Abstract
Cyclosporine has been established as a gold standard for its immunosuppressant action. Apart from this, the molecule is boon in treating broad spectrum of diseases like rheumatoid arthritis, psoriasis, and dry eye syndrome. The broad spectrum of cyclosporine demands efficient delivery systems by several routes. Neoral® and Sandimmune® are currently available formulations for oral route, whereas Restasis® is used for ocular delivery of cyclosporine. The available formulations serve the purpose only to a limited extent due to constraints like high molecular weight, low solubility, low permeability, bitter taste, and narrow therapeutic index of cyclosporine. Therefore, several novel formulations like microemulsion, self-emulsifying systems, nanoparticles, and microspheres were developed to overcome these constraints, exploring different routes like oral, ocular, and topical for cyclosporine. Additionally, iontophoresis and ultrasound-mediated delivery has also been studied to improve its poor permeability in topical delivery, whereas biodegradable implants were reported to increase the retention time in cornea and prolonged the release of cyclosporine by ocular route. Although these recent advances in cyclosporine delivery look promising, its clinical translation require in depth studies to deliver safe, efficacious, and stable formulation of cyclosporine. This review focuses on challenges of cyclosporine delivery and the recent advancements for overcoming the constraints.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cyclosporine is a neutral, lipophilic, cyclic undecapeptide with molecular weight of 1202 g/mol (Fig. 1). It is obtained naturally by extraction from Tolypocladium inflatum, Tolypocladium niveum, Aspergillus terreus, Penicillium fellutanum, and Aspergillus fumigatus [1]. Cyclosporine can also be synthesized chemically using N-methylated peptides via series of isonitrile coupling reaction [2, 3]. It has seven N-methylated peptide bonds, which have encouraged chemist to come up with an effective modification of these bonds to overcome the poor oral bioavailability (28%) of cyclosporine. Being a cyclic peptide, cyclosporine can easily penetrate the cells via passive diffusion which is the key facet of this wonder molecule [4]. Immense research has been carried out after the discovery of cyclosporine to develop several other N-methylated peptides which could not only impart receptor selectivity but also improve bioavailability [5]. Initially, it was investigated as an antifungal agent by Sandoz but clinical use was limited by its narrow spectrum. Later in 1976, the selective immunosuppressive action of cyclosporine was discovered and then it was emerged as a golden standard in immunopharmacology. The structural elucidation indicated that the active sites for immunosuppressive action are positions 1, 2, 3, and 11 [6].
Cyclosporine is effective against a broad spectrum of diseases however it is primarily explored for its use as an immunosuppressant [7]. Cyclosporine invention created an era of selective lymphocyte inhibition that aided in improving knowledge of technical, immunobiologically, and clinical aspects of transplantation [8]. Although cyclosporine cannot address all transplant-related complication, it definitely improved the incidence of chronic rejection and patient survival after organ transplantation. Cyclosporine was also explored for its local action to reduce pain in conditions like rheumatoid arthritis [9]. It is commonly used in treatment of psoriasis, atopic dermatitis, and toxic epidermal necrolysis [10]. Lately, cyclosporine has also used in treatment of chronic dry eye syndrome [11].
The journey of conventional formulations started with Sandimmune® oral solutions of cyclosporine (50 mg/mL and 100 mg/mL) by Sandoz. Later, Sandimmune® softgel capsules were brought into market to improve the patient compliance. Both Sandimmune® formulations were oil based, and it was hypothesized that these formulations were emulsified with the aid of bile salts in the gastrointestinal tract (GIT) upon oral administration. Consequently, the oral absorption of cyclosporine was critically influenced by the droplet size of in situ emulsion and the emulsification by pancreatic lipase. In this process, the meals rich in fat helped in enhancing bioavailability by increasing bile flow [12]. However, both Sandimmune® formulations exhibited large variation with respect to bioavailability and pharmacokinetics. Therefore, to improve pharmacokinetic properties of these formulations, Sandimmune® was converted into improved Neoral® formulations by innovator company. Neoral® was developed as microemulsion based formula which led to an immediate formation of dispersion when in contact with GIT fluid [13].
Since the new formulation is not dependent on bile secretion and food intake, comparatively improved absorption with less variability was observed. Neoral® solution showed a reduced droplet size of the microemulsion formed in the GIT which helped in further absorption. Neoral® served the purpose of improved drug delivery, but it was necessary to develop more efficacious and target specific drug delivery systems for cyclosporine which lead to intense research in this area. Recent patents of cyclosporine are listed in the Table 1, and list of marketed products (generic and brand) of cyclosporine is given in Table 2. Thus, this review article is based on comprehensive literature review on novel drug delivery system of cyclosporine with different routes of administration.
Mechanism of action of cyclosporine
Cyclosporine, an immunosuppressant, mainly targets the helper subset of T lymphocyte and lymphokine productions, which prevents the upregulation of immune system of the body after activating antigen presenting cell. T helper cell recognizes a foreign antigen which is in conjunction with self-antigen and activates CD4 and CD3 antigens [14, 15]. A series of reaction activates, which results in production and release of lymphokines and receptor expression which gives positive feedback T helper cell’s surface [16]. There are mainly two mechanisms reported by which cyclosporine acts in the body namely, “calcineurin/NFAT pathway” and “JNK and p38 signaling” pathways [17].
Calcineurin/NFAT pathway
Cyclosporine mainly acts by inhibition of T cells by blocking cytokines transcription genes like IL-2 and IL-4 [18]. Cyclosporine binds to T cells and attaches with cytosolic cyclophilins, abundant in clophilin T cell [19, 20]. This increases the intra-cellular calcium ion concentration which leads to activation of calmodulin. Calmodulin attaches to calcineurin A (calmodulin dependent protein phosphatase) and stimulates the auto-inhibitory action of calcineurin A which results in activation of phosphatases activity causing inflammation. However, cyclosporine and cyclophilin complex binds to calcineurin A and reduces the phosphatases activity, thereby reducing the inflammatory response [21, 22]. Family members of nuclear factor of activated T cell (NFAT) are dephosphorylated by calcineurin which allows the translocation into nucleus, showing genes expression by cis element NFAT [23]. De-phosphorylation by calcineurin inhibits the nuclear translocation of NFAT members, thus activating the T cells as depicted in Fig. 2.
Action on JNK and p38 signaling pathways
Recent studies show that the cyclosporine blocks both p38 and c-Jun N-terminal kinase (JNK) pathways in addition to calcineurin blocking activity [24]. Mitogen-activated protein kinase (MAPK) pathway is a mechanism in eukaryotic signaling cascade [25].
The distinct subgroups of MAPK are extracellular signal regulated kinase (ERK), JNK, and p38 in mammalian cell [26]. JNK and p38 work in stress response like inflammation and apoptosis [27, 28]. p38 signaling pathway stops the transcriptional activation of NFAT cis element consisting of binding site for AP1 and NFAT [29]. Thus, it shows the inhibition action of p38 and JNK by cyclosporine signifies the specificity for immunosuppressive action and, along with this, cyclosporine does not have any effect on ERK pathway activation [30].
Pharmacokinetics of cyclosporine
Cyclosporine is a lipophilic drug, which belongs to BCS class II which shows very poor solubility [31]. Pharmacokinetic of cyclosporine is characterized by irregular parameters and erratic oral bioavailability [32]. It shows slow and incomplete absorption from gastrointestinal tract (GIT) and gets predominantly absorbed from upper intestine [33]. The time when maximum concentration (tmax) of cyclosporine is attained is 1.5 to 2 h. The rate of absorption is affected by gastric motility, cholestasis, biliary diversion, steatorrhea, and reduced pancreatic secretion. It does not show pH-dependent solubility due to lack of ionizable functional groups. Interestingly, it shows unusual temperature-dependent solubility which is reported to be 106.1 μg/mL at 13 °C and 9.29 μg/mL at 38.5 °C [34]. This can be explained by the conformational change of the amino acid residue at position 8 which on loss of hydration water with increasing temperature affects the conformation of cyclosporine and subsequently its solubility [35]. There is a significant difference between the bioavailability of cyclosporine in various populations. African-American shows decreased bioavailability and low absorption as compared to whites [36]. This is because of variation in the frequency of polymorphisms in MDR1 and CYP3A enzyme gene encoding [37, 38].
Cyclosporine mostly binds to the lipoproteins of high, low, and very low density that acts as reservoir [39]. When the serum cholesterol level is above 3.1 mmol/Lit, cyclosporine shows toxic effect but surprisingly hypertriglyceridemia reduces the side effect. The volume of distribution is from 4 to 8 Lit per kg of body weight. Tissue contents of cytoplasmic binding show the slow accumulation of cyclosporine which retains for months, even after the discontinuation of therapy. Deposition of drug is found majorly in the liver, pancreas, kidney, heart, muscular tissue, and lungs.
The isoenzyme, cytochrome P-450, converts the cyclosporine in its metabolites retaining the cyclic structure with higher polarity. The biotransformation starts with hydroxylation on gamma or eta position of amino acids, intermolecular formation of tetrahydrofuran ether at first amino acid, and demethylation of fourth amino acid. Some metabolites are formed in second step by demethylation and hydroxylation. M1 and M17 are metabolites formed by hydroxylation of amino acids at positions 1 and 9 which exhibit considerable immunosuppressant effect. In contrast, M8 which is also formed by hydroxylation of amino acids at positions 1 and 9 and M21 which has an N-methylated amino acid at position 4 exhibited evidently reduced immunosuppressive activity when compared to cyclosporine [40]. Almost 90% of cyclosporine elimination is mainly by metabolism, having a half-life of 6 to 8 h, and the clearance rate is 2 to 32 mL/kg, varying from patient to patient. Higher dose is required for children as they show higher clearance rate than adults.
It does not produce mutagenicity or tumor induction in animals in vivo or in vitro. There are 20% chances of cyclosporine to cross blood–brain barrier in kidney recipients and liver transplants [41]. Cyclosporine oral suspension overdose causes mild syndromes like stomach upset, hypertension, flushing, and dysesthesias. A common complication among the transplant recipients is acute pancreatitis. It increases the level of serum prolactin and decreases the testosterone level which causes gynecomastia in males [42].
Cyclosporine has large inter- and intra-patient variabilities in absorption, and being a narrow therapeutic index drug, it has the potential to induce nephrotoxicity [43]. The irreversible morphological alterations in the kidney are major limiting factor for the use of cyclosporine. Due to the risk of nephrotoxicity, the dosage guidelines has been established to recommend an upper dose limit of 5 mg/kg/day and reduction in dose is also advisable when serum creatinine is raised by more than 30% of pre-treatment values [44]. Thus, therapeutic drug monitoring is essential for cyclosporine therapy as it has a high potential of exhibiting permanent toxicity to the kidney [45].
Constraints in drug delivery of cyclosporine
Belonging to BCS class II, cyclosporine has low solubility results into reduced absorption and consequently scarce bioavailability which is the underlying constraint in oral delivery and restricts its use as an oral immunosuppressant. The taste of cyclosporine is bitter which restrains patient compliance on oral administration [46]. Structurally, it is a high molecular weight compound which hinders its permeability, thereby limiting its use in treatment of dermatological disorders like pyoderma gangrenosum, atopic dermatitis, toxic epidermal necrolysis, and psoriasis [47]. In case of rheumatoid arthritis where cyclosporine is used to reduce the inflammation locally, permeability and penetration of cyclosporine are major loopholes. Cyclosporine is susceptible to enzyme degradation and poor corneal transfer, draining with tears which cause hindrance in its ocular delivery, hence limiting its use in treatment of chronic dry eye syndrome [48]. Another limiting parameter in ocular delivery is lack of predictive animal models available for ocular drug evaluation. Although cyclosporine has transformed various treatment therapies, its use is restricted due to the marginal difference between immunosuppression and nephrotoxicity [49]. It exhibits variable pharmacokinetic parameters leading to drastic differences in absorption profile. Age, race, and concomitant drug regimen are demographic factors affecting pharmacokinetic profile in given patient [50]. Erratic pharmacokinetic fluctuations of cyclosporine add on to the challenge in cyclosporine delivery. This wonder molecule can be explored clinically to treat a broad spectrum of disorders, and hence, overcoming these physicochemical and pharmacokinetic discrepancies is a primary concern in designing effective delivery systems of cyclosporine.
Oral drug delivery systems for cyclosporine
Oral route of drug delivery is one of the conventional yet well-accepted routes of drug delivery due to its non-invasive nature and ease in administration [51]. The innovator company, Sandoz, also formulated cyclosporine as oral capsules and oral solutions which were yet to be site specific and safer formulations. Therefore, the need to explore oral delivery system is evident considering its crucial immunosuppressant activity in organ transplantation. An overview the oral drug delivery systems available for cyclosporine is seen in Fig. 3.
Cyclosporine tablets
Cyclosporine tablets were formulated with an aim to improve stability, retention time at absorption site, improve dissolution, and taste masking. Most of the approaches were focused on self-emulsifying systems which can form a fine emulsion in GIT with mild agitation provided by gastric motility [52]. Based on the droplet size of emulsion formed, they are classified as self-nanoemulsifying systems and self-microemulsifying systems.
Self nanoemulsifying drug delivery system (SNEDDS) is the mixture of oil, surfactant, and co-surfactant that can spontaneously form oil in water nanoemulsion in GIT after oral administration [53]. Li et al. and Zhang et al. formulated controlled release osmotic pump tablets of cyclosporine via SNEDDS [54]. Labrafil M 1944 CS, Cremophor EL, and Transcutol P were used as oil, surfactant, and co-surfactant respectively for liquid SNEDDS. Various additives like sucrose, lactose monohydrate, partly gelatinized starch, povidone, and talc were used to compressed tablets by wet granulation method. Further, tablets were coated with cellulose acetate with pore forming agent, polyethylene glycol (PEG) 4000. It was observed that release rate was dependent on inner osmotic pressure, ratio of osmotic agent to suspending agent, amount of pore forming agent, and diameter of release orifice. The osmotic formulation revealed linear drug release over the period of 12 h, displaying zero-order kinetics. The in vivo pharmacokinetic study in beagle dogs showed that tmax was prolonged to 4.3 ± 0.5 h, and maximum serum concentration (cmax) was significantly reduced to 72.9 ± 10.9 ng/Lit when compared to Neoral® which had tmax of 1 h and cmax of 157.9 ± 44.5 ng/Lit. Also, Neoral® had biological half-life (t1/2) of 6.6 ± 1.6 h, whereas t1/2 of suggested formulation was 8.3 ± 3.4 h. Thus, this approach could be beneficial in the reduction of dosing frequency and overcoming the fluctuations in the pharmacokinetic profile of the conventional cyclosporine formulations.
In other study, Zhao et al. formulated self-microemulsifying tablets of cyclosporine by liquisolid compact technique in order to improve dissolution profile [55]. Here, the mixture of lauroglycol FCC:Maisine 35–1 (1:1 w/w) was used as oil phase; PEG 35 castor oil and PEG 400 were selected as surfactant and co-surfactant respectively. The liquid system is converted to powder form by blending with microcrystalline cellulose, and further, the mixture was compressed into tablet. In vitro multimedia dissolution studies, the self microemulsifying tablets showed 80%, 70%, and 98% drug release in deionized water, pH 1.2 simulated gastric fluid and pH 6.8 ± 0.1 simulated intestine fluid correspondingly at the end of 90 min, whereas the conventional tablets revealed very less drug release (20%, 15% and 18% in respective media) comparatively. Hence, self microemulsifying approach can be useful in improving rate and extend of cyclosporine dissolution.
To overcome the bitter taste of cyclosporine, Zidan et al. formulated taste masked orodispersible tablets by direct compression technique along with self-emulsifying approach [56]. Also, orodispersible tablet offers an excellent patient compliance, especially among the pediatric group. Capmul MCM-C8, Emulphor, sweet orange oil mixed together to form homogenous transparent crude self-emulsifying drug delivery system. Orodispersible tablets were prepared by cyclosporine loaded self-emulsifying drug delivery system mixed with water for 24 h in horizontal shaking bath, and the slurry was lyophilized and frozen at − 70 °C for 2 h. The taste masking efficiency was done in vitro using electronic tongue (e-tongue) with seven potentiometric sensors using Ag/AgCl as reference electrode. The optimized cyclosporine-loaded self-emulsifying drug delivery system and its oro-dispersible formulation were prepared as nanoemulsion either by disintegrating or by dispersing in 5 mL artificial saliva equivalent to 25 mg of cyclosporine. Taste masking efficiency was determined by Euclidean distance values and discrimination indices, and it was observed that the unpalatable taste of cyclosporine was concealed by formulating it into SEDDS orodispersible form.
Floating microspheres
Microspheres are spherical, solid matrix particles having particle size in micron range. Floating microsphere is a type of gastroretentive delivery system which floats on the gastric fluid to achieve desired drug release. Prolonged gastric retention helps to attain desired drug plasma concentration without much fluctuations [57]. Cyclosporine floating microspheres were prepared to extend the drug absorption in gastrointestinal tract, which consequently leads to increase in bioavailability.
Lee et al. formulated cyclosporine floating microsphere using Eudragit S100, polyvinyl alcohol, and tacrine by solvent diffusion method [58]. Eudragit S100 and drug were dissolved in ethanol, with addition of isopropanol and dichloromethane. The solution was then slowly introduced into 0.4% polyvinyl alcohol under stirring. The formed microspheres were collected via filtration and dried at 50 °C for 12 h. The particle size of the microsphere was observed 75 to 1000 μm. The microsphere process parameters were optimized; it was observed that the most stable emulsion of Eudragit S100 was in polyvinyl alcohol solution when dissolved in ethanol:dichloromethane (1:1) at 40 °C. In order to improve microspheres preparation, ethanol system was replaced by isopropanol for controlling diffusion rate. Isopropanol diffusion rate was slower than the ethanol; thus, it provides more time for droplet formation. When various ratios of ethanol and dichloromethane with isopropanol were prepared, yield was 74 to 96% with irregular shape particles. When dichloromethane and isopropanol were used without ethanol, diffusion rate became slower as more time was taken to harden. The use of all three organic phases results in improved diffusion. The fraction of microspheres floating on the medium in in vitro study was linearly reduced up to 24 h. Therefore, it could be interpreted that in vivo drug absorption would be linear for an extended duration.
Mucoadhesive microspheres
In order to improve retention time of the formulation, mucoadhesive microspheres were prepared that imparts advantages like improved absorption and bioavailability. Owing to its high surface to volume ratio and intimate contact with absorption site, prolonged release of the drug and site specific targeting can be achieved to reduce the dosing frequency subsequently [59].
Malaekeh-nikouei et al. formulated chitosan-coated microsphere encapsulated with cyclosporine by solvent evaporation–emulsification method [60]. Cyclosporine and poly(lactic-co-glycolic acid) (PLGA) were dissolved in dichloromethane, emulsified by polyvinyl alcohol 0.3% w/w using homogenizer. For chitosan microsphere coating, microsphere was immersed in chitosan (0.5% w/w) followed by centrifuged at 15,000 RPM for 15 min and further freeze dried under vacuum. The electrostatic charge on PLGA (positive) and chitosan (negative) causes the formation of coat on the microsphere. Further, the poly-cationic nature of chitosan provides electrostatic interaction with negatively charged mucus due to ionization of sialic acid. Chitosan flexible structure showed physical enlargement between molecular chain and mucus component leading to the prolonged residence time. Chitosan also improves drug absorption and provides protection against enzyme degradation in GIT. The in vitro mucin adsorption test indicated that adsorption of mucin on entire surface of chitosan microspheres was identical, and almost 70% adsorption was observed. The mucoadhesive properties of these delivery systems accompanied with its potential for surface modification would increase the prospects for efficient oral drug delivery of cyclosporine.
Being a most convenient route, oral drug delivery systems of cyclosporine with aforementioned approaches have been studied by researchers. These novel formulations help to improve dissolution rate, prolong the retention time at absorption site to increase absorption rate, and aid in taste masking which in turn helps to overcome the key constraints of cyclosporine oral delivery. Yet, oral delivery of this cyclic peptide faces the major challenge of degradation against gastric enzymes which has to be overcome to increase its use as an oral immunosuppressant.
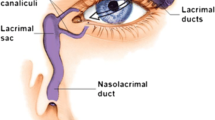
Ocular drug delivery systems for cyclosporine
Cyclosporine is preferred choice in treating inflammatory ocular conditions like chronic dry eye syndrome, uveitis, corneal healing, and vernal keratoconjunctivitis [61]. Considering broad spectrum of cyclosporine for ophthalmic diseases, it is crucial to develop effective, site-specific ocular delivery for local action. Poor solubility, large molecular weight, hydrophobic nature of cyclosporine, and protective mechanism of eyes make the development of its ocular delivery more challenging. Restasis® is US Food and Drug Administration approved ocular cyclosporine formulation, and Ikervis® has been recently approved for use in Europe. Still there is unmet need of more efficacious ocular formulations for cyclosporine [62, 63]. An outline of ocular drug delivery systems studied for cyclosporine is represented by Fig. 4.
Prodrug approach
Prodrugs are compounds which metabolized to get converted into pharmacologically active form [64]. The prodrug approach is used for cyclosporine in order to overcome its poor solubility and to enhance penetration. Rodriguez et al. formulated aqueous formulation of cyclosporine for ocular application by using N-methyl-glucamine salt as a prodrug having molecular weight of 1570 g/mol [65]. The ex vivo permeation and accumulation studies done using pig eyes showed that 80% of prodrug formulation could permeate through the cornea. In comparative permeation study, it was found that the amount of cyclosporine permeated through the cornea by prodrug approach was 20 to 140 times greater than cyclosporine in oil. The in vivo distribution studies in albinos Lewis rats indicated that the cyclosporine in prodrug form showed 70 times higher concentration in cornea when compared to cyclosporine in oil whereas in conjunctiva level of cyclosporine, prodrug was 5 times higher than the later [66]. It was concluded from the study that prodrug approach has several advantages such as higher permeation and accumulation capacities, higher tissue deposition, access of more drug through conjunctival route, and low risk of systemic complications.
Solid lipid nanoparticles
Solid lipid nanoparticles (SLNs) are dispersions of biodegradable solid lipids in water which allow incorporation of hydrophilic and hydrophobic drugs [67]. SLNs help in improving the solubility, penetration, and prolonged effect of cyclosporine when delivered via ocular route. Gökçe et al. formulated cyclosporine loaded SLNs for improving in vivo efficiency and evaluating ocular tolerance in rabbits [68]. SLNs were prepared by high shear homogenization followed by ultra-sonication method using glyceryl behenate, Pluronic F68, Tween 80 as lipid, surfactant, and co-surfactant. The rabbit cornea model was used for trans-corneal penetration due to its similarity with human eye. In in vivo study, the retention time of cyclosporine was prolonged to 8 h in the cal-de-sac and pre-corneal area due to the small size of SLNs. At physiological pH, anionic corneal epithelium allows the positively charged solute to cross the membrane selectively; however, negatively charged SLN particles provide therapeutic levels, possibly due to corneal cellular uptake. A conclusion could be drawn that the suggested approach could be promising in improving the corneal efficiency of cyclosporine.
Basaran et al. formulated cyclosporine loaded cationic SLNs for ocular delivery by hot homogenization method using tripalmitin, glyceryl dibehenate, and Tween 80 as lipid and surfactant to increase the corneal contact time of cyclosporine with help of octadecylamine [69]. The SLN formulation offers two advantages; first, it facilitates the transfer of drug through corneal route and second it ensures the adherence to the membrane, inhibiting draining with tears. In in vivo release profile studied in sheep model, the drug concentration in aqueous and vitreous humor was maintained up to 48 h. For chitosan and collagen nanoparticles, Lallemand et al. reported release of cyclosporine which was decreased after 2 h and 8 h respectively [70]. These SLN-based formulations were found to be superior in prolonging release of cyclosporine.
Injections
Since cyclosporine is used to treat chronic ocular inflammatory disorders, there is a need to develop drug delivery systems which prolongs the action of cyclosporine. Intra-vitreal injection prepared by using liposomes and microspheres was studied for developing its effective ocular delivery. Though this approach is invasive, it offers advantages like reduction in dosing frequency, prolonged retention time in cornea, bypassing protective mechanisms of eye, and avoiding loss of formulation with tears [71].
Alghadyan et al. formulated liposome bound cyclosporine for intra-vitreal injection by reverse phase evaporation process using phosphatidylcholine, phosphatidylglycerol, and cholesterol [72]. The systemic administration gives low therapeutic level of ocular cyclosporine concentration while topical application gives high corneal concentration and low vitreous concentration. The in vivo study performed in albino rabbits demonstrated gradual decrease in the concentration of cyclosporine in eye receiving liposomal dose. There is significant change in the t1/2 of free cyclosporine (6 h) to that of liposome-bound cyclosporine (3 days) which was indicative of prolong availability of the drug in liposome-bound form.
He et al. formulated the cyclosporine microsphere as treatment vehicle for uveitis in rabbits using PLGA, polyvinyl alcohol, and PEG 1000 by solvent evaporation followed by freeze drying [73]. The intra-vitreal injection modified with PF68 showed significant reduction in cellular infiltrate, inflammatory sign, protein level, and aqueous leukocyte count. The surfactant, PF68, increases the solubility of cyclosporine by solubilization effect, wetting the particle and lowering surface tension. The microsphere showed gradual release with increase in antiinflammatory action. From the in vivo study in albino rabbits, it was estimated that amount of cyclosporine entrapped would be sufficient to prolong its effect for 6 months.
In situ gels
Thermoresponsive ophthalmic in situ gels have been a promising drug delivery approach for ocular delivery as they possess excellent biocompatibility, increased drug loading efficiency, and controlled drug release characteristics [74]. In case of cyclosporine, they are used to increase corneal retention time and to obtain a prolonged release. Yijun Wu et al. designed a thermosensitive copolymer, hyaluronic acid-g-poly(N-isopropylacrylamide) (HAg-PNIPAAm), by coupling carboxylic end-capped PNIPAAm to aminated hyaluronic acid through amide bond linkages which were potential carrier [75]. The suggested formulation had drug loading efficiency of 73.92%. The in vitro release profile studies indicated that during initial period of 12 h the release was faster followed by a sustained release till 50 h. This approach also helped to achieve concentration of cyclosporine in cornea up to 1455.8 ng/g of tissue; this was higher as compared to other conventional approaches.
Contact Lens
The use of contact lens loaded with cyclosporine can help to overcome poor corneal retention and low bioavailability. Kapoor et al. suggested use of contact lens for cyclosporine made using nanostructured poly (2-hydroxyethyl methacrylate) (p-HEMA) hydrogels containing microemulsions or micelles of Brij-52 [76]. The bioavailability of cyclosporine when formulated as eye drops was less than 5%. The suggested approach was able to enhance bioavailability by 50%. Also, from the in vitro studies, it was estimated that cyclosporine could be delivered up to 20 days maintaining therapeutic doses. This approach thus helped in reducing dosing frequency by prolonging the effect of cyclosporine.
Implant
The frequent administration of injection is not easy, and hence, implants of biodegradable polymers are looked upon as substituents. They are effective for local treatment in ocular disorders to avoid systemic side effects. Cyclosporine implantable long-term sustained release formulation via use of biodegradable polymers could be beneficial [77]. This approach also overcomes the ocular constraints associated with protective mechanism of eye, poor retention time in cornea, poor penetration, and draining with tears. Apel et al. formulated subconjunctival biodegradable cyclosporine implant in corneal transplant therapy [78]. Cyclosporine was mixed with PLGA and dissolved in methylene chloride, and solvent was evaporated for 48 h. This film was then kept for degassing under vacuum for 3 days at 70 °C, 65 kPa pressure. The film of 5 mm in diameter was punched and sterilized with 2.5 MRad of Cobalt60 gamma radiation. The in vivo study in Dutch Belted rabbits showed that the release of cyclosporine from implant was complicated due to continuous degradation of polymer. As the polymer degrades, its molecular weight decreases which increases the permeability of cyclosporine.
Restasis® approval by US FDA has encouraged the investigation of ocular drug delivery systems for cyclosporine. Its main application in dry eye syndrome demands more effective ocular drug delivery system. The said ocular delivery systems have been useful to reduce enzyme degradation and may improve poor corneal transfer and retention time in cornea. Still, this can be improved further for making it more patient friendly and by decreasing dosing frequency.
Topical drug delivery systems for cyclosporine
Cyclosporine is gold standard for treatment of diseases like psoriasis, toxic epidermal necrolysis, atopic dermatitis, and inflammation associated with rheumatoid arthritis [79]. These diseases demand site specific topical therapy with local effect. Conventional treatment options could meet these requirements only to a limited extent. Being a topical drug delivery approach, one of the primary requisites of formulation to be effective is penetrating the stratum corneum. With the development of novel drug delivery systems like microemulsion, penetration enhancers, nanoparticles, iontophoresis technique, and ultrasound-mediated drug delivery approaches, it is possible to develop effective and safe topical formulation of cyclosporine, as represented in Fig. 5 [80].
Microemulsion
Microemulsions are mixture of oil surfactant and co-surfactant which are clear, thermodynamically stable, and isotropic in nature. They have considerable potential to incorporate wide range of drugs [81].
Liu et al. formulated microemulsion of cyclosporine using Aerosol OT, Tween 85, Iso propyl myristate, and water [82]. From the in vitro study, it was observed that, when the concentration of water increased in the microemulsion, permeation increases. It was anticipated that increase in the hydration level of stratum corneum facilitates the drug permeation. It was observed that permeation rate of cyclosporine was increased from 1.44 to 3.58 μg/mL with zero-order kinetics. The transdermal delivery of cyclosporine was increased up to 10 times using microemulsion approach as compare to topical drug suspension. Thus, microemulsion approach can improve transdermal permeation of cyclosporine significantly and aids in achieving site specific local effect.
Penetration enhancer
Penetration enhancers have been a mainstay in topical delivery since they help in enhancing penetration by decreasing barrier resistance [83]. The higher molecular weight of cyclosporine is responsible for its poor penetration through the skin. The use of penetration enhancer could be beneficial in overcoming this constraint of cyclosporine thereby developing efficient topical drug delivery. Lopes et al. formulated topical delivery of cyclosporine using monoolein as penetration enhancer [84]. It acts as penetration enhancer by increasing skin ceramides, fluidity of stratum corneum, and solubilization of lipophilic cyclosporine. Different concentrations of 0, 5, 10, 20, and 70% of monoolein were prepared by dissolving in propylene glycol followed by addition of cyclosporine. All concentrations of monoolein showed increased penetration up to 12 h post application, and when its 20 to 70% concentration was used, it increased the drug concentration in stratum corneum. It was observed that due to the lipophilic nature of monoolein and cyclosporine, they exhibited high affinity towards each other which facilitates the penetration of cyclosporine and drug retention in the skin.
Nanoparticles
Among the various types of nanoparticles, SLNs have been explored for topical delivery of cyclosporine. SLNs are drug carriers used in topical delivery to enhance permeation and obtain sustain release of drug. SLNs offer advantage of being biocompatible and biodegradable which helps in reducing the side effects [85]. Cyclosporine SLN formulation was developed to attain prolonged action of drug with improved penetration.
Varia et al. formulated and characterized cyclosporine loaded SLNs with optimization of variables [86]. The formulation was prepared by melt homogenization method using glyceryl palmitostearate, glyceryl monostearate, and soya phosphatidylcholine and was converted to dried form by spray drying. It was found that the two lipids glyceryl palmitostearate and glyceryl monostearate were considered to be the best carriers for cyclosporine due to high entrapment efficiency and narrow size distribution. Characterization studies showed smooth and non-porous surface of SLNs and in vitro release of cyclosporine from glyceryl monostearate followed Higuchi kinetics while glyceryl palmitostearate followed first-order kinetics. Cyclosporine–glyceryl monostearate SLNs showed initial burst release (14% in first hour) followed by slow and steady release pattern up to 20 h, whereas cyclosporine glyceryl palmitostearate SLNs did not show any burst release. This change in release could be attributed to difference in physicochemical properties of the lipids. The lipidic nature of SLNs accelerates penetration of cyclosporine and further helps in prolonging the release of drug which would aid in improving the therapeutic benefit.
Cyclosporine SLNs was formulated for skin penetration by melt homogenization method using 1,2,3-tridecanoylglycerol, l-a-phosphatidylcholine, t-butyl alcohol, and Tween 80 as lipids and surfactant. The study showed that the slightly negative charged nanoparticle was effective in skin penetration. The in vitro permeation experiments indicated that cyclosporine loaded SLNs had 2-fold higher permeation efficiency when compared to cyclosporine oil mixture [87].
Nanoparticles have at least one dimension less than 100 nm and have potential of improving penetration [88]. They also offer advantages of surface modification [89]. Zlotkin et al. formulated topically applied cyclosporine nanoparticle using butyl acetate, sodium cholate, and lecithin by solvent evaporation method to get particle size ranging from 30 to 650 nm [90]. In 30 nm, ex vivo penetration studies done using human skin indicated that penetration through skin was observed within 2 h while 24 h throughout the dermis. From the biological activity studies, there was no evidence of toxicity found.
Iontophoresis of lecithin vesicles
Iontophoresis is a technique of delivering drugs with the help of electric current [91]. Combining iontophoresis with lecithin vesicles which acts as a penetration enhancer helps to overcome poor penetration and low absorption rate of cyclosporine.
Boinpally et al. formulated lecithin vesicles of cyclosporine for skin permeation using soya phosphatidylcholine, sodium cholate, ethanol, and chloroform by rotary evaporator [92]. Lecithin and anodal iontophoresis enhanced the permeation of cyclosporine; cathodal iontophoresis presented lowest amount of penetration due to negatively charged cholate and chloride ions. Increased permeation of lecithin was done by electro-osmosis by passing electric current. The ex vivo absorption studies done using human skin showed that the suggested approach enhanced the absorption up to 4.9 times. The results of study were very encouraging for penetration enhancement and improving absorption rate of cyclosporine.
Guo et al. formulated lecithin vesicle carrier for transdermal delivery of cyclosporine using soya bean lipid, lecithin (prepared by column chromatography), and sodium cholate using conventional rotatory evaporation sonication method [93]. Lecithin and cyclosporine dissolved in methanol and chloroform mixture (1:1); the mixture was dried under vacuum to form thin film and then hydrated in 0.9% NaCl to form lipid coarse suspension followed by sonication. Sodium cholate was added to the NaCl suspension containing 3.75% of cyclosporine followed by vigorously shaken. The formulation was ultra-sonicated for 15 min and kept at 37 °C for 72 h until equilibrium was achieved. When iontophoresis is applied, increase in voltage applied increases the permeation but pre-treatment with enhancers changed the nature of skin. Lecithin vesicles with sodium cholate showed transfer of cyclosporine while sodium cholate micelles and vesicles without cholate failed to permeate into the skin. The synergistic effect of sodium cholate and lecithin enhances the penetration of vesicles into the skin. The cholate vesicles were capable of penetrating into the stratum corneum due to the transcutaneous hydration force caused by difference in concentration of water between the skin interior and skin surface. Loosening of interstices occurred due to hydration of skin helps in accumulation of cyclosporine; also, fusion of vesicles with skin enhances the penetration. In vivo study done in Kunming mice showed the measurable amount of flexible vesicle transported in the blood after 2 h while conventional vesicles failed for the same. When stratum corneum layer was destroyed, large amount of vesicles (187.329 53.21 ng/mL) was transferred in the blood within 1 h, showing that permeation barrier stratum corneum was bypassed. It can be concluded that combining iontophoresis with use of penetration enhancers increases penetration of cyclosporine.
Ultrasound-mediated drug delivery system
Low-frequency ultrasound governs the movement of drug molecules through the skin by using ultrasound, also termed as sonophoresis [94]. Combining this approach with use of penetration enhancers helps to improve penetration of cyclosporine, making the drug delivery more effective. Liu et al. formulated topical delivery of cyclosporine using azone, sodium lauryl sulfate (SLS), N-methyl pyrrolidine, and dimethyl sulfoxide (DMSO) as skin penetration enhancers by low-frequency ultrasound [95]. The in vitro study was carried on modified Franz diffusion apparatus. When ultrasound was applied alone, no significant exchange was observed at 0.4 W/cm2, whereas at 0.8 W/cm2, penetration was increased by 7-fold. It is believed that the ultrasound enhances the skin permeation by lowering the barrier properties of stratum corneum by creating the small pores on the skin surface and disorganizing the bilayer. When combining ultrasound and chemical enhancers, 25-fold increase in the dermal delivery was observed. Since the amount of penetration enhancers that can be used is limited for their safety concerns, this approach helps to overcome the drawback which makes penetration of cyclosporine more efficient.
Cyclosporine is mainstay treatment option for psoriasis and inflammation associated with rheumatoid arthritis, and thus, topical delivery systems would be more beneficial. Being a high molecular weight drug permeability of cyclosporine is very less. The above approaches can overcome poor topical penetration to a certain extent. In the future, the combination of approaches can be studied such as chemically modified drug formulated into topical nanoformulation. Nevertheless, none of the topical formulation of cyclosporine has been currently marketed which by itself demands more extensive study for development of effective formulation.
The constraints and recent advanced delivery systems suggested for cyclosporine are presented in Table 3.
Conclusion
The multifaceted therapeutic profile of cyclosporine commands the attention even after five decades of its discovery. The use of this well-established drug is still limited due to inherent constraints in drug delivery and its routes of administration. The advances in cyclosporine delivery have been reported by several research papers and patents. The low solubility and subsequent poor oral bioavailability of this drug are the bases of designing self-emulsifying systems, mucoadhesive, and floating systems to increase the GIT retention time and improve the rate and extent of absorption. The future aspects of oral drug delivery system may be focused on the use of synthetic modification of cyclosporine which not only addresses the poor solubility but also takes care of GIT enzyme degradation. Similarly, various nanoformulations can be used for improving GIT absorption or drug cocktails to overcome the cytochrome P-450 metabolism which ultimately help in improving absorption. In the ocular delivery of cyclosporine, the poor corneal transfer and less retention time in cornea act as a major barriers. These hurdles were overcome with the use of implants, liposome, and microsphere-based intra-vitreal injections and prodrug. Development of ophthalmic delivery systems can be further focused on chemically modified cyclosporine form to improve ocular penetration and permeation. The use of erodible inserts could be a promising approach to primarily reduce dosing frequency and increase patient compliance. The high molecular weight of cyclosporine reduces its penetration ability which is the major restraint in topical preparations. Hence, approaches like use of penetration enhancers, SLNs, iontophoresis, ultrasound, and microemulsions were recommended for topical delivery of cyclosporine. Novel topical formulations like microneedles, micro/nanosponges, nanogels, and electroporation may be explored to surpass stratum corneum, a major penetration barrier. Novel preparations of cyclosporine need formulation and process scalability to exploit them commercially. The regulatory aspects of formulations and patent exclusivity are other factors to be considered for successful market transfer. In conclusion, effective, non-toxic, stable, and patient friendly formulation is the need of hour for complete utilization of this wonder molecule, cyclosporine.
References
Kjer J, Debbab A, Aly AH, Proksch P. Methods for isolation of marine-derived endophytic fungi and their bioactive secondary products. Nat Protoc. 2010;5(3):479–90. https://doi.org/10.1038/nprot.2009.233.
Wu X, Stockdill JL, Wang P, Danishefsky SJ. Total synthesis of cyclosporine: access to N-methylated peptides via lsonitrile coupling reactions. J Am Chem Soc. 2010;132(12):4098–100. https://doi.org/10.1021/ja100517v.
Wenger RM. Synthesis of cyclosporine. Total syntheses of ‘cyclosporin A’ and ‘cyclosporin H’, two fungal metabolites isolated from the species Tolypocladium inflatum GAMS. Helv Chim Acta. 1984;67(2):502–25. https://doi.org/10.1002/hlca.19840670220.
Bockus AT, Lexa KW, Pye CR, Kalgutkar AS, Gardner JW, Hund KCR, et al. Probing the physicochemical boundaries of cell permeability and oral bioavailability in lipophilic macrocycles inspired by natural products. J Med Chem. 2015;58(11):4581–9. https://doi.org/10.1021/acs.jmedchem.5b00128.
Chatterjee J, Gilon C, Hoffman A, Kessler H. N-methylation of peptides: a new perspective in medicinal chemistry. Acc Chem Res. 2008;41(10):1331–42. https://doi.org/10.1021/ar8000603.
Wenger RM. Synthesis of cyclosporine and analogues: structural requirements for immunosuppressive activity. Angew Chem Int Ed Engl. 1985;24(2):77–85. https://doi.org/10.1002/anie.198500773.
Eid R. Therapeutic review. J Exot Pet Med. 2018;27(1):46–51. https://doi.org/10.1053/j.jepm.2017.10.016.
Hernández GL, Volpert OV, Íñiguez MA, Lorenzo E, Martínez-Martínez S, Grau R, et al. Selective inhibition of vascular endothelial growth factor–mediated angiogenesis by cyclosporin a. J Exp Med. 2001;193(5):607–20. https://doi.org/10.1084/jem.193.5.607.
Wells GA, Haguenauer D, Shea B, Suarez-Almazor ME, Welch V, Tugwell P, et al. Cyclosporine for treating rheumatoid arthritis. Cochrane Database Syst Rev. 1998;(2). https://doi.org/10.1002/14651858.CD001083.
Roekevisch E, Spuls PI, Kuester D, Limpens J, Schmitt J. Efficacy and safety of systemic treatments for moderate-to-severe atopic dermatitis: a systematic review. J Allergy Clin Immunol. 2014;133(2):429–38. https://doi.org/10.1016/j.jaci.2013.07.049.
Garrod R. Pulmonary rehabilitation in older people. CJ Geriatr Med. 2006;8(1):18–21. https://doi.org/10.3238/arztebl.2015.0071.
Czogalla A. Oral cyclosporine A - the current picture of its liposomal and other delivery systems. Cell Mol Biol Lett. 2009;14(1):139–52. https://doi.org/10.2478/s11658-008-0041-6.
Guada M, Lasa-Saracíbar B, Lana H, Del Carmen Dios-Viéitez M, Blanco-Prieto MJ. Lipid nanoparticles enhance the absorption of cyclosporine A through the gastrointestinal barrier: in vitro and in vivo studies. Int J Pharm. 2016;500(1–2):154–61. https://doi.org/10.1016/j.ijpharm.2016.01.037.
Borel JF, Feurer C, Magnée C, Stähelin H. Effects of the new anti-lymphocytic peptide cyclosporin A in animals. Immunology. 1977;32(6):1017–25.
Gauchat J, Khandjian EW, Weil R. Cyclosporin A prevents induction of the interleukin 2 receptor gene in cultured murine thymocytes. Proc Natl Acad Sci U S A. 1986;83(September):6430–4.
Colombani PM, Robb A, Hess AD. Cyclosporin a binding to calmodulin: a possible site of action on T lymphocytes. Science. 1985;228(4697):337–9. https://doi.org/10.1126/science.3885394.
Matsuda S, Koyasu S. Mechanisms of action of cyclosporine. Immunopharmacology. 2000;47(2–3):119–25. https://doi.org/10.1016/S0162-3109(00)00192-2.
Krönke M, Leonard WJ, Depper JM, Arya SK, Wong-Staal F, Gallo RC, et al. Cyclosporin A inhibits T-cell growth factor gene expression at the level of mRNA transcription. Proc Natl Acad Sci U S A. 1984;81(16):5214–8. https://doi.org/10.1073/pnas.81.16.5214.
Schmid FX. Protein folding: prolyl isomerases join the fold. Curr Biol. 1995;5(9):993–4. https://doi.org/10.1016/S0960-9822(95)00197-7.
Sigal NH. Is cyclophilin involved in the immunosuppressive and nephrotoxic mechanism of action of cyclosporin A? J Exp Med. 1991;173(3):619–28. https://doi.org/10.1084/jem.173.3.619.
Kiefer F, Tibbles LA, Anafi M, Janssen A, Zanke BW, Lassam N, et al. HPK1, a hematopoietic protein kinase activating the SAPK/JNK pathway. EMBO J. 1996;15(24):7013–25.
Klahr S, Ishidoya S, Morrissey J. Role of angiotensin II in the tubulointerstitial fibrosis of obstructive nephropathy. Am J Kidney Dis. 1995;26(1):141–6.
Matsuda S, Moriguchi T, Koyasu S, Nishida E. T lymphocyte activation signals for interleukin-2 production involve activation of MKK6-p38 and MKK7-SAPK/JNK signaling pathways sensitive to cyclosporin A. J Biol Chem. 1998;273(20):12378–82. https://doi.org/10.1074/jbc.273.20.12378.
Granelli-Piperno A. In situ hybridization for interleukin 2 and interleukin 2 receptor mRNA in T cells activated in the presence or absence of cyclosporin A. J Exp Med. 1988;168(5):1649–58. https://doi.org/10.1084/jem.168.5.1649.
Robinson MJ, Cobb MH. Mitogen-activated protein kinase pathways. Curr Opin Cell Biol. 1997;9(2):180–6. https://doi.org/10.1016/S0955-0674(97)80061-0.
Miskin JE, Charles CA, Lynnette CG, Dixon LA. Viral mechanism for inhibition of the cellular phosphatase calcineurin. Science. 1998;281(July):562–5.
Molkentin JD, Lu JR, Antos CL, Markham B, Richardson J, Robbins J, et al. A calcineurin-dependent transcriptional pathway for cardiac hypertrophy. Cell. 1998;93(2):215–28. https://doi.org/10.1016/S0092-8674(00)81573-1.
Timmerman LA, Clipstone NA, Ho SN, Northrop JP, Crabtree GR. Rapid shuttling of NF-AT in discrimination of Ca2+signals and immunosuppression. Nature. 1996;383:837–40. https://doi.org/10.1038/383837a0.
Su B, Jacinto E, Hibi M, Kallunki T, Karin M, Ben-Neriah Y. JNK is involved in signal integration during costimulation of T lymphocytes. Cell. 1994;77(5):727–36. https://doi.org/10.1016/0092-8674(94)90056-6.
Su B, Karint M. Mitogen-activated protein kinase cascades and regulation of gene expression. Curr Opin Immunol. 1996;8(3):402–11. https://doi.org/10.1016/S0952-7915(96)80131-2.
Yang SG. Biowaiver extension potential and IVIVC for BCS class II drugs by formulation design: case study for cyclosporine self-microemulsifying formulation. Arch Pharm Res. 2010;33(11):1835–42. https://doi.org/10.1007/s12272-010-1116-2.
Charman WN, Porter CJH, Mithani S, Dressman JB. Physicochemical and physiological mechanisms for the effects of food on drug absorption: the role of lipids and pH. J Pharm Sci. 1997;86(3):269–82. https://doi.org/10.1021/js960085v.
Fahr A. Cyclosporin clinical pharmacokinetics. Clin Pharmacokinet. 1993;24(6):472–95. https://doi.org/10.2165/00003088-199324060-00004.
Higgins C, Barnard A, Nixon R. Nanotechnology and contact dermatitis: applications and implications. Contact Dermatitis. 2016;75(3):77–8.
Müller RH, Runge S, Ravelli V, Mehnert W, Thünemann AF, Souto EB. Oral bioavailability of cyclosporine: solid lipid nanoparticles (SLN®) versus drug nanocrystals. Int J Pharm. 2006;317(1):82–9. https://doi.org/10.1016/j.ijpharm.2006.02.045.
Powles AV, Hardman CM, Porter WM, Cook T, Hulme B, Fry L. Renal function after 10 years treatment with cyclosporin for psoriasis. Br J Dermatol. 1998;138(3):443–9. https://doi.org/10.1046/j.1365-2133.1998.02122.x.
Thaçi D, Bräutigam M, Kaufmann R, Weidinger G, Paul C, Christophers E. Body-weight-independent dosing of cyclosporine micro-emulsion and three times weekly maintenance regimen in severe psoriasis. A randomised study. Dermatology. 2002;205(4):383–8. https://doi.org/10.1159/000066425.
Czech W, Bräutigam M, Weidinger G, Schöpf E. A body-weight-independent dosing regimen of cyclosporine microemulsion is effective in severe atopic dermatitis and improves the quality of life. J Am Acad Dermatol. 2000;42(4):653–9. https://doi.org/10.1016/S0190-9622(00)90180-4.
Oates JA, Wood AJJ, Kahan BD. Cyclosporine. N Engl J Med. 1989;321(25):1725–38. https://doi.org/10.1056/NEJM198912213212507.
Copeland KR, Yatscoff RW, McKenna R. Immunosuppressive activity of cyclosporine metabolites compared and characterized by mass spectroscopy and nuclear magnetic resonance. Clin Chem. 1990;36(2):225–9.
Pickrell MD, Sawers R, Michael J. Pregnancy after renal transplantation: severe intrauterine growth retardation during treatment with cyclosporin A. Br Med J (Clin Res Ed). 1988;296(6625):825–6. https://doi.org/10.1136/bmj.296.6625.825-a.
Rajfer J, Sikka SC, Lemmi C, Koyle MA. Cyclosporine inhibits testosterone biosynthesis in the rat testis. Endocrinology. 1987;121(2):586–9. https://doi.org/10.1210/endo-121-2-586.
Robson D. Review of the pharmacokinetics, interactions and adverse reactions of cyclosporine in people, dogs and cats. Vet Rec. 2003;152(24):739–48. https://doi.org/10.1136/vr.152.24.739.
Vercauteren SB, Bosmans JL, Elseviers MM, Verpooten GA, De Broe ME. A meta-analysis and morphological review of cyclosporine-induced nephrotoxicity in auto-immune diseases. Kidney Int. 1998;54(2):536–45. https://doi.org/10.1046/j.1523-1755.1998.00017.x.
Mohammadpour N, Elyasi S, Vahdati N, Mohammadpour AH, Shamsara J. A review on therapeutic drug monitoring of immunosuppressant drugs. Iran J Basic Med Sci. 2011;14(6):485–98. https://doi.org/10.1046/j.1365-2125.1999.00911.x.
Aguirre TAS, Teijeiro-Osorio D, Rosa M, Coulter IS, Alonso MJ, Brayden DJ. Current status of selected oral peptide technologies in advanced preclinical development and in clinical trials. Adv Drug Deliv Rev. 2016;106:223–41. https://doi.org/10.1016/j.addr.2016.02.004.
Reichrath J, Bens G, Bonowitz A, Tilgen W. Treatment recommendations for pyoderma gangrenosum: an evidence-based review of the literature based on more than 350 patients. J Am Acad Dermatol. 2005;53(2):273–83. https://doi.org/10.1016/j.jaad.2004.10.006.
Wilson SE, Perry HD. Long-term resolution of chronic dry eye symptoms and signs after topical cyclosporine treatment. Ophthalmology. 2007;114(1):76–9. https://doi.org/10.1016/j.ophtha.2006.05.077.
Hernández-García V. Contents of the digestive tract of a false killer whale (Pseudorca crassidens) stranded in Gran Canaria (Canary Islands, Central East Atlantic). Bull Mar Sci. 2002;71(1):367–9. https://doi.org/10.1002/bdd.
Tao XR, Xia XY, Zhang J, Tong LY, Zhang W, Zhou X, et al. CYP3A4∗18B and CYP3A5∗3 polymorphisms contribute to pharmacokinetic variability of cyclosporine among healthy Chinese subjects. Eur J Pharm Sci. 2015;76:238–44. https://doi.org/10.1016/j.ejps.2015.05.011.
Muheem A, Shakeel F, Jahangir MA, Anwar M, Mallick N, Jain GK, et al. A review on the strategies for oral delivery of proteins and peptides and their clinical perspectives. Saudi Pharm J. 2016;24(4):413–28. https://doi.org/10.1016/j.jsps.2014.06.004.
Vasconcelos T, Marques S, Sarmento B. Measuring the emulsification dynamics and stability of self-emulsifying drug delivery systems. Eur J Pharm Biopharm. 2018;123:1–8. https://doi.org/10.1016/j.ejpb.2017.11.003.
Yu JY, Chong PHJ. A survey of clustering schemes for mobile ad hoc networks. IEEE Commun Surv Tutorials. 2005;7(1):32–47. https://doi.org/10.1080/17425247.2016.1218462.
Zhang X, Yi Y, Qi J, Lu Y, Tian Z, Xie Y, et al. Controlled release of cyclosporine A self-nanoemulsifying systems from osmotic pump tablets: near zero-order release and pharmacokinetics in dogs. Int J Pharm. 2013;452(1–2):233–40. https://doi.org/10.1016/j.ijpharm.2013.05.014.
Zhao X, Zhou YQ, Potharaju S, Lou H, Sun HM, Brunson E, et al. Development of a self micro-emulsifying tablet of cyclosporine A by the liquisolid compact technique. Int J Pharm Sci Res. 2011;2(9):2299–308.
Zidan AS, Aljaeid BM, Mokhtar M, Shehata TM. Taste-masked orodispersible tablets of cyclosporine self-nanoemulsion lyophilized with dry silica. Pharm Dev Technol. 2015;20(6):652–61. https://doi.org/10.3109/10837450.2014.908307.
Mukund JY, Kantilal BR, Sudhakar RN. Floating microspheres: a review. Braz J Pharm Sci. 2012;48(1):17–30. https://doi.org/10.1590/S1984-82502012000100003.
Lee J, Park TG, Choi H. Development of oral drug delivery system using floating microspheres. J Microencapsul. 1999;16:715–29. https://doi.org/10.1080/026520499288663.
Kaurav H, Hari Kumar SL, Kaur A. Mucoadhesive microspheres as carriers in drug delivery: a review. Int J Drug Dev Res. 2012;4(2):21–34. https://doi.org/10.1002/rnc.
Malaekeh-Nikouei B, Sajadi Tabassi SA, Jaafari MR. Preparation, characterization, and mucoadhesive properties of chitosan-coated microspheres encapsulated with cyclosporine A. Drug Dev Ind Pharm. 2008;34(5):492–8. https://doi.org/10.1080/03639040701744004.
Labbé A, Baudouin C, Ismail D, Amrane M, Garrigue JS, Leonardi A, et al. Utilisation de la cyclosporine A topique : une étude pan-européenne. J Fr Ophtalmol. 2017;40(3):187–95. https://doi.org/10.1016/j.jfo.2016.12.004.
Agarwal P, Rupenthal ID. Modern approaches to the ocular delivery of cyclosporine A. Drug Discov Today. 2016;21(6):977–88. https://doi.org/10.1016/j.drudis.2016.04.002.
Lallemand F, Schmitt M, Bourges JL, Gurny R, Benita S, Garrigue JS. Cyclosporine A delivery to the eye: a comprehensive review of academic and industrial efforts. Eur J Pharm Biopharm. 2017;117:14–28. https://doi.org/10.1016/j.ejpb.2017.03.006.
Dahan A, Zimmermann EM, Ben-Shabat S. Modern prodrug design for targeted oral drug delivery. Molecules. 2014;19(10):16489–505. https://doi.org/10.3390/molecules191016489.
Hamel AR, Hubler F, Mutter M. Water-soluble prodrugs of cyclosporine A with tailored conversion rates. J Pept Res. 2005;65(3):364–74. https://doi.org/10.1111/j.1399-3011.2005.00234.x.
Rodriguez-Aller M, Guillarme D, El Sanharawi M, Behar-Cohen F, Veuthey JL, Gurny R. In vivo distribution and ex vivo permeation of cyclosporine A prodrug aqueous formulations for ocular application. J Control Release. 2013;170(1):153–9. https://doi.org/10.1016/j.jconrel.2013.04.019.
Battaglia L, Gallarate M, Serpe L, Foglietta F, Muntoni E, del Pozo Rodriguez A, et al. Chapter 7. In: Ocular delivery of solid lipid nanoparticles: Elsevier Inc; 2018. https://doi.org/10.1016/B978-0-12-813687-4.00007-4.
Gökçe EH, Sandri G, Eǧrilmez S, Bonferoni MC, Güneri T, Caramella C. Cyclosporine a-loaded solid lipid nanoparticles: ocular tolerance and in vivo drug release in rabbit eyes. Curr Eye Res. 2009;34(11):996–1003. https://doi.org/10.3109/02713680903261405.
Lallemand F, Felt-Baeyens O, Besseghir K, Behar-Cohen F, Gurny R. Cyclosporine A delivery to the eye: a pharmaceutical challenge. Eur J Pharm Biopharm. 2003;56(3):307–18. https://doi.org/10.1016/S0939-6411(03)00138-3.
Başaran E, Demirel M, Sirmagül B, Yazan Y. Cyclosporine-A incorporated cationic solid lipid nanoparticles for ocular delivery. J Microencapsul. 2010;27(1):37–47. https://doi.org/10.3109/02652040902846883.
Mitragotri S, Burke PA, Langer R. Overcoming the challenges in administering biopharmaceuticals: formulation and delivery strategies. Nat Rev Drug Discov. 2014;13(9):655–72. https://doi.org/10.1038/nrd4363.
Alghadyan AA, Peyman GA, Khoobehi B, Milner S, Liu K. Liposome-bound cyclosporine : clearance after intravitreal injection. Int Ophthalmol. 1988;12(2):109–12. https://doi.org/10.1007/BF0013713.
He Y, Wang J-C, Liu Y-L, Ma Z-Z, Zhu X-A, Zhang Q. Therapeutic and toxicological evaluations of cyclosporine a microspheres as a treatment vehicle for uveitis in rabbits. J Ocul Pharmacol Ther. 2006;22(2):121–31. https://doi.org/10.1089/jop.2006.22.121.
Cao Y, Zhang C, Shen W, Cheng Z, Yu L, Ping Q. Poly(N-isopropylacrylamide)-chitosan as thermosensitive in situ gel-forming system for ocular drug delivery. J Control Release. 2007;120(3):186–94. https://doi.org/10.1016/j.jconrel.2007.05.009.
Wu Y, Yao J, Zhou J, Dahmani FZ. Enhanced and sustained topical ocular delivery of cyclosporine a in thermosensitive hyaluronic acid-based in situ forming microgels. Int J Nanomedicine. 2013;8:3587–601. https://doi.org/10.2147/IJN.S47665.
Kapoor Y, Chauhan A. Ophthalmic delivery of Cyclosporine A from Brij-97 microemulsion and surfactant-laden p-HEMA hydrogels. Int J Pharm. 2008;361(1–2):222–9. https://doi.org/10.1016/j.ijpharm.2008.05.028.
Lee D. Intraocular implants for the treatment of autoimmune uveitis. J Funct Biomater. 2015;6(3):650–66. https://doi.org/10.3390/jfb6030650.
Apel A, Oh C, Chiu R, Saville B, Cheng YL, Rootman D. A subconjunctival degradable implant for cyclosporine delivery in corneal transplant therapy. Curr Eye Res. 1995;14(8):659–67. https://doi.org/10.3109/02713689508998493.
Musa SH, Basri M, Masoumi HRF, Shamsudin N, Salim N. Enhancement of physicochemical properties of nanocolloidal carrier loaded with cyclosporine for topical treatment of psoriasis: in vitro diffusion and in vivo hydrating action. Int J Nanomedicine. 2017;12:2427–41. https://doi.org/10.2147/IJN.S125302.
Katare O, Raza K, Singh B, Dogra S. Novel drug delivery systems in topical treatment of psoriasis: rigors and vigors. Indian J Dermatol Venereol Leprol. 2010;76(6):612. https://doi.org/10.4103/0378-6323.72451.
Lawrence MJ, Rees GD. Microemulsion-based media as novel drug delivery systems. Adv Drug Deliv Rev. 2012;64(SUPPL):175–93. https://doi.org/10.1016/j.addr.2012.09.018.
Liu H, Li S, Wang Y, Han F, Dong Y. Bicontinuous water-AOT/Tween85-isopropyl myristate microemulsion: a new vehicle for transdermal delivery of cyclosporin A. Drug Dev Ind Pharm. 2006;32(5):549–57. https://doi.org/10.1080/03639040500529168.
Marwah H, Garg T, Goyal AK, Rath G. Permeation enhancer strategies in transdermal drug delivery. Drug Deliv. 2016;23(2):564–78. https://doi.org/10.3109/10717544.2014.935532.
Lopes LB, Collett JH, Bentley MVLB. Topical delivery of cyclosporin A: an in vitro study using monoolein as a penetration enhancer. Eur J Pharm Biopharm. 2005;60(1):25–30. https://doi.org/10.1016/j.ejpb.2004.12.003.
Lauterbach A, Müller-Goymann CC. Applications and limitations of lipid nanoparticles in dermal and transdermal drug delivery via the follicular route. Eur J Pharm Biopharm. 2015;97(July):152–63. https://doi.org/10.1016/j.ejpb.2015.06.020.
Sawant K, Varia J, Dodiya S. Cyclosporine a loaded solid lipid nanoparticles: optimization of formulation, process variable and characterization. Curr Drug Deliv. 2008;5(1):64–9. https://doi.org/10.2174/156720108783331069.
Kim ST, Jang DJ, Kim JH, Park JY, Lim JS, Lee SY, et al. Topical administration of cyclosporin A in a solid lipid nanoparticle formulation. Pharmazie. 2009;64(8):510–4. https://doi.org/10.1691/ph.2009.8373.
Khan I, Saeed K, Khan I. Nanoparticles: properties, applications and toxicities. Arab J Chem. 2017. https://doi.org/10.1016/j.arabjc.2017.05.011.
Kotsuchibashi Y, Nakagawa Y, Ebara M. Nanoparticles. Biomater Nanoarchitectonics. 2016;5(June):7–23. https://doi.org/10.1016/B978-0-323-37127-8.00002-9.
Frušić-Zlotkin M, Soroka Y, Tivony R, Larush L, Verkhovsky L, Brégégère FM, et al. Penetration and biological effects of topically applied cyclosporin A nanoparticles in a human skin organ culture inflammatory model. Exp Dermatol. 2012;21(12):938–43. https://doi.org/10.1111/exd.12051.
Alkilani AZ, McCrudden MTC, Donnelly RF. Transdermal drug delivery: innovative pharmaceutical developments based on disruption of the barrier properties of the stratum corneum. Pharmaceutics. 2015;7(4):438–70. https://doi.org/10.3390/pharmaceutics7040438.
Boinpally RR, Zhou SL, Devraj G, Anne PK, Poondru S, Jasti BR. Iontophoresis of lecithin vesicles of cyclosporin A. Int J Pharm. 2004;274(1–2):185–90. https://doi.org/10.1016/j.ijpharm.2004.01.016.
Guo J, Ping Q, Sun G, Jiao C. Lecithin vesicular carriers for transdermal delivery of cyclosporin A. Int J Pharm. 2000;194(2):201–7. https://doi.org/10.1016/S0378-5173(99)00361-0.
Park D, Park H, Seo J, Lee S. Sonophoresis in transdermal drug deliverys. Ultrasonics. 2014;54(1):56–65. https://doi.org/10.1016/j.ultras.2013.07.007.
Liu H, Li S, Pan W, Wang Y, Han F, Yao H. Investigation into the potential of low-frequency ultrasound facilitated topical delivery of cyclosporin A. Int J Pharm. 2006;326(1–2):32–8. https://doi.org/10.1016/j.ijpharm.2006.07.022.
Koppelstaetter C, Kern G, Leierer G, Mair SM, Mayer G, Leierer J. Effect of cyclosporine, tacrolimus and sirolimus on cellular senescence in renal epithelial cells. Toxicol in Vitro. 2018;48(September 2017):86–92. https://doi.org/10.1016/j.tiv.2018.01.004.
Kvien TK, Scherer HU, Burmester GR. Rheumatoid Arthritis. EULAR Compend Rheum Dis. 2009;333(3):61–80. https://doi.org/10.1038/nrrheum.2009.31.
Stevenson D, Tauber J, Reis BL. Efficacy and safety of cyclosporin A ophthalmic emulsion in the treatment of moderate-to-servere dry eye disease: a dose-ranging, randomized trial. Ophthalmology. 2000;107(5):967–74. https://doi.org/10.1016/S0161-6420(00)00035-X.
Donnenfeld E, Pflugfelder SC. Topical ophthalmic cyclosporine: pharmacology and clinical uses. Surv Ophthalmol. 2009;54(3):321–38. https://doi.org/10.1016/j.survophthal.2009.02.002.
Biren TA, Barr RJ. Dermatologic applications of cyclosporine. Arch Dermatol. 1986;122(9):1028–32. https://doi.org/10.1001/archderm.1986.01660210078022.
Lebwohl M, Ellis C, Gottlieb A, Koo J, Krueger G, Linden K, et al. Cyclosporine consensus conference: with emphasis on the treatment of psoriasis. J Am Acad Dermatol. 1998;39(3):464–75. https://doi.org/10.1016/S0190-9622(98)70325-1.
Dorinda Shelley E, Shelley WB. Cyclosporine therapy for pyoderma gangrenosum associated with sclerosing cholangitis and ulcerative colitis. J Am Acad Dermatol. 1988;18:1084–8. https://doi.org/10.1016/S0190-9622(88)70111-5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Patel, D., Wairkar, S. Recent advances in cyclosporine drug delivery: challenges and opportunities. Drug Deliv. and Transl. Res. 9, 1067–1081 (2019). https://doi.org/10.1007/s13346-019-00650-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-019-00650-1