Abstract
Recent studies of migration and the left-behind have found that elders with migrant children actually experience better health outcomes than those with no migrant children, yet these studies raise many concerns about self-selection. Using three rounds of panel survey data from the Indonesian Family Life Survey, we employ the counterfactual framework developed by Rosenbaum and Rubin to examine the relationship between having a migrant child and the health of elders aged 50 and older, as measured by activities of daily living (ADL), self-rated health (SRH), and mortality. As in earlier studies, we find a positive association between old-age health and children’s migration, an effect that is partly explained by an individual’s propensity to have migrant children. Positive impacts of migration are much greater among elders with a high propensity to have migrant children than among those with low propensity. We note that migration is one of the single greatest sources of health disparity among the elders in our study population, and point to the need for research and policy aimed at broadening the benefits of migration to better improve health systems rather than individual health.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
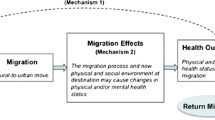
Population aging and migration pose a potential crisis of old-age support in less-developed countries (LDCs), particularly in rural areas that lack institutional support mechanisms, such as nursing homes. Yet, recent studies of the impact of children’s migration on elders left behind by migrant kin suggest an alternative conclusion. Rather than creating a healthcare vacuum in rural areas, migration can actually be a valuable resource for improving health and development (Nyberg-Sørensen et al. 2002; Ozden and Schiff 2007). An emerging literature has begun to address such effects, generally finding better health among elders with migrant children than among those without (Kuhn 2005; Nguyen et al. 2006). This literature, however, has yet to address issues of self-selection bias, whereby individuals who are most likely to remain in good health are also most likely to have migrant children, making it difficult to establish whether children’s migration actually causes better health.
Social and demographic researchers have grown increasingly concerned with establishing causal relationships between individual behaviors and health outcomes (Bhrolcháin 2001; Lieberson 1987, 1991; Link and Phelan 1995; McMichael 1999; Raftery 2001; Sobel 2000). Establishing causation is particularly challenging for a behavior like migration, which is both embedded in, and determined by, a nexus of social and economic advantages and disadvantages that also directly or indirectly affect health (Curran 2002; Curran and Saguy 2001; Portes and Sensenbrenner 1993). While demand for migrants is exogenously driven by labor markets, supply is determined by national and regional variations; observed micro-level factors such as gender, kinship, socioeconomic status, and health itself; and unmeasurable latent factors that could include aggression, risk-seeking, and savvy (Curran and Rivero-Fuentes 2003; Knodel and Saengtienchai 2007; Massey 1988, 1990, 1999). Although many studies have addressed causation when modeling effects of migration on the health of migrants themselves, such scrutiny has not yet been applied to the health of the left-behind (Hummer et al. 1999; Palloni and Arias 2004).
We address these concerns here by modeling the effects of internal migration of prime-age adults on the health of parents left behind in rural areas of Indonesia. In Indonesia, as in a great many LDCs, absolute numbers and relative proportions of elderly among the total population are rising as fertility and mortality rates decline, placing an increasing health burden on family members and health care systems (Chang 1992; Kabir et al. 1998; Rahman 2000). Internal migration opportunities in Indonesia have been facilitated by a steady rise in both gross domestic product (GDP) and foreign investment in conjunction with increased labor force human capital (Brown 2003; Hill 1995, 1996; Hugo 1982; Speare and Harris 1986). The rich data available from three rounds of Indonesian Family Life Survey (IFLS) provide detailed kinship modules and a large sample size, both necessary for our study. These factors make Indonesia an excellent site to examine the effect of migration on the health of rural elders.
Our research design achieves greater causal certainty by longitudinally ordering events and employing a counterfactual methodological framework developed by Rosenbaum and Rubin (1983a, 1984; Rubin 1974, 1977) to address self-selection into migration. We briefly review the consequences of migration for the left-behind, potential sources and consequences of self-selection, and approaches to account for selection. We then detail our plan of analysis and report the results of models by using a counterfactual framework for the association between children’s migration and an elder’s self-rated health status, observed mobility impairments, and mortality.
Background
Old-Age Health and Migration in Developing Countries
After controlling for age and sex variations, researchers have found intergenerational social support networks to be the most important predictors of old-age health and survival in LDCs, even in the face of declining family size (DaVanzo and Chan 1994; Hermalin 2002; Kalache and Sen 1998; Rahman 1999; Rahman et al. 2004; Seeman et al. 1994). By contrast, studies in LDCs offer limited support for the direct impact of socioeconomic status, wealth, or education on health that are found in many wealthy nations (Cutler et al. 2006; Frankenberg et al. 1999; Liang et al. 2001; Rogers et al. 2000; Zimmer et al. 2004; Zimmer and Martin 2007). As such, increasing levels of migration from rural areas have generated concerns regarding the social penalty for left-behind elders in the form of reduced functional support and increased psychosocial isolation (Chang 1992; Rahman 1999).
Empirical research, however, has suggested that parents may actually benefit from their child’s migration (Beard and Kunharibowo 2001; Frankenberg et al. 2002; Keasberry 2001; Knodel and Debavalya 1997; Kuhn 2005, 2006; Rahman 1999, 2000; Toyota et al. 2007). Kuhn (2005) evaluated the effects of migration on the health of left-behind elders in rural Bangladesh and found that compared with elders with no migrant children, those with children living outside their district or country were both 30% more likely to be in good health (according to self-reported health and physical exams) and 30% less likely to have died in a subsequent four-year follow-up period. Therefore, rather than being a catalyst for destroying traditional systems of health production through children’s absence, migration may instead play a key role in a revised theoretical framework of the role of migrant children in old-age support.
Such findings support the well-established expectations of the “New Economics of Labor Migration,” a cooperative model in which migrants share risks and resources with the left-behind and base their migration decisions on preexisting household conditions and parental needs (Kreager 2006; Kuhn 2003; Stark and Bloom 1985; VanWey 2004). Cooperative models point to clear pathways that may offset any social penalty associated with children’s migration (Frankenberg et al. 2002; Keasberry 2001; Knodel and Debavalya 1997; Rahman 2001). For example, remittances, or economic transfers, from migrants to the left-behind can improve the standard of living of the elderly on a daily basis (Asis 2006; Frankenberg and Kuhn 2004; Hadi 1999; Kanaiaupuni and Donato 1999). Further, migrant children may provide significantly larger financial transfers during a health crisis, acting as a basic health insurance policy. Finally, increasing levels of technology can facilitate communication concerning health-related information via phone calls or the Internet (Frank and Hummer 2002; Hadi 1999; Kanaiaupuni et al. 2005; Taylor 1999). Improved communication may also mitigate the social penalties associated with having a migrant child (Guo et al. 2009; Knodel and Saengtienchai 2007; Kreager 2006).
A cooperative framework also reshapes our understanding of migrant selectivity. While some elders might suffer as a result of a child’s migration, this very possibility might encourage children to avoid migration altogether unless their parents are on a healthy trajectory. More generally, the cooperative model suggests that migrants may have greater education, socioeconomic resources, or social capital, and thus their kin may also have better health outcomes even in the absence of migration (Massey et al. 1999; VanWey 2004). These sources of self-selection cast doubt on the positive association between migration and the health of left-behind elders.
Selection and Causation
Recent years have seen an intensified interest in addressing self-selection in observational social statistics, particularly with respect to establishing causal relationships (Marini and Singer 1988; Miech et al. 1999). This is especially true in the migration literature (Borjas 1987). Considerable research has addressed the “healthy migrant effect,” whereby migrants are typically healthier than randomly selected individuals from their home community (Abraido-Lanza et al. 1999; Jasso et al. 2004; Marmot et al. 1984; Palloni and Arias 2004; Sorlie et al. 1993; Wingate and Alexander 2006). Concerns of self-selection are also relevant when examining the impact of kin migration on the health of the left-behind.
Several sources of self-selection bias may potentially overstate the positive effects of migration on the health of the left-behind. First, healthy migrants may share a latent genetic predisposition for good health with their parents. Second, shared latent factors (e.g., determination, innovation) may both select the child into migration as well as drive the parents toward better health-seeking behaviors. Third, considerable evidence now suggests that migrants may emerge from families with greater social or economic resources than families without migrants, thereby predisposing their parents to better health (Kuhn 2003, 2005; Portes and Sensenbrenner 1993; VanWey 2004). Finally, as we discussed earlier, declining parental health may impinge directly on a child’s migration decision. Although a panel design can address some of these concerns by observing changes in health after controlling for a given baseline health status, concerns still persist regarding the latent aspects of self-selection that are too difficult to control for in statistical models (Palloni and Morenoff 2001).
In response to these concerns, scholars have employed several approaches, including randomized or quasi-randomized experiments and instrumental variables (Duncan et al. 2007; Huston et al. 2005; McKenzie et al. 2010). A number of studies have used an instrumental variable (IV) that predicts the treatment variable but not the outcome variable, thereby mimicking random assignment (Antman 2008; McKenzie and Hildebrandt 2005). The most common IV approach uses ecological variables, such as distance to key destination sites or migration access points (e.g., roads and ports), to identify selection into migration. However, such instruments, if they are available, typically identify only between-community variation in migration activity, not variation between households within the same community. Moreover, a robust theoretical model of the social determinants of health would anticipate that these ecological factors would have direct effects on health, drawing into question their external validity as instruments.
An alternate approach to addressing self-selection in observational data is the counterfactual framework that we employ in this article. In the counterfactual approach, a composite propensity score is estimated from a series of observed covariates that predict the probability that an individual will engage in a treatment behavior (Rosenbaum and Rubin 1983a, 1983b, 1984; Rubin 1974, 1977). From this score, a pseudo-randomized experimental data set is generated that ensures every treatment case is matched by a comparable, counterfactual control case. This restriction is called the “area of common support” (ACS). Balance is further achieved by identifying propensity blocks within which the treatment and control propensity scores are statistically similar. These blocks ensure that “the covariate distribution for those in the control group is approximately the same as the treatment group” (Little and Rubin 2000:138). Further balance is gained through the matching of treatment and control cases with common propensity or covariates to identify an “average treatment effect” (Rosenbaum and Rubin 1983a, 1983b; Rubin 1974).
Propensity scores, which have been used in several fields to adjust for potential selection biases into a specific “treatment” group, have been found to eliminate significant portions of the selection bias present in simple observational estimates (Diaz and Handa 2006). For example, epidemiologists have used the counterfactual approach for evaluating the behavioral determinants of health (Aiken et al. 1994; Cochran 1968; Gum et al. 2001; Joffe and Rosenbaum 1999; Stone et al. 1995; Sturmer et al. 2006). A few studies have applied the counterfactual approach to migration, studying the effects of migration distance on wage growth (Ham et al. 2004), the quality of the education-occupation match (Quinn and Rubb 2005), the effects of remittances on household labor supply (Acosta 2006), and the effect of past migration to the United States on the wealth of older Mexicans (Wong et al. 2007).
In a recent randomized experimental study of the effects of migration on wages, McKenzie et al. (2010) compared their “gold standard” experimental coefficients with those derived from an ordinary least squares (OLS) model, a number of IV models, and a propensity score model. Compared with the experimental estimate, the OLS estimates overstated coefficients by about 40%. The effectiveness of IV specifications depended on the quality of the instrument and overestimated the effect between 8% and 82%, depending on the instrument employed. In comparison, propensity score specifications overstated point estimates by about 19%–20% relative to the experimental results, removing about one-half of the bias present in the OLS approach. Statistical testing showed that the propensity estimates did not significantly differ from the experimental estimates. Taken together, the counterfactual estimator outperformed OLS or IV using a generic instrument.
No studies to date have used a counterfactual approach to address the consequences of migration on the health of the left-behind, despite the pressing empirical need to assess whether the main effects of migration are, in fact, properly identified. The approach, however, is well-suited to account for the tendency of migration to augment preexisting social cleavages. It also presents the opportunity to stratify results by propensity block, thereby conducting a series of mini-experiments on the effect of children’s migration on adult health among groups of high, medium, and low propensity to engage in treatment behaviors.
Our estimation strategy involves the proper sequencing and identification of the precursors of migration (selection), migration itself (the stimuli), and health outcomes. We conceptualize the “treatment” as having an internal migrant child, and address the extent to which the positive effects of children’s migration on health are explained by the propensity to have migrant children. Our propensity score analysis focuses on predisposing variables well-known to impinge on the migration decision, including household socioeconomic status, prior migration experience, education, availability of kin, and prior parental health status. Moreover, each of these variables is also a potential predictor of old-age health and mortality in its own right. With a stable and theoretically informed set of propensity factors, our models of old-age health focus on the treatment effects of migration, with only basic controls for factors that are well-known to affect adult health status (e.g., age, sex, total number of children) and no measures of the intervening impacts of migration (e.g., remittances). After our approach and the significance of migration treatment effects are established, future work may address intervening pathways and interactions with other predictors of old-age health.
We focus exclusively on the impact of internal migration, rather than international migration, for two reasons. First, although international migration is the more widely recognized and lucrative form of migration, a larger proportion of most populations (including those in our study sample) is impacted by internal migration. Second, the concentration of international migration in a small number of provinces prevented the identification of an area of common support in which propensity covariates were balanced across cases with and without international migrant children. In contrast, the covariates of internal migration are readily balanced.
Data and Methods
Data
Data for this study come from the Indonesia Family Life Survey (IFLS), an ongoing panel survey of individuals and households in Indonesia. The first wave of the IFLS (IFLS-1) was conducted in 1993 and contains detailed information regarding economic, demographic, and health measurements. IFLS-1 included 7,224 households from 13 provinces, resulting in a sample population that is broadly representative of 83% of Indonesia’s diverse population (Frankenberg et al. 1995). Provinces were selected in order to “maximize representation of the population, capture the cultural and socio-economic diversity of Indonesia, and be cost-effective to survey given the size and terrain of the country” (Frankenberg and Thomas 2000:4). IFLS-1 sampled individuals within households; while all adults had a probability of being sampled, primacy was given to household heads, their spouses, and household members older than 50 (Frankenberg and Jones 2004). IFLS-2 was conducted in 1997 in all surviving and offshoot households from IFLS-1 (Frankenberg and Thomas 2000). IFLS-2 had a high retention rate, with 94.4% of Round 1 respondents interviewed. IFLS-3, conducted in 2000, achieved similarly high follow-up rates (95.3%) (Frankenberg and Thomas 2000).
We focus on a subset of IFLS respondents who were older than 50 at the time of IFLS-2 and were residing in a rural area at the time of IFLS-1. We restrict the sample to rural populations because economic opportunities tend to be concentrated in urban areas. Migrations from rural areas tend to be oriented around these opportunities, while migrations out of urban areas are more difficult to characterize. This tendency is reflected in higher rates of interhousehold resource transfers between rural elders and their internal migrant children than for urban elders with rural migrant children (Frankenberg and Kuhn 2004).Footnote 1
Our final sample in this study consists of those individuals who (1) resided in a rural household in IFLS-1, (2) were age 46 or older in IFLS-1 (age 50 in IFLS-2), (3) completed the in-depth individual survey as part of IFLS-1, (4) were successfully followed between Rounds 1 and 2, and (5) had either a completed survey in IFLS-3 or were determined to have deceased. Of 3,346 adults aged 46 and older in rural IFLS-1 households, only 3,089 (92.3%) answered the in-depth individual survey, of which 318 (10.3%) died before IFLS-2, leaving 2,771 surviving respondents at the time of IFLS-2. Of those 2,771 respondents, 286 (10.3%) did not have a completed follow-up survey, leaving 2,485 respondents as of IFLS-2. IFLS-3 failed to track or ascertain the survival status of 34 (1.4%) of the remaining sample, leaving a sample of 2,451 adults. Finally, 296 respondents (12.1%) did not have responses to all reported and observed health questions and were therefore excluded, resulting in an analytic sample of 2,155 adults older than age 50 in IFLS-2 who were followed to IFLS-3. Among those who survived, 2,045 had information on their self-reported health, and 2,016 had information on their activities of daily living (ADLs).
Measures
Health Measures
Mortality between Rounds 2 and 3 of the survey is indicated by proxy reports from individuals remaining in the respondent’s house. For respondents surviving to Round 3, we measure health status in two ways: general self-reported health (SRH) status and self-reported ADLs. SRH is a binary variable indicating whether health was poor or fair. Good or excellent SRH is the referent category.Footnote 2 An ADL index measures respondent limitation in eight functional activities: to carry a heavy load; sweep the house; walk 5 kilometers; bow, squat, and/or kneel; dress without help; stand up from a chair; go to the bathroom without help; or stand up from a chair without help.
Migration Measures
Data on children’s migration come from IFLS-2. Internal migrant children are defined as those children who reside within the country, but not within the same district as their parents, ranging from zero to six migrant children.Footnote 3 To calculate propensities for having migrant children, a dummy variable indicates whether a respondent had at least one migrant child versus no migrant children (referent).
Controls
Our multivariate analysis includes controls for age, measured as a continuous variable ranging from 50 to 99; and sex, where female is coded as 1, and male is the referent. To address potential differences between respondents who have few children versus those with many, we control for the total number of children aged 15 and older as the “supply” of children available to provide old-age support. This variable is derived from the IFLS-2 survey reports. Additionally, multivariate models control for both SRH status and ADLs in 1993 to capture the baseline health status of the respondents. Both variables are derived identically to the outcome measures previously described from Round 3 of the IFLS.
Propensity Score Controls
The propensity score equation requires control measures that are well-defined, stable, and have substantial overlap between treatment and control groups (Rosenbaum and Rubin 1983b). First, we include economic factors that may predispose respondents to having migrant children, such as total household assets and net receipt of financial transfers from other households (also an indicator of past migration history). In addition to enabling children’s migration, higher SES is also associated with better health; therefore, it is crucial that respondents are balanced on this measure (VanWey 2004). Assets are calculated in rupiah, converted to $US at 1,800 rupiah/dollar, and converted into deciles based on the overall asset distribution.Footnote 4 Predisposing characteristics of the respondent’s children that may influence the likelihood that a child will migrate are also included: the total number of children aged 15 and older, the number who completed secondary schooling, and the number married (Massey et al. 1999; Mincer 1978; Sjaastad 1962). These measures are derived from data in IFLS-2. The propensity model includes dummy variables for province of origin, as previous work has shown that regional variations in culture and SES result in differential returns from migration (Kreager 2006).
Plan of Analysis
We calculate propensity scores by using the Stata package pscore, developed by Becker and Ichino (2002). A logistic regression model estimates the probability of treatment uptake (D i )—in this case, having a migrant child—based on a series of covariates (X i ) based on the following formula:
where W are measures of prior household wealth and migration history, C are child characteristics (size, composition, human capital), and a series of dummy variables account for province. The resulting propensity score is the predicted probability of treatment.
Then pscore proceeds to identify whether propensity Eq. (1) can be used to balance the pretreatment variables such that exposure to treatment is pseudo-randomized (Becker and Ichino 2002). First, pscore identifies the ACS, which excludes all cases that do not have a suitable counterfactual match (i.e., cases whose propensity is so high that there is no control case with a similar propensity). Cases in the ACS are then divided iteratively into an optimal number of propensity blocks, in which the average propensity of treatment and control cases do not differ statistically. Within each propensity block, the means of all predisposing covariates in X i are tested for differences. If either the propensity score or the covariates are imbalanced (i.e., significantly different) within any of the propensity blocks, the balancing equation has failed, and the study cannot proceed without a new balancing equation. If a set of propensity blocks are identified in which the propensity scores and covariates of treatment and control cases are comparable, we have identified a balanced design.
Having identified an area of common support, a propensity score, and propensity blocks, we proceed to use the three rounds of IFLS data to estimate the effects of children’s migration on health using three approaches. First, we estimate a series of regression models that properly sequence the relationship between prior health, children’s migration, and subsequent health:
where H ij3 can be any of three health outcomes of emphasis in this study for respondent i in community j measured in IFLS-3; \( {\overline {Mig}_{{ij2}}} \) measures the collective migration behavior of the children of respondent i measured in IFLS-2; H ij1 is a control for health status at the time of IFLS-1; and P (\( {\overline {Mig}_{{ij2}}} \)) is an estimate of the propensity for the children of the respondent to migrate. We use OLS to analyze the relationship between migration and ADLs; we use logistic regression to examine the relationship between migration and mortality, migration and SRH, and migration and ADLs. For each outcome, we test models that do not include propensity score adjustments, models that restrict the sample to the ACS, models that use the restricted sample and a linear propensity score term as a control, and models that use a restricted sample and controls for propensity block.
The second analytic approach that we employ is the calculation of the average treatment effect. As stated earlier, the pscore package matches individuals with similar propensities to be in the treatment group (X 1) or the control group (X 0). Using these scores, we can then calculate the “average treatment effect” based on nearest neighbor matching:

,where Y 1 and Y 0 are the potential outcomes in the two counterfactual situations: having a migrant child and not having a migrant child; and Ґ is the average treatment effect of having a migrant child on our dependent variable of interest (mortality, SRH, or ADLs). Matching is our most robust estimator because it is a nonparametric estimate of the relationship between a child’s migration and health (Winship and Morgan 1999). Therefore, the mean difference between these two groups is the effect of a particular treatment on an outcome of interest.
The third approach that we employ is running subclassified multivariate models based on low, medium, and high propensities to have a migrant child. Performing multivariate analyses within subclasses allows us to examine whether the relationship between having a migrant child and health varies by propensity of having said migrant child. Subclasses are derived from the propensity blocks identified by pscore. Because of the small sample sizes in the six propensity blocks, we combined blocks to create high, low, and medium groups. The low propensity group consists of Block 1, or 26% of the population that have the lowest propensity to have a migrant child, of which 10% of respondents had a migrant child. The middle group, or respondents representing the median level of out-migration, corresponds to Blocks 2 and 3; this group makes up 40% of the total sample, and 24% of them have a migrant child. Finally, the high propensity group was constructed from Blocks 4, 5, and 6 to represent groups that have above-average migration rates and propensities. In this group, 34% of the sample is represented, and 55% of respondents have a migrant child.
Results
Descriptive Results
Table 1 presents descriptive statistics. Panel A focuses on variables included in the models measuring the effect of migration on elderly kin’s health, and Panel B describes the variables used to construct the propensity score.
Panel A shows that roughly 5% of the sample died between IFLS-2 and IFLS-3, and 22% of the sample reported being in poor or fair health at the time of IFLS-3. Interestingly, between IFLS-2 and IFLS-3, respondents lost an average of 0.3 of 8 possible points on the ADL index. This table shows that our key independent variable, children’s internal migration, is relatively common among the study population. The average respondent has 0.58 migrant children, of 3.77 adult children on average, and 29.7% of respondents have at least one internal migrant child. Furthermore, there is a significant positive association between children’s migration in 1997 and better parental health outcomes in 2000. Respondents with no migrant children were twice as likely to die between 1997 and 2000 as those with migrant children (6.0% versus 3.3%). Among the survivors, those with migrant children were 19% less likely to report poor SRH than those without migrant children (19.2% versus 23.7%) and also reported 43% fewer ADL limitations (0.20 versus 0.35).
Panel B illustrates the extent to which migration is correlated with a number of predisposing variables that we include in the propensity score equation.Footnote 5 Respondents with at least one migrant child reported more total numbers of children (5.23 versus 3.16), significantly higher percentages of children that completed secondary school and postsecondary school, and higher percentages of married children. Additionally, respondents with migrant children reported greater household assets and net transfers received compared with respondents without migrant children. This suggests that in addition to having fewer assets to begin with, parents with no migrant children also provide more support to family members than they receive. The descriptive table implies that there are important differences between respondents with migrant children and those without for both their health outcomes and their predisposing variables for children’s migration, providing compelling evidence to proceed with the counterfactual analysis.
Propensity Blocks
To address the selection issues illustrated in Table 1, we create a propensity score using the pscore package. The results, in Table 2, show that the “supply” of children older than age 15 (β = .79, p < .001), children that have completed secondary (β = .35, p < .001) or postsecondary schooling (β = .35, p < .001), and the log net remittances (β = .09, p < .001) are positively associated with having a migrant child.Footnote 6 Assets are shown to be another important predictor of migration, but in a more complex fashion. Compared with the lowest asset deciles, migration becomes increasingly likely among higher deciles up to a peak in the fifth decile. Migration has a roughly equal likelihood among the upper deciles and the lowest deciles.
Finally, we observe strong province-level variations in the propensity to migrate. Respondents from West Sumatra, Lampung, Central Java, and Yogyakarta, all lying in close proximity to major urban hubs, have a higher likelihood of migration than the reference region of North Sumatra. As in most societies, regional variation in migration propensity is a potential source of omitted variable bias and further justifies a counterfactual design. After controlling for these factors, we found no significant association between prior health status in IFLS-1, either SRH or ADL, and the likelihood of having migrant children in IFLS-2, and thus do not include these variables in the propensity equation.
As a check on the effectiveness of counterfactual analysis in creating a pseudo-random design, Table 3 shows the mean values of the two most important covariates of children’s migration behavior: prior transfers received in 1993 and total children in 1997. These covariates are organized by the total sample, by the sample inside and outside the ACS, and by propensity blocks. Without propensity score adjustments, there are significant differences between those with and without a migrant child for both variables. The significant differences persist when the sample is limited to the ACS. Looking by propensity block, however, there are no significant differences in the number of children or past transfer receipt in any of the propensity blocks. In other words, although the blocks differ from one another in terms of propensity to migrate and the covariates of migration, the treated and untreated cases in each of these blocks are comparable.
Table 4 provides descriptive information for children’s migration and health outcomes by the full sample, the ACS, and propensity block. The ACS, identified by pscore, includes individuals with propensities to have a migrant child that range from 0.02 to 0.99, or 2,033 of the 2,155 initial respondents (94.3% of the original sample). The 122 cases outside the area of common support have very low migration propensity: only 5.7% had a migrant child compared with 33.6% inside the ACS. Within the ACS, Block 1—the low propensity block—is the largest, consisting of 25% of respondents. Block 6, the high propensity block, is the smallest treatment block, with 9% of respondents. The average proportion having an internal migrant child ranges from 5.9% in Block 1 to 90.3% in Block 6. The average number of migrant children (the dosage) ranges from just 0.07 in Block 1 to 2.72 in Block 6.
Panel B of Table 4 illustrates the variations in health outcomes across propensity blocks. Roughly 5% of all respondents died, but 7.4% of those outside the ACS died. Within the area of common support, the eventual likelihood of mortality was much lower in the two highest propensity blocks—3.5% in Block 5, and 3.2% in Block 6—than in the lower four blocks (which range from 4.4% to 6.7%). For the two SRH measures in 2000, no clear pattern emerges with respect to variation between treatment blocks. With respect to ADL limitations, however, the number of limitations is higher among respondents lying outside the ACS than those inside. Taken together, these patterns suggest that the returns of child’s migration to elderly kin’s health are differentially associated with the propensity to have a migrant child.
Multivariate Analysis
Having identified an ACS and propensity measures, we proceed to model mortality between IFLS-2 and IFLS-3, and both SRH and ADLs in IFLS-3, using a multivariate approach. Health results are vulnerable to the effects of differential mortality bias, as survival to IFLS-3 was considerably higher for the group with migrant children. The effect of this bias, however, would be to reduce the size and significance of our estimates.
Table 5 shows base models of migration-health relationships for the full sample, without controlling for the propensity to have a migrant child. For each variable, the columns indicate models using the any migrant children dummy variable or a count of the number of migrant children as the independent variable. In all cases, migrant children are associated with a reduced risk of negative health outcomes. We also find that health deteriorates with older age. Women have a slightly greater risk of poor health (significant only for ADL limitations) but a significantly lower risk of mortality. The total number of children older than age 15 has a mild negative association with poor SRH but is not associated with mortality or ADL limitations. Controls for prior health status operate in the expected fashion; past limitations predict future limitation and mortality.
Table 6 demonstrates the impact of introducing a counterfactual approach to the observed associations between migration and the three health outcomes. We report the effects of child’s migration using two different measures: a dummy variable for any migrant child, and the number of migrant children. Model 1 reintroduces the unadjusted coefficients from Table 5. Models 2–4 restrict the analysis to the ACS. For those respondents in the area of common support, Model 3 adds a control variable indicating the predicted propensity to have a migrant child, and Model 4 adds a series of dummy variables indicating the respondent’s propensity block. The final column presents the average treatment effect. All models include the same controls for demographic factors and prior health status shown in Table 5.
Panel A of Table 6 shows that propensity adjustments have little impact on the magnitude of the migration-mortality association, but they do affect the level of significance. Restricting the sample to the ACS reduces the impact of any migrant child by only 5% and 3% for the number of migrant children. This restriction, however, reduces the significance of the effect of any migrant children from the p < .05 level of significance to the p < .10 level. Similarly, adjustments for propensity score and block have little impact on the magnitude of the migrant child coefficients but lead to further increases in the standard error of the migration estimates, thereby reducing the level of significance of the effects. The calculated average treatment effect suggests a 4% reduction in mortality for those with a migrant child (p < .10).
Panel B of Table 6 demonstrates the substantial impact of propensity score adjustments on the association between migration and poor SRH. Restricting the sample to the ACS reduces the magnitude of coefficients for any migrant child and number of migrant children by 8% and 6%, respectively. Adjustments for propensity score and propensity block have a more substantial impact on the association, accounting for about a 30% reduction in the coefficient for any migrant children compared with the unadjusted model and a 40% reduction in the effect of the number of migrant children. To summarize, Model 1 suggests that respondents with migrant children have 35% lower odds of reporting poor SRH in the next three years than those without; however, restricting the sample to the ACS and controlling for propensity score indicates a more conservative reduction of 23%. More importantly, coefficients and the average treatment effect for both measures of migration fall well below the level of statistical significance.
Panel C of Table 6 finds that propensity corrections have little impact on the association between migration and ADL limitations. On average, the corrections reduce the impact of children’s migration by roughly 10%. The relationship between any migrant children and ADLs, however, remains significant at the p < .05 level. This result suggests that the impact of migration on ADLs does not vary by propensity to migrate. Indeed, although migration reduces disability, this does not mean that those selecting themselves into migration are necessarily those who would benefit most from migration. The average treatment effect shows that the ADL scale is reduced by 0.15 points for those with a migrant child and is significant at the p < .05 level.
Propensity Block Analysis
Table 7 presents the results of subclassified models of mortality, SRH, and ADLs for respondents in the low, medium, and high migration propensity groups. These models allow us to examine whether those with higher migration propensities benefit more from migration than those with low propensities. These models include all control variables included in previous models as well as dummy variables for propensity block for the medium and high groups, which include more than one block. Panel A of Table 7 shows that the effect of any migrant child and number of migrant children on mortality is negative in all propensity groups. The effect sizes are much larger and statistically significant only for the high propensity group.Footnote 7 In other words, those respondents with the highest propensity to have migrant children are also those who benefit most in terms of improved survival.
Figure 1 summarizes the substance of these effects for mortality outcomes. What emerges is a strong overall mortality gradient between the low, medium, and high propensity blocks. The calculated probability of dying is twice as high in the low propensity group as in the high propensity group.Footnote 8 This does not reflect, however, a tendency for those in the high propensity group to be better off, irrespective of whether they have migrant children. On the contrary, elders who lack migrant children have comparable levels of mortality, irrespective of their propensity group. The overall mortality advantage of the high propensity group is driven instead by the two-thirds reduction in mortality risk for those with migrant children relative to those without. The gap between the low and medium propensity groups, however, is driven primarily by the tendency for the former group to have higher mortality, irrespective of children’s migration status. From a counterfactual standpoint, the medium propensity group would have the best health outcomes in the absence of migration, but migration allows the high propensity group to surpass them.
Panel B of Table 7 suggests a different pattern of SRH by propensity status. The negative association between children’s migration and poor SRH appears to hold only for those in the middle propensity block. Figure 2 summarizes the relationship between children’s migration and the probability of reporting poor SRH for the three propensity groups. Levels of SRH exhibit a mild gradient running from low to high propensity, with the low propensity group reporting substantially worse SRH (27% poor) than either the medium (21%) or high (19%) groups. In the absence of migration, the middle group, which benefited most from migration in terms of SRH, would look more similar to the low propensity group than the high propensity group. In other words, the benefits of migration for the medium propensity group merely serve to narrow the gap between the medium and the high propensity group. It is important to keep in mind, however, the potential role of mortality selection in these results. Higher rates of mortality among the medium propensity group may have left behind a more robust group of survivors than in the high propensity group.
Panel C of Table 7 examines the link between migration and ADLs and reveals a similar pattern to the child’s migration-SRH analysis. The benefits of children’s migration for reducing ADL limitations are largely concentrated in the middle propensity group. The importance of group-specific analysis is particularly striking in this case. Figure 3 summarizes the relationship between migration and ADL limitations for each propensity group. When respondents both with and without migrant children are grouped together, there appears to be a gradient, with the high propensity group having the fewest limitations. Further, when the analysis is disaggregated by whether respondents have a migrant child, we see that those persons in the middle propensity group who have a migrant child are better off than any other group. Without the benefit of migration, the medium propensity group would have had no fewer, and perhaps more, ADL limitations than the low propensity group. Conversely, those respondents in the low propensity group appear to suffer a health penalty by having a migrant child. Indeed, those respondents in the low category with a migrant child have substantially higher predicted ADL limitations than those without, providing compelling evidence that the benefits of migration are concentrated within specific subgroups.
Discussion and Conclusion
The interaction between migration and population aging has generated concern over the well-being of elderly persons in rural areas of LDCs, where institutional care mechanisms cannot substitute for children who have migrated to urban areas. The results in this article do not confirm these fears. Instead, they corroborate past work that has found positive effects of children’s migration on the health of left-behind parents. We improve upon earlier work by using a longitudinal design and a counterfactual framework to examine whether these returns are differentially associated with the propensity to have a migrant child. We take advantage of the counterfactual approach in three ways: by controlling for propensity, calculating an average treatment effect, and performing subclassified analysis. Although migration decisions are embedded in an array of predisposing factors that make elders with migrant children differ from those without migrant children, we nonetheless found sufficient overlap to identify an area of common support covering 94% of our sample, including individuals with a predicted propensity ranging from 2% to 99%.
We find that propensity accounts for some of the positive association between migration of children and the subsequent health of elders. The effect of children’s migration was relatively robust for the outcome of mortality, highly robust for limitations in ADLs, but considerably less robust for SRH. At minimum, we confirm that children’s migration does not diminish elderly kin’s health in rural areas—an important finding in itself. If our estimates are unbiased, they imply a mortality reduction attributable to children’s migration of about 3.6 percentage points, or from 6% mortality risk over a three-year follow-up period for those without migrant children to a 2.4% risk for those with migrant children. For a population in which 30% of elders have migrant children, this implies a 1.2-percentage-point reduction in population mortality attributable to children’s migration, or about a 20% reduction in total mortality risk associated with children’s migration.
We also measure the differential effects of children’s migration on the health of left-behind elders across propensity groups. For each measure of health, we find that the benefits of migration principally accrued to those with higher migration propensities. For all health outcomes, those in the lowest propensity group saw no health benefits from their children’s moves. For SRH outcomes, migration provided the greatest benefit to those with a moderate propensity to have migrant children, but the high propensity group nonetheless performed better overall on all outcome measures. In the case of mortality, benefits primarily accrued to the high propensity group.
How do we reconcile the substantial health returns to children’s migration for the medium propensity group with their continued mortality disadvantage relative to the high propensity group? First, mortality is a more distant outcome than morbidity. It is therefore not surprising that mortality would be the outcome in which the high propensity group saw its greatest advantage. Second, all models controlled for prior health status. Our results therefore reflect only the further benefits of migration as of 1997 on health through 2000, meaning that the high propensity group may have already accrued substantial health benefits that are controlled out of our models.
The question of accumulated benefit raises a key limitation of this and other migration impact studies: namely, that we measure current migration status rather than new migration episodes. Although our research design is longitudinal and lends itself to the sequential identification of predisposing characteristics, treatments, and outcomes, we do measure current migration status, which is a combination of new and preexisting migration episodes, rather than looking only at new episodes. However, in Indonesia, as in most populations, the relative infrequency of new migration episodes initiating over a four-year time window would provide insufficient statistical power for measuring health variations.
A second limitation of our study relates to the remaining sources of selectivity not captured in our model. First, our results may be influenced by attrition bias because our full sample is restricted to persons who survived between IFLS-1 and IFLS-2, and our SRH and ADL analyses are further restricted to those who survived to IFLS-3. We may therefore, at the outset, have lost a proportion of the population in the worst health. Furthermore, our results cannot account for unobserved sources of self-selection as thoroughly as would a randomized controlled study. Future studies will face the difficulty of identifying an area of common support for treatments with less overlap in their covariates, including international migration in the Indonesian context.
Nonetheless, our findings add to the growing body of evidence on positive health impacts of migration for the left-behind by introducing a causal framework and addressing differential impacts by propensity group. They force us to consider the complex role of migration in emerging adult health disparities in many LDCs in several ways. First, the health advantage gained by elders with migrant children, compared with those without, is itself a form of health disparity. Recent research has found a relatively limited empirical association between traditional measures of socioeconomic status (i.e., wealth, education) and mortality in many LDCs (Liang et al. 2001; Zimmer et al. 2004; Zimmer and Martin 2007). We thus might argue that migration is the single greatest source of health disparity among the rural elderly in many LDCs and deserves considerably greater attention in national reporting.
Second, the health benefits of migration do not accrue equally to all elders, with significantly greater benefits for high propensity groups and no benefits for low propensity groups. To be clear, we are not saying that migration exacerbates preexisting health disparities, as mere membership in the high propensity group accords no health benefits to elders. Instead, we are stating that contingent on children’s migration, those in the high propensity group will benefit more than others. To complicate things further, our propensity groups do not coincide with any easily identifiable socioeconomic or class distinction, despite the inclusion of a number of socioeconomic factors—such as family size, education, and province of origin—in our propensity equation. Finally, we must recognize that as the migration process unfolds over time and through the gradual accumulation of migration-specific social capital across communities and networks, health benefits could accrue to low propensity elders, either through increased migration or through changes in the economy or health system driven indirectly by the migration process (Kuhn 2003; Massey et al. 1999).
In the meantime, we must recognize that migration is a powerful determinant of health, but not a panacea for emerging health needs in LDCs. Migration has only limited potential to address the health needs of all elders. Separate evidence suggests that migration may be less beneficial, or even detrimental, to the health of the left-behind spouses and children of migrants (Asis and Baggio 2003; Battistella and Gastardo-Conaco 1998; Roy and Nangia 2003). Future research must more specifically address the barriers in the migration process that make it both less common and less beneficial for some. Such work could point the way to the development of social or financial markets that can mitigate the risks and spread the benefits of the migration to have a greater impact on rural health. Innovative programs—such as migration insurance, rotating migration credit circles, and remittance investment funds—could allow migration to reach its true potential by extending its impact from solely helping immediate families to improving whole communities and health systems.
Notes
Our results for rural respondents hold for urban areas, although models that combine both rural and urban populations tend to be driven by the rural results.
The four-category general health question yielded little variation between the poor versus nonpoor dichotomy. In the study group, 95% of respondents were either “somewhat healthy” or “somewhat unhealthy,” 4% were unhealthy, and 1% were healthy.
The term district refers to the kabupaten, or regency: the unit of government below province.
Deciles cover the following ranges in U.S. dollars: 0–225; 227–588; 589–1,000; 1,009–1,506; 1,507–2,197; 2,203–3,069; 3,072–4,466; 4,470–6,714; 6,769–12,608; 12,667–42,000.
For child characteristics, we use data from IFLS-2 (1997) to ensure comparability to our independent migration variable, which is calculated from IFLS-2. For household asset variables, we use data from IFLS-1 (1993) to capture socioeconomic predisposition over a longer time span.
Separate counts for male and female children were not included because they did not improve model fit. This conforms with previous research, suggesting that male and female migration patterns are comparable in this population (Frankenberg and Kuhn 2004).
While statistical power is limited in our low propensity block, with only 56 treatment cases of 560 total, the effects are well below the level of statistical significance.
These are predicted probabilities derived from separate models; thus, the results are not directly comparable.
References
Abraido-Lanza, A. F., Dohrenwend, B. P., Ng-Mak, D. S., & Turner, J. B. (1999). The Latino mortality paradox: A test of the ‘salmon bias’ and healthy migrant hypotheses. American Journal of Public Health, 89, 1543–1548.
Acosta, P. (2006). Labor supply, school attendance, and remittances from international migration: The case of El Salvador (Policy Research Working Paper No. 3903). World Bank, Washington, DC.
Aiken, L. H., Smith, H. L., & Lake, E. T. (1994). Lower medicare mortality among a set of hospitals known for good nursing care. Medical Care, 32, 771–787.
Antman, F. M. (2008). Who cares for the elderly? Intrafamily resource allocation and migration in Mexico (Working Paper No. 08-01). Boulder, CO: Department of Economics, University of Colorado at Boulder.
Asis, M. M. B. (2006). Living with migration: Experiences of left-behind children in the Philippines. Asian Population Studies, 2, 45–67.
Asis, M. M. B., & Baggio, F. (2003, September). The other face of migration: Children and families left behind. Paper presented at the 8th International Metropolis Conference, Vienna, Austria.
Battistella, G., & Gastardo-Conaco, M. C. G. (1998). The impact of labor migration on the children left behind: A study of elementary school children in the Philippines. Sojourn, 13, 220–241.
Beard, V. A., & Kunharibowo, Y. (2001). Living arrangements and support relationships among elderly Indonesians: Case studies from Java and Sumatra. International Journal of Population Geography, 7, 17–33.
Becker, S., & Ichino, A. (2002). Estimation of average treatment effects based on propensity scores. The Stata Journal, 2, 358–377.
Bhrolcháin, M. N. (2001). ‘Divorce effects’ and causality in the social sciences. European Sociological Review, 17, 33–57.
Borjas, G. J. (1987). Self-selection and the earnings of immigrants. The American Economic Review, 77, 531–553.
Brown, C. (2003). A short history of Indonesia: The unlikely nation? Crows Nest: Allen and Unwin.
Chang, T. P. (1992). Implications of changing family structures on old-age support in the ESCAP Region. Asia-Pacific Population Journal, 7(2), 49–66.
Cochran, W. G. (1968). The effectiveness of adjustment by subclassification in removing bias in observational studies. Biometrics, 24, 295–313.
Curran, S. R. (2002). Migration, social capital, and the environment: Considering migrant selectivity and networks in relation to coastal ecosystems. Population and Environment: Methods of Analysis, Population and Development Review, 28(Suppl.), 89–125.
Curran, S. R., & Rivero-Fuentes, E. (2003). Engendering migrant networks: The case of Mexican migration. Demography, 40, 289–307.
Curran, S. R., & Saguy, A. C. (2001). Migration and cultural change: A role for gender and social networks? Journal for International Women’s Studies, 2(3), 54–77.
Cutler, D., Deaton, A., & Lleras-Muney, A. (2006). The determinants of mortality. The Journal of Economic Perspectives, 20(3), 97–120.
DaVanzo, J., & Chan, A. (1994). Living arrangements of older Malaysians: Who coresides with their adult children. Demography, 31, 95–113.
Diaz, J. J., & Handa, S. (2006). An assessment of propensity score matching as a nonexperimental impact estimator: Evidence from Mexico’s PROGRESA program. The Journal of Human Resources, XLI, 319–345.
Duncan, G., Huston, A., & Weisner, T. (2007). Higher ground: New hope for the working poor and their children. New York: Russell Sage Foundation.
Frank, R., & Hummer, R. A. (2002). The other side of the paradox: The risk of low birth weight among infants of migrant and nonmigrant households within Mexico. International Migration Review, 36, 746–765.
Frankenberg, E., & Thomas, D. (2000). The Indonesia Family Life Survey (IFLS): Study design and results from Waves 1 and 2. Santa Monica: RAND.
Frankenberg, E., & Jones, N. R. (2004). Self-rated health and mortality: Does the relationship extend to a low income setting? Journal of Health and Social Behavior, 45, 441–452.
Frankenberg, E., & Kuhn, R. S. (2004). The role of social context in shaping intergenerational relations in Indonesia and Bangladesh. Annual Review of Gerontology & Geriatrics, 24, 177–198.
Frankenberg, E., Karoly, L. A., Gertler, P., Achmad, S., Agung, I. G., Hatmadji, S. H., & Sudharto, P. (1995). The 1993 Indonesian Family Life Survey: Overview and field report. Santa Monica: RAND.
Frankenberg, E., Beegle, K., Sikoki, B., & Thomas, D. (1999). Health, family planning and wellbeing in Indonesia during an economic crisis: Early results from the Indonesian Family Life Survey (Labor and Population Program Working Paper Series 99-06). Santa Monica, CA: RAND.
Frankenberg, E., Lillard, L., & Willis, R. J. (2002). Patterns of intergenerational transfers in Southeast Asia. Journal of Marriage and Family, 64, 624–641.
Gum, P. A., Thamilarasan, M., Watanabe, J., Blackstone, E. H., & Lauer, M. S. (2001). Aspirin use and all-cause mortality among patients being evaluated for known or suspected coronary artery disease: A propensity analysis. Journal of the American Medical Association, 286, 1187–1194.
Guo, M., Chi, I., & Silverstein, M. (2009). Intergenerational support of Chinese rural elders with migrant children: Do sons’ or daughters’ migrations make a difference? Journal of Gerontological Social Work, 52, 534–554.
Hadi, A. (1999). Overseas migration and the well-being of those left behind in rural communities of Bangladesh. Asia-Pacific Population Journal, 14(1), 43–58.
Ham, J. C., Li, X., & Reagan, P. B. (2004). Propensity score matching, a distance-based measure of migration, and the wage growth of young men (IEPR Working Paper No. 05.13). Los Angeles, CA: Institute of Economic Policy Research, University of Southern California.
Hermalin, A. I. (2002). The well-being of the elderly in Asia: A four-country comparative study. Ann Arbor: University of Michigan Press.
Hill, H. (1995). Indonesia’s great leap forward? Technology development and policy issues. Bulletin of Indonesian Economic Studies, 31(2), 83–123.
Hill, H. (1996). The Indonesian economy since 1966: Southeast Asia’s emerging giant. Cambridge: Cambridge University Press.
Hugo, G. J. (1982). Circular migration in Indonesia. Population and Development Review, 8, 59–84.
Hummer, R. A., Rogers, R. G., Nam, C. B., & LeClere, F. B. (1999). Race/ethnicity, nativity, and U.S. adult mortality. Social Science Quarterly, 80, 136–153.
Huston, A. C., Duncan, G. J., McLoyd, V. C., Crosby, D. A., Ripke, M. N., Weisner, T. S., & Eldred, C. A. (2005). Impacts on children of a policy to promote employment and reduce poverty for low-income parents: New hope after 5 years. Developmental Psychology, 41, 902–918.
Jasso, G., Massey, D. S., Rosenzweig, M. R., & Smith, J. P. (2004). Immigrant health: Selectivity and acculturation. In N. B. Anderson, R. A. Bulatao, & B. Cohen (Eds.), Critical perspectives on racial and ethnic differences in health in late life (pp. 227–266). Washington, DC: National Academies Press.
Joffe, M. M., & Rosenbaum, P. R. (1999). Invited commentary: Propensity scores. American Journal of Epidemiology, 150, 327–333.
Kabir, Z. N., Szebehely, M., Tishelman, C., Chowdhury, A. M. R., Hojer, B., & Winbland, B. (1998). Aging trends––Making an invisible population visible: The elderly in Bangladesh. Journal of Cross-Cultural Gerontology, 13, 361–378.
Kalache, A., & Sen, K. (1998). Ageing in developing countries, principles and practice of geriatric medicine. Chichester: Wiley.
Kanaiaupuni, S. M., & Donato, K. M. (1999). Migradollars and mortality: The effects of migration on infant survival in Mexico. Demography, 36, 339–353.
Kanaiaupuni, S. M., Donato, K. M., Thompson-Colón, T., & Stainback, M. (2005). Counting on Kin: Social networks, social support and child health. Social Forces, 83, 1137–1164.
Keasberry, I. N. (2001). Elder care and intergenerational relationships in rural Yogyakarta, Indonesia. Aging and Society, 21, 641–665.
Knodel, J., & Debavalya, N. (1997). Living arrangements and support among the elderly in South-East Asia: An introduction. Asia-Pacific Population Journal, 12(4), 5–16.
Knodel, J. E., & Saengtienchai, C. (2007). Rural parents with urban children: Social and economic implications of migration for the rural elderly in Thailand. Population Space and Place, 13, 193–210.
Kreager, P. (2006). Migration, social structure and old-age support networks: A comparison of three Indonesian communities. Ageing & Society, 26, 37–60.
Kuhn, R. (2003). Identities in motion: Social exchange networks and rural-urban migration in Bangladesh. Contributions to Indian Sociology, 37(1–2), 311–337.
Kuhn, R. (2005). A longitudinal analysis of health and mortality in a migrant-sending region of Bangladesh. In S. Jatrana, M. Toyota, & B. S. A. Yeoh (Eds.), Migration and health in Asia (pp. 318–357). London: Routledge.
Kuhn, R. (2006). The effects of fathers’ and siblings’ migration on children’s pace of schooling in a migrant-sending region of Bangladesh. Asian Population Studies, 2, 69–92.
Liang, J., Liu, X., & Gu, S. (2001). Transitions in functional status among older people in Wuhan, China: Socioeconomic differentials. Journal of Clinical Epidemiology, 54, 1126–1138.
Lieberson, S. (1987). Making it count: The improvement of social research and theory. Berkeley: University of California Press.
Lieberson, S. (1991). Small N’s and big conclusions: An examination of the reasoning in comparative studies based on a small number of cases. Social Forces, 70, 307–320.
Link, B. G., & Phelan, J. (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, 35, 80–94.
Little, R. J., & Rubin, D. B. (2000). Causal effects in clinical and epidemiological studies via potential outcomes: Concepts and analytical approaches. Annual Review of Public Helath, 21, 121–145.
Marini, M. M., & Singer, B. (1988). Causality in the social sciences. Sociological Methodology, 18, 347–409.
Marmot, M. G., Adelstein, A. M., & Bulusu, L. (1984). Lessons from the study of immigrant mortality. Lancet, 1, 1455–1457.
Massey, D. S. (1988). Economic development and international migration in comparative perspective. Population and Development Review, 14, 383–413.
Massey, D. S. (1990). Social structure, household strategies, and the cumulative causation of migration. Population Index, 56, 3–26.
Massey, D. S. (1999). International migration at the dawn of the twenty-first century: The role of the state. Population and Development Review, 25, 303–322.
Massey, D. S., Arango, J., Hugo, G., Kouaouci, A., Pellegrino, A., & Taylor, J. E. (1999). Worlds in motion: Understanding international migration at the end of the millennium. New York: Oxford University Press.
McKenzie, D., & Hildebrandt, N. (2005). The effects of migration on child health in Mexico. Economia, 6, 257–289.
McKenzie, D., Gibson, J., & Stillman, S. (2010). How important is selection? Experimental vs. non-experimental measures of the income gains from migration. Journal of the European Economic Association, 8, 913–945.
McMichael, A. J. (1999). Prisoners of the proximate: Loosening the constraints on epidemiology in an age of change. American Journal of Epidemiology, 149, 887–897.
Miech, R. A., Caspi, A., Moffitt, T. E., Entner, B. R., Wright, P., & Silva, A. (1999). Low socioeconomic status and mental disorders: A longitudinal study of selection and causation during young adulthood. The American Journal of Sociology, 104, 1096–1131.
Mincer, J. (1978). Family migration decisions. Journal of Political Economy, 8, 749–773.
Nguyen, L., Yeoh, B. S. A., & Toyota, M. (2006). Migration and the well-being of the ‘left behind’ in Asia. Asian Population Studies, 2, 37–44.
Nyberg-Sørensen, N., Van Hear, N., & Engberg-Pedersen, P. (2002). The migration-development nexus evidence and policy options state-of-the-art overview. International Migration, 40(5), 3–47.
Ozden, C., & Schiff, M. (2007). International migration, economic development and policy. New York and Washington, DC: Palgrave Macmillan and World Bank.
Palloni, A., & Arias, E. (2004). Paradox lost: Explaining the Hispanic adult mortality advantage. Demography, 41, 385–415.
Palloni, A., & Morenoff, J. D. (2001). Interpreting the paradoxical in the Hispanic paradox: Demographic and epidemiologic approaches. Annals of the New York Academy of Sciences, 954, 140–174.
Portes, A., & Sensenbrenner, J. (1993). Embeddedness and immigration: Notes on the social determinants of economic action. The American Journal of Sociology, 98, 1320–1350.
Quinn, M. A., & Rubb, S. (2005). The importance of education-occupation matching in migration decisions. Demography, 42, 153–167.
Raftery, A. E. (2001). Statistics in sociology, 1950–2000: A selective review. Sociological Methodology, 31, 1–45.
Rahman, M. O. (1999). Age and gender variation in the impact of household structure on elderly mortality. International Journal of Epidemiology, 28, 485–491.
Rahman, M. O. (2000). The impact of co-resident spouses and sons on elderly mortality in rural Bangladesh. Journal of Biosocial Science, 32, 89–98.
Rahman, M. O. (2001). Living arrangements and the health of older persons in developing countries: Evidence from rural Bangladesh. Population Bulletin of the United Nations: Ageing and Living Arrangements of Older Persons. Critical Issues and Policy Responses. Special Issue Nos. 42/43:330–47. New York: United Nations.
Rahman, M. O., Menken, J., & Kuhn, R. (2004). The impact of family members on the self-reported health of older men and women in a rural area of Bangladesh. Ageing and Society, 24, 903–920.
Rogers, R. G., Hummer, R. A., & Nam, C. B. (2000). Living and dying in the USA: Behavioral, health, and social differences in adult mortality. New York: Academic Press.
Rosenbaum, P. R., & Rubin, D. B. (1983a). Assessing sensitivity to an unobserved covariate in an observational study with binary outcome. Journal of the Royal Statistical Society, 45, 212–218.
Rosenbaum, P. R., & Rubin, D. B. (1983b). The central role of the propensity score in observational studies for causal effects. Biometrika, 70, 41–55.
Rosenbaum, P. R., & Rubin, D. B. (1984). Reducing bias in observational studies using subclassification on the propensity score. Journal of the American Statistical Association, 79, 516–524.
Roy, A. K., & Nangia, P. (2003). Reproductive health status of left behind women of male outmigrants: A study of rural Bihar, India. In S. Jatrana, M. Toyota, & B. S. A. Yeoh (Eds.), Migration and health in Asia (pp. 209–241). London: Routledge.
Rubin, D. B. (1974). Estimating the causal effects of treatment in randomized and nonrandomized studies. Journal of Educational Psychology, 66, 688–701.
Rubin, D. B. (1977). Assignment to treatment group on the basis of a covariate. Journal of Educational Statistics, 2, 1–26.
Seeman, T. E., Charpentier, P. A., Berkman, L. F., Tinetti, M. E., Guralnik, J. M., Albert, M., & Rowe, J. W. (1994). Predicting changes in physical performance in a high-functioning elderly Cohort: MacArthur studies of successful aging. Journal of Gerontology, 49, M97–M108.
Sjaastad, L. A. (1962). The costs and returns of human migration. Journal of Political Economy, 70, 80–93.
Sobel, M. E. (2000). Causal inference in the social sciences. Journal of the American Statistical Association, 95, 647–651.
Sorlie, P. D., Backlund, E., Johnson, N. J., & Rogot, E. (1993). Mortality by hispanic status in the United States. Jounral of the American Medical Association, 270, 246–248.
Speare, A., Jr., & Harris, J. (1986). Education, earnings, and migration in Indonesia. Economic Development and Cultural Change, 34, 223–244.
Stark, O., & Bloom, D. E. (1985). The new economics of labor migration. The American Economic Review, 75, 173–178.
Stone, R. A., Obrosky, D. S., Singer, D. E., Kapoor, W. N., Fine, M. J., & the Pneumonia Patient Outcomes Research Team (PORT) Investigators. (1995). Propensity score adjustment for pretreatment differences between hospitalized and ambulatory patients with community-acquired pneumonia. Medical Care, 33, AS56–AS66.
Sturmer, T., Joshi, M., Glynn, R. J., Avorn, J., Rothman, K. J., & Schneeweiss, S. (2006). A review of the application of propensity score methods yielded increasing use, advantages in specific settings, but not substantially different estimates compared with conventional multivariate methods. Journal of Clinical Epidemiology, 59, 437–447.
Taylor, E. G. (1999). The new economics of labour migration and the role of remittances in the migration process. International Migration, 37(1), 63–88.
Toyota, M., Yeoh, B. S., & Nguyen, L. (2007). Bringing the ‘left behind’ back into view in Asia: A framework for understanding the ‘migration-left behind nexus.’ Population, Space, and Place, 13, 157–161.
VanWey, L. K. (2004). Altruistic and contractual remittances between male and female migrants and household in rural Thailand. Demography, 41, 739–756.
Wingate, M. S., & Alexander, G. R. (2006). The healthy migrant theory: Variations in pregnancy outcomes among US-born migrants. Social Science & Medicine, 62, 491–498.
Winship, C., & Morgan, S. L. (1999). The estimation of causal effects from observational data. Annual Review of Sociology, 25, 659–706.
Wong, R., Palloni, A., & Soldo, B. J. (2007). Wealth in middle and old age in Mexico: The role of international migration. International Migration Review, 41, 127–151.
Zimmer, Z., & Martin, L. G. (2007). Key topics in the study of older adult health in developing countries that are experiencing population aging. Journal of Cross-Cultural Gerontology, 22, 235–241.
Zimmer, Z., Chayovan, N., Lin, H.-S., & Natividad, J. (2004). How indicators of socioeconomic status relate to physical functioning of older adults in three Asian societies. Research on Aging, 26, 224–258.
Acknowledgment
This research was supported by National Science Foundation Grant 0422976. Additional support came from National Institute on Aging Grant R03AG19294-01A1 and NIA Grant 5P30AG017248-02. The authors thank Richard Rogers, Francisca Antman, Ying Lu, and Steve Stillman for their helpful advice; Jarron Saint Onge, Kunga Lama, and Yaffa Truelove for research assistance; Christine Peterson and the IFLS Support Team for data assistance; and Graham Smith and Andrew Linke for editorial assistance. An earlier version of this article was presented at the annual meeting of the Population Association of America in New York in March 2007.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuhn, R., Everett, B. & Silvey, R. The Effects of Children’s Migration on Elderly Kin’s Health: A Counterfactual Approach. Demography 48, 183–209 (2011). https://doi.org/10.1007/s13524-010-0002-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13524-010-0002-3