footnote 18 However, the Anuario Estadístico de Salud (Dirección Nacional de Registros Médicos y de Salud 2010) clearly stated that the definitions for perinatal and late fetal deaths used by Cuba follow the WHO ICD-10 definitions, which to the best of our knowledge do not include LTAs as part of fetal deaths.Footnote 19 Last, it is possible that Cuba has understated ENDs rather than misclassified them as LFDs. In this case, our suggested adjustments can be considered a lower bound on the true IMR. We discuss this issue in detail in the following section.
Empirical Strategy
Previous Literature on IMR Estimation
The Brass (1964) and Trussell (1975) methods (and versions derived from them) have been the most widely used early techniques for correcting the IMR so that it may be comparable across countries and reflect as little discrepancy as possible. Recent studies (e.g., Anthopolos and Becker 2010) have noted that the underlying assumptions of these methods might not be realistic in today’s global and highly mobile world. An important assumption is that cohort losses observed in fertility surveys are due to mortality. However, in today’s dynamic world, these losses might instead be the result of migration or displacement due to conflicts, among other things.
A second wave of methods corrects for the underreporting of infant deaths using, primarily, imputation techniques. The main idea behind these methods is to impute questionable indicators with those of countries with more rigorous recording systems and see how the overall mortality trends change as a result. Typical examples are the studies of Kingkade and Sawyer (2001) and Aleshina and Redmond (2005) for various Central Asian and Eastern European countries.
More recent studies diverging from these two methodologies model infant mortality using determinants of economic and social welfare (e.g., Anthopolos and Becker 2010; Lofgren and Lozano 2015). Typical determinants include measures of public health development, social and economic development indicators, and quality of health care and other public amenities. The main contribution of this method is to allow these determinants to serve as explanatory variables, and hence predictors, of the IMR in a standard regression model. Theoretical and empirical support for these determinants comes primarily from the health economics literature where households choose (under certain constraints) health inputs in order to maximize health outcomes. In this case, the health outcome is infant mortality, and the optimization problem is to minimize it.
A New Methodology
In this section, we present a simple three-stage method that builds on the existing IMR correction literature. In Stage 1, we adjust the LFD-END ratio to avoid the discrepancies demonstrated in Figs. 2 (panel a) and 3. Stage 2 adjusts the LFDs and ENDs to obtain lower bounds on their true values. Last, in Stage 3, we adjust the IMR using the corrected input values.
-
Stage 1: Adjusting the LFD-END Ratio
We adjust the late fetal to early neonatal deaths ratio (LFD-END ratio, hereafter) by partially following a combination of the imputation and determinants methodologies. More specifically, we present two alternative approaches for the adjustment of the LFD-END ratio. The first approach, in the spirit of the imputations methodology, uses the reported ratios for the PERISTAT countries as a lower and upper bound for the corrected ratio for Cuba.Footnote 20 The second technique involves estimating a model of the LFD-END ratio as a function of typical fetal and newborn health determinants for the PERISTAT countries. The estimated model is then used to predict the corresponding ratio for Cuba using the observed characteristics.
In the first approach, we define a lower and upper bound for the true LFD-END ratio for Cuba under the following assumption:
-
Assumption 1: The true LFD-END ratio for Cuba is within the range of the reported LFD-END ratio observed in the PERISTAT countries.
Assumption 1 is necessary because the true LFD-END ratio for Cuba is unknown. Moreover, the reported ratio appears to be, as suggested by the evidence presented in the previous section, substantially above its expected value. Therefore, a plausible step is to assume that the true ratio lies within the bounds of the PERISTAT ratios. Using the PERISTAT sample minimum and maximum values for the LFD-END ratios (1.04 and 3.03, respectively), we define r min. and r max. as the minimum and maximum bounds on the LFD-END ratio for Cuba, where r min. = 1.04 and r max. = 3.03.
The second approach for adjusting the LFD-END ratio uses regression techniques. More specifically, we regress the reported LFD-END ratio on a set of determinants of LFD and END using the PERISTAT countries only. We then use the estimated coefficients from this model along with the observed values of the determinants for Cuba to obtain a prediction of the Cuban LFD-END ratio. The predicted ratio is, therefore, the product of the estimated coefficients from the PERISTAT sample and their corresponding determinants observed in Cuba.
More specifically, we estimate the following equation via ordinary least squares (OLS):
where r i is the observed LFD-END ratio for country i in PERISTAT, and x i is a k × 1 vector of k determinants of LFD and END for country i. We use the following eight determinants in various specifications of Eq. (1): maternal mortality rate, abortion rate, rate of LBW, adolescent fertility rate, prevalence of anemia among pregnant women, health expenditure, GDP per capita, and number of practicing physicians.Footnote 21 The maternal mortality rate, abortion rate, rate of LBW, adolescent fertility rate, and prevalence of anemia among pregnant women are considered direct determinants of both LFD and END,Footnote 22 while health expenditure, GDP per capita, and number of practicing physicians capture variation in health care provision, economic development, and other indirect determinants of prepartum and postpartum health.Footnote 23 The determinants in x i are measured in logs. β is a k × 1 vector of parameters to be estimated. Finally, ε i is a zero-mean error term.Footnote 24
As Anthopolos and Becker (2010) noted, measurement error due to underreporting of deaths is an important consideration in this literature because coefficient estimates like those from Eq. (1) might be biased as a result (and hence predictions from the estimated model will be biased). In their case, Anthopolos and Becker (2010) estimated a frontier model that takes into account the residual skewness problem caused by underreporting of deaths by most countries in their sample. In this study, we avoid this problem by using a sample for which underreporting is quite unlikely. Recall that the PERISTAT study was designed precisely to collect reliable and comparable perinatal mortality data across the countries in the sample. Although the data are reliable, the countries in the sample may not represent a random sample of countries considered to be “developed.” We discuss this issue, as well as the effect that it might have on the coefficient estimates and statistical significance, in Online Resource 1.
Although we avoid measurement issues given our sample, it is fair to point out that the predictors in Eq. (1) are endogenously determined. However, the main goal of our exercise is to predict the LFD-END ratio rather than obtain the underlying causal effect of these variables on the LFD-END ratio. In other words, we are interested in the correlations between these variables and the LFD-END ratio.Footnote 25
To obtain the LFD-END ratio for Cuba, we first obtain a prediction of the log of the ratio using the estimated coefficients from Eq. (1) and then retransform the log prediction using the typical normality-based approach.Footnote 26 That is, the predicted ratio for Cuba r Cuba is given by:
where x Cuba is the k × 1 vector of observed determinants for Cuba; β̂ is the k × 1 vector of estimated coefficients using the PERISTAT sample; \( {\widehat{\upsigma}}_{\upvarepsilon}^2 \) is the estimated variance of the residuals ε; and exp is the exponential or anti-log function. To avoid the normality assumption, we also estimate r Cuba using the smearing estimator proposed by Duan (1983), which allows calculating the level predictions without any specific assumption on the errors. Refer to Online Resource 1, Table S3, for results using the smearing estimator along with a brief discussion. The estimates, however, do not differ greatly from those obtained using the normality assumption.
Panel a of Table 1 presents the estimated coefficients from Eq. (1) using the PERISTAT countries as the sample observations. Each specification includes at least one direct determinant of LFD or END and one determinant of overall public health quality and development. Because this regression is performed to obtain correlations that allow us to predict the LFD-END ratio for Cuba (i.e., Eq. (2)), we do not discuss the estimated relationships formally in the text. In general, signs and significance of coefficients on each determinant are as expected. Refer to Online Resource 1 for a detailed discussion of the empirical analysis. Panel b of Table 1 displays the point estimate and 95 % confidence interval of Cuba’s predicted ratio for each of the five specifications of Eq. (1).Footnote 27 The estimated ratios for Cuba range between 1.19 and 1.59, depending on the specification used. Compared with the 2004 reported ratio of 6.10, the expected ratio is three to five times lower. Additionally, each ratio prediction for Cuba is below the PERISTAT average ratio of 1.87. This finding is supported by the fact that the observed covariates for Cuba tend to be closer to those of countries in the PERISTAT sample with LFD-END ratios that are lower than average.
The interval predictions of the ratio range between 0.67 and 3.83. A closer look at the different specifications reveals that the high range is the result of Eqs. (3) and (4). Excluding the interval limits associated with these specifications from the analysis reduces the overall range of the predictions across all remaining specifications to 0.67 and 2.97.Footnote 28
-
Stage 2: Adjusting the LFD and END
The adjustment of the ratio in the previous section (using the imputation or determinants approach) provides a value for r in the following equation:
where LFD * and END * are the true (and thus unknown) late fetal and early neonatal deaths, respectively, and r is the adjusted ratio obtained in the previous section.Footnote 29 Because Eq. (3) contains two unknowns, LFD * and END *, we specify a second equation in order to obtain values for LFD * and END *. Before defining the second equation, we make the following assumption:
-
Assumption 2: Perinatal deaths are correctly reported by Cuba.
Assumption 2 states that although both END and LFD might be misreported, their sum (i.e., perinatal deaths) is not. Plausibility of Assumption 2 comes from the fact that perinatal deaths are relatively simpler to report because by definition, they do not depend on the classification of live births. More specifically, to classify a death as perinatal, the health professional is not required to determine or even know (based on standard classifications) whether the birth is live or not, which tends to be a significant source of confusion given the different definitions. For example, a death occurring intrapartum (i.e., during childbirth) might raise doubts as to whether it should be classified as an LFD or END. This death, however, is classified as perinatal without hesitation. Therefore, although there might be some misreporting in LFDs and ENDs, perinatal death reports tend to be less complicated and more accurate.
Letting PD denote reported perinatal deaths, we specify the following identity:
where PD is known and assumed to be correctly specified by Assumption 2. Solving for the corrected late fetal and early neonatal deaths, we find the following:
where both LFD * and END * are functions of fully observable values of r (defined in various ways in Stage 1) and PD (obtained from Cuba’s reported statistics and assumed to be correctly reported by Assumption 2).Footnote 30 If perinatal deaths are underreported (i.e., Assumption 2 does not hold), then LFD * and END * will be underestimated. Consequently, application of this method is most appropriate for countries with relatively good coverage of perinatal death statistics. If underreporting is suspected, LFD * and END * should be logically interpreted as lower bounds on the true values. In the case of Cuba, where most births occur at health facilities, the issue of poor coverage of perinatal deaths does not seem very daunting.Footnote 31
-
Stage 3: Adjusting the IMR
We use the corrected late fetal and early neonatal deaths from Stage 2 to correct the reported IMR. Letting ID * and ID R denote true and reported infant deaths, respectively, and letting END R denote the reported early ENDs, we calculate the corrected infant deaths for Cuba using the following specification:
where END * is defined by Eq. (6), and the term in parentheses gives all deaths occurring after the early neonatal period. Substituting Eq. (6) into Eq. (7), we obtain an expression for the true infant deaths that is a function of fully observable values:
where ID R, END R, and PD are reported by Cuban authorities, and r is the LFD-END ratio found in Stage 1. After ID * is obtained, it is straightforward to calculate the IMR.
It is important to highlight several aspects of this three-stage calculation. First, from Eq. (8), we can see more clearly the implication of Assumption 2. If perinatal deaths (PDs) are undercounted, the value of ID * will be understated. Thus, it is important to stress that true infant deaths might in fact be higher than the calculated values presented in this article. Second, if deaths after the early neonatal period (ID R – END R) are understated in official statistics, the value of ID * will be equally understated. The degree of underestimation in postneonatal deaths, however, might not be very substantial given that most infant deaths occur in the early neonatal period, which is the period being corrected in this study. Nonetheless, the corrected values presented in this article should be considered a lower bound on the true mortality indicators for Cuba.
Findings
Column 1 in Table 2 presents the reported LFMR, ENMR, and IMR from Cuban data, and the analogous values obtained using the proposed new methodology (columns 2–4). We obtain the values by first using Eqs. (5), (6), and (7) to adjust the raw deaths and then applying the mortality rate definitions to obtain the rates. The panels of Table 2 correspond to the two approaches in Stage 1 used to obtain the corrected LFD-END ratio for Cuba.
For each approach (i.e., imputation and determinants), we present three possible values of the adjusted LFD-END ratio for Cuba. The three possible values are the lower, middle, and upper bounds that the adjusted LFD-END ratio might take based on each approach. With the imputation approach, the lower and upper bounds on the estimated ratio are simply the lowest and highest values for the LFD-END ratio observed in PERISTAT (columns 2 and 4, respectively), while the middle value is the observed median (column 3).Footnote 32 With the determinants approach, the middle value is the point estimate of the prediction (column 3), and the lower and upper bounds (denoted as r .025 and r .975, respectively) are the lower and upper limits of the 95 % prediction interval for Eq. (5) in Table 1. We choose Eq. (5) as the preferred specification because it uses covariates for which Cuba is not an outlier, thus reducing the standard error of the prediction.Footnote 33
For brevity, we discuss the findings using the middle-valued LFD-END ratio as the main ratio estimate (r median in the case of the imputation approach, and r in the case of the determinants approach). We refer briefly to findings using the lower and upper bounds for the ratio at the end of the section. Last, because reference is made to the number of deaths in the discussion, Table 2 also provides these values.
Late Fetal Mortality Rate
The LFMR reported by Cuba in 2004 is higher than expected when compared with the reported ENMR (13.60 vs. 2.13). In column 3 of Table 2, correcting this measure produces an adjusted LFMR that ranges between 8.73 to 9.79 deaths per 1,000 births, depending on the approach used. This adjustment implies a difference between reported rates and the calculated rate using the new methodology of about three to four deaths per 1,000 births. In terms of raw deaths, this new calculation suggests that between 33 % to 50 % of all deaths officially classified as LFD perhaps should be classified as ENDs.
Early Neonatal Mortality Rate
Column 1 of Table 2 shows that for the year 2004, Cuban authorities reported an ENMR of only 2.13 deaths per 1,000 live births. After adjustments, however, this rate might actually be between 5.39 and 6.45 deaths per 1,000 live births depending on the approach used (column 3), suggesting that the ENMR is 2.5 to 3 times higher than the reported one. In terms of raw deaths, potentially 414 to 549 early neonatal deaths are unaccounted for—or, more likely, wrongly classified as late fetal deaths. In relative terms, our new calculation implies that between 60 % to 67 % of all early neonatal deaths were either omitted from official statistics or wrongly classified as late fetal deaths.
Infant Mortality Rate
Using the new methodology, the IMR of Cuba likely ranges between 9.04 and 10.11 infant deaths per 1,000 live births compared with the 5.79 reported officially. To put these figures in perspective, the actual rate might be as much as 76 % higher (10.11 vs. 5.79) than the reported one. It is possible that 36 % to 43 % of all infant deaths in Cuba in 2004 might be misreported.
Recall that our earlier discussion uses the middle value of the adjusted LFD-END ratio to obtain the adjusted mortality rates. Using the lower bounds of the adjusted ratio to calculate mortality rates (i.e., r min. in the imputation approach and r .025 in the determinants approach) reveals that the ENMR and IMR tend to be higher than the aforementioned ones because a lower LFD-END ratio implies higher early neonatal deaths relative to late fetal deaths. The largest calculations are 8.65 for the ENMR and 12.31 for the IMR (using the determinants approach presented in panel b of Table 2). For such estimates, the amount of underreporting is overwhelming: the corrected ENMR is more than four times the reported value (8.65 vs. 2.13), and the corrected IMR is more than twice the reported one (12.31 vs. 5.79).
In the case where the estimated ratio is relatively high (i.e., r max. in the imputation approach and r .975 in the determinants approach), the estimates of the ENMR and IMR are lower than the ones using the middle-valued ratio. Depending on the resulting calculations, the reported ENMR and IMR for Cuba may not be artificially low if they are contained within the limits of the imputation bounds or if they are inside the confidence interval of the determinants prediction. However, a closer look at the results in Table 2 reveals that even the lowest possible estimates of the true ENMR and IMR are significantly higher than the officially reported values.Footnote 34 In the case of the ENMR, the lowest possible estimate of 3.80 deaths per 1,000 live births is almost twice the 2.13 reported value.Footnote 35 Similarly, the lowest possible IMR estimated is close to 29 % higher than the reported 5.79 deaths per 1,000 live births.
Updated Ranks
The fact that the IMR is a widely used indicator for cross-country comparisons makes the exercise of analyzing the effect of the corrected IMR on the relative rankings a necessary one. When compared with the PERISTAT sample, the adjusted mortality rates suggest that Cuba’s standing is significantly affected. In the case of the ENMR, the corrected value is much higher than the PERISTAT average of 2.36 and well above the highest ENMR observed in this sample.Footnote 36 Moreover, Cuba’s adjusted IMR places it at the bottom of the PERISTAT sample. It is close to twice the observed average of 5.06 and higher than all other PERISTAT countries.
On a broader scale, comparing the adjusted IMR values for Cuba with those of countries from different income levels and regions of the world suggests significant drops in the mortality rankings. Figure 4 shows boxplots of the infant mortality rates for high- and middle-income countries (panel a) and European, Latin American, and North American countries (panel b).Footnote 37 The solid vertical line represents the mid-value for the calculated IMR in Cuba, and the dashed vertical line represents the reported IMR.Footnote 38 Notice that in panel a, Cuba’s reported IMR is within the range of high-income countries and significantly lower than the IMR of middle-income countries. However, the estimated median value (solid vertical line) is substantially higher than the median for high-income countries (10.11 in Cuba vs. 4.60 in high-income countries).
Corrected ranks by income level and world regions, 2004. World Bank definitions for geographic location as well as income division (i.e., high, middle income) are used. L. Am. refers to Latin America, and N. Am. refers to North America. The solid vertical line represents the median IMR estimated for Cuba using the determinants approach. The vertical dashed line represents the reported IMR for Cuba
Panel b of Fig. 4 provides boxplots of the IMR for different regions of the world. The choice of Europe and North America is to illustrate how Cuba’s estimated IMR fares compared with that of relatively rich countries to which it is often associated. The choice of Latin America comes from the fact that Cuba is often cited as a “positive” outlier in the region because of its superior infant mortality indicators. Looking at the reported values (dashed line), Cuba’s IMR is the lowest in Latin America and well within the ranges of Europe and North America. However, Cuba’s corrected median IMR rate (solid line) is higher than that of Europe and North America.Footnote 39 Surprising, however, is that compared with Latin America, Cuba might not be a “positive” outlier after all. Although still low compared with the region, the actual infant mortality rate in Cuba might be higher than that of Chile (8 deaths per 1,000 live births) and close to that of Costa Rica (9.4 deaths per 1,000 live births).
Conclusion
In this study, we use unique data from 28 countries with similar reporting criteria in fetal and infant deaths in order to construct a new methodology for calculating IMR in countries with observed discrepancies in the components of this indicator. The new methodology explores two approaches to adjusting the reported late fetal, early neonatal, and infant deaths. It further examines the recent claim that Cuba has achieved IMRs that are comparable with those of developed countries.
Our findings cast doubt on the validity of the infant mortality figures reported by Cuba and the commonly held belief that such figures are comparable with those of more developed nations. Additionally, the new methodology shows that the relative infant mortality ranking of Cuba declines when underreporting is taken into account. A similar argument holds for other key indicators, such as the late fetal and the early neonatal mortality rates.
The analysis suggests two recommendations. First, reported mortality statistics that exhibit a sharp gap between END and LFD should be more closely scrutinized. Second, an augmented or more inclusive measure of mortality that includes both infant as well as late fetal deaths can be used to accurately capture mortality with the least difficulty and discrepancy in measurement. More importantly, this measure could help reduce the incentive to misclassify the components of perinatal deaths in order to reduce the IMR.
This article presents a simple yet applicable method for correcting the LFMR, ENMR, and IMR. The method can be applied to other countries or regions that exhibit reporting disparities similar to the ones evidenced in Cuba. However, the use of this method is not recommended in cases where countries have poor coverage of perinatal mortality (i.e., deaths during the late fetal and early neonatal periods are not observed or recorded). Instead, this procedure may be more suitable for countries or regions with relatively good observance of perinatal deaths but where classification of the components of this mortality indicator (i.e., late fetal and early neonatal deaths) are prone to error and, hence, lead to discrepancies like the ones observed in Cuba.
Notes
These calculations use World Bank data from the period 2001–2011, which is the most recent decade for which GDP and IMR data are available for both Cuba and OECD countries. Specifically, average GDP per capita in constant 2005 U.S. dollars is $4,077 (Cuba) and $35,844 (OECD), and average IMR is 5.45 (Cuba) and 4.28 (OECD). Using purchasing power parity–adjusted GDP per capita, the ratio of GDP per capita between OECD countries and Cuba, and that of the United States and Cuba, is 2.39 and 3.22, respectively.
Refer to the Data and Definitions section for definitions of late fetal and early neonatal deaths.
Throughout this study, we use the fetus weight (rather than the gestational age) as the classification criteria for late fetal deaths. Hence, a death of a fetus weighing 500 g or more constitutes a late fetal death.
Following the ICD-10 definitions, the late fetal mortality rate (LFMR) uses total births (live births + fetal deaths) instead of live births only.
A follow-up study describes these deaths for the year 2004 (World Health Organization, WHO 2007).
The definition of a live birth varies greatly from country to country and even within countries. For example, some countries declare a live birth only if the newborn weighs at least 500 g or if the gestational age is at least 22 weeks, while other countries might have no lower limit on classifications of live births.
For more information on data collection for each country, refer to the European Perinatal Health Report prepared by the EURO-PERISTAT (2008) project.
In the case of fetal deaths, most PERISTAT countries use a cutoff for their classifications of at least 500 g or 22 weeks of gestation as recommended by the WHO ICD-10 definitions. In the case of live births, most countries did not have a limit on weight or gestational age in their classifications.
Data for the United Kingdom is divided into three regions: England and Wales, Northern Ireland, and Scotland. In this analysis, we exclude France because of an obvious disparity in the reported live births and fetal deaths (i.e., only 14,737 live births are reported when, according to other sources, there were more than 700,000). Cyprus and Greece were excluded because of missing comparable information on fetal deaths.
Similar to PERISTAT countries, Cuba reports all deaths of fetuses weighting at least 500 g. In the case of live births, it is not clear from the Anuario Estadístico de Salud (2010) whether very LBW and extremely LBW births are included in their classification. However, the definition of live births does not play a significant part in the correction of mortality statistics presented in this article.
Stillbirths are equivalent to late fetal deaths.
A 2004 follow-up study by the same organization found that the average LFMR and ENMR across various world regions are very similar. For example, the average LFMR and ENMR for Africa were 28 and 29, respectively; for Asia, 25 and 23; for Latin America and the Caribbean, 8 and 10; for Europe, 5 and 4; and for North America, 3 and 3.
Recall that the WHO study states that the LFD should equal or, more likely, exceed the END.
Refer to Online Resource 1, Fig. S1, for the LFD-END ratio for Cuba between 1996 and 2012, along with LFDs and ENDs.
See Belanger and Flynn (2009) for a discussion of abortions and state-sponsored abortion policies in Cuba.
An alternative point of concern is that PERISTAT countries might classify LTAs as LFDs. In the case of PERISTAT countries, there is very little indication that they include LTAs as part of LFDs. According to the report, most countries used the WHO’s ICD-10 definition as well. However, it is important to highlight that even if PERISTAT countries include LTAs in their LFDs, the results presented in this article are valid because Cuba’s LFD-END ratio is an outlier even when PERISTAT countries’ ratios are artificially inflated by the inclusion of LTAs. See footnote 30 for a detailed explanation of this aspect after discussing the empirical methodology.
This expands on the idea presented in Gonzalez (2015).
Table S2 in Online Resource 1 provides a detailed description of these determinants.
Hemminki and Rimpela (1991) and Singh et al. (1997) provided examples of studies where LBW is clearly associated with anemic women. Other studies, such as Tamura et al. (1996) and Rondo et al. (1997), showed a positive association between preterm delivery (an important determinant of fetal deaths) and the incidence of anemia in mothers. See Allen (2000) for a survey of the detrimental effects of anemia on pregnancy outcomes. In the case of adolescent pregnancy, Olausson et al. (1999) found that the risk of neonatal mortality is significantly increased for mothers aged 13–17 relative to mothers aged 20–24. The rates of very preterm births are also significantly higher for the former age group relative to the latter. In the case of maternal mortality, Anderson et al. (2007) found in Haiti that after a maternal death, the likelihood of experiencing the loss of the child is approximately 55 %. In the case of abortions, we want to capture the possibility that abortions may affect LFDs in cases where LTAs may be classified as LFDs. We thank an anonymous referee for this suggestion.
Refer to Online Resource 1 for further discussion of the choice of dependent variable and the functional form for Eq. (1).
Refer to Shmueli (2010) for a detailed treatment of the differences between explanatory and predictive modeling.
Recall that because all specifications use a log-log form, the linear prediction needs to be retransformed from logs to levels.
Refer to Online Resource 1 for a detailed description of the specifications used. The 95 % confidence intervals of the predictions (in brackets below the point estimates in Table 1) are calculated via bootstrap with 250 replications. Each replication involves a draw of the sample with replacement and of size equal to the sample size in the corresponding specification. The lower and upper levels of the interval are given by the 2.5 and 97.5 percentiles, respectively, of the distribution of estimates obtained from the 250 replications.
Both the high point estimate and the wide confidence interval in Eqs. (3) and (4) relative to other specifications result from including two regressors—namely, the maternal mortality rate and the number of physicians—for which Cuba is a significant outlier. As discussed in Online Resource 1, this leads to unnecessary inflation of the standard error of the prediction (Verbeek 2008) and hence the limits of the confidence interval.
Because the proceeding analysis uses the adjusted ratio for Cuba, we omit the Cuba subscript used before.
In Eq. (6), if PERISTAT countries classify late-term abortions as LFDs, then r would be higher, and thus Cuba’s corrected ENDs would be lower than if LTAs were not part of LFDs in comparison countries. If that is the case, then Cuba’s corrected ENDs should be interpreted as a lower bound on the actual ENDs.
An interesting exercise that might be used to assess the validity of Assumption 2 would be to compare perinatal mortality rates across urban and rural regions in Cuba. The idea is that the quality of perinatal mortality records may differ substantially between rural and urban areas as is the case in many developing countries. Therefore, lower levels of perinatal mortality in rural areas relative to urban areas should raise flags on the quality of the perinatal statistics. Unfortunately, Cuba does not provide fetal and neonatal mortality data by region or urban/rural status in order to perform these comparisons. However, most births in Cuba occur within health facilities, even in rural areas. For example, for 2004, Cuba reported that 99.9 % of births took place in health facilities (Dirección Nacional de Registros Médicos y de Salud 2010).
r min., r median, and r max. are 1.04, 1.80, and 3.03, respectively.
See Verbeek (2008), for example, for a detailed treatment of this issue.
These estimates are the ones obtained using the imputation approach presented in panel a of Table 2.
This value corresponds to using the highest LFD-END ratio observed in the PERISTAT sample.
The highest ENMR corresponds to Latvia with 3.78 deaths per 1,000 live births.
The data used to classify countries by income (high, middle) and geographical region (Europe, Latin America, North America) are from statistics reported by the World Bank (2015).
The solid vertical line uses the determinants approach (column 3, panel b in Table 2). The same analysis using the estimates from the imputation approach yields similar conclusions.
The boxplot for North America includes only two countries (Canada and the United States). Therefore, the lower and upper ends of the box are the reported IMR for these two countries, and the middle line is simply the average of the IMR for the two.
References
Aleshina, N., & Redmond, G. (2005). How high is infant and child mortality in central and eastern Europe and the CIS? Population Studies, 59, 39–54.
Allen, L. H. (2000). Anemia and iron deficiency: Effects on pregnancy outcomes. American Journal of Clinical Nutrition, 71, 1280–1284.
Anderson, F., Morton, S., Naik, S., & Gebrian, B. (2007). Maternal mortality and the consequences on infant and child survival in rural Haiti. Maternal and Child Health Journal, 11, 395–401.
Anthopolos, R., & Becker, C. M. (2010). Global infant mortality: Correcting for undercounting. World Development, 38, 467–481.
Belanger, D., & Flynn, A. (2009). The persistence of induced abortion in Cuba: Exploring the notion of an “abortion culture.” Studies in Family Planning, 40, 13–26.
Birchenall, J. A. (2007). Economic development and the escape from high mortality. World Development, 35, 543–568.
Brass, W. (1964, December). Uses of census and survey data for the estimation of vital rates. Paper presented at the African Seminar on Vital Statistics, Addis Ababa, Ethiopia.
Chay, K. Y., & Greenstone, M. (2000). The convergence in black-white infant mortality rates during the 1960’s. American Economic Review, 90, 326–332.
Cooper, R. S., Kenelly, J. F., & Orduez-Garca, P. (2006). Health in Cuba. International Journal of Epidemiology, 35, 817–824.
DePalma, A. (2007). “Sicko,” Castro and the “120 Years Club.” New York Times. Retrieved from http://www.nytimes.com/2007/05/27/weekinreview/27depalma.html
Dirección Nacional de Registros Médicos y de Salud. (2010). Anuario Estadístico de Salud 2010. La Habana, Cuba: Dirección Nacional de Registros Médicos y de Salud.
Duan, N. (1983). Smearing estimate: A nonparametric retransformation method. Journal of the American Statistical Association, 78, 605–610.
European Commission. (2003). Demographic statistics: Definitions and methods of collection in 31 European countries (Population and Social Conditions Working Paper No. 25). Luxembourg: Office for Official Publications of the European Communities.
EURO-PERISTAT. (2008). European perinatal health report. Retrieved from http://www.europeristat.com/
Foster, A., Gutierrez, E., & Kumar, N. (2009). Voluntary compliance, pollution levels, and infant mortality in Mexico. American Economic Review, 99, 191–197.
Gonzalez, R. (2015). Infant mortality in Cuba: Myth and reality. Cuban Studies, 43, 19–39.
Gruber, J., Hendren, N., & Townsend, R. M. (2014). The great equalizer: Health care access and infant mortality in Thailand. American Economic Journal: Applied Economics, 6, 91–107.
Gupta, S., Verhoeven, M., & Tiongson, E. R. (2003). Public spending on health care and the poor. Health Economics, 12, 685–696.
Hemminki, E., & Rimpela, U. (1991). Iron supplementation, maternal packed cell volume, and fetal growth. Archives of Disease in Childhood, 66, 422–425.
Hirschfeld, K. (2007a). Health, politics, and revolution in Cuba since 1898. Piscataway, NJ: Transaction Publishers.
Hirschfeld, K. (2007b). Reexamining the Cuban health care system: Toward a qualitative critique. Cuban Affairs, 2(3). Retrieved from http://www.cubanaffairsjournal.org
Kingkade, W., & Sawyer, C. (2001, August). Infant mortality in Eastern Europe and the former Soviet Union before and after the breakup. Paper presented at the 2001 IUSSP Meetings, Salvador de Bahia, Brazil.
Lofgren, K., & Lozano, R. (2015, May). Perinatal mortality in Mexico: Levels and trends by state and municipality, 1990 to 2013. Paper presented at the annual meeting of the Population Association of America, San Diego, CA.
McFarlane, A., Gissler, M., Bolumar, F., & Rassmusen, S. (2003). The availability of perinatal health indicators in Europe. European Journal of Obstetrics and Gynecology and Reproductive Biology, 111, 15–32.
McGuire, J. W. (2006). Basic health care provision and under-5 mortality: A cross-national study of developing countries. World Development, 34, 405–425.
Olausson, P. O., Cnattingius, S., & Haglund, B. (1999). Teenage pregnancies and risk of late fetal death and infant mortality. BJOG: An International Journal of Obstetrics and Gynaecology, 106, 116–121.
Ozcan, S. (2002). Does the mortality decline promote economic growth? Journal of Economic Growth, 7, 411–439.
Preston, S. H. (2007). The changing relation between mortality and level of economic development. International Journal of Epidemiology, 36, 484–490.
Pritchett, L., & Summers, L. (1996). Wealthier is healthier. Journal of Human Resources, 31, 841–868.
Rondo, P., Abbott, R., Rodrigues, L., & Tomkins, A. (1997). The influence of maternal nutritional factors on intrauterine growth retardation in Brazil. Paediatric and Perinatal Epidemiology, 11, 152–166.
Shmueli, G. (2010). To explain or to predict? Statistical Science, 25, 289–310.
Singh, P., Tyagi, M., Kumar, A., Dash, D., & Shankar, R. (1997). Fetal growth in maternal anemia. Journal of Tropical Pediatrics, 43, 89–92.
Stusser, R. J. (2012). Demystifying the Cuban health system: Insider’s view. Cuba in Transition, 21, 222–234.
Tamura, T., Goldenberg, R., Johnston, K., Cliver, S., & Hickey, C. (1996). Serum ferritin: A predictor of early spontaneous preterm delivery. Obstetrics and Gynecology, 87, 360–365.
Trussell, T. J. (1975). A re-estimation of the multiplying factors for the brass technique for determining childhood survivorship rates. Population Studies, 29, 97–108.
United Nations. (2013). Millennium development goals and beyond, 2015. Retrieved from http://www.un.org/millenniumgoals/
Velkoff, V. A., & Miller, J. E. (1995). Trends and differentials in infant mortality in the Soviet Union, 1970–90: How much is due to misreporting? Population Studies, 49, 241–258.
Verbeek, M. (2008). A guide to modern econometrics (3rd ed.). Chichester, UK: John Wiley and Sons.
World Bank. (2015). World Bank Databank. Retrieved from http://databank.worldbank.org
World Health Organization (WHO). (1993). International statistical classification of diseases and related health problems (10th revision) (ICD-10). Geneva, Switzerland: WHO.
World Health Organization (WHO). (2006). Neonatal and perinatal mortality: Country, regional and global estimates. Geneva, Switzerland: WHO.
World Health Organization (WHO). (2007). Neonatal and perinatal mortality: Country, regional and global estimates 2004. Geneva, Switzerland: WHO.
Acknowledgments
We thank Roberto Martin Gonzalez, M.D., Charles Becker, and participants at the annual meeting of the Association for the Study of Cuban Economy (ASCE) for useful comments and suggestions.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
ESM 1
(PDF 280 kb)
Rights and permissions
About this article
Cite this article
Gonzalez, R.M., Gilleskie, D. Infant Mortality Rate as a Measure of a Country’s Health: A Robust Method to Improve Reliability and Comparability. Demography 54, 701–720 (2017). https://doi.org/10.1007/s13524-017-0553-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13524-017-0553-7