Abstract
With the rising number of individuals in their 50s and 60s who are infected with HIV, concerns have emerged about possible increases in the rates of non-HIV-associated dementias. The current study examined the prevalence of mild cognitive impairment (MCI) in older HIV-infected adults, since MCI is an intermediate state between typical cognitive aging and dementia that emerges in this age range. Participants included 75 adults with HIV disease aged 50 years and older who were on combination antiretroviral therapy (cART) and had undetectable plasma viral loads and 80 demographically similar HIV-seronegative comparison subjects. Participants completed a research neuropsychological evaluation that was used to classify MCI according to the comprehensive diagnostic scheme described by Bondi et al. (J Alzheimers Dis 42:275–289, 2014). HIV-infected persons were over seven times more likely to have an MCI designation (16 %) than their seronegative counterparts (2.5 %). Within the HIV+ cohort, MCI had minimal overlap with diagnoses of asymptomatic neurocognitive impairment and was significantly associated with older age, lower Karnofsky Scale of Performance Scores, and mild difficulties performing instrumental activities of daily living (iADLs). HIV infection in older adults is associated with a notably elevated concurrent risk of MCI, which may increase the likelihood of developing non-HIV-associated dementias as this population ages further.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The prevalence of older adults (aged ≥50) living with HIV has grown considerably in recent years (CDC 2012) and is predicted to rise to well over 50 % by 2020 (Brooks et al. 2012). Advancing age in HIV+ adults carries an increased risk for HIV-associated, non-AIDS (HANA) conditions (e.g., cardiovascular disease) and problems in multiple organ systems, including the central nervous system (High et al. 2012). In parallel, HIV-associated neurocognitive disorders (HAND) have persisted in the era of combination antiretroviral therapy (cART; Heaton et al. 2010). Older HIV+ adults are at a particularly increased risk for HAND (Valcour et al. 2004). Taken together, these factors have raised concerns that the HIV population may be increasingly vulnerable to developing non-HIV-associated dementias such as Alzheimer’s disease (AD).
Although controversial (Iudicello et al. 2012), there is some evidence to suggest that HIV may precipitate a neuropathological process similar to that observed in AD. Biomarkers such as beta amyloid (Green et al. 2005; cf. Ances et al. 2012) and tau (Brew et al. 2005) can be altered in HIV disease. Older HIV+ adults who are carriers of ApoEε4 may be at higher risk of HAND (Valcour et al. 2004), especially in combination with amyloid beta plaques (Soontornniyomkij et al. 2012). HIV-associated neuropathologies in the medial temporal region may contribute to declines in delayed episodic memory—a hallmark feature of AD (Maki et al. 2009; Moore et al. 2006). Nevertheless, extant studies focus on HIV-infected persons in their early 50s (Scott et al. 2011), which is younger than the typical age of onset for most non-HIV-associated dementias. Thus, one potential approach to determining the risk of older HIV+ adults for incipient dementia is to draw from the typical cognitive aging literature and determine whether HIV is associated with elevated rates of mild cognitive impairment (MCI).
MCI is a transitional state between typical cognitive aging and dementia (Petersen 2004) that may be observed in persons in their 50s (Anstey et al. 2013). Prevalence estimates of MCI in seronegative older adults range from 5 to 20 % (Hänninen et al. 2002; Lopez et al. 2003; Petersen et al. 2010). There are several potential benefits to exploring the relevance of the MCI diagnostic criteria to older HIV+ adults. First, these criteria have been applied with great success to clinical populations with frontal systems pathology—most notably Parkinson’s disease (Geurtsen et al. 2014; Goldman and Litvan 2011). Second, there is long-standing controversy surrounding the optimal way to diagnose milder forms of neurocognitive disorders in HIV disease (for review, see Nightingale et al. 2014), arguments about which have regained momentum in recent years specifically in regards to the utility of asymptomatic neurocognitive impairment (ANI) (Grant et al. 2014; Su et al. 2015). Thus, considering the wealth of evidence in support of the MCI criteria both in typical and pathological aging (e.g., Parkinson’s disease), an examination of their application to older HIV+ adults seems well justified. Therefore, we aimed to estimate the concurrent risk of MCI in older HIV+ adults, in whom we sought to determine the clinicodemographic and real-world correlates of MCI.
Methods
Participants
The study sample included 155 participants aged 50 years and older who were recruited from the greater San Diego community and local, urban HIV clinics. HIV serostatus for 75 HIV-seropositive (HIV+) and 80 HIV-seronegative comparison individuals (HIV−) was confirmed using standard Western blot and/or a point-of-care test (MedMira Inc., Nova Scotia, Canada). All HIV+ participants were prescribed cART and had undetectable viral loads. Participants were excluded if they had histories of psychosis, current psychiatric disorders (e.g., depression, substance use), major neuromedical conditions (e.g., head injury with loss of consciousness >30 min, stroke, seizure disorder, multiple sclerosis, non-HIV-associated dementia), estimated verbal IQs below 70 on the Wechsler Test of Adult Reading (WTAR; Psychological Corporation 2001), or positive breathalyzer or urine toxicology screens for illicit drugs (except marijuana) on the day of testing. Consistent with MCI research diagnostic criteria (Bondi et al. 2014), we also excluded participants with clinical functional impairment as operationalized by two or more areas of “dependence”: (1) unemployment (not due to elective retirement); (2) endorsed clinically notable declines in instrumental activities of daily living (iADLs) on a modified form of the Lawton and Brody (Lawton and Brody 1969) ADL Scale (i.e., finance management, purchasing groceries, cooking, using transportation, shopping, medication management, and social activity planning; (3) endorsed clinically notable declines in basic activities of daily living (bADLs) on a modified form of the Lawton and Brody ADL scale (i.e., housekeeping/cleaning, laundry, home repairs, bathing, and dressing); or (4) scores <90 on the Karnofsky Scale of Performance Status (Karnofsky and Burchenal 1949), which is a scale that has been applied previously in HIV samples (Gandhi et al. 2011; Morgan et al. 2012). Thus, by these criteria, any participants with minor neurocognitive disorder (MND) or HIV-associated dementia (HAD) using the Frascati criteria for HAND (Antinori et al. 2007) were excluded. Seventy-three percent (n = 55) of HIV-infected individuals were cognitively normal and 27 % (n = 20) met Frascati criteria for ANI (Antinori et al. 2007).
Materials and procedure
All participants provided written, informed consent prior to completing a comprehensive medical, psychiatric, and neuropsychological research evaluation for which they received nominal financial compensation. The university’s human subjects committee (IRB protocol numbers 081481 and 071656) approved the parent study from which these participants were drawn.
All participants were administered a comprehensive neuropsychological test battery by certified research assistants. Measures for MCI group classification were selected from the larger battery in order to examine domains that are typically considered in the MCI literature, including (1) delayed memory, Logical Memory subtest from the Wechsler Memory Scale, 3rd edition (WMS-III; Psychological Corporation 1997) and the long-delay free recall trial of the California Verbal Learning Test, 2nd edition (CVLT-II; Delis et al. 2000); (2) executive functions, Trailmaking Test, Part B (Army Individual Test Battery 1944) and the total moves score from the Tower of London Test (Drexel Version; Culbertson and Zillmer 1999); (3) language, Boston Naming Test (BNT; Goodglass et al. 2001) and verbal (action) fluency test (see Piatt et al. 1999 and Woods et al. 2006 for further details); (4) attention, WMS-III Digit Span and CVLT-II Trial 1; and (5) speed of information processing, Trailmaking Test, Part A and the Total Execution Time from the Tower of London Test.
MCI designations were made using comprehensive neuropsychological criteria as described by Bondi et al. (2014), as these criteria provide a balance of sensitivity and specificity and are less susceptible to false-positive errors than conventional diagnostic criteria (Edmonds et al. 2014). MCI designation was operationalized by endorsement of cognitive symptoms >1 SD above the normative mean on the cognitive symptoms scale of the Profile of Mood States (POMS; McNair et al. 1981) and either (1) scoring >1 SD below the mean of normative data on both neuropsychological measures within one or more domains or (2) scoring >1 SD below the mean of normative data on one test in each of at least three cognitive domains. The group of participants with MCI was further divided by MCI subtype (Petersen 2004), including (1) single domain amnestic (impaired only in the domain of delayed memory), (2) single domain non-amnestic (impaired in one non-memory domain), (3) multiple domain amnestic (impaired in the domain of delayed memory and one or more domains), or (4) multiple domain non-amnestic (impaired in multiple non-memory domains).
Finally, we also generated traditional neurocognitive summary scores and Frascati diagnoses of ANI from the complete evaluation (see Woods et al. 2013), which included measures of motor skills (Grooved Pegboard; Heaton et al. 2004; Kløve 1963) and learning (WMS-III Logical Memory I and CVLT-II Total Trials 1–5) to round out the test battery detailed above. Individual normed T scores were converted into deficit scores (range = 0 [normal] to 5 [severe]; see Carey et al. 2004 for details) and averaged to generate neurocognitive domain scores and a global deficit score (GDS; Carey et al. 2004) that were used to determine ANI per Frascati criteria.
Results
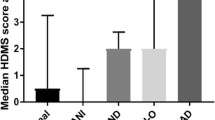
Descriptive demographic and clinical information for HIV+ and HIV− individuals is shown in Table 1. There were no serostatus group differences on any demographic or clinical variables (ps > .10). As shown in Fig. 1, a chi-square test of independence showed a significant association between HIV serostatus and the likelihood of having an MCI designation, χ 2 (1) = 9.36, p = .004. Specifically, HIV+ individuals were at 7.43 (95 % confidence interval = 1.60, 34.42) times greater odds to have MCI designation (total percentage of 16 %) than were HIV− individuals (total percentage of 2.5 %). In the entire HIV+ group, seven subjects met the criteria for multiple domain non-amnestic MCI (58 % of those with MCI, 11 % of the HIV+ sample) and five subjects met the criteria for multiple domain amnestic MCI (42 % of those with MCI, 8 % of the HIV+ sample). None of the HIV+ individuals with MCI had single domain non-amnestic or single domain amnestic MCI.
Next, we examined the clinicodemographic factors from Table 1 and functional outcomes that might be associated with MCI in HIV. All continuous variables were non-normally distributed (all Shapiro-Wilk W Tests ps < .05) so non-parametric Wilcoxon rank-sums tests were used for analyses. Among the HIV+ individuals, an MCI designation was associated with older age (χ 2 (1) = 8.01, p = .006), whereby individuals over the age of 60 were at 6.62 (95 % confidence interval = 1.77, 24.75) times greater odds to have MCI (see Fig. 1). In addition, MCI designations among the HIV+ individuals were significantly associated with lower continuous Karnofsky Scale of Performance Status scores (χ 2 (1) = 5.12, p = .024, Hedge’s g = −.33), and greater mean endorsement of decline from a previous level of iADL ability (χ 2 (1) = 4.48, p = .034, Hedge’s g = .46), but not bADL (p = .57). No other clinical or demographic variables listed in Table 1 differed between individuals with or without MCI among individuals with HIV (all ps > .05).
Finally, we were also interested in the extent to which MCI diagnoses were associated with global deficit scores (GDS) and Frascati ANI diagnoses. HIV+ individuals with MCI had significantly higher continuous GDS values than HIV+ participants without MCI (χ 2 (1) = 9.15, p = .003, Hedge’s g = −.98). Given the possibility that premorbid factors may influence MCI designations, we also covaried education and premorbid IQ (i.e., WTAR) in this analysis, which did not dampen the strong association between MCI and GDS (t(1) = −3.74, p < .001). However, the association between MCI and ANI was characterized by only a slight rate of agreement (i.e., Kappa = .14; see Table 2). Among the 20 persons with ANI, 5 were designated as having MCI (i.e., rate of positive diagnostic agreement = .31). Among the 55 persons without ANI, 48 were designated as not having MCI (i.e., rate of negative diagnostic agreement = .81).
Discussion
With the rising prevalence of adults in their 50s and 60s living with HIV disease, concerns have emerged about possible increases in the future risk of non-HIV-associated dementias in this population. This study examined the possibility that older individuals with HIV may have higher rates of MCI, which is widely considered to be an intermediate stage between normal cognitive aging and dementia. Findings showed that HIV infection was associated with a considerably elevated concurrent risk of meeting research diagnostic criteria for MCI. In fact, HIV-infected individuals had an over sevenfold greater odds of being diagnosed with MCI than their seronegative counterparts, which was not better accounted for by clinicodemographic factors—including mood and substance use disorders—as the groups were comparable on these variables. The prevalence rate of MCI for HIV+ adults ages 60 to 70 years in the present study was increased nearly fourfold than the rate observed in typically aging cohorts of the same age (Anstey et al. 2013). MCI designations among HIV+ individuals were also associated with greater difficulties in iADLs, which may be indicative of an increased risk for incipient dementia.
HIV-infected individuals with MCI were exclusively classified as having multiple domain subtypes of MCI that, compared to single domain subtypes, often are associated with increased risk for developing dementias (Ganguli et al. 2011). The lack of HIV+ individuals designated as having a single domain subtype also suggests that the HIV+ individuals with MCI may have a relatively robust diagnostic profile of cognitive impairments, as single domain subtypes are more likely to revert back to normal functioning at follow-up compared to multiple domain MCI (Bickel et al. 2006; Summers and Saunders 2012). Studies of MCI in typically aging populations have suggested that a non-amnestic MCI designation is associated with an increased risk of developing either AD or non-AD dementias (e.g., vascular dementia; Busse et al. 2006; Ferman et al. 2013; Roberts et al. 2010). In turn, individuals with non-amnestic MCI evidence increased reversion to normal functioning (Ganguli et al. 2011). By way of contrast, amnestic MCI is thought to be more closely associated with progression specifically to AD (Damian et al. 2013). The equal prevalence of amnestic and non-amnestic MCI in the present study suggests that the specific dementia syndrome to which HIV-infected individuals may be vulnerable remains to be determined, as it is possible that MCI may confer a risk of AD or non-AD dementias, including HIV-associated dementia. Indeed, this interpretation is not inconsistent with previous studies in HIV, which have found that HIV-associated neurocognitive deficits do not necessarily fit those that are observed in “cortical” dementias (Iudicello et al. 2012). Future studies should apply cluster and discriminant analyses to examine the profiles of statistically determined MCI phenotypes in HIV, with particular emphasis on determining whether these phenotypes parallel the deficits indicative of frontal-subcortical or cortical profiles.
Our findings suggest that HIV infection increases the risk for having an MCI designation, which, in typically aging cohorts, is less prevalent for adults in their 60s than in relatively older groups (Anstey et al. 2013). The findings of the present study suggest that HIV+ individuals may undergo accelerated cognitive aging. It has been shown, for example, that HIV+ individuals showed a similar pattern and level of cognitive performance as much older seronegatives (Van Gorp et al. 1989). Indeed, the present sample of HIV+ individuals in their 60s had prevalence rates of MCI that were similar to those typically observed in seronegative adults aged 70 and over (Ward et al. 2012). These cognitive deficits in the cART era appear to be driven by a rise in the prevalence of impairment in memory and executive functions among HIV+ individuals who are medically asymptomatic (Heaton et al. 2011). Moreover, older HIV+ adults are less likely than their younger or seronegative counterparts to experience “successful” neurocognitive aging (e.g., Moore et al. 2014), which is related to poorer everyday functioning (Malaspina et al. 2011) and lower health-related quality of life (Moore et al. 2014). As such, as HIV-infected individuals continue to age, it will be increasingly important to determine whether an increased risk for MCI in HIV consequentially confers an increased likelihood of developing non-HIV-related dementias and more severe declines in everyday functioning.
The clinical relevance of the MCI diagnosis in HIV is supported by evidence that HIV+ subjects with MCI had lower clinician-rated functional status and reported mild declines in iADL. Although preserved independence in everyday functioning is required for an MCI designation, studies examining everyday functioning in typically aging samples have found that mild deficits in iADL abilities often exist in MCI (Schmitter-Edgecombe et al. 2009) and may be associated with baseline risk for developing dementia (Reppermund et al. 2013). Accordingly, some diagnostic schemes allow for mild declines in iADL (Winblad et al. 2004) or subtle interference with function such that tasks require more effort or take more time than they did previously (American Psychiatric Association 2013). While an MCI designation in the HIV+ individuals was associated with increased age, there was no significant association between age and everyday functioning in the HIV+ sample as a whole nor within the HIV+ MCI group specifically (ps > .10). As such, these data suggest that having an MCI designation is related to increased age, but that the functional deficits reported by these individuals are not age-related. In HIV, iADL deficits have been found to be associated with neuropsychological impairment (Heaton et al. 2004), and iADL deficits may be attributable to memory decline due to shallow encoding in older adults with HIV (Fazeli et al. 2014). While the present findings should be interpreted cautiously regarding dementia risk, the neuropsychological and everyday functioning profile of HIV+ individuals with MCI in the present study is consistent with those that are considered to be at risk for developing dementia syndromes.
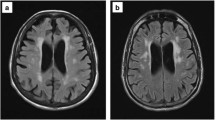
There are several limitations to this retrospective cross-sectional study that deserve consideration. Studies of MCI often explore whether particular biomarkers predict MCI prevalence in typically aging individuals (Anstey et al. 2013). Future investigations into MCI in HIV may therefore wish to explore various biomarkers relevant to HIV and MCI (e.g., CSF beta amyloid or tau levels, MRI markers of neurodegeneration), as well as genetic factors such as ApoEε4. Future longitudinal studies should examine the candidate pathways through which an individual with HIV infection could conceivably reach an MCI designation. HIV infection may directly initiate a biological cascade that results in vascular involvement or increased risk of developing amyloid-β plaques and neurofibrillary tangles, as seen in AD. Another possibility is that the biological and cognitive insult of HIV infection may decrease an individual’s cognitive reserve, and combined with the effects of normal aging and/or very early vascular or AD-type neuropathology, may cause the individual to pass a threshold of impairment in one or more cognitive domains. Although HIV-associated neuropathologies are predominately frontostriatal (Plessis et al. 2014), the hippocampus and other medial temporal lobe structures may also be vulnerable to HIV infection (Pfefferbaum et al. 2014). These latter findings are not inconsistent with those found in MCI, which implicate medial and inferior temporal lobes, as well as temporoparietal structures (Jak et al. 2009). Further, MCI criteria have been reliably applied to aging populations with diseases that include frontal systems pathology such as Parkinson’s disease (Geurtsen et al. 2014; Goldman and Litvan 2011). Future studies should address whether HIV-infected individuals with MCI are particularly susceptible to structural or functional alterations in these regions, as such evidence would highlight the clinical utility of these criteria in aging individuals with HIV. While one may question the extent to which the present findings apply to a broader and more diverse HIV population such as to individuals not prescribed cART and with detectable viral loads who were excluded from the present study, these exclusion criteria may offer increased utility to clinicians, as older individuals with these health profiles more often present in clinical settings. Another limitation is that by virtue of being a retrospective study specifically in HIV, we did not include tests of spatial cognition, including visuoperception and visual memory; future studies should aim to address the question of whether these particular domains are affected in HIV-MCI—as they have been shown to be affected in aging MCI studies (Clark et al. 2013).
Finally, a few words regarding the extent to which consideration of MCI in HIV disease is warranted given the widely used Frascati criteria (Antinori et al. 2007). Indeed, there are present controversies about the extent to which milder forms of HAND represent clinically valuable diagnostic entities (Nightingale et al. 2014). The current nomenclature for diagnosing asymptomatic HAND (ANI) requires intact daily functioning and neurocognitive deficits in at least two domains that are attributable to HIV infection (Antinori et al. 2007; Blackstone et al. 2012). A recent longitudinal study by Grant et al. (2014) demonstrated that ANI is associated with an increased risk for earlier development of symptomatic HAND, which requires that HIV-associated deficits interfere with functional capabilities. The finding that MCI designations were highly associated with GDS suggests that the MCI criteria correspond to commonly used psychometric approaches in HIV; however, our data also show that the two criteria-based methods of determining impairment have only a very slight correspondence. Although the negative diagnostic agreement was strong (81 %), the positive diagnostic agreement was quite weak (31 %) with only 25 % of ANI subjects also meeting MCI criteria. In addition to MCI criteria being more liberal, there are domains considered by MCI criteria but not by ANI (i.e., language, visuoperception), and domains included in ANI criteria but not in those for MCI (e.g., motor), which warrant additional inquiries into whether MCI-specific domains decline due to HIV infection. A few additional findings increase our confidence that the elevated MCI risk observed in this HIV+ cohort is not simply an alternate manifestation of ANI. First, there were no significant associations between MCI and traditional HIV disease markers (e.g., nadir CD4); in fact, there are a growing number of studies in the cART era showing that clinical factors other than HIV disease severity are more strongly predictive of neurocognitive impairment in infected cohorts (Becker et al. 2009). Second, and relatedly, this was a well-managed HIV+ sample that was on effective cART, thereby further decreasing the likelihood that the MCI findings are exclusively an artifact of ANI. Finally, we observed a strong age-associated risk of MCI in this HIV+ group, which is interpretively important because age is historically the strongest risk factor for MCI among seronegatives (for review, see Mariani et al. 2007). Moreover, a post hoc analysis showed that older age (over 60 years) was not associated with ANI in this elderly HIV+ group, χ 2 (1) = 0.15, p = .903, thereby providing some evidence of dissociability of key predictors for ANI and MCI. Nevertheless, determining the extent to which MCI criteria maintain poor sensitivity or superior specificity relative to existing criteria should be a point of emphasis in future studies. Thus, it remains an empirical question whether these related systems have current and prognostic clinical value, and future longitudinal investigations should determine the extent to which MCI criteria allow for better predictions of non-HIV related dementias in persons living with HIV infection.
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. Washington, DC: Author
Ances BM, Benzinger TL, Christensen JJ, Thomas J, Venkat R, Teshome M, Aldea P, Fagan AM, Holtzman DM, Morris JC, Clifford DB (2012) 11C-PiB imaging of human immunodeficiency virus-associated neurocognitive disorder. Arch Neurol 69:72–77. doi:10.1001/archneurol.2011.761
Anstey KJ, Cherbuin N, Eramudugolla R, Sargent-Cox K, Easteal S, Kumar R, Sachdev P (2013) Characterizing mild cognitive disorders in the young-old over 8 years: prevalence, estimated incidence, stability of diagnosis, and impact on IADLs. Alzheimers Dement 9:640–648. doi:10.1016/j.jalz.2012.11.013
Antinori A, Arendt G, Becker JT, Brew BJ, Byrd DA, Cherner M, Clifford DB, Cinque P, Epstein LG, Goodkin K, Gisslen M, Grant I, Heaton RK, Joseph J, Marder K, Marra CM, McArthur JC, Nunn M, Price RW, Pulliam L, Robertson KR, Sacktor N, Valcour V, Wojna VE (2007) Updated research nosology for HIV-associated neurocognitive disorders. Neurology 69:1789–1799. doi:10.1212/01.WNL.0000287431.88658.8b
Army Individual Test Battery (1944) Manual of directions and scoring. War Department, Adjutant General’s Office, Washington, DC
Becker JT, Kingsley L, Mullen J, Cohen B, Martin E, Miller EN, Ragin A, Sacktor N, Selnes OA, Visscher BR, Multicenter AIDS Cohort Study (2009) Vascular risk factors, HIV serostatus, and cognitive dysfunction in gay and bisexual men. Neurology 73:1292–1299. doi:10.1212/WNL.0b013e3181bd10e7
Bickel H, Mosch E, Seigerschmidt E, Siemen M, Forstl H (2006) Prevalence and persistence of mild cognitive impairment among elderly patients in general hospitals. Dement Geriatr Cogn Disord 21:242–250. doi:10.1159/000091397
Blackstone K, Moore DJ, Heaton RK, Franklin DR, Woods SP, Clifford DB, Collier AC, Marra CM, Gelman BB, McArthur JC, Morgello S, Simpson DM, Rivera-Mindt M, Deutsch R, Ellis RJ, Hampton Atkinson J, Grant I, CHARTER Group (2012) Diagnosing symptomatic HIV-associated neurocognitive disorders: self-report versus performance-based assessment of everyday functioning. J Int Neuropsychol Soc 18:79–88. doi:10.1017/S135561771100141X
Bondi MW, Edmonds EC, Jak AJ, Clark LR, Delano-Wood L, McDonald CR, Nation DA, Libon DJ, Au R, Galasko D, Salmon DP (2014) Neuropsychological criteria for mild cognitive impairment improves diagnostic precision, biomarker associations, and progression rates. J Alzheimers Dis 42:275–289. doi:10.3233/JAD-140276
Brew BJ, Pemberton L, Blennow K, Wallin A, Hagberg L (2005) CSF amyloid beta42 and tau levels correlate with AIDS dementia complex. Neurology 65:1490–1492. doi:10.1212/01.wnl.0000183293.95787.b7
Brooks JT, Buchacz K, Gebo KA, Mermin J (2012) HIV infection and older Americans: the public health perspective. Am J Public Health 102:1516–1526. doi:10.2105/AJPH.2012.300844
Busse A, Hensel A, Gühne U, Angermeyer MC, Riedel-Heller SG (2006) Mild cognitive impairment: long-term course of four clinical subtypes. Neurology 67:2176–2185. doi:10.1212/01.wnl.0000249117.23318.e1
Carey CL, Woods SP, Rippeth JD, Gonzalez R, Moore DJ, Marcotte TD, Grant I, Heaton RK, The HNRC Group (2004) Initial validation of a screening battery for the detection of HIV-associated cognitive impairment. Clin Neuropsychol 18:234–248. doi:10.1080/13854040490501448
Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 U.S. dependent areas—2010. HIV Surveillance Supplemental Report 2012;17(No. 3, part A). http://www.cdc.gov/hiv/topics/surveillance/resources/reports/. Published June 2012
Clark LR, Delano-Wood L, Libon DJ, McDonald CR, Nation DA, Bangen KJ, Au R, Salmon DP, Bondi MW (2013) Are empirically-derived subtypes of mild cognitive impairment consistent with conventional subtypes? J Int Neuropsychol Soc 19:635–645. doi:10.1017/S1355617713000313
Culbertson WC, Zillmer EA (1999) The tower of London, Drexel University, research version: examiner’s manual. Multi-Health Systems, North Tonawanda
Damian M, Hausner L, Jekel K, Richter M, Froelich L, Almkvist O, Boada M, Bullock R, De Deyn PP, Frisoni GB, Hampel H, Jones RW, Kehoe P, Lenoir H, Minthon L, Olde Rikkert MGM, Rodriguez G, Scheltens P, Soininen H, Spiru L, Touchon J, Tsolaki M, Vellas B, Verhey FRJ, Winblad B, Wahlund L, Wilcock G, Visser PJ (2013) Single-domain amnestic mild cognitive impairment identified by cluster analysis predicts Alzheimer’s disease in the European prospective DESCRIPA study. Dement Geriatr Cogn Disord 36:1–19. doi:10.1159/000348354
Delis DC, Kramer JH, Kaplan E, Ober BA (2000) The California verbal learning test, 2nd edn. The Psychological Corporation, San Antonio
Edmonds EC, Delano-Wood L, Clark LR, Jak AJ, Nation DA, McDonald CR, Libon DJ, Au R, Galasko D, Salmon DP, Bondi MW, Alzheimer’s Disease Neuroimaging Initiative (2014) Susceptibility of the conventional criteria for mild cognitive impairment to false-positive diagnostic errors. Alzheimers Dement. doi:10.1016/j.jalz.2014.03.005
Fazeli PL, Doyle KL, Scott JC, Iudicello JE, Casaletto KB, Weber E, Moore DJ, Morgan EE, Grant I, Woods SP, HNRP Group (2014) Shallow encoding and forgetting are associated with dependence in instrumental activities of daily living among older adults living with HIV infection. Arch Clin Neuropsychol 29:278–288. doi:10.1093/arclin/acu009
Ferman TJ, Smith GE, Kantarci K, Boeve BF, Pankratz VS, Dickson DW, Graff-Radford NR, Wszolek Z, Van Gerpen J, Uitti R, Pedraza O, Murray ME, Aakre J, Parisi J, Knopman DS, Petersen RC (2013) Nonamnestic mild cognitive impairment progresses to dementia with Lewy bodies. Neurology 81:2032–2038. doi:10.1212/01.wnl.0000436942.55281.47
Gandhi NS, Skolasky RL, Peters KB, Moxley RT, Creighton J, Roosa HV, Selnes OA, McArthur J, Sacktor N (2011) A comparison of performance-based measures of function in HIV-associated neurocognitive disorders. J Neurovirol 17:159–165. doi:10.1007/s13365-011-0023-8
Ganguli M, Snitz BE, Saxton JA, Chang C-CH, Lee CW, Vander Bilt J, Hughes TF, Loewenstein DA, Unverzagt FW, Petersen RC (2011) Outcomes of mild cognitive impairment by definition: a population study. Arch Neurol 68:761–767. doi:10.1001/archneurol.2011.101
Geurtsen GJ, Hoogland J, Goldman JG, Schmand BA, Tröster AI, Burn DJ, Litvan I, MDS Study Group on the Validation of PD-MCI Criteria (2014) Parkinson’s disease mild cognitive impairment: application and validation of the criteria. J Parkinsons Dis 4:131–137. doi:10.3233/JPD-130304
Goldman JG, Litvan I (2011) Mild cognitive impairment in Parkinson’s disease. Minerva Med 102:441–459
Goodglass H, Kaplan E, Barresi B (2001) Boston diagnostic aphasia examination, 3rd edn. Lippincott Williams Wilkins, Philadelphia
Grant I, Franklin DR, Deutsch R, Woods SP, Vaida F, Ellis RJ, Letendre SL, Marcotte TD, Atkinson JH, Collier AC, Marra CM, Clifford DB, Gelman BB, McArthur JC, Morgello S, Simpson DM, McCutchan JA, Abramson I, Gamst A, Fennema-Notestine C, Smith DM, Heaton RK, CHARTER Group (2014) Asymptomatic HIV-associated neurocognitive impairment increases risk for symptomatic decline. Neurology 82:2055–2062. doi:10.1212/WNL.0000000000000492
Green DA, Masliah E, Vinters HV, Beizai P, Moore DJ, Achim CL (2005) Brain deposition of beta-amyloid is a common pathologic feature in HIV positive patients. AIDS 19:407–411
Hänninen T, Hallikainen M, Tuomainen S, Vanhanen M, Soininen H (2002) Prevalence of mild cognitive impairment: a population-based study in elderly subjects. Acta Neurol Scand 106:148–154
Heaton RK, Marcotte TD, Mindt MR, Sadek J, Moore DJ, Bentley H, McCutchan JA, Reicks C, Grant I, HNRC Group (2004) The impact of HIV-associated neuropsychological impairment on everyday functioning. J Int Neuropsychol Soc 10:317–331. doi:10.1017/S1355617704102130
Heaton RK, Clifford DB, Franklin DR, Woods SP, Ake C, Vaida F, Ellis RJ, Letendre SL, Marcotte TD, Atkinson JH, Rivera-Mindt M, Vigil OR, Taylor MJ, Collier AC, Marra CM, Gelman BB, McArthur JC, Morgello S, Simpson DM, McCutchan JA, Abramson I, Gamst A, Fennema-Notestine C, Jernigan TL, Wong J, Grant I, CHARTER Group (2010) HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology 75:2087–2096. doi:10.1212/WNL.0b013e318200d727
Heaton RK, Franklin DR, Ellis RJ, McCutchan JA, Letendre SL, Leblanc S, Corkran SH, Duarte NA, Clifford DB, Woods SP, Collier AC, Marra CM, Morgello S, Mindt MR, Taylor MJ, Marcotte TD, Atkinson JH, Wolfson T, Gelman BB, McArthur JC, Simpson DM, Abramson I, Gamst A, Fennema-Notestine C, Jernigan TL, Wong J, Grant I, CHARTER Group, HNRC Group (2011) HIV-associated neurocognitive disorders before and during the era of combination antiretroviral therapy: differences in rates, nature, and predictors. J Neurovirol 17:3–16. doi:10.1007/s13365-010-0006-1
High KP, Brennan-Ing M, Clifford DB, Cohen MH, Currier J, Deeks SG, Deren S, Effros RB, Gebo K, Goronzy JJ, Justice AC, Landay A, Levin J, Miotti PG, Munk RJ, Nass H, Rinaldo CR, Shlipak MG, Tracy R, Valcour V, Vance DE, Walston JD, Volberding P, OAR Working Group on HIV and Aging (2012) HIV and aging: state of knowledge and areas of critical need for research. A report to the NIH office of AIDS research by the HIV and Aging Working Group. J Acquir Immune Defic Syndr 60(Suppl 1):S1–S18. doi:10.1097/QAI.0b013e31825a3668
Iudicello JE, Woods SP, Deutsch R, Grant I, HNRP Group (2012) Combined effects of aging and HIV infection on semantic verbal fluency: a view of the cortical hypothesis through the lens of clustering and switching. J Clin Exp Neuropsychol 34:476–488. doi:10.1080/13803395.2011.651103
Jak AJ, Bangen KJ, Wierenga CE, Delano-Wood L, Corey-Bloom J, Bondi MW (2009) Contributions of neuropsychology and neuroimaging to understanding clinical subtypes of mild cognitive impairment. Int Rev Neurobiol 84:81–103. doi:10.1016/S0074-7742(09)00405-X
Karnofsky DA, Burchenal JH (1949) The clinical evaluation of chemo-therapeutic agents in cancer. In: Maclead CM (ed) Evaluation of chemotherapeutic agents. Columbia University Press, New York, pp 191–205
Kløve H (1963) Grooved pegboard. Lafayette Instruments, Indiana
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Lopez OL, Jagust WJ, DeKosky ST, Jagust WJ, DeKosky ST, Becker JT, Fitzpatrick A, Dulberg C, Breitner J, Lyketsos C, Jones B, Kawas C, Carlson M, Kuller LH (2003) Prevalence and classification of mild cognitive impairment in the Cardiovascular Health Study Cognition Study: part 1. Arch Neurol 60:1385–1389. doi:10.1001/archneur.60.10.1385
Maki PM, Cohen MH, Weber K, Little DM, Fornelli D, Rubin LH, Perschler P, Gould F, Martin E (2009) Impairments in memory and hippocampal function in HIV-positive vs HIV-negative women: a preliminary study. Neurology 72(19):1661–1668
Malaspina L, Woods SP, Moore DJ, Depp C, Letendre SL, Jeste D, Grant I, HNRP Group (2011) Successful cognitive aging in persons living with HIV infection. J Neurovirol 17:110–119. doi:10.1007/s13365-010-0008-z
Mariani E, Monastero R, Ercolani S, Mangialasche F, Caputo M, Feliziani FT, Vitale DF, Senin U, Mecocci P, ReGAI Study Group (2007) Vascular risk factors in mild cognitive impairment subtypes. Findings from the ReGAl project. Dement Geriatr Cogn Disord 24:448–456. doi:10.1159/000110653
McNair DM, Lorr M, Droppleman LF (1981) Profile of mood states. Educational and Industrial Testing Service, San Diego
Moore DJ, Masliah E, Rippeth JD, Gonzalez R, Carey CL, Cherner M, Ellis RJ, Achim CL, Marcotte TD, Heaton RK, Grant I, HNRC Group (2006) Cortical and subcortical neurodegeneration is associated with HIV neurocognitive impairment. AIDS 20:879–887. doi:10.1097/01.aids.0000218552.69834.00
Moore RC, Fazeli PL, Jeste DV, Moore DJ, Grant I, Woods SP, HNRP Group (2014) Successful cognitive aging and health-related quality of life in younger and older adults infected with HIV. AIDS Behav 18:1186–1197. doi:10.1007/s10461-014-0743-x
Morgan EE, Iudicello JE, Weber E, Duarte NA, Riggs PK, Delano-Wood L, Ellis R, Grant I, Woods SP, HNRP Group (2012) Synergistic effects of HIV infection and older age on daily functioning. J Acquir Immune Defic Syndr 61:341–348. doi:10.1097/QAI.0b013e31826bfc53
Nightingale S, Winston A, Letendre S, Michael BD, McArthur JC, Khoo S, Solomon T (2014) Controversies in HIV-associated neurocognitive disorders. Lancet Neurol 13:1139–1151. doi:10.1016/S1474-4422(14)70137-1
Petersen RC (2004) Mild cognitive impairment as a diagnostic entity. J Intern Med 256:183–194. doi:10.1111/j.1365-2796.2004.01388.x
Petersen RC, Roberts RO, Knopman DS, Geda YE, Cha RH, Pankratz VS, Boeve BF, Tangalos EG, Ivnik RJ, Rocca WA (2010) Prevalence of mild cognitive impairment is higher in men. The Mayo Clinic Study of Aging. Neurology 75:889–897. doi:10.1212/WNL.0b013e3181f11d85
Pfefferbaum A, Rogosa DA, Rosenbloom MJ, Chu W, Sassoon SA, Kemper CA, Deresinski S, Rohlfing T, Zahr NM, Sullivan EV (2014) Accelerated aging of selective brain structures in human immunodeficiency virus infection: a controlled, longitudinal magnetic resonance imaging study. Neurobiol Aging 35:1755–1768. doi:10.1016/j.neurobiolaging.2014.01.008
Piatt AL, Fields JA, Paolo AM, Tröster AI (1999) Action (verb naming) fluency as an executive function measure: convergent and divergent evidence of validity. Neuropsychologia 37:1499–1503
Plessis SD, Vink M, Joska JA, Koutsilieri E, Stein DJ, Emsley R (2014) HIV infection and the fronto-striatal system: a systematic review and meta-analysis of fMRI studies. AIDS 28:803–811. doi:10.1097/QAD.0000000000000151
Psychological Corporation (1997) WAIS-III and WMS-III technical manual. San Antonio, TX: Author
Psychological Corporation (2001) Manual for the Wechsler Test of Adult Reading (WTAR). San Antonio: Author
Reppermund S, Brodaty H, Crawford JD, Kochan NA, Draper B, Slavin MJ, Troller JN, Sachdev PS (2013) Impairment in instrumental activities of daily living with high cognitive demand is an early marker of mild cognitive impairment: the Sydney memory and ageing study. Psychol Med 43:2437–2445. doi:10.1017/S003329171200308X
Roberts RO, Knopman DS, Geda YE, Cha RH, Roger VL, Petersen RC (2010) Coronary heart disease is associated with non-amnestic mild cognitive impairment. Neurobiol Aging 31:1894–1902. doi:10.1016/j.neurobiolaging.2008.10.018
Schmitter-Edgecombe M, Woo E, Greeley DR (2009) Characterizing multiple memory deficits and their relation to everyday functioning in individuals with mild cognitive impairment. Neuropsychology 23:168–177. doi:10.1037/a0014186
Scott JC, Woods SP, Carey CL, Weber E, Bondi MW, Grant I, HNRC Group (2011) Neurocognitive consequences of HIV infection in older adults: an evaluation of the “cortical” hypothesis. AIDS Behav 15:1187–1196. doi:10.1007/s10461-010-9815-8
Soontornniyomkij V, Moore DJ, Gouaux B, Soontornniyomkij B, Tatro ET, Umlauf A, Masliah E, Levine AJ, Singer EJ, Vinters HV, Gelman BB, Morgello S, Cherner M, Grant I, Achim CL (2012) Cerebral β-amyloid deposition predicts HIV-associated neurocognitive disorders in APOE ε4 carriers. AIDS 26:2327–2335. doi:10.1097/QAD.0b013e32835a117c
Su T, Schouten J, Geurtsen GJ, Wit FW, Stolte IG, Prins M, Portegies P, Caan MWA, Reiss P, Majoie CB, Schmand BA, AGEhIV Cohort Study Group (2015) Multivariate normative comparison, a novel method for more reliably detecting cognitive impairment in HIV infection. AIDS 29:547–557. doi:10.1097/QAD.0000000000000573
Summers MJ, Saunders NLJ (2012) Neuropsychological measures predict decline to Alzheimer’s dementia from mild cognitive impairment. Neuropsychology 26:498–508. doi:10.1037/a0028576
Valcour V, Shikuma C, Shiramizu B, Watters M, Poff P, Selnes O, Holck P, Grove J, Sacktor N (2004) Higher frequency of dementia in older HIV-1 individuals: the Hawaii Aging with HIV-1 Cohort. Neurology 63:822–827
Van Gorp WG, Miller EN, Satz P, Visscher B (1989) Neuropsychological performance in HIV-1 immunocompromised patients: a preliminary report. J Clin Exp Neuropsychol 11:763–773. doi:10.1080/01688638908400930
Ward A, Arrighi HM, Michels S, Cedarbaum JM (2012) Mild cognitive impairment: disparity of incidence and prevalence estimates. Alzheimers Dement 8:14–21. doi:10.1016/j.jalz.2011.01.002
Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund L-O, Nordberg A, Bäckmkan L, Albert M, Almkvist O, Arai H, Basun H, Blennow K, de Leon M, DeCarli C, Erkinjuntti T, Giacobini E, Graff C, Hardy J, Jack C, Jorm A, Ritchie K, van Duijn C, Visser P, Petersen RC (2004) Mild cognitive impairment—beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med 256:240–246. doi:10.1111/j.1365-2796.2004.01380.x
Woods SP, Morgan EE, Dawson M, Scott JC, Grant I, HNRC Group (2006) Action (verb) fluency predicts dependence in instrumental activities of daily living in persons infected with HIV-1. J Clin Exp Neuropsychol 28:1030–1042. doi:10.1080/13803390500350985
Woods SP, Hoebel C, Pirogovsky E, Rooney A, Cameron MV, Grant I, Gilbert PE, HNRP Group (2013) Visuospatial temporal order memory deficits in older adults with HIV infection. Cogn Behav Neurol 26:171–180. doi:10.1097/WNN.0000000000000013
Acknowledgments
The San Diego HIV Neurobehavioral Research Program [HNRP] group is affiliated with the University of California, San Diego; the Naval Hospital, San Diego; and the Veterans Affairs San Diego Healthcare System; and includes the following: Director: Igor Grant, M.D.; Co-Directors: J. Hampton Atkinson, M.D., Ronald J. Ellis, M.D., Ph.D., and J. Allen McCutchan, M.D.; Center Manager: Thomas D. Marcotte, Ph.D.; Jennifer Marquie-Beck, M.P.H.; Melanie Sherman; Neuromedical Component: Ronald J. Ellis, M.D., Ph.D. (P.I.), J. Allen McCutchan, M.D., Scott Letendre, M.D., Edmund Capparelli, Pharm.D., Rachel Schrier, Ph.D., Debra Rosario, M.P.H., Neurobehavioral Component: Robert K. Heaton, Ph.D. (P.I.), Mariana Cherner, Ph.D., Jennifer E. Iudicello, Ph.D., David J. Moore, Ph.D., Erin E. Morgan, Ph.D., Matthew Dawson; Neuroimaging Component: Terry Jernigan, Ph.D. (P.I.), Christine Fennema-Notestine, Ph.D., Sarah L. Archibald, M.A., John Hesselink, M.D., Jacopo Annese, Ph.D., Michael J. Taylor, Ph.D.; Neurobiology Component: Eliezer Masliah, M.D. (P.I.), Cristian Achim, M.D., Ph.D., Ian Everall, FRCPsych., FRCPath., Ph.D. (Consultant); Neurovirology Component: Douglas Richman, M.D., (P.I.), David M. Smith, M.D.; International Component: J. Allen McCutchan, M.D., (P.I.); Developmental Component: Cristian Achim, M.D., Ph.D.; (P.I.), Stuart Lipton, M.D., Ph.D.; Participant Accrual and Retention Unit: J. Hampton Atkinson, M.D. (P.I.); Data Management Unit: Anthony C. Gamst, Ph.D. (P.I.), Clint Cushman (Data Systems Manager); Statistics Unit: Ian Abramson, Ph.D. (P.I.), Florin Vaida, Ph.D., Reena Deutsch, Ph.D., Anya Umlauf, M.S.. David P. Sheppard, Jennifer E. Iudicello, Mark W. Bondi, Katie L. Doyle, Erin E. Morgan, Paul J. Massman, Paul E. Gilbert, and Steven Paul Woods have no financial conflicts of interest related to this work. The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, nor the US Government. The authors thank Marizela Cameron and P. Katie Riggs for their help with study management and Donald Franklin and Stephanie Corkran for their help with data processing. This study was supported by NIH grants R01-MH073419, T32-DA31098, L30-DA0321202, P30-MH62512, and K24-AG026431.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sheppard, D.P., Iudicello, J.E., Bondi, M.W. et al. Elevated rates of mild cognitive impairment in HIV disease. J. Neurovirol. 21, 576–584 (2015). https://doi.org/10.1007/s13365-015-0366-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-015-0366-7