Abstract
Background
Cancer stem cells (CSCs) are regulated by several signaling pathways that ultimately control their maintenance and expansion. NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) forms a protein complex that controls DNA transcription and, as such, plays an important role in proliferation, inflammation, angiogenesis, invasion and metastasis. The NF-κB signaling pathway, which has been found to be constitutively activated in CSCs from a variety of cancers, participates in the maintenance, expansion, proliferation and survival of CSCs. Targeted disruption of this pathway may profoundly impair the adverse phenotype of CSCs and may provide a therapeutic opportunity to remove the CSC fraction. In particular, it may be attractive to use specific NF-κB inhibitors in chronic therapeutic schemes to reduce disease progression. Exceptional low toxicity profiles of these inhibitors are a prerequisite for use in combined treatment regimens and to avoid resistance.
Conclusion
Although still preliminary, recent evidence shows that such targeted strategies may be useful in adjuvant chemo-preventive settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
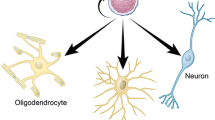
Cancer stem cells (CSCs) are thought to initiate and sustain tumor growth, including the formation and propagation of metastatic foci at distant sites [1–3]. According to this paradigm, only CSCs are able to self-renew indefinitely and to differentiate into various cell types, whereas other cells within a tumor cannot [4]. CSCs have three main properties: 1) the capacity to initiate tumors and to drive neoplastic proliferation, 2) the ability to produce unlimited copies of themselves through self-renewal and 3) the potential to give rise to more differentiated progeny. CSCs can evolve from normal stem cells (NSCs), since these cells are prone to accumulate mutations due to their long lifespan. CSCs can also arise from restricted progenitor or differentiated cells by genetic or epigenetic alterations that activate self-renewal mechanisms and allow them to acquire a CSC phenotype [5]. In this review, after briefly summarizing the basic knowledge of NF-κB signaling and its role in cancer, we will describe the most relevant recent findings of this signaling cascade in the regulation of the CSC phenotype, and possible ways to harness this knowledge for therapeutic purposes.
2 The NF-κB signaling pathway
NF-κB refers to a family of transcription factors that controls the expression of a large number of genes related to immune responses, development, survival, proliferation, angiogenesis, invasion and metastasis [6]. This family comprises five transcription factors, i.e., RelA (p65), RelB, c-Rel, NFκB1 (p50/p105) and NFκB2 (p52/p100). RelA (p65), RelB and c-Rel are synthesized as mature proteins. Rel proteins contain a N-terminal Rel homology domain (RHD) essential for dimerization and DNA binding, and a C-terminal transcriptional activation domain (TAD). NFκB1 and NFκB2 are synthesized as long precursors denoted p105 and p100, respectively. p105 and p100 contain a N-terminal RHD and a C-terminal ankyrin repeat domain, which is processed by the proteasome. After proteolysis, p105 and p100 give rise to p50 and p52. Both p50 and p52 contain a RHD, but lack a TAD [6, 7]. NF-κB transcription factors homo- or hetero-dimerize to activate transcription. p65:p50, c-Rel:p50 and RelB:p52 are the most important dimers, since they regulate many cellular and physiological processes. Homo-dimers or hetero-dimers of p50 or p52 can still bind to DNA, but they are unable to activate gene transcription. They act, instead, as transcriptional repressors by blocking the consensus sites of NF-κB [6].
In un-induced cells, specific inhibitors (inhibitors of kB, i.e., IκB) retain NF-κB subunits in the cytoplasmic compartment. p100 and p105 can also act as NF-κB inhibitors, since they contain five to seven ankyrin repeat modules and perform the same cytosolic-retaining function as IκB proteins. IκB interaction masks the nuclear localization sequence in the NF-κB proteins, thus preventing nuclear translocation and activation [6, 7]. NF-κB signaling can be activated in response to a variety of stimuli, including viral or bacterial infection, exposure to pro-inflammatory cytokines, mitogens and growth factors, and to oxidative stress conditions.
There are two main signaling pathways that activate the NF-κB transcriptional activity. The canonical NF-κB pathway mediates rapid and reversible inflammatory and immune responses, whereas the non-canonical NF-κB pathway mediates slow responses during e.g. development [7, 8]. The canonical NF-κB pathway can be activated by many pro-inflammatory factors such as cytokines (IL1β, TNFα), pathogen-associated molecular patterns (PAMPs) and some danger-associated molecular patterns (DAMPs). Upon binding of these factors to their receptors, the IκB kinase (IKK) complex (IKKα, IKKβ and IKKγ) is activated through recruitment of several proteins involved in ubiquitin chain formation. These proteins allow the activation of kinases such as TAK1, which can phosphorylate IKKβ at serine (Ser) 177 and Ser 181, thereby activating it [8]. Once the IKK complex is activated, it phosphorylates IκB proteins (IκBα, IκBβ and IκBε) and triggers their poly-ubiquitination and subsequent degradation by the 26S proteasome. After IκB degradation, NF-κB is released into the nucleus to allow transcriptional activation. RelA and cRel form either homo- or hetero-dimers with p50 to activate the canonical pathway. RelA:RelA, RelA:p50, c-Rel:c-Rel and c-Rel:p50 are the main canonical pathway members [4, 5]. The non-canonical NF-κB pathway is activated by lymphotoxin β (LTβ), CD40 ligand (CD40L), B cell activating factor (BAFF) and receptor activator of NF-κB ligand (RANKL). Activation of the non-canonical pathway requires de novo protein synthesis and stabilization of NIK (NF-κB-interacting kinase), also called MAP3K14. NIK phosphorylates and activates IKK complexes formed by two subunits of IKKα [9]. IKKα and NIK phosphorylate p100, thereby inducing its partial proteolysis, and allow the release of p52/RelB or p52/p65 complexes [10].
3 NF-κB signaling and cancer
The NF-κB signaling pathway plays a major role in tumor biology, since it regulates key processes during the initiation and progression of various types of cancer [11, 12]. Based on the broad range of target genes and tissues involved, NF-κB may be one of the most common regulators of cancer. Direct and indirect effects of this transcription factor complex in tumor initiation and progression have been found using several animal models of e.g. hepatocellular carcinoma, gastric cancer and lung cancer [13, 14]. In most tumors, NF-κB signaling is constitutively active, promoting processes such as proliferation, angiogenesis, invasion, metastasis, chemo-resistance and radio-resistance. This signaling pathway can promote cell growth by inducing the expression of many genes that regulate proliferation, including cyclin D1, D2, D3, cyclin E, CDK2 and c-Myc. Alternatively, NF-κB can promote growth signals through GM-CSF and IL6 [15]. It is also known that inhibition of this pathway impedes the growth of tumor cells and directs them to apoptotic cell death [11, 16]. Additionally, NF-κB can activate the transcription of several genes involved in the suppression of extrinsic and intrinsic apoptosis, such as the inhibitory protein FLIP, BCL2, BclxL and several IAPs [17–19]. Inhibition of apoptosis enables the accumulation of mutated premalignant and malignant cells, allowing the development and progression of cancer. However, it has also been shown that under certain circumstances NF-κB can induce apoptosis and positively regulate pro-apoptotic genes. Thus, NF-κB may have contrasting roles in different tissues, depending on the microenvironment context [15, 16].
NF-κB has also been found to play an important role in the formation of new blood vessels in tumors (angiogenesis) through the production of cytokines such as TNF, IL1, and IL6. These cytokines stimulate the expression of vascular endothelial growth factor (VEGF), which is the primary regulator of angiogenesis. NF-κB can also induce the expression of additional angiogenic regulators such as CXCL1, CXCL8 and IL8. In addition, NF-κB can promote the expression of adhesion molecules such as ICAM-1 and E-selectin and proteins involved in the invasion of tumor cells (metalloproteinases, MMPs) [16, 17, 20]. Additionally, it has been found that NF-κB can promote epithelial-mesenchymal transition (EMT), an event strongly related with invasion and formation of metastatic foci in many types of tumors [21, 22]. Finally, an inflammatory microenvironment, which is largely produced by activation of NF-κB, also contributes to carcinogenesis through cytokine production and the processing of signals that promote tumor growth [23].
4 Activation of NF-κB signaling in cancer stem cells
There is ample evidence showing that constitutive activation of NF-κB signaling participates in the initiation and progression of cancer [24]. More recently, it has been shown that the NF-κB pathway is activated preferentially in the cancer stem cells (CSC) of diverse malignancies, including leukemia, glioblastoma, prostate, ovary, breast, pancreatic and colon cancer [25–31].
5 NF-κB signaling in leukemia
In acute myelogenous leukemia (AML), a subpopulation of leukemic stem cells (LSCs) exhibits constitutive NF-κB activity. Interestingly, normal hematopoietic stem cells (HSCs) and non-LSC lack this activity [25]. In these cells, NF-κB is activated through the canonical pathway, probably by p50 and p65 dimers [25]. p65 is located in the nuclear fraction of LSCs, while it is retained mostly in the cytoplasm in the HSCs [32]. LSCs exhibit increased expression levels of NF-κB-regulated genes (i.e., Tnf, Ncf2, Il15ra, Litaf) compared to HSCs and non-LSC. Differences in the NF-κB status in LSCs versus other cells are mainly due to the high proteasomal activity in these cells, which increases the degradation of the IκBα protein and promotes subsequent NF-κB activation. This phenomenon is consistently observed in different types of AML and it is thought to be maintained by autocrine TNF-α signaling [32]. Since the canonical NF-κB pathway plays an important role in the survival of LSCs [25, 33–35], it represents a potential target for therapeutic intervention to eradicate LSCs while sparing normal HSCs.
6 NF-κB signaling in glioblastoma
Glioblastoma cancer stem cells (GCSs) exhibit constitutive activation of the NF-κB pathway, mainly due to p65 over-expression. STAT3 and p65 bind to adjacent sites in the Notch1 promoter and induce the activation of Notch signaling. STAT3/NF-κB signaling up-regulates the expression of Notch1, Hes5, Jag1, Numb, DTx3 and DVl3, and down-regulates the expression of RBPJ, a negative modulator of Notch signaling [31]. Interactions between the Notch and NF-κB signaling pathways have been observed in several other tissues as well, where increased Notch activation has been found to lead to NF-κB induction and inhibition or down-regulation of Notch1 has been found to lead to decreased NF-κB activity [36]. STAT3/NF-κB/Notch signaling is key to the regulation of self-renewal and survival of GSCs. Interestingly, GSCs harbor a higher number of NFΚBIA deletions compared to non-stem cells. NFΚBIA deletion decreases intracellular levels of the NF-κB inhibitor (IκBα), thereby inducing p65 and activating the NF-κB pathway [37]. In GSCs, activation of the canonical pathway results in an increased expression of NF-κB target genes such as IL8, CXCL11, BCL-2, BCL-X and TRAIL [31]. The expression of pro-inflammatory genes, in turn, activates the canonical NF-κB pathway allowing stem cells to survive and self-renew [38].
The exact role of canonical NF-κB signaling in GSCs remains to be established. NF-κB activation has been reported to promote the acquisition of a pro-inflammatory phenotype [38] and the survival and tumorigenicity of GSCs [39]. However, alternative evidence suggests that the NF-κB pathway is mainly activated during differentiation of GSCs, i.e., NF-κB inhibition has been found to preclude the differentiation of GSC, causing growth arrest and senescence due to the reduction of cyclin D1 levels. [40]. The role of the NF-κB pathway in the differentiation of GSCs needs to be addressed in further detail in order to clarify its function during differentiation.
RelB controls the expression of stem cell-related genes such as Olig2 through activation of the non-canonical NF-κB pathway in GSCs. Both neural progenitor cells and GSCs are known to express Olig2 [41]. It is well-established that activation of the non-canonical pathway promotes survival, motility and invasion of glioblastomas, but the exact role of this pathway in GSCs remains to be elucidated.
7 NF-κB signaling in prostate cancer
Prostate cancer stem cells (PCSCs) over-express genes associated with inflammation, cell adhesion and metastasis, including NF-κB [26] and IL6 [27]. IL6 is a NF-κB target that also activates NF-κB, creating a positive feedback loop that allows constitutive activation of the pathway [26]. Interestingly, IL6 induces the conversion of prostate cancer cells into CSCs in a dose-dependent manner [42]. NF-κB associated proteins are over-expressed in the PCSC fraction [27], and these cells exhibit highly activated PKC and NF-κB pathways, suggesting that PKCα may constitutively activate the NF-κB pathway through phosphorylation of IKKβ [26]. Unlike non-cancer stem cells, PCSCs express low levels of IκBα and show increases in the accumulation of p65 and its acetylated form, p65 (acetyl-K310). Furthermore, p65 is constitutively localized in the nuclei of PCSCs, suggesting that sustained activation of the canonical NF-κB pathway may have functional implications in these cells.
8 NF-κB signaling in ovarian cancer
Ovarian cancer stem cells (OCSC) exhibit a constitutively active NF-κB signaling pathway and a concomitant production of pro-inflammatory cytokines and growth factors such as IL1B, IL6, IL8, MCP-1, MIP-1α, RANTES, GROa, GM-CSF and G-CSF, which are regulated by the NF-κB pathway. These data suggest that OCSCs can create an inflammatory microenvironment through the NF-κB pathway [28, 43]. This pro-inflammatory microenvironment is essential for the support of tumor growth and CSC self-renewal. In line with this, it has been shown that NF-κB inhibition can prevent both tumor growth and enrichment of the stem cell population [43]. Interestingly, OCSCs are able to proliferate even in the presence of effective concentrations of anti-cancer drugs, i.e., administration of paclitaxel and carboplatin to OCSCs induces the activation of NF-κB and enables the proliferation of CD44+ cells, whereas the same treatment in non-stem cells induces an apoptotic response. These results show that OCSCs are resistant to anti-cancer drugs, and that this resistance is partly regulated through NF-κB activation [28]. OCSCs display a stronger metastatic capacity than non-CSCs. These cells express higher levels of chemokines and chemokine receptors such as CCL5, CCR1, CCR3 and CCR5. Noteworthy, CCL5 signaling promotes migration and invasion of OCSCs in an autocrine way through the up-regulation of MMP9 in a NF-κB-dependent manner. CCL5 induces p65 translocation and activation of the NF-κB pathway, thus regulating the metastatic potential of OCSCs [44]. In spite of the important role of the NF-κB pathway in the survival, migration and invasion of OCSCs, little is known about the NF-κB associated factors involved in this regulation. Some evidence indicates that OCSCs express very low levels of miR-199A, a known regulator of IKKβ and the canonical NF-κB pathway and, thus, it seems that the canonical NF-κB pathway is involved in OCSC regulation [28, 45].
OCSCs with a CD44+/VE-cadherin-/CD34- phenotype participate in tumor vascularization through an IKKβ-dependent and VEGF-independent mechanism. These cells have the capacity to differentiate into CD44+/VE-cadherin+/CD34+ endothelial cells. This capacity is unique to the OCSC fraction and, as such, OCSCs can act as vascular progenitors after NF-κB pathway activation [46]. Interestingly, the IKKβ inhibitor bay11-7082 prevents angiogenesis, but has no effect on blood vessel development through normal endothelial cells. These results show that the canonical NF-κB pathway cannot only induce the secretion of pro-angiogenic factors such as IL6, IL8 and VEGF, but can also influence the ability of OCSCs to differentiate and produce endothelial cells, which may contribute to the vascularization of ovarian tumors.
9 NF-κB signaling in breast cancer
The role of NF-κB in CSCs has been studied relatively thoroughly in breast cancer. In these tumors, the CSC population can be identified by the expression of CD44, EpCAM and a low or absent expression of CD24. Several studies have shown that breast CSCs (BCSCs) exhibit a significantly higher NF-κB activity than cells without this phenotype (i.e., CD44-/CD24+) [29, 47]. The NF-κB activity in BCSCs seems to be proportional to the absence of the CD24 protein. It has e.g. been found that exogenous expression of CD24 in CD44+/CD24- BCSCs can inhibit NF-κB signaling, thereby affecting BCSC proliferation. Moreover, it has been found that the expression of CD24 can sensitize BCSCs to apoptosis induction by DNA-damaging anti-cancer drugs [48]. These results suggest that the NF-κB pathway is active in the BCSC fraction and that its activation may confer certain advantages to the CSC population.
In order to elucidate the role of the NF-κB pathway in the biology of BCSCs, Liu et al. employed an IκB super-repressor protein (IκB-SR) that lacks phosphorylation sites for IKKβ and, thereby, prevents NF-κB activation. It was found that IκB-SR over-expression induced a decrease in the proportion of BCSCs in HER2-dependent murine tumors. Likewise, inhibition of NF-κB reduced the formation of mammospheres in non-adherent conditions. This effect was found to be largely due to a reduction in the expression levels of stem cell factors such as Sox2 and Nanog, factors that regulate stem cell populations in many tissues. These results suggest that the NF-κB pathway regulates the expansion of BCSCs in an IKKβ-dependent fashion [49]. Signaling through IKKβ is, however, not the only way to expand BCSCs. In fact, it has been found that mice harboring inactivating IKKα mutations exhibit a delay in tumor development in a HER2-dependent model. Furthermore, cancer cells derived from these tumors showed a significant reduction in the formation of secondary mammospheres, suggesting that also IKKα is a key kinase governing the self-renewal capacity of BCSCs [50]. Recently, it has been shown that IKKα and its activator (NIK) are required for the expansion of CSCs in HER2-induced tumors. The NIK-IKKα cascade acts by phosphorylating and reducing the amount of nuclear p27, a well-known negative regulator of the G1-S cell cycle transition checkpoint, thus restoring CSCs self-renewal capacity in IKKα-deficient mice [51]. Recently, our group has shown that NIK mediates stemness in breast cancer cell lines. We found that shRNA-mediated inhibition of NIK reduced the expression of CSC markers and impaired the clonogenicity and tumorigenesis of these cell lines both in vitro and in vivo. Interestingly, we observed a physical co-localization of aldehyde dehydrogenase (ALDH), a well-known stem cell marker, and the NIK protein in primary breast cancer samples, supporting the relevance of this protein in human breast cancer (unpublished data). Recently, Schramek et al. showed that deletion of IKKα in mammary epithelial cells can affect tumor formation in a murine model induced by a progesterone derivative (MPA). IKKα can be activated by RANKL, thus inducing cell proliferation and expansion of luminal progenitor cells. Interestingly, tumor cells obtained from mice deficient in RANK are unable to form secondary mammospheres. These results indicate that loss of RANK expression affects the ability of CSCs to self-renew [52]. In line with this, exogenous expression of RANK was found to increase the population of (CD44+/CD24low) stem cells and to induce epithelial-mesenchymal transition (EMT) [53]. Recently, it has been shown that inflammation induced by NF-κB activation plays an important role in the maintenance of the BCSC population through an epigenetic mechanism. This mechanism involves the regulation of Lin28B, an inhibitor of microRNA (miRNA) biogenesis, that decreases let-7a miRNA expression which, in turn, regulates IL6 expression. IL6 activates NF-κB, thus forming a positive regulatory circuit. BCSCs express higher levels of Lin28B and lower levels of let-7a compared to non-stem cancer cells [54]. Interestingly, IL6 can also transform non-stem cells into BCSCs [42]. Moreover, it has been found that disruption of IL6 results in a reduction of the CSC population and inhibits tumor growth and metastasis. IL6 is, at least partially, responsible for trastuzumab resistance in breast cancer [55]. Several reports have shown that BCSCs secrete chemokines and cytokines that regulate their maintenance in an autocrine manner. Yamamoto et al. showed that non-stem cells, such as tumor-associated macrophages, tumor-associated fibroblasts [56], and other differentiated cancer cells provide a permissive microenvironment to support the CSC population [57]. Non-stem cells secrete Jagged1 (JAG1), a known ligand of Notch signaling, through NIK-dependent NF-κB activation. Induction of JAG1 was found to result in stimulation of Notch signaling and CSC expansion. Interestingly, the NIK-NFκB-JAG1-Notch1 axis regulates CSC populations only in basal-like breast tumors. NF-κB/TNFα signaling also regulates a stem cell-like phenotype through up-regulation of EMT mediators such as Slug [58] and Twist [22] in breast cancer. Slug and Twist are regulated through canonical NF-κB activation and their expression results in the acquisition of a mesenchymal phenotype. It has been found that induction of EMT in breast cancer cells leads to the acquisition of a stem cell phenotype [59]. NF-κB signaling participates in the induction of EMT, thus promoting mammosphere formation and increasing the invasive capacity of breast cancer cells [21, 22, 58].
Together, these results indicate that the canonical and non-canonical NF-κB pathways cooperate to activate different downstream targets, leading to a high self-renewal ability, a sustained proliferation and survival and tumorigenesis of BCSCs.
10 NF-κB signaling in pancreatic cancer
Pancreatic CSCs are characterized by an over-expression of NF-κB and other stem cell regulators [60], and it has been shown that pancreatic CSCs exhibit high NF-κB activity [61, 62]. The NF-κB pathway regulates the migration and invasion of pancreatic CSCs, and NF-κB activation is required for maintenance of their stemness phenotype. In addition, pancreatic CSCs also depend on SOX9 expression for their invasive properties. p65 directly binds to the SOX9 promoter and positively regulates its expression. NF-κB and SOX9 regulate the CSC population. It is worth noting that the expression of p65 and SOX9 overlap with the previously identified CSC population, underscoring that canonical NF-κB signaling is important in CSC regulation [62]. Additional data suggest that NF-κB activity in pancreatic CSCs is mediated by p50/RelA, p52/RelA and c-Rel homodimers. In contrast, non-stem cancer cells only express p50/p50 homodimers, which lack transactivating activity. It has also been found that in pancreatic CSCs NF-κB can promote apoptosis resistance to anti-cancer drugs by up-regulating anti-apoptotic proteins such as XIAP, cIAP and FLIP [61].
11 NF-κB signaling in colon cancer
The canonical NF-κB pathway induces the expression of genes encoding stem cell-associated factors and, in addition, regulates the intestinal stem cell compartment through IKKβ [63]. Over-expression of IKKβ has been found to result in activation of β-catenin/WNT signaling, thereby inducing proliferation and the formation of tumors. These results indicate that both NF-κB and WNT signaling can drive intestinal tumorigenesis [63]. p65 binds to β-catenin/Tcf via CBP, thereby enhancing WNT signaling and inducing de-differentiation of intestinal non-stem cells and, by doing so, providing tumor stem cell properties to them. NF-κB activity depends on TNFα and K-Ras, which enhance the interaction between β-catenin and CBP [64]. The canonical NF-κB pathway is an important mediator of intestinal stem cell proliferation and tumor initiation. During colorectal carcinogenesis after APC loss, p65 binds to the promoter regions of the stem cell marker genes Lgr5, Olfm4 and Rgmb in a process that depends on RAC1 expression [65]. In addition, there is increasing evidence that inflammation is involved in the development of diverse epithelial tumors. In the colon, this is exemplified by an interplay between microflora-induced innate immunity responses in intestinal stem cells within their niche. This process is extensively regulated by NF-κB [66]. Since NF-κB is anomalously activated early in carcinogenesis, there are ample opportunities to take advantage of this activation for the design of preventive and therapeutic tools (see below).
Together, these results show that the NF-κB pathway is constitutively active in CSCs derived from many types of tumors and that activation of this pathway has functional implications for self-renewal and maintenance of the CSC population. Activation of NF-κB in these cells affects the expression of apoptotic genes, inflammatory cytokines, adhesion molecules and cell cycle regulators that stimulate cell proliferation and influence tumor growth by regulating CSC maintenance. Expression of NF-κB target genes sustains the undifferentiated state and allows CSCs to self-renew, even in the presence of common chemotherapeutic drugs (Fig. 1). This is an indication that this signaling pathway may serve as a diagnostic, prognostic and therapeutic target for a large number of tumors.
NF-κB regulates the cancer stem cell (CSC) phenotype. Activation of both canonical and non-canonical NF-κB pathways has been observed in CSCs. The pro-inflammatory cytokine TNFα induces activation of the canonical NF-κB pathway through its cognate receptor and thereby induces IKK complex formation, which leads to IκB phosphorylation. IκB acts as a NF-κB repressor in un-stimulated conditions by blocking nuclear translocation of NF-κB dimers. Once IκB is phosphorylated, it is degraded by the proteasome, allowing NF-κB activation. Non-canonical NF-κB activation has also been observed in CSCs. RANKL (receptor activator of NF-κB ligand) induces activation of the kinase NIK through its receptor. NIK activates IKKα, allowing phosphorylation of p100. Phosphorylated p100 is processed by the proteasome, allowing NF-κB nuclear translocation. Over-expression of NF-κB responsive genes has been observed in CSCs. These genes are involved in diverse oncogenic responses such as proliferation, metastasis, apoptosis avoidance, angiogenesis and maintenance of the stemness phenotype. Inhibition of the NF-κB pathway in CSCs by diverse approaches (see Table 1) can compromise their self-renewal, and thus tumorigenic, abilities
12 Drugs that inhibit NF-κB target CSCs
Since NF-κB activation plays a crucial role in the maintenance and expansion of CSCs in many tumors, it has been suggested that NF-κB inhibitors might be used to specifically eliminate the CSC population. Conventional chemotherapeutic agents do not target the CSC population. In fact, several drugs (i.e., taxanes, vinca alkaloids, nucleoside analogues and topo-isomerase inhibitors) activate the NF-κB pathway [67], which conceivably could promote the expansion of CSCs and, thus, disease recurrence. Although not extensively studied, NF-κB-mediated CSC expansion could be one of the main mechanisms for intrinsic resistance to chemotherapy. So, the use of NF-κB inhibitors could offer a therapeutic opportunity for many tumors. In fact, the potential of these NF-κB inhibitors to kill CSCs has recently been assessed, and a large number of molecules has been reported to be able to inhibit the NF-κB pathway through different mechanisms. Some molecules were found to compromise the binding of NF-κB to DNA, prevent the phosphorylation and degradation of some of its regulatory components and/or prevent the formation of IKK complexes [68]. Finally, all inhibitors were found to prevent the transcription of NF-κB target genes. In Table 1 some of the most widely studied molecules are listed.
SN50, a cell permeable peptide with a nuclear localization sequence for p50, inhibits NF-κB by interfering with its translocation. Recently, it has been shown that SN50 can induce the differentiation of glioblastoma cancer stem cells (GCSC) through down-regulation of the stem cell markers CD133, SOX2 and NAC1, and up-regulation of the differentiation markers MAP-2 and GFAP. As a result, GCSCs fail to form neurospheres and are reduced in their abilities to invade and generate tumors in vivo. Furthermore, SN50 was found to increase the sensitivity of CSCs to the chemotherapeutic agent temozolomide and to radiation treatment [69]. SN50 can also suppresses the colony and sphere forming abilities of liver cancer cell lines, which correlates with the extent of NF-κB inhibition [70].
Parthenolide, a sesquiterpene lactone derived from the medicinal herb Feverfew (Tanacetum parthenium), binds to and inhibits IKKβ, thereby blocking activation of the canonical NF-κB pathway [71]. Parthenolide impairs cell self-renewal and reduces the CSC populations in leukemias, nasopharyngeal carcinomas, prostate and breast cancers [26, 34, 35, 72, 73]. The parthenolide inhibitory action on self-renewal, sphere-forming activity and in vivo tumor-initiation ability are dose-dependent [26, 34, 72, 73]. Additionally, inhibition of NF-κB through parthenolide reduces BCSC proliferation [73] and induces apoptosis in prostate and leukemic CSCs, indicating that NF-κB is also imperative for the survival of these cells [26]. Noteworthy, it has been found that parthenolide almost exclusively targets CSCs and has minimal effects on non-stem breast cancer cells [73].
Celastrol, a tripterine extracted from the Chinese medicine herb Celastrus orbiculatus, has been found to inhibit IKK activation and to suppress NF-κB activation [74]. Celastrol diminishes the nuclear localization of p65 and ablates leukemic and progenitor stem cells [75]. In prostate cancer cell lines, celastrol has been found to eradicate the ability of CSCs to initiate tumors in vivo and to dramatically impact their ability to generate secondary spheres [26].
Tanshinone IIA, a lipophilic diterpene isolated from Salvia miltiorrhiza, has been found to prevent p65 nuclear translocation in breast CSCs. This compound was found to inhibit the growth of breast CSCs both in vitro and in vivo by blocking IL6/STAT3/NF-κB signaling [76].
Eriocalyxin B (EriB), an ent-kauranoid diterpenoid isolated from Isodon eriocalyx, has been found to inhibit NF-κB transcriptional activity by interfering with the binding of p65 and p50 to their respective response elements [77]. EriB was found to exhibit an anti-tumor effect in leukemia and various cancer cell lines [78]. In ovarian CSCs, EriB prevented the degradation of IκBα and, thereby, decreased the levels of p65 in their nuclei [79]. EriB treatment also inhibited cytokine production and reduced the levels of XIAP (apoptosis inhibitory protein). Ovarian CSCs are resistant to apoptosis mediated through TNF and FasL. EriB treatment, however, was found to sensitize OCSCs to be killed through FAS/TNFα-mediated apoptosis [79].
Sulforaphane, an isothiocyanate derived from broccoli, prevents active NF-κB dimers from binding to the κB sites of its targets, thereby preventing the expression of apoptosis inhibitor proteins in the CSC population [61]. Sulforaphane was also found to block the nuclear translocation of NF-κB, leading to a low expression of its targets in prostate and colon cancer cells [80]. Sulforaphane induces apoptosis of CSCs and profoundly affects their clonogenic capacity in a NF-κB-dependent manner [61]. In pancreatic CSCs, sulforaphane blocks NF-κB binding [81] and eliminates the resistance of CSCs to TRAIL by interfering with NF-κB signaling [61]. Sulforaphane treatment reduces colony and spheroid formation, disrupts ALDH activity and increases cell death in pancreatic CSCs [81]. It has been shown that sulforaphane exhibits an important synergy when administrated in combination with other drugs. Sulforaphane in combination with e.g. sorafenib (a multi-kinase inhibitor) was found to significantly reduce tumor growth in nu/nu mice without having toxic side-effects, which correlated with a diminished CSC population [81]. Sulforaphane and gemcitabine were found to increase the inhibition of stem cell characteristics and to abolish the growth of pancreatic and prostate CSC xenografts without inducing any additional toxicity in mice. Sulforaphane acts through down-regulating c-Rel expression and, consequently, NF-κB activity. In addition, sulforaphane down-regulates Notch1, which may also be involved in the inhibition of NF-κB signaling [82].
A recently described compound, IMD-0354, inhibits IKKβ and blocks IκBα phosphorylation, thus preventing p65 translocation. IMD-O354 treatment decreases the CSC fraction in a dose-dependent manner and reduces the expression of stem cell factors. IMD-O354 alone or in combination with doxorubicin enhances tumor cytotoxicity and prevents multidrug resistance (MDR) [83].
Bay11-7082 and Bay11-7085 act by inhibiting IκBα phosphorylation, thus blocking IκB degradation and maintaining NF-κB in an inactive state [84]. Bay11-708 treatment dramatically reduces mammosphere formation in BCSCs [58]. Furthermore, Bay11-708 completely suppresses the secretion of pro-inflammatory cytokines involved in CSC regulation [55]. Additional drugs such dehydroxymethylepoxyquinomicin (DHMEQ) inhibit the nuclear translocation of NF-kB dimers [85]. It has been found that DHMEQ dramatically reduces the tumorigenic potential of CD44+/CD24- BCSC [29] and that this compound decreases the frequency of mammosphere formation in a dose-dependent manner. In addition, cells treated with this inhibitor failed to generate secondary mammospheres [86]. Dimethyl amino parthenolide (Dampt), a synthetic analogue of parthenolide, has been found to eradicate the CSC population in myeloid and lymphoid leukemias, both in vivo and in vitro. Furthermore, Dampt was found to induce apoptosis in leukemia progenitor cells while sparing normal hemopoietic stem cells (HSCs) [35]. Similarly, other NF-κB inhibitors such as pyrrolidinedithiocarbamate (PDTC) and its analogue diethyldithiocarbamate (DETC) preferentially inhibited sphere formation in breast cancer [73] and in vivo studies have shown that PDTC treatment can inhibit tumor growth and synergize with paclitaxel [73]. These results indicate that BCSCs may be selectively removed through inhibition of the NF-κB pathway. 481407 compound, a cell-permeable potent site-binding inhibitor of IKKβ, induces apoptosis in prostate CSCs, indicating that NF-κB is important for the survival of these cells as well [26]. In addition, 481407 was found to reduce the ability of CSCs to generate secondary spheres and to eliminate the tumorigenic potential of prostate CSCs [26]. MG-132 blocks the degradation of IκB through inhibition of the 26S proteasome, allowing the retention of NF-κB in the cytoplasm and preventing its nuclear translocation [87]. In AML MG-132 induces a strong apoptotic response, preferentially in the leukemic stem cells (LSCs), while sparing normal HSCs [25, 33]. In prostate cancer, MG-132 eliminates the secondary sphere-forming ability of CSCs.
13 Clinical compounds
There are a few examples of compounds that, although not developed specifically to inhibit NF-κB, modulate its pathway and that are currently in clinical use.
Niclosamide, a FDA-approved anti-helmintic drug, has been found to eliminate LSCs through NF-κB inhibition and the production of reactive oxygen species, without affecting the normal population of hematopoietic progenitor cells [88].
Sulindac, a non-steroidal anti-inflammatory (NSAID) drug, has been found to effectively prevent colon cancer in human and murine models [89]. In the murine models, this drug inhibited COX-2, WNT/β-catenin and NF-κB signaling [90–92]. The chemo-preventive effect of sulindac is partly based on the elimination of CSCs through induction of apoptosis. Sulindac is particularly active in stem cells harboring nuclear β-catenin and, thus, removes (intestinal) stem cells with aberrant activation of WNT signaling [72]. Indeed, sulindac and other NSAIDs such as celecoxib, can effectively reduce the number and size of adenomas in familial adenomatous polyposis (FAP) syndrome patients. These data suggest that sulindac can efficiently target CSCs. As yet, however, there are no data available from long-term surveys indicating that there is a reduction in cancer risk [89, 93]. In animal models of breast cancer, a derivative of sulindac (phosphosulindac) has been shown to target breast CSCs, thereby reducing their tumorigenic capacity [94].
Bortezomib (Velcade, Millenium) is a drug that has recently been approved for its use in myeloma and Hodgkin lymphoma. Bortezomib, a known proteasome inhibitor, is also a strong NF-κB inhibitor. Recently, Cheresh et al. found that erlotinib, an effective inhibitor of EGFR kinase, induces the expression of CD61, a molecule that confers stem-cell characteristics and drug resistance [95]. CD61 signals through KRAS/RalB to activate NF-κB and, by doing so, promotes the stem-cell phenotype. Bortezomib is able to block this activation and synergizes with erlotinib to suppress therapy resistance. Clinical assays are now underway in patients to test if this combination is useful in lung cancer patients. Since the cytotoxic effect of bortezomib is independent of cell division, it has a potential advantage for the eradication of low cycling leukemia cells that depend on the NF-κB pathway to self-renew. Recently, Attar et al. showed that a combination of bortezomib and lenalidomide could elicit a synergic cytotoxic effect in patients with AML and myelodysplastic syndrome [96]. Interestingly, it was found that bortezomib in combination with daunorubicin and cytarabine induced a complete remission in 61 % of the patients with AML [97]. Although not documented, part of the clinical effectiveness of bortezomib could be due to a direct effect on CSCs.
Finally, curcumin, a polyphenol derived from Curcuma longa, appears particularly promising [18]. This compound, which is a strong inhibitor of NF-κB signaling, has been tested in phase I and II trials as adyuvant therapy in several cancer types [98] and as a chemo-preventive in colorectal cancer [99, 100]. Curcumin has also been found to be effective in minimizing the growth and invasiveness of breast CSCs. Curcumin and epigallocatechin-3-gallate can inhibit STAT3 phosphorylation and prevent STAT/NF-κB (p65) interaction, thereby reducing the BCSC fraction [101]. Targeting NF-κB signaling by curcumin also reduces cell viability and increases cell death in liver cancer cell lines. Its effects are directly related to the extent of NF-κB inhibition [70]. In colon cancer, curcumin reduces the relative expression of stem cell markers. However, it promotes the autophagic survival of colon CSCs [70]. Since this compound can selectively kill CSCs as opposed to normal tissue stem cells [102], it represents an example of the potential utility of an NF-κB inhibitor in the clinic. Nevertheless, low oral bioavailability and unexpected toxicity added to a paucity of randomized, placebo-controlled and double-blind studies has so far precluded its clinical use in cancer patients. Currently, new derivatives and conjugates with enhanced pharmacological properties and reduced toxicity are being developed to make this compound a success in the clinic [103–106].
14 Conclusions and perspectives
Activation of the canonical NF-κB pathway is a common feature of CSCs from many types of tumors. There are ample indications supporting the participation of this signaling pathway in the self-renewal, proliferation, survival and differentiation of CSCs. The non-canonical NF-κB pathway is also involved, although there is as yet insufficient information to fully define its role. Even when the relationship between NF-κB and CSCs is settled, the key molecules involved in the regulation of CSCs are still unknown. NF-κB can promote the expression of many genes involved in self-renewal, proliferation, differentiation, survival, inflammation, invasion and metastasis, which could be involved in the regulation of CSCs. Recent evidence suggests that it is possible to eliminate or reduce the CSC population through drugs or other compounds that suppress NF-κB activation. Such NF-κB inhibitors provide a therapeutic opportunity to eliminate the CSC fraction, which is responsible for cancer growth and recurrence. In particular, the possibility of using these compounds in chronic schemes to reduce disease progression appears attractive. Studies in animal models aimed at testing the efficacy of NF-κB inhibitors as chemo-sensitizers and chronic schemes aimed at reducing relapses are needed to close the gap to the clinic. Exceptional low toxicity profiles are required to be able to use combined regimens and to avoid resistance. New compounds, such as curcumin derivatives or conjugates, hold promise in this respect.
References
T. Reya, S.J. Morrison, M.F. Clarke, I.L. Weissman, Stem cells, cancer, and cancer stem cells. Nature 414, 105–111 (2001)
J. Di, T. Duiveman-de Boer, P.L. Zusterzeel, C.G. Figdor, L.F. Massuger, R. Torensma, The stem cell markers Oct4A, Nanog and c-Myc are expressed in ascites cells and tumor tissue of ovarian cancer patients. Cell. Oncol. 36, 363–374 (2013)
A. Koren, H. Motaln, T. Cufer, Lung cancer stem cells: a biological and clinical perspective. Cell. Oncol. 36, 265–275 (2013)
N.A. Lobo, Y. Shimono, D. Qian, M.F. Clarke, The biology of cancer stem cells. Annu. Rev. Cell Dev. Biol. 23, 675–699 (2007)
R. Bjerkvig, B.B. Tysnes, K.S. Aboody, J. Najbauer, A.J. Terzis, Opinion: the origin of the cancer stem cell: current controversies and new insights. Nat. Rev. Cancer 5, 899–904 (2005)
M.S. Hayden, S. Ghosh, Signaling to NF-kappaB. Genes Dev. 18, 2195–2224 (2004)
M.S. Hayden, S. Ghosh, Shared principles in NF-kappaB signaling. Cell 132, 344–362 (2008)
V.F. Shih, R. Tsui, A. Caldwell, A. Hoffmann, A single NFκB system for both canonical and non-canonical signaling. Cell Res. 21, 86–102 (2011)
L. Ling, Z. Cao, D.V. Goeddel, NF-kappaB-inducing kinase activates IKK-alpha by phosphorylation of Ser-176. Proc. Natl. Acad. Sci. U. S. A. 95, 3792–3797 (1998)
G. Qing, Z. Qu, G. Xiao, Stabilization of basally translated NF-kB-inducing kinase (NIK) protein functions as a molecular switch of processing of NF-kB2 p100. J. Biol. Chem. 280, 40578–40582 (2005)
W.E. Naugler, M. Karin, NF-kappaB and cancer-identifying targets and mechanisms. Curr. Opin. Genet. Dev. 18, 19–26 (2008)
D.K. Biswas, Q. Shi, S. Baily, I. Strickland, S. Ghosh, A.B. Pardee, J.D. Iglehart, NF-kappa B activation in human breast cancer specimens and its role in cell proliferation and apoptosis. Proc. Natl. Acad. Sci. U. S. A. 101, 10137–10142 (2004)
J. Bollrath, F.R. Greten, IKK/NF-kappaB and STAT3 pathways: central signalling hubs in inflammation-mediated tumour promotion and metastasis. EMBO Rep. 10, 1314–1319 (2009)
F.R. Greten, L. Eckmann, T.F. Greten, J.M. Park, Z.W. Li, L.J. Egan, M.F. Kagnoff, M. Karin, IKKbeta links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell 118, 285–296 (2004)
H.L. Pahl, Activators and target genes of Rel/NF-kappaB transcription factors. Oncogene 18, 6853–6866 (1999)
M. Karin, Nuclear factor-kappaB in cancer development and progression. Nature 441, 431–436 (2006)
E. Bandala, M. Espinosa, V. Maldonado, J. Melendez-Zajgla, Inhibitor of apoptosis-1 (IAP-1) expression and apoptosis in non-small-cell lung cancer cells exposed to gemcitabine. Biochem. Pharmacol. 62, 13–19 (2001)
K. Mohankumar, S. Pajaniradje, S. Sridharan, V.K. Singh, L. Ronsard, A.C. Banerjea, B.C. Selvanesan, M.S. Coumar, L. Periyasamy, R. Rajagopalan, Apoptosis induction by an analog of curcumin (BDMC-A) in human laryngeal carcinoma cells through intrinsic and extrinsic pathways. Cell. Oncol. 37, 439–454 (2014)
V. Papanikolaou, N. Stefanou, S. Dubos, I. Papathanasiou, M. Palianopoulou, V. Valiakou, A. Tsezou, Synergy of leptin/STAT3 with HER2 receptor induces tamoxifen resistance in breast cancer cells through regulation of apoptosis-related genes. Cell. Oncol. 38, 155–164 (2015)
X. Dolcet, D. Llobet, J. Pallares, X. Matias-Guiu, NF-kB in development and progression of human cancer. Virchows Archiv : Int. J. Pathol. 446, 475–482 (2005)
M.A. Huber, N. Azoitei, B. Baumann, S. Grunert, A. Sommer, H. Pehamberger, N. Kraut, H. Beug, T. Wirth, NF-kappaB is essential for epithelial-mesenchymal transition and metastasis in a model of breast cancer progression. J. Clin. Invest. 114, 569–581 (2004)
C.W. Li, W. Xia, L. Huo, S.O. Lim, Y. Wu, J.L. Hsu, C.H. Chao, H. Yamaguchi, N.K. Yang, Q. Ding, Y. Wang, Y.J. Lai, A.M. LaBaff, T.J. Wu, B.R. Lin, M.H. Yang, G.N. Hortobagyi, M.C. Hung, Epithelial-mesenchymal transition induced by TNF-alpha requires NF-kappaB-mediated transcriptional upregulation of Twist1. Cancer Res. 72, 1290–1300 (2012)
H. Korkaya, S. Liu, M.S. Wicha, Regulation of cancer stem cells by cytokine networks: attacking cancer’s inflammatory roots. Clin. Cancer. Res.: Off. J. Am. Assoc. Cancer Res. 17, 6125–6129 (2011)
M. Karin, NF-kappaB and cancer: mechanisms and targets. Mol. Carcinog. 45, 355–361 (2006)
M.L. Guzman, S.J. Neering, D. Upchurch, B. Grimes, D.S. Howard, D.A. Rizzieri, S.M. Luger, C.T. Jordan, Nuclear factor-kappa B is constitutively activated in primitive human acute myelogenous leukemia cells. Blood 98, 2301–2307 (2001)
V.K. Rajasekhar, L. Studer, W. Gerald, N.D. Socci, H.I. Scher, Tumour-initiating stem-like cells in human prostate cancer exhibit increased NF-kappaB signalling. Nat. Commun. 2, 162 (2011)
R. Birnie, S.D. Bryce, C. Roome, V. Dussupt, A. Droop, S.H. Lang, P.A. Berry, C.F. Hyde, J.L. Lewis, M.J. Stower, N.J. Maitland, A.T. Collins, Gene expression profiling of human prostate cancer stem cells reveals a pro-inflammatory phenotype and the importance of extracellular matrix interactions. Genome Biol. 9, R83 (2008)
A.B.. Alvero, R. Chen, H.H. Fu, M. Montagna, P.E. Schwartz, T. Rutherford, D.A. Silasi, K.D. Steffensen, M. Waldstrom, I. Visintin, G. Mor, Molecular phenotyping of human ovarian cancer stem cells unravels the mechanisms for repair and chemoresistance. Cell Cycle 8, 158–166 (2009)
M. Murohashi, K. Hinohara, M. Kuroda, T. Isagawa, S. Tsuji, S. Kobayashi, K. Umezawa, A. Tojo, H. Aburatani, N. Gotoh, Gene set enrichment analysis provides insight into novel signalling pathways in breast cancer stem cells. Br. J. Cancer 102, 206–212 (2010)
R. Liu, X. Wang, G.Y. Chen, P. Dalerba, A. Gurney, T. Hoey, G. Sherlock, J. Lewicki, K. Shedden, M.F. Clarke, The prognostic role of a gene signature from tumorigenic breast-cancer cells. N. Engl. J. Med. 356, 217–226 (2007)
J.M. Garner, M. Fan, C.H. Yang, Z. Du, M. Sims, A.M. Davidoff, L.M. Pfeffer, Constitutive activation of signal transducer and activator of transcription 3 (STAT3) and nuclear factor kappaB signaling in glioblastoma cancer stem cells regulates the Notch pathway. J. Biol. Chem. 288, 26167–26176 (2013)
Y. Kagoya, A. Yoshimi, K. Kataoka, M. Nakagawa, K. Kumano, S. Arai, H. Kobayashi, T. Saito, Y. Iwakura, M. Kurokawa, Positive feedback between NF-kappaB and TNF-alpha promotes leukemia-initiating cell capacity. J. Clin. Invest. 124, 528–542 (2014)
M.L. Guzman, C.F. Swiderski, D.S. Howard, B.A. Grimes, R.M. Rossi, S.J. Szilvassy, C.T. Jordan, Preferential induction of apoptosis for primary human leukemic stem cells. Proc. Natl. Acad. Sci. U. S. A. 99, 16220–16225 (2002)
M.L. Guzman, R.M. Rossi, L. Karnischky, X. Li, D.R. Peterson, D.S. Howard, C.T. Jordan, The sesquiterpene lactone parthenolide induces apoptosis of human acute myelogenous leukemia stem and progenitor cells. Blood 105, 4163–4169 (2005)
M.L. Guzman, R.M. Rossi, S. Neelakantan, X. Li, C.A. Corbett, D.C. Hassane, M.W. Becker, J.M. Bennett, E. Sullivan, J.L. Lachowicz, A. Vaughan, C.J. Sweeney, W. Matthews, M. Carroll, J.L. Liesveld, P.A. Crooks, C.T. Jordan, An orally bioavailable parthenolide analog selectively eradicates acute myelogenous leukemia stem and progenitor cells. Blood 110, 4427–4435 (2007)
H.L. Ang, V. Tergaonkar, Notch and NFkappaB signaling pathways: do they collaborate in normal vertebrate brain development and function? BioEssays: News Rev. Mol. Cell Dev. Biol. 29, 1039–1047 (2007)
M. Patane, P. Porrati, E. Bottega, S. Morosini, G. Cantini, V. Girgenti, A. Rizzo, M. Eoli, B. Pollo, F.L. Sciacca, S. Pellegatta, G. Finocchiaro, Frequency of NFKBIA deletions is low in glioblastomas and skewed in glioblastoma neurospheres. Mol. Cancer 12, 160 (2013)
M. Tafani, M. Di Vito, A. Frati, L. Pellegrini, E. De Santis, G. Sette, A. Eramo, P. Sale, E. Mari, A. Santoro, A. Raco, M. Salvati, R. De Maria, M.A. Russo, Pro-inflammatory gene expression in solid glioblastoma microenvironment and in hypoxic stem cells from human glioblastoma. J. Neuroinflammation 8, 32 (2011)
A.B.. Hjelmeland, Q. Wu, S. Wickman, C. Eyler, J. Heddleston, Q. Shi, J.D. Lathia, J. Macswords, J. Lee, R.E. McLendon, J.N. Rich, Targeting A20 decreases glioma stem cell survival and tumor growth. PLoS Biol. 8, e1000319 (2010)
L. Nogueira, P. Ruiz-Ontanon, A. Vazquez-Barquero, M. Lafarga, M.T. Berciano, B. Aldaz, L. Grande, I. Casafont, V. Segura, E.F. Robles, D. Suarez, L.F. Garcia, J.A. Martinez-Climent, J.L. Fernandez-Luna, Blockade of the NFkappaB pathway drives differentiating glioblastoma-initiating cells into senescence both in vitro and in vivo. Oncogene 30, 3537–3548 (2011)
D.W. Lee, D. Ramakrishnan, J. Valenta, I.F. Parney, K.J. Bayless, R. Sitcheran, The NF-kappaB RelB protein is an oncogenic driver of mesenchymal glioma. PLoS One 8, e57489 (2013)
D. Iliopoulos, H.A. Hirsch, G. Wang, K. Struhl, Inducible formation of breast cancer stem cells and their dynamic equilibrium with non-stem cancer cells via IL6 secretion. Proc. Natl. Acad. Sci. U. S. A. 108, 1397–1402 (2011)
I. Chefetz, A.B.. Alvero, J.C. Holmberg, N. Lebowitz, V. Craveiro, Y. Yang-Hartwich, G. Yin, L. Squillace, M. Gurrea Soteras, P. Aldo, G. Mor, TLR2 enhances ovarian cancer stem cell self-renewal and promotes tumor repair and recurrence. Cell Cycle 12, 511–521 (2013)
H. Long, R. Xie, T. Xiang, Z. Zhao, S. Lin, Z. Liang, Z. Chen, B. Zhu, Autocrine CCL5 signaling promotes invasion and migration of CD133+ ovarian cancer stem-like cells via NF-kappaB-mediated MMP-9 upregulation. Stem Cells 30, 2309–2319 (2012)
R. Chen, A.B.. Alvero, D.A. Silasi, M.G. Kelly, S. Fest, I. Visintin, A. Leiser, P.E. Schwartz, T. Rutherford, G. Mor, Regulation of IKKbeta by miR-199a affects NF-kappaB activity in ovarian cancer cells. Oncogene 27, 4712–4723 (2008)
A.B.. Alvero, H.H. Fu, J. Holmberg, I. Visintin, L. Mor, C.C. Marquina, J. Oidtman, D.A. Silasi, G. Mor, Stem-like ovarian cancer cells can serve as tumor vascular progenitors. Stem Cells 27, 2405–2413 (2009)
M. Shipitsin, L.L. Campbell, P. Argani, S. Weremowicz, N. Bloushtain-Qimron, J. Yao, T. Nikolskaya, T. Serebryiskaya, R. Beroukhim, M. Hu, M.K. Halushka, S. Sukumar, L.M. Parker, K.S. Anderson, L.N. Harris, J.E. Garber, A.L. Richardson, S.J. Schnitt, Y. Nikolsky, R.S. Gelman, K. Polyak, Molecular definition of breast tumor heterogeneity. Cancer Cell 11, 259–273 (2007)
J.H. Ju, K. Jang, K.M. Lee, M. Kim, J. Kim, J.Y. Yi, D.Y. Noh, I. Shin, CD24 enhances DNA damage-induced apoptosis by modulating NF-kappaB signaling in CD44-expressing breast cancer cells. Carcinogenesis 32, 1474–1483 (2011)
M. Liu, T. Sakamaki, M.C. Casimiro, N.E. Willmarth, A.A. Quong, X. Ju, J. Ojeifo, X. Jiao, W.S. Yeow, S. Katiyar, L.A. Shirley, D. Joyce, M.P. Lisanti, C. Albanese, R.G. Pestell, The canonical NF-kappaB pathway governs mammary tumorigenesis in transgenic mice and tumor stem cell expansion. Cancer Res. 70, 10464–10473 (2010)
Y. Cao, J.L. Luo, M. Karin, IkappaB kinase alpha kinase activity is required for self-renewal of ErbB2/Her2-transformed mammary tumor-initiating cells. Proc. Natl. Acad. Sci. U. S. A. 104, 15852–15857 (2007)
W. Zhang, W. Tan, X. Wu, M. Poustovoitov, A. Strasner, W. Li, N. Borcherding, M. Ghassemian, M. Karin, A NIK-IKKalpha module expands ErbB2-induced tumor-initiating cells by stimulating nuclear export of p27/Kip1. Cancer Cell 23, 647–659 (2013)
D. Schramek, A. Leibbrandt, V. Sigl, L. Kenner, J.A. Pospisilik, H.J. Lee, R. Hanada, P.A. Joshi, A. Aliprantis, L. Glimcher, M. Pasparakis, R. Khokha, C.J. Ormandy, M. Widschwendter, G. Schett, J.M. Penninger, Osteoclast differentiation factor RANKL controls development of progestin-driven mammary cancer. Nature 468, 98–102 (2010)
M. Palafox, I. Ferrer, P. Pellegrini, S. Vila, S. Hernandez-Ortega, A. Urruticoechea, F. Climent, M.T. Soler, P. Munoz, F. Vinals, M. Tometsko, D. Branstetter, W.C. Dougall, E. Gonzalez-Suarez, RANK induces epithelial-mesenchymal transition and stemness in human mammary epithelial cells and promotes tumorigenesis and metastasis. Cancer Res. 72, 2879–2888 (2012)
D. Iliopoulos, H.A. Hirsch, K. Struhl, An epigenetic switch involving NF-kappaB, Lin28, Let-7 MicroRNA, and IL6 links inflammation to cell transformation. Cell 139, 693–706 (2009)
H. Korkaya, G.I. Kim, A. Davis, F. Malik, N.L. Henry, S. Ithimakin, A.A. Quraishi, N. Tawakkol, R. D’Angelo, A.K. Paulson, S. Chung, T. Luther, H.J. Paholak, S. Liu, K.A. Hassan, Q. Zen, S.G. Clouthier, M.S. Wicha, Activation of an IL6 inflammatory loop mediates trastuzumab resistance in HER2+ breast cancer by expanding the cancer stem cell population. Mol. Cell 47, 570–584 (2012)
M.D. Hale, J.D. Hayden, H.I. Grabsch, Tumour-microenvironment interactions: role of tumour stroma and proteins produced by cancer-associated fibroblasts in chemotherapy response. Cell. Oncol. 36, 95–112 (2013)
M. Yamamoto, Y. Taguchi, T. Ito-Kureha, K. Semba, N. Yamaguchi, J. Inoue, NF-kappaB non-cell-autonomously regulates cancer stem cell populations in the basal-like breast cancer subtype. Nat. Commun. 4, 2299 (2013)
G. Storci, P. Sansone, S. Mari, G. D’Uva, S. Tavolari, T. Guarnieri, M. Taffurelli, C. Ceccarelli, D. Santini, P. Chieco, K.B. Marcu, M. Bonafe, TNFalpha up-regulates SLUG via the NF-kappaB/HIF1alpha axis, which imparts breast cancer cells with a stem cell-like phenotype. J. Cell. Physiol. 225, 682–691 (2010)
S.A. Mani, W. Guo, M.J. Liao, E.N. Eaton, A. Ayyanan, A.Y. Zhou, M. Brooks, F. Reinhard, C.C. Zhang, M. Shipitsin, L.L. Campbell, K. Polyak, C. Brisken, J. Yang, R.A. Weinberg, The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 133, 704–715 (2008)
A. Van den Broeck, H. Vankelecom, W. Van Delm, L. Gremeaux, J. Wouters, J. Allemeersch, O. Govaere, T. Roskams, B. Topal, Human pancreatic cancer contains a side population expressing cancer stem cell-associated and prognostic genes. PLoS One 8, e73968 (2013)
G. Kallifatidis, V. Rausch, B. Baumann, A. Apel, B.M. Beckermann, A. Groth, J. Mattern, Z. Li, A. Kolb, G. Moldenhauer, P. Altevogt, T. Wirth, J. Werner, P. Schemmer, M.W. Buchler, A.V. Salnikov, I. Herr, Sulforaphane targets pancreatic tumour-initiating cells by NF-kappaB-induced antiapoptotic signalling. Gut 58, 949–963 (2009)
L. Sun, L.A. Mathews, S.M. Cabarcas, X. Zhang, A. Yang, Y. Zhang, M.R. Young, K.D. Klarmann, J.R. Keller, W.L. Farrar, Epigenetic regulation of SOX9 by the NF-kappaB signaling pathway in pancreatic cancer stem cells. Stem Cells 31, 1454–1466 (2013)
K. Vlantis, A. Wullaert, Y. Sasaki, M. Schmidt-Supprian, K. Rajewsky, T. Roskams, M. Pasparakis, Constitutive IKK2 activation in intestinal epithelial cells induces intestinal tumors in mice. J. Clin. Invest. 121, 2781–2793 (2011)
S. Schwitalla, A.A. Fingerle, P. Cammareri, T. Nebelsiek, S.I. Goktuna, P.K. Ziegler, O. Canli, J. Heijmans, D.J. Huels, G. Moreaux, R.A. Rupec, M. Gerhard, R. Schmid, N. Barker, H. Clevers, R. Lang, J. Neumann, T. Kirchner, M.M. Taketo, G.R. van den Brink, O.J. Sansom, M.C. Arkan, F.R. Greten, Intestinal tumorigenesis initiated by dedifferentiation and acquisition of stem-cell-like properties. Cell 152, 25–38 (2013)
K.B. Myant, P. Cammareri, E.J. McGhee, R.A. Ridgway, D.J. Huels, J.B. Cordero, S. Schwitalla, G. Kalna, E.L. Ogg, D. Athineos, P. Timpson, M. Vidal, G.I. Murray, F.R. Greten, K.I. Anderson, O.J. Sansom, ROS production and NF-kappaB activation triggered by RAC1 facilitate WNT-driven intestinal stem cell proliferation and colorectal cancer initiation. Cell Stem Cell 12, 761–773 (2013)
Y. Ben-Neriah, M. Karin, Inflammation meets cancer, with NF-kappaB as the matchmaker. Nat. Immunol. 12, 715–723 (2011)
V. Maldonado, J. Melendez-Zajgla, A. Ortega, Modulation of NF-kappa B, and Bcl-2 in apoptosis induced by cisplatin in HeLa cells. Mutat. Res. 381, 67–75 (1997)
C. Nakanishi, M. Toi, Nuclear factor-kappaB inhibitors as sensitizers to anticancer drugs. Nat. Rev. Cancer 5, 297–309 (2005)
L. Zhang, X. Ren, Y. Cheng, X. Liu, J.E. Allen, Y. Zhang, Y. Yuan, S.Y. Huang, W. Yang, A. Berg, B.S. Webb, J. Connor, C.G. Liu, Z. Lu, W.S. El-Deiry, J.M. Yang, The NFkappaB inhibitor, SN50, induces differentiation of glioma stem cells and suppresses their oncogenic phenotype. Cancer Biol. Ther. 15, 602–611 (2014)
J.U. Marquardt, L. Gomez-Quiroz, L.O. Arreguin Camacho, F. Pinna, Y.H. Lee, M. Kitade, M.P. Dominguez, D. Castven, K. Breuhahn, E.A. Conner, P.R. Galle, J.B. Andersen, V.M. Factor and S.S. Thorgeirsson, Curcumin effectively inhibits oncogenic NF-kB signaling and restrains stemness features in liver cancer, J. Hepatol. (2015)
B.H. Kwok, B. Koh, M.I. Ndubuisi, M. Elofsson, C.M. Crews, The anti-inflammatory natural product parthenolide from the medicinal herb Feverfew directly binds to and inhibits IkappaB kinase. Chem. Biol. 8, 759–766 (2001)
K. Liao, B. Xia, Q.Y. Zhuang, M.J. Hou, Y.J. Zhang, B. Luo, Y. Qiu, Y.F. Gao, X.J. Li, H.F. Chen, W.H. Ling, C.Y. He, Y.J. Huang, Y.C. Lin, Z.N. Lin, Parthenolide inhibits cancer stem-like side population of nasopharyngeal carcinoma cells via suppression of the NF-kappaB/COX-2 pathway. Theranostics 5, 302–321 (2015)
J. Zhou, H. Zhang, P. Gu, J. Bai, J.B. Margolick, Y. Zhang, NF-kappaB pathway inhibitors preferentially inhibit breast cancer stem-like cells. Breast Cancer Res. Treat. 111, 419–427 (2008)
J.H. Lee, T.H. Koo, H. Yoon, H.S. Jung, H.Z. Jin, K. Lee, Y.S. Hong, J.J. Lee, Inhibition of NF-kappa B activation through targeting I kappa B kinase by celastrol, a quinone methide triterpenoid. Biochem. Pharmacol. 72, 1311–1321 (2006)
D.C. Hassane, M.L. Guzman, C. Corbett, X. Li, R. Abboud, F. Young, J.L. Liesveld, M. Carroll, C.T. Jordan, Discovery of agents that eradicate leukemia stem cells using an in silico screen of public gene expression data. Blood 111, 5654–5662 (2008)
C. Lin, L. Wang, H. Wang, L. Yang, H. Guo, X. Wang, Tanshinone IIA inhibits breast cancer stem cells growth in vitro and in vivo through attenuation of IL-6/STAT3/NF-kB signaling pathways. J. Cell. Biochem. 114, 2061–2070 (2013)
C.H. Leung, S.P. Grill, W. Lam, W. Gao, H.D. Sun, Y.C. Cheng, Eriocalyxin B inhibits nuclear factor-kappaB activation by interfering with the binding of both p65 and p50 to the response element in a noncompetitive manner. Mol. Pharmacol. 70, 1946–1955 (2006)
L. Wang, W.L. Zhao, J.S. Yan, P. Liu, H.P. Sun, G.B. Zhou, Z.Y. Weng, W.L. Wu, X.Q. Weng, X.J. Sun, Z. Chen, H.D. Sun, S.J. Chen, Eriocalyxin B induces apoptosis of t(8;21) leukemia cells through NF-kappaB and MAPK signaling pathways and triggers degradation of AML1-ETO oncoprotein in a caspase-3-dependent manner. Cell Death Differ. 14, 306–317 (2007)
A.L. Leizer, A.B.. Alvero, H.H. Fu, J.C. Holmberg, Y.C. Cheng, D.A. Silasi, T. Rutherford, G. Mor, Regulation of inflammation by the NF-kappaB pathway in ovarian cancer stem cells. Am. J. Reprod. Immunol. 65, 438–447 (2011)
Y. Li, T. Zhang, Targeting cancer stem cells with sulforaphane, a dietary component from broccoli and broccoli sprouts. Future Oncol. 9, 1097–1103 (2013)
V. Rausch, L. Liu, G. Kallifatidis, B. Baumann, J. Mattern, J. Gladkich, T. Wirth, P. Schemmer, M.W. Buchler, M. Zoller, A.V. Salnikov, I. Herr, Synergistic activity of sorafenib and sulforaphane abolishes pancreatic cancer stem cell characteristics. Cancer Res. 70, 5004–5013 (2010)
G. Kallifatidis, S. Labsch, V. Rausch, J. Mattern, J. Gladkich, G. Moldenhauer, M.W. Buchler, A.V. Salnikov, I. Herr, Sulforaphane increases drug-mediated cytotoxicity toward cancer stem-like cells of pancreas and prostate. Mol. Ther. 19, 188–195 (2011)
A. Gomez-Cabrero, W. Wrasidlo, R.A. Reisfeld, IMD-0354 targets breast cancer stem cells: a novel approach for an adjuvant to chemotherapy to prevent multidrug resistance in a murine model. PLoS One 8, e73607 (2013)
J.W. Pierce, R. Schoenleber, G. Jesmok, J. Best, S.A. Moore, T. Collins, M.E. Gerritsen, Novel inhibitors of cytokine-induced I kappa B alpha phosphorylation and endothelial cell adhesion molecule expression show anti-inflammatory effects in vivo. J. Biol. Chem. 272, 21096–21103 (1997)
A. Ariga, J. Namekawa, N. Matsumoto, J. Inoue, K. Umezawa, Inhibition of tumor necrosis factor-alpha -induced nuclear translocation and activation of NF-kappa B by dehydroxymethylepoxyquinomicin. J. Biol. Chem. 277, 24625–24630 (2002)
K. Hinohara, S. Kobayashi, H. Kanauchi, S. Shimizu, K. Nishioka, E. Tsuji, K. Tada, K. Umezawa, M. Mori, T. Ogawa, J. Inoue, A. Tojo, N. Gotoh, ErbB receptor tyrosine kinase/NF-kappaB signaling controls mammosphere formation in human breast cancer. Proc. Natl. Acad. Sci. U. S. A. 109, 6584–6589 (2012)
J. Adams, The proteasome: a suitable antineoplastic target. Nat. Rev. Cancer 4, 349–360 (2004)
Y. Jin, Z. Lu, K. Ding, J. Li, X. Du, C. Chen, X. Sun, Y. Wu, J. Zhou, J. Pan, Antineoplastic mechanisms of niclosamide in acute myelogenous leukemia stem cells: inactivation of the NF-kappaB pathway and generation of reactive oxygen species. Cancer Res. 70, 2516–2527 (2010)
M.J. Thun, S.J. Henley, C. Patrono, Nonsteroidal anti-inflammatory drugs as anticancer agents: mechanistic, pharmacologic, and clinical issues. J. Natl. Cancer Inst. 94, 252–266 (2002)
W. Qiu, X. Wang, B. Leibowitz, H. Liu, N. Barker, H. Okada, N. Oue, W. Yasui, H. Clevers, R.E. Schoen, J. Yu, L. Zhang, Chemoprevention by nonsteroidal anti-inflammatory drugs eliminates oncogenic intestinal stem cells via SMAC-dependent apoptosis. Proc. Natl. Acad. Sci. U. S. A. 107, 20027–20032 (2010)
A.M. Seo, S.W. Hong, J.S. Shin, I.C. Park, N.J. Hong, D.J. Kim, W.K. Lee, W.J. Lee, D.H. Jin, M.S. Lee, Sulindac induces apoptotic cell death in susceptible human breast cancer cells through, at least in part, inhibition of IKKbeta. Apoptosis: Int. J. Programmed Cell Death 14, 913–922 (2009)
S.J. Shiff, B. Rigas, The role of cyclooxygenase inhibition in the antineoplastic effects of nonsteroidal antiinflammatory drugs (NSAIDs). J. Exp. Med. 190, 445–450 (1999)
C.V. Rao, B.S. Reddy, NSAIDs and chemoprevention. Curr. Cancer Drug Targets 4, 29–42 (2004)
C. Zhu, K.W. Cheng, N. Ouyang, L. Huang, Y. Sun, P. Constantinides, B. Rigas, Phosphosulindac (OXT-328) selectively targets breast cancer stem cells in vitro and in human breast cancer xenografts. Stem Cells 30, 2065–2075 (2012)
L. Seguin, S. Kato, A. Franovic, M.F. Camargo, J. Lesperance, K.C. Elliott, M. Yebra, A. Mielgo, A.M. Lowy, H. Husain, T. Cascone, L. Diao, J. Wang, I.I. Wistuba, J.V. Heymach, S.M. Lippman, J.S. Desgrosellier, S. Anand, S.M. Weis, D.A. Cheresh, An integrin beta(3)-KRAS-RalB complex drives tumour stemness and resistance to EGFR inhibition. Nat. Cell Biol. 16, 457–468 (2014)
E.C. Attar, P.C. Amrein, J.W. Fraser, A.T. Fathi, S. McAfee, M. Wadleigh, D.J. Deangelo, D.P. Steensma, R.M. Stone, J. Foster, D. Neuberg, K.K. Ballen, Phase I dose escalation study of bortezomib in combination with lenalidomide in patients with myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML). Leuk. Res. 37, 1016–1020 (2013)
E.C. Attar, D.J. De Angelo, J.G. Supko, F. D’Amato, D. Zahrieh, A. Sirulnik, M. Wadleigh, K.K. Ballen, S. McAfee, K.B. Miller, J. Levine, I. Galinsky, E.G. Trehu, D. Schenkein, D. Neuberg, R.M. Stone, P.C. Amrein, Phase I and pharmacokinetic study of bortezomib in combination with idarubicin and cytarabine in patients with acute myelogenous leukemia. Clin. Cancer Res. 14, 1446–1454 (2008)
K.G. Troselj, R.N. Kujundzic, Curcumin in combined cancer therapy. Curr. Pharm. Des. 20, 6682–6696 (2014)
R.E. Carroll, R.V. Benya, D.K. Turgeon, S. Vareed, M. Neuman, L. Rodriguez, M. Kakarala, P.M. Carpenter, C. McLaren, F.L. Meyskens Jr., D.E. Brenner, Phase IIa clinical trial of curcumin for the prevention of colorectal neoplasia. Cancer Prev. Res. 4, 354–364 (2011)
L.M. Howells, J. Mahale, S. Sale, L. McVeigh, W.P. Steward, A. Thomas, K. Brown, Translating curcumin to the clinic for lung cancer prevention: evaluation of the preclinical evidence for its utility in primary, secondary, and tertiary prevention strategies. J. Pharmacol. Exp. Ther. 350, 483–494 (2014)
S.S. Chung, J.V. Vadgama, Curcumin and epigallocatechin gallate inhibit the cancer stem cell phenotype via down-regulation of STAT3-NFkappaB signaling. Anticancer Res. 35, 39–46 (2015)
P.P. Sordillo, L. Helson, Curcumin and cancer stem cells: curcumin has asymmetrical effects on cancer and normal stem cells. Anticancer Res. 35, 599–614 (2015)
A.M. Alizadeh, M. Sadeghizadeh, F. Najafi, S.K. Ardestani, V. Erfani-Moghadam, M. Khaniki, A. Rezaei, M. Zamani, S. Khodayari, H. Khodayari, M.A. Mohagheghi, Encapsulation of curcumin in diblock copolymer micelles for cancer therapy. Biomed. Res. Int. 2015, 824746 (2015)
M.J. Dehghan Esmatabadi, B. Farhangi, Z. Safari, H. Kazerooni, H. Shirzad, F. Zolghadr, M. Sadeghizadeh, Dendrosomal curcumin inhibits metastatic potential of human SW480 colon cancer cells through down-regulation of claudin1, zeb1 and hef1-1 gene expression. Asian Pac. J. Cancer Prev. 16, 2473–2481 (2015)
J.C. Lien, C.M. Hung, Y.J. Lin, H.C. Lin, T.C. Ko, L.C. Tseng, S.C. Kuo, C.T. Ho, J.C. Lee and T. Way, Pculin02H, a curcumin derivative, inhibits proliferation and clinical drug resistance of HER2-overexpressing cancer cells. Chem. Biol. Interact. 235, 17–26 (2015)
V. Zeighamian, M. Darabi, A. Akbarzadeh, M. Rahmati-Yamchi, N. Zarghami, F. Badrzadeh, R. Salehi, F.S. Tabatabaei Mirakabad, M. Taheri-Anganeh, PNIPAAm-MAA nanoparticles as delivery vehicles for curcumin against MCF-7 breast cancer cells. Artif. Cells Nanomed. Biotechnol. 1–8 (2015)
Acknowledgments
The work at Jorge Melendez-Zajgla laboratory was funded by CONACyT grant 132931.
Conflict of Interest
The authors declare that they have no competing interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vazquez-Santillan, K., Melendez-Zajgla, J., Jimenez-Hernandez, L. et al. NF-κB signaling in cancer stem cells: a promising therapeutic target?. Cell Oncol. 38, 327–339 (2015). https://doi.org/10.1007/s13402-015-0236-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-015-0236-6