Abstract
Although the induction of the cellular DNA damage response by herpes simplex virus-1 (HSV-1) infection of epithelial cells in tissue culture promotes productive infection, there has been no experimental observation of the effect of the cellular DNA damage response on HSV-1 infection in vivo or in neuronal derived cell lines in tissue culture. Thus, it has been speculated that the lack of cellular DNA damage induction during infection of neurons may promote latency in these cells. This work examines the profile of HSV-1 promoter induction and protein expression, in the absence or presence of infection; using cellular DNA damage inducing topoisomerase inhibitors (Camptothecin and Etoposide) on a neuroblastoma cell line (C1300) in which HSV-1 infection fails to induce the DNA damage response. In the absence of infection, a plasmid expressing the immediate early ICP0 promoter was the most induced by the DNA damage drug treatments compared to the early (RR) and late (VP16) gene promoters. Similarly, drug treatment of C1300 cells infected with HSV-1 virus showed enhanced protein expression for ICP0, but not ICP4 and VP16 proteins. However, when the cells were infected with a HSV-1 virus defective in the immediate early gene trans-activator VP16 (in814) and treated with the DNA damaging drugs, there was enhanced expression of immediate early and late HSV-1 proteins. Although, viral infection of the neuroblastoma cell alone did not induce DNA damage, cellular DNA damage induced by drug treatments facilitated viral promoter induction and viral protein expression. This implicates a mechanism by which HSV-1 viral genes in a quiescent or latent state may become induced by cellular DNA damage in neuronal cells to facilitate productive infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Herpes simplex virus-1 (HSV-1) is an alphaherpesvirus which infects both dividing cells (epithelial cells) and non-dividing cells (neurons). In the former cell type, lytic development ensues, while in the latter latency can be established. The latent genomes can reactivate in the neurons, and following anterograde movement of viral particles by fast axonal transport to the initial site of infection at the epithelium, begin another cycle of lytic infection. The cascade of infection, latency and reactivation lasts for the lifetime of the infected individual.
The mechanism of HSV-1 lytic infection is well understood, unlike the process of latency and reactivation. Latency establishment seems to be dependent on the size of initial infection (Preston 2007; Sawtell 1998) versus the efficiency of the host immune response, which counters the viral assault (Freeman et al. 2007; Leib et al. 1999; Pasieka et al. 2008). Once latency is established, the virus is maintained in the neurons. This maintenance is commonly associated with sporadic reactivation episodes. HSV-1 recurrence is one of the leading causes of blindness in industrialized nations (Perng and Jones 2010) and can also lead to encephalitis and death (Gebhardt et al. 2009; Mailles and Stahl 2009).
Stress has been implicated as a cause of reactivation. In human studies, it has been shown that mental stress correlates with HSV-1 reactivation in latently infected individuals (Freeman et al. 2007). In animal models, reactivation-inducing stressors include heat shock (Loiacono et al. 2003; Preston and Nicholl 2008; Sawtell and Thompson 1992), irradiation (Loiacono et al. 2003), and chemicals inducers (Bloom et al. 1994; Colgin et al. 2001; Preston and Nicholl 2008). Nonetheless, the cascade of viral gene induction for reactivation is not known. Both ICP0 (Everett 2000; Halford and Schaffer 2001) and VP16 (Miller et al. 2006; Thompson et al. 2009) proteins have been reported as the primary component for reactivation. Given that viral protein expression has not been detected in latently infected neurons (Derfuss et al. 2009; Loiacono et al. 2003), the induction of these genes from the latent genome has not been characterized. There have been in vitro studies in non-neuronal cells showing induction of HSV-1 gene promoters during stress in the absence of any viral proteins (Kushnir et al. 2009) that implicates the ability of cellular transcription factors to induce HSV-1 promoters. This is not surprising as HSV-1, like many other animal viruses (Machida et al. 2010; Schwartz et al. 2007; Shin et al. 2006), has manipulated the cellular machinery in various ways to promote its infectivity (Everett et al. 1998; Wysocka et al. 2003; Zhu et al. 2004). For example, HSV-1 recruits the cellular host cell factor-1 (HCF-1) and ocotomer-1 (OCT-1) to form a complex with virion protein VP16 to initiate lytic infection (Wysocka and Herr 2003).
In this study, we examined the effects of cellular DNA damage on HSV-1 promoter induction in the absence of viral proteins as well as HSV-1 protein expression during cellular DNA damage in a neuroblastoma cell line (C1300). It is known that DNA damage caused by irradiation can induce HSV-1 reactivation in animal (Goade et al. 2001; Laycock et al. 1991; Shimeld et al. 1990; Suzuki et al. 1994) and cellular models (Colgin et al. 2001; Zurlo and Yager 1984). Interestingly, HSV-1 infection of non-neuronal cells induces the ATM (ataxia telangiectasia mutated) branch of the DNA damage pathway and abrogation of components of this pathway leads to a decrease in HSV-1 infection (Lilley et al. 2005). However, the DNA damage pathway is not induced during infection of differentiated neuronal cells (Lilley et al. 2005). This failure to activate the DNA damage pathway has been speculated as influential in the establishment of HSV-1 latency in this cell type (Lilley et al. 2005). Although, HSV-1 infection cannot induce the DNA damage pathway in mature neurons, this pathway is functional and inducible by internal and external factors (De Zio et al. 2012; Fishel et al. 2007; Ramos-Espinosa et al. 2012). Here, we show that non-virally induced cellular DNA damage can promote HSV-1 infection in neurons similarly to virally induced DNA damage during infection of non-neuronal cells.
Materials and methods
Cell lines and viruses
C1300 cells were purchased from the ATCC. Cells were maintained in DMEM with 10%FBS. The HSV-1 strains used in this work were in1814 (VP16 insertion mutant) (Ace et al. 1989) and its wild type 17+ virus.
Plasmid
The pGL3 promoter vector (Promega) was used as backbone to construct HSV-1 promoter encoding plasmids where the promoters can drive expression of a luciferase cassette. The ribonucleotide reductase (RR) promoter was PCR amplified from HSV-1 genomic DNA strain 17+ using the forward primer: 5′-gtgaggtcgtgacgacg-3′ and reverse primer: 5′-ttcaacagacgcggcg-3′ and cloned into the SmaI–HindIII site in the pGL3 plasmid. The VP16 promoter construct was constructed same as RR using the forward primer: 5′-tgggtggggtt-3′ and the reverse primer: 5′-ccaaggaagagcgtccg-3′. An immediate early CMV-promoter control plasmid was made by removal of the CMV promoter region from pcDNA3 plasmid using BglII and HindIII enzymes and cloned into pGL3 digested with same enzyme. The ICP0 construct was a gift from Dr. David Leib (Dartmouth).
Transfection/infection experiment
C1300 cells were transfected with HSV-1 promoter plasmids or the CMV plasmid. The following day, cells were infected with McKrae virus at MOI of 5 for 1 h at 37 °C. Virus was removed and fresh media added and incubation was continued for 16 h. Cells were washed in 1× PBS and lysed. Next, a Bradford assay was done for protein normalization followed by the measurement of luciferase expression as per manufacturer’s instructions (Promega).
Stress conditions
C1300 cells were transfected with promoter plasmid constructs for 4 h. Transfection media was replaced with fresh DMEM and 10 % FBS and allowed to incubate 20 h. Cells were treated with the drugs Etoposide and Camptothecin (Sigma-Aldrich). Cells were lysed and protein contents were normalized using Bradford assay according to the manufacturer’s instruction (Bio-Rad). The cell lysates were used to determine luciferase expression as per the manufacturer’s instructions (Promega) or for Western blot analysis.
Infection
C1300 cells were infected with in1814 (VP16 insertion mutant) or 17+ virus for 1 h at 37 °C with hand agitation every 15 min. Virus was removed and fresh media was added in the presence of 100 μM Etoposide or 5 mM hexamethylene bisacetamide (HMBA). Cells were lysed at 3 or 8 h using RIPA buffer (Pierce). Protein contents were quantitated by Bradford assay and subjected to Western blotting.
Results
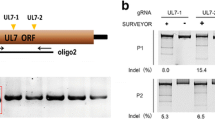
The HSV-1 promoter constructs are inducible during lytic infection
The promoter regions relating to the three classes of HSV-1 genes were cloned into the pGL3 plasmid to drive expression of a luciferase cassette (as described in the Methods). The promoters were derived from HSV-1 genes ICP0 (α gene), RR (β gene) and VP16 (γ gene). The immediate early cytomegalovirus (CMV) promoter was also cloned into the pGL3 plasmid to serve as a positive control for gene expression. To determine the functionality of the promoter constructs, C1300 cells were transfected with each plasmid followed by HSV-1 infection of the transfected cells for 16 h. The expression of luciferase served as the parameter for quantitating promoter activity. The results (Fig. 1) show that all the promoter constructs were significantly induced by co-infection compared to uninfected and induction of the ICP0 promoter was enhanced significantly more than the induced RR and VP16 promoters. Furthermore, it was interesting to note that the CMV promoter construct was also induced after HSV-1 infection. However, as expected, non-transfected cells (cell) did not show improved luciferase expression after infection.
HSV-1 promoter constructs induced by co-infection. C1300 cells were transfected with luciferase cassette encoding plasmids pGL3-ICP0 (ICP0), pGL3-Ribonucleotide reductase (RR), and pGl3-VP16 (VP16) or the positive control plasmid pGL3-CMV (CMV). Transfected and un-transfected (cell) samples were infected (bare) with HSV-1 virus at an m.o.i. of 5 for 16 h or left uninfected (black). Cells were lysed and protein contents were normalized using Bradford assay. Luciferase expression was quantitated using the luminoskan ascent machine (Thermo Electron Corporation). This figure is representative of two independent experiments. Each bar represents triplicate samples and one-way ANOVA and Tukey post-test were performed using PRISM statistical analysis software
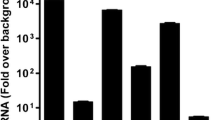
DNA damaging drugs increased ICP0 promoter activity in C1300 cells
Camptothecin and Etoposide, which are topoisomerase I and II inhibitors, respectively, were used to induce DNA damage in the C1300 cells. The cellular DNA damage pathway induction by dosage treatment with Camptothecin (Fig. 2a) and Etoposide (Fig. 2b) were measured through determination of the phosphorylation of histone H2Ax (γ-H2Ax). The dosages of 1, 5, 30, 100, 250, and 350 μM were used on pGL3-CMV transfected C1300 cells for 8 h and Western blot analysis showed Camptothecin induction of γ-H2Ax starting from 1 μM and continued up to 250 μM, followed by a decrease in H2Ax phosphorylation starting at 350 μM. While in the etoposide treated samples, γ-H2Ax was noticeably induced at 5 μM and continued to increase up to 100 μM and was similarly expressed at 250- and 350-μM concentrations. As controls, the level of unphosphorylated H2Ax and β-actin were used for normalization of protein expression in the cell. Subsequently, 5 μM of Camptothecin and 100 μM of Etoposide were used to treat C1300 cells transfected with pGL3 plasmids encoding the HSV-1 ICP0, RR or VP16 promoter and also a CMV promoter plasmid was used as a control for transfection efficiency. The induction of the promoters was measured through expression of a downstream luciferase cassette. Figure 2c and d shows luciferase expression from HSV-1 promoter plasmid transfected cells only (black bar) compared to drug treated transfected samples (stripped bar). The ICP0 promoter was significantly induced by the etoposide treatment (Fig. 2d) and there was around a 2-fold induction by Camptothecin treatment (Fig. 2c). Of note, Camptothecin treatment of infected fibroblast cells showed significant improvement in viral titer, although, the ICP0 promoter was induced by only 2-folds as observed here (Preston and McFarlane 1998). Neither drug treatments significantly affected RR and VP16 promoter activity under this experimental condition. Both drugs significantly induced the control CMV promoter (Fig. 2c and d).
DNA damaging drugs enhance ICP0 promoter directed expression of luciferase. C1300 cells were transfected with pGL3-CMV plasmid for 16 h and treated with DNA damage drugs Camptothecin (a) and Etoposide (b) at dosages of 1, 5, 30, 100, 250 and 350 μM. Controls were pGL3-CMV transfected only (drug-free) and cell only samples. Cells were washed in cold 1xPBS and lysed by RIPA buffer. Cell lysate were normalized using Bradford assay followed by determination of the protein levels of γH2Ax, H2Ax and β-actin by Western blot. C1300 cells were transfected with HSV-1 promoter constructs pGL3-ICP0, pGL3-RR, pGL3-VP16 and the control plasmid pGL3-CMV. The next day, cells were treated with 5 μM Camptothecin (c) or 100 μM Etopside (d) for 24 h. Cells were washed with 1xPBS and lysed with Reporter lysis buffer. Bradford assay was performed on lysates to normalize protein levels followed by measurement of the level of luciferase expression using the luminoskan ascent machine (Thermo Electron corporation). Luciferease expression from transfected cells that were drug treated (bare) was compared to untreated cells (black). One-way ANOVA and Tukey post-test were performed using PRISM statistical analysis software
Cellular DNA damage enhances HSV-1 protein expression in C1300 cells
In order to determine the influence of cellular DNA damage on HSV-1 protein expression from the viral genome, C1300 cells were infected with wild type HSV-1 17+ virus (Fig. 3a) or VP16 mutant in1814 virus (Fig. 3b) and treated with 100 μM etoposide or 5 mM HMBA. HMBA is a compound that facilitates transcription of cellular (Bartholomeeusen et al. 2012) as well as viral genes (McFarlane et al. 1992). It has been shown to activate transcription through induction of the PI3K/Akt pathway (Contreras et al. 2007). HMBA treatment of cells can cause HIV-1 reactivation from latency (Contreras et al. 2007), HSV-1 infection enhancement (Hafezi et al. 2012), as well as cellular differentiation through modification in the cell transcriptional processes (Wei et al. 2011). Here, HMBA is used as a positive control for viral gene induction.
DNA damage increased the level of HSV-1 protein expression during infection. C1300 cells were infected with 17+ (a) or in1814 (b) virus and treated with 100 μM Etoposide (Etop) or 5 mM hexamethylene bisacetamide (HMBA) for 3 h. Vero cells were infected with in1814 virus (c). The in1814 infected cells were allowed to recover for 5 h in absence of drugs. Cells were lysed using RIPA buffer and protein lysates were normalized by Bradford assay. The level of HSV-1 proteins ICP4, ICP0 and VP16, as well as γ-H2Ax and β-actin were measured by Western blotting and compared with untreated infected cells (No treatment) and cell only (No virus) samples
The level of HSV-1 proteins ICP0, ICP4 and VP16 was determined by Western blotting. When cells were infected with HSV-1 17+ virus and treated with etoposide or HMBA, ICP0 protein expression was enhanced compared to infection only (No treatment) and cell only (No virus) samples (Fig. 3a). The finding in Fig. 2, which showed ICP0 promoter induction from transfected C1300 cells by etoposide treatment, supports this result. There was also some enhancement of VP16 protein by etoposide and HMBA compared to infection only, but ICP4 protein level was similar for all the infected samples. Strong γ-H2Ax induction by the etoposide treatment was shown. β-Actin was used as a loading control.
To get a broader sense of the effect of DNA damage on HSV-1 protein expression, a VP16 mutant virus with growth deficiency (in1814) was used to infect C1300 cells followed by treatment with etoposide and HMBA. In1814 has an insertion in the transactivating domain of its VP16 protein that abrogates its transactivating ability (Ace et al. 1989). The level of HSV-1 protein expression in drug treated samples was compared to the infected only sample (No treatment) (Fig. 3b). Surprisingly, ICP0 was not readily detected from any of the in1814 infected C1300 cell samples. However, infection of Vero cells with in1814 showed ICP0 expression (Fig. 3c). ICP0 was expressed at a lower level in C1300 cells compared to the other HSV-1 proteins analyzed even when wild type HSV-1 virus was used for infection (Fig. 3a). Unlike the wild type infection (Fig. 3c), ICP4 and VP16 protein levels were enhanced by etoposide and HMBA treatments with HSV-1 in1814 infection of C1300 cells (Fig. 3b). In addition, as has previously been reported, a DNA damage response is induced by HSV-1 virus infection of non-neuronal cells as demonstrated by γ-H2Ax expression in in1814 infected Vero cells (Fig. 3c) (Lilley et al. 2005). In contrast, infection alone could not induce a DNA damage response in the C1300 cells.
Discussion
The induction of the cellular DNA damage pathway can be restrictive to viral infection. Thus many viruses have evolved ways to disrupt the DNA damage pathway, to facilitate their infections (Ebina et al. 2012; Liang et al. 2006; Machida et al. 2010; Shin et al. 2006; Smith and Daniel 2011), while viruses, like HIV-1 and AAV, which cannot counter the cellular DNA damage response (DDR) are restricted by it (Cervelli et al. 2008; Ebina et al. 2012; Porteus et al. 2003; Schwartz et al. 2007; Smith and Daniel 2011).
HSV-1 has leveraged aspects of the cellular DDR induced by its infection in non-neuronal cells to facilitate its growth in these cells (Shirata et al. 2005). In brief, disruption of the ATR (Mohni et al. 2010; Wilkinson and Weller 2006) and DNA -PKcs (Lilley et al. 2005; Wilkinson and Weller 2006) pathways lead to enhanced HSV-1 infection, while ATM pathway activation supports HSV-1 infection (Lilley et al. 2005). In contrast, HSV-1 infection of differentiated neurons does not trigger the cell DDR as shown in this paper (Fig. 3) and the work of others (Lilley et al. 2005). However, it has been shown that the HSV-1 genome can become reactivated by ultraviolet light (UV)-induced DNA damage in vivo (Goade et al. 2001; Ichihashi et al. 2004; Laycock et al. 1991; Loiacono et al. 2003; Shimeld et al. 1990), and in vitro (Zurlo and Yager 1984) systems. Our results show that cellular DNA damage induced by a topoisomerase II enzyme inhibitor can enhance viral protein expression in a neuroblastoma cell line in which HSV-1 infection did not trigger the DNA damage response pathway, as measured by γ-H2Ax induction (Fig. 3). Additionally, the DNA damage treatment enhanced ICP0 promoter activity in the absence of any other viral genes and this may have implication for the mechanism of HSV-1 reactivation from neurons.
A determination of the factor(s) involved in inducing the ICP0 promoter during DNA damage may help in increasing our understanding of HSV-1 reactivation pathway. In this system, we used a cycling cancerous neuron-like cell line. The cancerous quality of the cell may influence its DNA damage profile, thus, it will be important to determine if the ICP0 promoter is similarly induced in healthy differentiated primary neurons. For such a system, ultraviolet light, irradiation or a non-cell-cycling-dependent drug may be used to induce DNA damage. It is well established that ultraviolet light can induce HSV-1 reactivation (Goade et al. 2001). UV causes DNA damage through production of cyclobutane pyrimidine dimers (CPD) and 6–4 photoproducts (6–4 PP), which can lead to the induction of the ATM/ATR pathways through DNA breaks (Rastogi et al. 2010; Sinha and Hader 2002).
It has been shown that UV can induce reactivation of HSV-1 virus from a mouse model (Goade et al. 2001) and this is supported by the finding of Ramos-Espinosa et al. showing the high susceptibility of neurons to ultraviolet mediated DNA damage compared to reactive oxygen species mediated damage (Ramos-Espinosa et al. 2012). Neurons are highly metabolic and produce high levels of ROS which can damage DNA and deficiency in DNA damage repair pathways in neurons is associated with many neurological diseases (Fishel et al. 2007). The two most active repair pathways in neurons are the base excision repair (BER) and nucleotide excision repair (NER) pathways (Fishel et al. 2007). The question to pose is how might these pathways influence HSV-1 life cycle in the neurons? There are two pathways to NER, which are the global genome repair (GG-NER) and transcription-coupled repair (TC-NER). GG-NER is not active in neurons, but they are fully capable of mounting a TC-NER response (Nouspikel and Hanawalt 2000, 2002; van der Wees et al. 2007). This creates a neuronal cell environment in which the DNA damage response induction is influenced not by the level of DNA damage, but rather by the location site of the damage in the genome. Consequently, understanding the effects of the threshold of DNA damage on HSV-1 reactivation may give us insight in the randomness/sporadic nature of this virus reactivation from neurons.
As demonstrated in this work, DNA damage in neurons induced HSV-1 ICP0 promoter in absence of all other viral proteins and also enhanced ICP0 expression during lytic infection in a neuron-like cell. ICP0 expression alone can induce HSV-1 reactivation (Halford et al. 2001) and as such has been suggested as the coordinator of HSV-1 reactivation (Everett 2000; Halford and Schaffer 2001).
References
Ace CI, McKee TA, Ryan JM, Cameron JM, Preston CM (1989) Construction and characterization of a herpes simplex virus type 1 mutant unable to transinduce immediate-early gene expression. J Virol 63:2260–2269
Bartholomeeusen K, Xiang Y, Fujinaga K, Peterlin BM (2012) BET bromodomain inhibition activates transcription via a transient release of P-TEFb from 7SK snRNP. J Biol Chem 284:36609–36616
Bloom DC, Devi-Rao GB, Hill JM, Stevens JG, Wagner EK (1994) Molecular analysis of herpes simplex virus type 1 during epinephrine-induced reactivation of latently infected rabbits in vivo. J Virol 68:1283–1292
Cervelli T, Palacios JA, Zentilin L, Mano M, Schwartz RA, Weitzman MD, Giacca M (2008) Processing of recombinant AAV genomes occurs in specific nuclear structures that overlap with foci of DNA-damage-response proteins. J Cell Sci 121:349–357
Colgin MA, Smith RL, Wilcox CL (2001) Inducible cyclic AMP early repressor produces reactivation of latent herpes simplex virus type 1 in neurons in vitro. J Virol 75:2912–2920
Contreras X, Barboric M, Lenasi T, Peterlin BM (2007) HMBA releases P-TEFb from HEXIM1 and 7SK snRNA via PI3K/Akt and activates HIV transcription. PLoS Pathog 3:1459–1469
De Zio D, Bordi M, Cecconi F (2012) Oxidative DNA damage in neurons: implication of ku in neuronal homeostasis and survival. Int J Cell Biol 2012:752420
Derfuss T, Arbusow V, Strupp M, Brandt T, Theil D (2009) The presence of lytic HSV-1 transcripts and clonally expanded T cells with a memory effector phenotype in human sensory ganglia. Ann N Y Acad Sci 1164:300–304
Ebina H, Kanemura Y, Suzuki Y, Urata K, Misawa N, Koyanagi Y (2012) Integrase-independent HIV-1 infection is augmented under conditions of DNA damage and produces a viral reservoir. Virology 427:44–50
Everett RD (2000) ICP0, a regulator of herpes simplex virus during lytic and latent infection. Bioessays 22:761–770
Everett RD, Freemont P, Saitoh H, Dasso M, Orr A, Kathoria M, Parkinson J (1998) The disruption of ND10 during herpes simplex virus infection correlates with the Vmw110- and proteasome-dependent loss of several PML isoforms. J Virol 72:6581–6591
Fishel ML, Vasko MR, Kelley MR (2007) DNA repair in neurons: so if they don't divide what's to repair? Mutat Res 614:24–36
Freeman ML, Sheridan BS, Bonneau RH, Hendricks RL (2007) Psychological stress compromises CD8+ T cell control of latent herpes simplex virus type 1 infections. J Immunol 179:322–328
Gebhardt BM, Focher F, Eberle R, Manikowski A, Wright GE (2009) Effect of combinations of antiviral drugs on herpes simplex encephalitis. Drug Des Devel Ther 3:289–294
Goade DE, Nofchissey RA, Kusewitt DF, Hjelle B, Kreisel J, Moore J, Lyons CR (2001) Ultraviolet light induces reactivation in a murine model of cutaneous herpes simplex virus-1 infection. Photochem Photobiol 74:108–114
Hafezi W, Lorentzen EU, Eing BR, Muller M, King NJ, Klupp B, Mettenleiter TC, Kuhn JE (2012) Entry of herpes simplex virus type 1 (HSV-1) into the distal axons of trigeminal neurons favors the onset of nonproductive, silent infection. PLoS Pathog 8:e1002679
Halford WP, Schaffer PA (2001) ICP0 is required for efficient reactivation of herpes simplex virus type 1 from neuronal latency. J Virol 75:3240–3249
Halford WP, Kemp CD, Isler JA, Davido DJ, Schaffer PA (2001) ICP0, ICP4, or VP16 expressed from adenovirus vectors induces reactivation of latent herpes simplex virus type 1 in primary cultures of latently infected trigeminal ganglion cells. J Virol 75:6143–6153
Ichihashi M, Nagai H, Matsunaga K (2004) Sunlight is an important causative factor of recurrent herpes simplex. Cutis 74:14–18
Kushnir AS, Davido DJ, Schaffer PA (2009) Role of NF-Y in stress-induced activation of the HSV-1 ICP0 promoter. J Virol 84:188–200
Laycock KA, Lee SF, Brady RH, Pepose JS (1991) Characterization of a murine model of recurrent herpes simplex viral keratitis induced by ultraviolet B radiation. Invest Ophthalmol Vis Sci 32:2741–2746
Leib DA, Harrison TE, Laslo KM, Machalek MA, Moorman NJ, Virgin HW (1999) Interferons regulate the phenotype of wild-type and mutant herpes simplex viruses in vivo. J Exp Med 189:663–672
Liang X, Pickering MT, Cho NH, Chang H, Volkert MR, Kowalik TF, Jung JU (2006) Deregulation of DNA damage signal transduction by herpesvirus latency-associated M2. J Virol 80:5862–5874
Lilley CE, Carson CT, Muotri AR, Gage FH, Weitzman MD (2005) DNA repair proteins affect the lifecycle of herpes simplex virus 1. Proc Natl Acad Sci U S A 102:5844–5849
Loiacono CM, Taus NS, Mitchell WJ (2003) The herpes simplex virus type 1 ICP0 promoter is activated by viral reactivation stimuli in trigeminal ganglia neurons of transgenic mice. J Neurovirol 9:336–345
Machida K, McNamara G, Cheng KT, Huang J, Wang CH, Comai L, Ou JH, Lai MM (2010) Hepatitis C virus inhibits DNA damage repair through reactive oxygen and nitrogen species and by interfering with the ATM-NBS1/Mre11/Rad50 DNA repair pathway in monocytes and hepatocytes. J Immunol 185:6985–6998
Mailles A, Stahl JP (2009) Infectious encephalitis in france in 2007: a national prospective study. Clin Infect Dis 49:1838–1847
McFarlane M, Daksis JI, Preston CM (1992) Hexamethylene bisacetamide stimulates herpes simplex virus immediate early gene expression in the absence of trans-induction by Vmw65. J Gen Virol 73:285–292
Miller CS, Danaher RJ, Jacob RJ (2006) ICP0 is not required for efficient stress-induced reactivation of herpes simplex virus type 1 from cultured quiescently infected neuronal cells. J Virol 80:3360–3368
Mohni KN, Livingston CM, Cortez D, Weller SK (2010) ATR and ATRIP are recruited to herpes simplex virus type 1 replication compartments even though ATR signaling is disabled. J Virol 84:12152–12164
Nouspikel T, Hanawalt PC (2000) Terminally differentiated human neurons repair transcribed genes but display attenuated global DNA repair and modulation of repair gene expression. Mol Cell Biol 20:1562–1570
Nouspikel T, Hanawalt PC (2002) DNA repair in terminally differentiated cells. DNA Repair (Amst) 1:59–75
Pasieka TJ, Lu B, Leib DA (2008) Enhanced pathogenesis of an attenuated herpes simplex virus for mice lacking Stat1. J Virol 82:6052–6055
Perng GC, Jones C (2010) Towards an understanding of the herpes simplex virus type 1 latency-reactivation cycle. Interdiscip Perspect Infect Dis 2010:262415
Porteus MH, Cathomen T, Weitzman MD, Baltimore D (2003) Efficient gene targeting mediated by adeno-associated virus and DNA double-strand breaks. Mol Cell Biol 23:3558–3565
Preston CM (2007) Reactivation of expression from quiescent herpes simplex virus type 1 genomes in the absence of immediate-early protein ICP0. J Virol 81:11781–11789
Preston CM, McFarlane M (1998) Cytodifferentiating agents affect the replication of herpes simplex virus type 1 in the absence of functional VP16. Virology 249:418–426
Preston CM, Nicholl MJ (2008) Induction of cellular stress overcomes the requirement of herpes simplex virus type 1 for immediate-early protein ICP0 and reactivates expression from quiescent viral genomes. J Virol 82:11775–11783
Ramos-Espinosa P, Rojas E, Valverde M (2012) Differential DNA damage response to UV and hydrogen peroxide depending of differentiation stage in a neuroblastoma model. Neurotoxicology
Rastogi RP, Richa KA, Tyagi MB, Sinha RP (2010) Molecular mechanisms of ultraviolet radiation-induced DNA damage and repair. J Nucleic Acids 2010:592980
Sawtell NM (1998) The probability of in vivo reactivation of herpes simplex virus type 1 increases with the number of latently infected neurons in the ganglia. J Virol 72:6888–6892
Sawtell NM, Thompson RL (1992) Rapid in vivo reactivation of herpes simplex virus in latently infected murine ganglionic neurons after transient hyperthermia. J Virol 66:2150–2156
Schwartz RA, Palacios JA, Cassell GD, Adam S, Giacca M, Weitzman MD (2007) The Mre11/Rad50/Nbs1 complex limits adeno-associated virus transduction and replication. J Virol 81:12936–12945
Shimeld C, Hill TJ, Blyth WA, Easty DL (1990) Reactivation of latent infection and induction of recurrent herpetic eye disease in mice. J Gen Virol 71(Pt 2):397–404
Shin YC, Nakamura H, Liang X, Feng P, Chang H, Kowalik TF, Jung JU (2006) Inhibition of the ATM/p53 signal transduction pathway by Kaposi's sarcoma-associated herpesvirus interferon regulatory factor 1. J Virol 80:2257–2266
Shirata N, Kudoh A, Daikoku T, Tatsumi Y, Fujita M, Kiyono T, Sugaya Y, Isomura H, Ishizaki K, Tsurumi T (2005) Activation of ataxia telangiectasia-mutated DNA damage checkpoint signal transduction elicited by herpes simplex virus infection. J Biol Chem 280:30336–30341
Sinha RP, Hader DP (2002) UV-induced DNA damage and repair: a review. Photochem Photobiol Sci 1:225–236
Smith JA, Daniel R (2011) Up-regulation of HIV-1 transduction in nondividing cells by double-strand DNA break-inducing agents. Biotechnol Lett 33:243–252
Suzuki N, Kimoto H, Koseki H, Miura N, Watanabe T, Inaba N, Takamizawa H, Hashizume S (1994) Human cell clones, RSa and UVr-1, differing in their capability for UV-induced virus reactivation and phenotypic mutation. Mutat Res 306:211–222
Thompson RL, Preston CM, Sawtell NM (2009) De novo synthesis of VP16 coordinates the exit from HSV latency in vivo. PLoS Pathog 5:e1000352
van der Wees C, Jansen J, Vrieling H, van der Laarse A, Van Zeeland A, Mullenders L (2007) Nucleotide excision repair in differentiated cells. Mutat Res 614:16–23
Wei M, Wang Z, Yao H, Yang Z, Zhang Q, Liu B, Yu Y, Su L, Zhu Z, Gu Q (2011) P27(Kip1), regulated by glycogen synthase kinase-3beta, results in HMBA-induced differentiation of human gastric cancer cells. BMC Cancer 11:109
Wilkinson DE, Weller SK (2006) Herpes simplex virus type I disrupts the ATR-dependent DNA-damage response during lytic infection. J Cell Sci 119:2695–2703
Wysocka J, Herr W (2003) The herpes simplex virus VP16-induced complex: the makings of a regulatory switch. Trends Biochem Sci 28:294–304
Wysocka J, Myers MP, Laherty CD, Eisenman RN, Herr W (2003) Human Sin3 deacetylase and trithorax-related Set1/Ash2 histone H3-K4 methyltransferase are tethered together selectively by the cell-proliferation factor HCF-1. Genes Dev 17:896–911
Zhu Q, Yao J, Wani G, Chen J, Wang QE, Wani AA (2004) The ubiquitin–proteasome pathway is required for the function of the viral VP16 transcriptional activation domain. FEBS Lett 556:19–25
Zurlo J, Yager JD (1984) U.v.-enhanced reactivation of u.v.-irradiated herpes virus by primary cultures of rat hepatocytes. Carcinogenesis 5:495–500
Acknowledgments
We thank Dr. David Leib (Dartmouth) for the ICP0 construct. We also thank Mark Boyer and Nick Ruskowski for excellent technical assistance. This work was supported by grants from NIH, NS-33768 and NS-29390. K.V. was supported by NIH training grant T32 DK-007748.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Volcy, K., Fraser, N.W. DNA damage promotes herpes simplex virus-1 protein expression in a neuroblastoma cell line. J. Neurovirol. 19, 57–64 (2013). https://doi.org/10.1007/s13365-012-0140-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-012-0140-z