Abstract
The purpose of this work was to develop an effective carbomer hydrogel to be used to treat second-degree burns that combined ciprofloxacin and lidocaine (CbCipLid hydrogel). Its antibiotic and anesthetic efficacy and the physical and chemical properties of the CbCipLid hydrogel (release rate and kinetics, rheology, appearance, and drug content) were evaluated both before and after a sterilization cycle and also after 6 months of storage. For the in vivo studies, second-degree burns were developed in a rat model. Animals were divided into three groups: CbCipLid hydrogel, silver sulfadiazine cream (reference), and carbomer hydrogel (as control). The treatments were applied daily for 21 days, and the healing was monitored by macroscopic observation and histologic evaluation. The anesthetic effect was evaluated through the corneal touch threshold in a rabbit eye model. The CbCipLid hydrogel obtained is transparent and allows the loading of ciprofloxacin above its solubility at a neutral pH, with a rheology which is convenient for topical administration. Its physical and chemical properties remained unchanged after sterilization and for at least six additional months. Both ciprofloxacin and lidocaine are reversibly released from the CbCipLid hydrogel with a kinetics fitting the Higuchi model. The presence of a biologic-like fluid increased the rate of drug delivery through an ionic exchange mechanism. Treatment with the CbCipLid hydrogel decreased the wound-healing period, compared with the reference, and was associated with a greater number of fibroblasts and a faster rate of epithelialization and dermis reconstruction. These differences were assigned to the moist environment provided by the hydrogel and also to the presence of a therapeutic concentration of ciprofloxacin. Moreover, CbCipLid hydrogel provides an immediate anesthetic effect, which is significantly more intense than that of the reference. Based on these results, it is believed that the CbCipLid hydrogel could be a potential candidate in the prophylaxis/treatment of second-degree burns.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A burn is an injury to the skin or other organic tissue, which could be caused by heat or due to radiation, radioactivity, electricity, friction, or contact with chemicals. Burns are a serious global public health problem, with an estimated 180,000 deaths occurring each year. In addition, non-fatal burns are a leading cause of morbidity, including prolonged hospitalization, disfigurement, and disability, often with resulting stigma and rejection [1].
Depending on the depth, burn injuries are classified as first, second, or third degree. Although superficial second-degree burns can heal quickly with minimal scarring, deep second- and third-degree burns can take several weeks to heal and tend to form scars [2]. Moreover, superficial second-degree burns can progress to a deeper burn if the wound dries out or becomes infected [3]. In this context, the management of burn wounds can have a considerable influence on the time taken for the wound to heal, the long-term quality and appearance of the scar, and the risk for burn wound infection.
As second-degree burns are very painful [4], the current treatment focuses on infectious prophylaxis and analgesia or anesthesia. At present, a cream containing silver sulfadiazine (SSD) is the antimicrobial gold standard for treatment, due to its effectiveness against both Gram-positive and Gram-negative bacteria [5]. Most of the SSD-based creams also contain lidocaine (Lid) to relieve pain and vitamin V to promote re-epithelization [6]. Nevertheless, several drawbacks have been associated with the use of SSD-containing creams, such as poor scar penetration, discoloration (brown/gray/blue) of the skin and systemic complications, including neutropenia, erythema multiforme, crystalluria, and methemoglobinemia [7]. Also, before each re-application, the wound must be scrubbed thoroughly to remove residual cream and ensure it is well cleaned [5]. Furthermore, the need for a twice-daily application of SSD-containing creams and SSD cytotoxicity have been reported to delay wound healing [5, 8, 9]. Therefore, there is still a significant demand for topical formulations that can provide, sustained antimicrobial benefits, pain relief, and also promote wound healing.
Ciprofloxacin (Cip) is a leader among the third-generation fluoroquinolones with a broad spectrum of antibacterial activity and good penetration in most tissues [10]. It has an efficient topical antibiotic activity and a very low incidence of spontaneous resistance [11]. In aqueous solution, Cip exists mainly in its zwitterionic form owing to an acid/base interaction between the basic nitrogen of the piperazine and the carboxylic acid groups (Fig. 1) with the low aqueous solubility of Cip at physiological pH (0.17 mg/mL) being the main factor that prevents the design of liquid dosage forms [12]. In fact, the Cip isoelectric point is at pH 7.42, with its aqueous compatibility occurring at a rather basic or acid pH.
Lid is the most important local anesthetic and is widely used by topical route in creams and gels. From the chemical point of view, it is a tertiary aliphatic amine with a pKa = 8.01 and a solubility of 11.6 mg/g at pH = 7.59 [13]. Carbomer (Cb) is a synthetic polymethacrylate, which is available in several forms (71G NF, 971P NF, 980 NF, 5984 EP, 934P NF, 940 NF, and 1342 NF) and extensively used by topical route since it forms viscous hydrogels and also has bioadhesive properties. Consequently, it has found a wide variety of applications in gels, lotions, creams, bioadhesive formulations, toothpaste, suspensions, and tablets [14].
Previous studies have shown that Cb loading with Cip and an appropriate proportion of Na+ yields physically stable dispersions in which the aqueous compatibility of Cip is significantly enhanced due to ion pairing between Cip and Cb [15]. Similarly, the amine groups of Lid can also form ionic complexes with Cb and an appropriate proportion of Na+. In both cases, the dispersions behave as a smart molecular matrix of the drugs, since they can provide sustained release when in contact with biological fluid-like solutions.
The combination of Cip and Lid in therapeutic doses in a ternary hydrogel with Cb would be expected to act as an antimicrobial and anesthetic, thus preventing secondary infections and also providing pain relief. However, to the best of our knowledge, this is the first report of using a Cip/Lid composite for burn treatment. The aim of this work was to develop this hydrogel and to investigate its antibiotic and anesthetic effectiveness in second-degree burns.
Materials and methods
All chemical reagents and solvents used were of pharmaceutical or analytical quality with ultrapure water being obtained by the Milli Q® purification system.
Glacial acetic acid at 99.5% was purchased from Cicarelli®, Argentina; acetonitrile was from Sintorgan®, Argentina; ciprofloxacin hydrochloride, lidocaine (Lid), lidocaine hydrochloride, and Carbomer 934P NF (Cb) were from Parafarm®, Argentina); sodium hydroxide 1 M solution (NaOH) was from Anedra®, Argentina; and 5% dextrose and 0.9% sodium chloride solutions were from Braun®, Argentina.
Cip as a base was obtained from ciprofloxacin hydrochloride according to Bermudez et al. [16]. Briefly, ciprofloxacin hydrochloride was neutralized with an equimolar amount of 1 M NaOH. The solid precipitated was washed with cold water, filtered, and dried at 60 °C to constant weight. The resulting solid was free of chlorides, as determined by the limit test described by the Argentinian Pharmacopeia [17], presented a FTIR profile according to that described by International Pharmacopeia, and melted at 263–264 °C (with decomposition).
The equivalents of carboxylic groups per gram of Cb (12 × 10−3 eq/g) were assayed by acid-base titration. Platsul A® cream from Souberian Chobet Laboratory (Argentina) was used, which contained silver sulfadiazine (SSD) (1%), Lid (0.66%), and vitamin A (248,000 UI).
Preparation of the antibiotic-anesthetic hydrogel (CbCipLid hydrogel)
For the development of the CbCipLid hydrogel, a dose of Cip approved for topical (ophthalmic) administration (0.3%) [18] and a dose of Lid contained in the SSD cream (0.67%) [6] were used. Briefly, a 0.5% (w/w) dispersion of Cb in water was prepared and NaOH was added, under stirring at an amount sufficient to salify 10% of Cb carboxylic acid groups. The dispersion was covered with Parafilm® and left overnight in the refrigerator to improve the hydration of the Cb chains. Afterwards, the dispersion was heated to 90 °C and Cip, previously suspended in water, was added at a sufficient amount to neutralize 15% of Cb carboxylic acid groups. Stirring and heating were maintained until the Cip particles disappeared. Then, Lid was added as a powder in sufficient quantity to neutralize 47% of the acidic groups of Cb with stirring and heating then performed until a transparent system was obtained. The weight of the hydrogel was corrected by the addition of water and the system was left for 24 h at room temperature to ensure the interaction of the drugs with Cb. The same hydrogel but without the drugs was also prepared and used as a control (CbNa hydrogel), with its pH being regulated to 7.0 by the addition of NaOH solution in order to acquire a pH similar to CbCipLid hydrogel.
Stability of CbCipLid hydrogel
Ten grams of CbCipLid hydrogel were fractionated in 25 mL inactinic bottles, covered with a swab of cotton and gauze and sterilized in an autoclave at 120 °C and 1 atm for 15 min. Subsequently, these were closed with a screw cap in an aseptic environment and stored for 6 months at 25 °C and 40% RH.
The physical and chemical properties were evaluated in triplicate both before and after the sterilization cycle and also after 6 months of storage. The pH was determined with a semisolid pH-meter Mettler Toledo® equipped with an electrode InLab® Viscous (Mettler Toledo, USA). The color and appearance were evaluated macroscopically to search for any lumps, crystals, or foreign substances. The weight change was determined with an analytical balance, and it was considered that no variation had occurred when the difference in weight was ≤ 0.05%. The contents of Cip and Lid in the systems were determined as follows: 500 μL of the hydrogel were added to a 10-mL flask and brought to final volume with ultrapure water. This solution was heated and sonicated until a homogeneous dispersion was obtained, after which, 500 μL aliquots were made to a final volume of 10 mL with an acetic acid solution prepared with water and glacial acetic acid (930:50), adjusted at pH 3.4 with 1 M NaOH. The samples were filtered using 0.45 μm Millipore® filters and immediately subjected to high-performance liquid chromatography-ultraviolet (HPLC-UV) for quantification.
In vitro release kinetics
The in vitro release kinetics study was carried out using Franz type diffusion cells. These cells are bicompartmental chambers, where the receiver compartment, which has a capacity of 15–17 mL, was filled with 0.9% degassed NaCl solution or distilled water. The donor compartment consisted of a cylinder provided at one end with a synthetic cellulose acetate membrane (Sigma®, 12,000 D) with an effective diffusion area of 1.25 cm2. On this membrane, after being overnight hydrated, an accurately weighed amount of the hydrogel was placed (approximately 340 mg to assure the sink conditions of the drugs). At the beginning of the test, 0.9 mL aliquots were taken at preset intervals (5, 10, 15, 30, and 45 min and 1, 1.5, 2, 3, 4, 5, 6, and 24 h) and the sampled volume was replaced with an equal volume of fresh medium, thermostated at 37 °C.
Sampling was performed at the midpoint of the recipient compartment with the aid of a 1-cm3 syringe and needle, and samples were immediately frozen until further analysis by HPLC-UV. All these experiments were performed six times. Next, the kinetics drug release was studied by fitting the release data using two common mathematical models: zero-order and Higuchi [19]. The slope of the straight line represents the rate constant, with, the determination coefficient (r2) being used as an indicator of the level of fit of the data of each model.
Quantification of Cip and Lid by HPLC-UV
Instruments and analytical conditions
The technique described in USP 40-NF35 [20] for the quantification of Lid was modified and validated for its simultaneous quantification with Cip. A Waters Breeze System (Waters Corp., USA) HPLC system was used, with a 1525 binary pump, Waters 717 plus autosampler, Column thermostatic furnace (Waters 1500 series column heater), and a PDA 2996 detector. All data were acquired using Empower® Pro software. The separation of the analytes was achieved with a Luna® C18 reverse phase column (5 μm particle size, 150 × 4.6 mm) and a C18 guard column (4 × 3 mm ID), (Phenomenex, USA). The mobile phase consisted of acetic acid solution:acetonitrile (4:1), which was filtered and degassed, and the injection volume was 50 μL. Chromatographic runs were performed at 1 mL/min and detected by UV at λ = 254 and 277 nm for Lid and Cip, respectively.
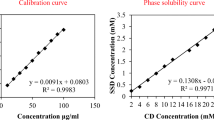
Calibration curves
Stock solutions of Cip and Lid were each prepared at a concentration of 15.0 mg/mL of Cip and 53.0 mg/mL for Lid in the acetic acid solution. Working solutions of Cip and Lid were prepared by diluting their stock solutions to concentrations of 1.5–150.0 μg/mL (Cip) and 5.3–530 μg/mL (Lid) with acetic acid solution. Both stock and working solutions were used immediately. In addition, solutions of Lid (26.5 μg/mL) spiked with Cip concentrations of 1.5–150.0 μg/mL and solutions of Cip (15.0 μg/mL) spiked with Lid (5.3–530.0 μg/mL) were prepared to verify that this technique permitted the simultaneous quantification, without interferences. For the separation of Cip and Lid, the resolution (R) was determined by Eq. (1)
where t2 and t1 are the retention times of the two analytes, and W2 and W1 are the widths of the base of the corresponding peaks, obtained by extrapolating the sides with the baseline [17].
Method validation
Validation was carried out following the criteria for Guide Q2 (R1) [21]. The selectivity, linearity, intra- and interday accuracy and precision, and the limit of quantification were determined. In addition, a 1-cycle freeze-thaw testing was conducted by freezing the working solutions (− 18 °C) for 24 h. Then, the samples were thawed at room temperature for another 24 h and analyzed by HPLC-UV to check for any significant changes.
Rheological evaluation of CbCipLid hydrogel
The flow curves of the CbCipLid hydrogel were determined at 25 °C (room temperature), 35 °C (skin temperature), and 37 °C (mucous membrane temperature). The flow curves obtained for CbNa hydrogel were also determined for comparison. A Haake® rotational viscometer was used and data were analyzed by VT 500® v 1.31 software. The sensor utilized was a cylinder-cup MV2, and the following values were assigned to each interval: interval 1, 0–9 s−1 for 3 min; interval 2, 9 s−1 during 3 min; and interval 3, 9–0 s−1 for 3 min. The shear stress (τ, Pa) was plotted as a function of the shear rate (γ, s−1), and the average viscosity of the system was determined at 9 s−1. All measurements were performed in triplicate.
Ethical protocols
The studies were conducted according to the ethical protocols described in the Guide to the Care and Use of Experimental Animals, the Institutional Animal Care and Use Committee Guidebook and Association for Research in Vision and Ophthalmology (ARVO) Guidelines for the Use of Animals in Ophthalmic and Vision Research. In addition, the experiments were approved by the Ethics Committee of the Facultad de Ciencias Químicas, Universidad Nacional de Córdoba, Argentina (Res HCD 1571/11 and Res HCD 342/09).
In vivo wound-healing test
Twelve healthy male Wistar rats with an average weight of 250–270 g were divided into cages according to the treatment received and kept in a room with controlled temperature (21 ± 5 °C), with free access to water and food and exposed to light/dark cycles of 12 h.
Skin second-degree burns were produced according to a method described by Yaman et al. [7]. First, the rats were anesthetized with a single intraperitoneal injection of 75.5 mg/kg ketamine (Ketonal® 100) and 0.3 mg/kg acepromazine (Inadrim® 1%). Then, the lower dorsal region of each animal was shaved and a visual examination was performed to rule out possible cuts. An injury was made by exposure to a metal device (1 cm in diameter, 10 g cylinder) pre-heated by immersion in boiling water for 20 s without additional pressure. After receiving the burn, the rats were randomized and assigned to three groups (n = 4 per group): treated with CbCipLid hydrogel, treated with SSD cream (reference), and treated with CbNa hydrogel (control). All groups received 0.2 mL of the corresponding treatment, which was applied once every day for 21 days with the aid of a 1-mL syringe, pre-packaged under aseptic conditions. Before each treatment application, the wounds were cleaned with sterile gauze embedded with physiological solution.
An active control (SSD cream) was used as an alternative to no treatment, since we consider that there is already sufficient evidence in the literature of how the model responds to a second-degree burn, which involves the marked presence of inflammatory cells and exudates, a lower number of fibroblasts, the disorganization of collagen fibers, and a delay in the healing processes [4, 22, 23]. Similarly, Yaman et al. and Han et al. [7, 24] used the vehicle of the study formulation as a control. In this way, we managed to reduce the number of experimental animals, according to the Guide Care and Use of Experimental Animals.
Macroscopic examination
The wounds were observed daily in all groups for their appearance, color, size, hair growth, and three clinical signs of a possible infection process (heat, redness, and swelling).
Histopathological study
Burned skin tissue biopsies were collected under anesthesia, using a punch in the center of the wound at 0-, 7-, 14-, and 21-day post-burn. These samples were fixed in 10% neutral buffered formalin, embedded in paraffin, and cut with a microtome into 5 μm sections. Sections were subsequently processed with the hematoxylin-eosin universal technique. Photomicrographs were taken at a magnification of ×100 using an Olympus BX41 optical light videomicroscope and processed with Infinity Analyze® v5.0.2 software. The thickness variation of the epidermis and the amount of fibroblasts in the dermis (20 fields of each biopsy) were recorded and expressed as means ± standard errors from at least four separate experiments. In addition, epidermal continuity and dermal organization were scored as the relative frequency of cases (Table 1).
Collagen organization was quantified as a function of the birefringence observed under polarized light [22], using the same microscope with an interference filter in order to obtain monochromatic light with λ = 546 nm and a Sénarmont compensator that introduced an optical retardation of λ/4. The luminescence intensity observed in the photomicrographs with a magnification of ×100 was quantified with the Image Processing Lab® v2.8.0 software and expressed as the absolute luminescence percentage.
The ANOVA test was used to evaluate differences in epidermal thickness and fibroblastic population among treatments, followed by the Tukey test for mean comparisons. The Chi square method was used to establish statistical associations between histological scores and treatments, which were analyzed using a post-burn time-stratified Cochran-Mantel-Haenszel test. Additionally, birefringence values of the different treatments were compared by ANOVA followed by the Tukey test, with p < 0.05 considered to be significant. Analytical probes were performed using the InfoStat® v.2012 software (InfoStat Group, Argentina).
CbCipLid hydrogel anesthetic effect
The corneal touch threshold (CTT) test was performed to evaluate the duration and intensity of the anesthetic effect of Lid from the hydrogel. This test has been previously used to evaluate the anesthetic capacity of ophthalmic formulations [25,25,27] and was adapted here to compare the anesthetic capacity of Lid from the CbCipLid hydrogel and from a solution containing the same concentration of Lid (0.67%, as hydrochloride, pH = 5.9). In order to obtain isosmotic products, both the CbCipLid hydrogel and Lid solution were prepared using 5% dextrose as vehicle and the final osmolarity was determined by cryoscopic descent with an osmometer (Osmomat 030-D, Gonotec®, Alemania). The isoosmotic Lid solution was used as the positive control instead of SSD cream, since this cream is formulated in a vehicle that is not compatible with ophthalmic administration.
Seven male New Zealand albino rabbits from 2.0 to 2.5 kg were used in these experiments. These animals were kept in a room at 21 ± 5 °C with free access to water and food and exposed to light/dark cycles of 12 h. The rabbits were randomly assigned to three experimental groups: treated with CbCipLid hydrogel, treated with 0.67% Lid in 5% dextrose solution (reference), and treated with 5% dextrose solution (control).
All the treatments were carried out using a single 50-μL conjunctival instillation according to the assigned groups. The right eyes of six rabbits were instilled with the test treatment, while the left ones received the reference treatment. A seventh rabbit received the control treatment in both eyes.
The CTT was measured in the center of the eye of each rabbit using an adapted Cochet-Bonnet corneal esthesiometer, according to a methodology described by McAlvin et al. [25], see Fig. 2a, which consisted of a nylon monofilament of adjustable length from 6.0 to 0.5 cm (esthesiometers 1 to 12, Fig. 2b).
The pressure exerted which is inversely proportional to the length of the monofilament stimulated the corneal touch receptors, thereby inducing the corneal blink reflex. The filament length required to elicit a blink response is a measure of the degree of analgesia, with CTT being defined as the longest monofilament (minimum pressure) that produced a blink response, which was recorded by a blinded investigator. As shown in Fig. 2a, the test was begun by gently placing the monofilament perpendicularly onto the cornea and applying enough pressure to cause the filament to bend. The eyes were probed with the monofilament in this fashion three times, with the minimum interval used between measurements being 1 s. This experiment was commenced using the longest 6.0 cm (esthesiometer 1) to determine a blink response. In the event of a partial blink, the cornea was probed three additional times to confirm the presence or absence of a blink response. If no blink was elicited, the filament length was reduced by 0.5 cm and testing was repeated until a blink was elicited (aesthesiometers 2 … 12). The stimulation period was within ± 30 s. Basal corneal sensitivity (time 0) was measured immediately before treatment instillations. CTT was then subsequently measured at 5, 10, 15, 25, 35, 45, 60, and 75 min, after which, the corneal sensitivity returned to baseline for both treated groups. The control group was treated identically. The anesthetic effect (in arbitrary units) of each treatment was considered the inverse of CTT (cm−1) and plotted vs. time (min). The time to achieve the maximum anesthetic (AEmax), the maximum anesthesia time (Tmax), and the area under the curve (ABC) were determined using the Microsoft Excel® 2010 program.
The anesthetic effect of the treatments at each time was compared by the Kruskal-Wallis test, with p < 0.05 being considered significant. The differences in the area under the curve (AUC) between CbCipLid hydrogel and Lid solution were determined by the t test (p < 0.05), and analytical probes were performed using the InfoStat® v.2012 software (InfoStat Group, Argentina).
An absence of corneal damage after the test was indicated by the lack of fluorescence under blue light after instillation of a drop of fluorescein on each eye.
Results
Preparation of CbCipLid hydrogel
The CbCipLid hydrogel was obtained in minimal steps using water as solvent and a small proportion of sodium. The hydrogel was transparent, with no evidence of precipitated drug, suggesting an acid-base interaction between Cb and the drugs, which produced an increase of at least 17.65 times in the apparent solubility of Cip at neutral pH. The physical and chemical properties of CbCipLid hydrogel remained unchanged after an autoclave cycle and after 6 months of storage at controlled temperature and relative humidity (Table 2 ).
HPLC-UV method validation
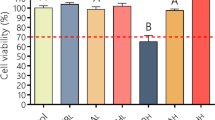
No interference for the qualitative-quantitative determination of Cip and Lid was observed, so the HPLC method used permitted the selective determination of both drugs, with a resolution between peaks of 26 (from Eq. 1). In addition, the calibration curves proved to be linear over the range of concentrations tested (y = 458,077x − 260,463, r2 = 0.9989 for Cip and y = 6956x − 3732, r2 = 0.9999 for Lid). The inter- and intraday values of precision and accuracy were less than 15% for the lower concentration and less than 10% for medium and higher concentrations. Moreover, the samples remained unchanged after a freezing-thawing cycle. All the parameters determined were within the internationally accepted criteria [21].
In vitro release kinetics
Delivery properties of Cip and Lid from CbCipLid hydrogel were studied using water and 0.9% NaCl as receptor media. The solution of NaCl was selected to simulate the saline properties of biological fluids such as burn exudates. When water was the receptor medium, Cip and Lid were slowly delivered from the hydrogel. As water was replaced by NaCl solution, the released rate was significantly increased for both drugs (Fig. 3). The release kinetics fitted the Higuchi model, indicating that the drug release from CbCipLid hydrogel was related to Fick’s law of diffusion. The constant rate increased 3.95 and 8.39 times for Cip and Lid, respectively (Table 3).
a Amount released versus time of Cip (square symbols) and Lid (round symbols), from CbCipLid hydrogel towards 0.9% NaCl (filled symbols) or deionized water (empty symbols) at 37 °C. The values are expressed as means ± standard errors. b Linear fit kinetics of the amount released versus √time of Cip and Lid in 0.9% NaCl and deionized water
Rheological evaluation
Figure 4 shows the shear stress (Ƭ, Pa) as a function of the shear rate (γ, s−1) for CbCipLid hydrogel and CbNa hydrogel at 25 °C. The hydrogel showed a non-Newtonian plastic behavior without thixotropy, presenting a yield stress value higher than 100 Pa. The average viscosity of CbCipLid hydrogel revealed no change for the range of temperatures tested, with values of 150.5 (25 °C), 149.9 (35 °C), and 150.8 Pa s−1 (37 °C). The flow viscosity for CbNa hydrogel was 133.2 at 25 °C.
In vivo wound-healing test
No mortality was seen during the study, with no outward signs of pain or discomfort being noted and the animals’ behavior (e.g., food intake and daily activity) appearing normal. In addition, none of the burn wounds showed any signs of a possible infection (exudate, color changes, etc.).
As observed in Fig. 5, the wounds closed at 21 days in the three groups. However, between days 7 and 14, the narrowing of the wound area in the groups treated with CbCipLid hydrogel and CbNa hydrogel was faster than that in the group treated with SSD cream. On day 14, the CbCipLid hydrogel group showed regenerated skin, which indicated that the wounds were almost healed.
Representative photomicrographs of burn wounds after treatment with SSD cream (reference), CbNa hydrogel (control), and CbCipLid hydrogel. H&E (×100, scale bars are 100 μm). Animals treated with CbNa hydrogel and CbCipLid hydrogel showed more areas with epithelial confluence (day 7). Dermal infiltrate and detritus tended to resolve earlier in rats treated with CbNa hydrogel and CbCipLid hydrogel (day 14). Recovery of skin appendages was earlier seen in CbCipLid hydrogel-treated rats than in those treated with CbNa hydrogel and SSD cream (day 14). Less papillary dermis, which is responsible of epithelial support, was found after the treatment with SSD cream, with collagenous fibers being closer to epidermis (day 21)
A histopathological examination showed a faster epithelization in the CbCipLid hydrogel group, as revealed by the significantly marked thickening of the new epidermis, which culminated on day 7 (p < 0.05) (Fig. 6a) but decreased, as expected, during dermis-related epithelial recovery [28]. In contrast, the maximum epithelium thickening for SSD cream and CbNa hydrogel-treated groups was at 14 days, with the thickness difference between these two groups being non-significant. Continuous epidermis (score 3) was achieved after 7, 14, and 21 post-burn days (Fig. 6b) for CbCipLid hydrogel, CbNa hydrogel, and SSD cream.
a Epidermal thickness (μm) versus time (days) of CbCipLid hydrogel ( ), CbNa hydrogel (
), CbNa hydrogel ( ), and SSD cream (
), and SSD cream ( ). The thickness variation was recorded and expressed as means ± standard errors (*p < 0.05). Statistical analysis was performed with ANOVA followed by the Tukey test for mean comparisons. Error bars represent standard errors of means. b Epidermis scores were recorded as relative frequency of cases/week as absent (
). The thickness variation was recorded and expressed as means ± standard errors (*p < 0.05). Statistical analysis was performed with ANOVA followed by the Tukey test for mean comparisons. Error bars represent standard errors of means. b Epidermis scores were recorded as relative frequency of cases/week as absent ( ), discontinuous (
), discontinuous ( ), and continuous (
), and continuous ( ). Statistical analysis was performed with the Chi square method and then the post-burn time-stratified Cochran-Mantel-Haenszel test (*p < 0.05)
). Statistical analysis was performed with the Chi square method and then the post-burn time-stratified Cochran-Mantel-Haenszel test (*p < 0.05)
The number of dermal fibroblasts increased quickly in both CbCipLid hydrogel and CbNa hydrogel groups, showing a maximum number at 7 days. Both these treatments significantly accelerated fibroblastic recovery, returning to the initial count at 14 days (p < 0.05). However, the number of dermal fibroblasts in the SSD cream group increased more slowly, with a maximum number recorded at 14 days (Fig. 7a).
a Dermal fibroblast (number) versus time of SSD cream ( ), CbNa hydrogel (
), CbNa hydrogel ( ), and CbCipLid hydrogel (
), and CbCipLid hydrogel ( ). The amount of fibroblasts in the dermis was recorded and expressed as means ± standard errors (*p < 0.05). Statistical analysis was performed with ANOVA followed by the Tukey test for mean comparisons. Error bars represent standard errors of means. b Dermis scores were recorded as relative frequency of cases/week as I, complete dermal disorganization (
). The amount of fibroblasts in the dermis was recorded and expressed as means ± standard errors (*p < 0.05). Statistical analysis was performed with ANOVA followed by the Tukey test for mean comparisons. Error bars represent standard errors of means. b Dermis scores were recorded as relative frequency of cases/week as I, complete dermal disorganization ( ); II, reticular recovery with papillary disorganization (
); II, reticular recovery with papillary disorganization ( ); III, recovery of reticular and papillary dermis (
); III, recovery of reticular and papillary dermis ( ); IV, normal reticular dermis with papillary recovery (
); IV, normal reticular dermis with papillary recovery ( ); and V, complete dermal organization (
); and V, complete dermal organization ( ). Statistical analysis was performed with the Chi square method followed by the post-burn time-stratified Cochran-Mantel-Haenszel test (*p < 0.05)
). Statistical analysis was performed with the Chi square method followed by the post-burn time-stratified Cochran-Mantel-Haenszel test (*p < 0.05)
Although the three treatments achieved complete dermal organization after 3 weeks, the CbNa hydrogel and CbCipLid hydrogel groups managed this earlier than the SSD cream group (p < 0.05) (Fig. 7b). In this regard, the epidermal continuity and dermal score were statistically associated (p < 0.0001), i.e., epithelial healing was linked to the recovery of the underlying connective tissue. In agreement, at 21 days, collagen fibers revealed different levels of birefringence (Fig. 8), with the CbCipLid hydrogel group having the highest luminescence, indicating a higher yield, and SSD cream showing the lowest.
Quantification of birefringence-related luminescence for each treatment expressed as percentages. Error bars represent standard errors of means from experimental quadruplicates and their representative photomicrographs (×100, scale bars are 100 μm) are shown at 21 days post-burning. Statistical analysis was performed with ANOVA followed by the Tukey test (*p < 0.05)
CbCipLid hydrogel anesthetic effect
Figure 9 shows the anesthetic effect as a function of time and the parameters obtained from these profiles. The mean baseline CTT of both eyes was in the range from 6 to 5 cm (aesthesiometers 1–3) and, as observed in Fig. 9 , the anesthetic effect of both CbCipLid hydrogel and Lid solution was noticeable from the beginning of the treatment until around 45 min (p < 0.05). However, this effect was statistically higher over time in the CbCipLid hydrogel group until approximately 35 min (p < 0.05). In agreement, the AUC(0–75) obtained in the CbCipLid hydrogel group was 2.66-fold higher than that of the Lid solution group (p < 0.05). No significant differences were observed in Tmax.
Anesthetic effect (arbitrary units) vs. time (min) determined in rabbits eyes treated with dextrose solution ( ), Lid solution (
), Lid solution ( ), and CbCipLid hydrogel (
), and CbCipLid hydrogel ( ). The anesthetic effect was defined as the inverse of CTT (cm−1). Error bars represent standard errors of means. Statistical analysis of the anesthetic effect of the treatments at each time was performed with the Kruskal-Wallis test. The asterisk denotes differences between dextrose solution and both CbCipLid hydrogel and Lid solution and the number sign denotes differences between CbCipLid hydrogel and Lid solution. Differences in the area under the curve (AUC) between the CbCipLid hydrogel and Lid solution were determined by the t test (p < 0.05)
). The anesthetic effect was defined as the inverse of CTT (cm−1). Error bars represent standard errors of means. Statistical analysis of the anesthetic effect of the treatments at each time was performed with the Kruskal-Wallis test. The asterisk denotes differences between dextrose solution and both CbCipLid hydrogel and Lid solution and the number sign denotes differences between CbCipLid hydrogel and Lid solution. Differences in the area under the curve (AUC) between the CbCipLid hydrogel and Lid solution were determined by the t test (p < 0.05)
Discussion
Healing of skin wounds is a complicated process involving epidermal regeneration, fibroblast proliferation, neovascularization, and biomolecule synthesis [4]. Although there have been some advances in treatments, there is no obvious best solution [29].
The systemic delivery of antibiotics entails poor penetration into ischemic and necrotic tissue and can cause systemic toxicity because of the high doses required to produce an effect [30]. There have also been numerous reports of microbial resistance linked to the use of oral or injectable antibiotics [31]. However, the local delivery of antibiotics is an alternative that may enable the maintenance of a high local antibiotic concentration for an extended duration of release without systemic toxicity [32].
The ionic interaction between polyelectrolytes and acid or basic drugs is a valuable resource for obtaining new materials with physicochemical, pharmaceutical, and biopharmaceutical properties that differ from those of their precursors. In the CbCipLid hydrogel, the increase in the apparent solubility of Cip, which allowed the loading of the dose at a pH close to neutrality, is attributed to the ionic interaction between Cb and Cip in aqueous dispersion, which generated a high degree of ionic condensation. In fact, the procedure used to obtain CbCipLid hydrogel permitted an acid-base interaction between the amine groups of Cip (pKa = 8.74) and Lid (pKa = 8.01) with the acidic groups of Cb (pKa ≈ 6), according to Eqs. (2) and (3):
where HN-R-COOH and HN-R-COOH represent Cip and Lid, respectively, and (Cb-COO−+H2N-R-COOH) and (Cb-COO−+H2N-R) represent the ionic pairs.
It is worth noting that the procedure used to obtain the CbCipLid hydrogel is very versatile and may also be used to favor the interaction of Cb with similar drugs containing amine groups, such as moxifloxacin or norfloxacin, which have also been proposed to treat or prevent burn wound infections [33, 34]. Thus, further experiments should now be conducted to explore the feasibility of obtaining similar systems containing these drugs.
As expected, the CbCipLid hydrogel supports final sterilization by autoclaving, which facilitates the fulfillment of the microbiological requirements of products for topical administration in open wounds, i.e., the absence of revivable microorganisms [17]. Preliminary stability information showed that the hydrogel was stable after 6 months under controlled temperature and humidity conditions. Definitive stability studies for registration purposes should be carried out in the final package and under the standardized conditions for the corresponding climatic zone. In addition, Cb is an inexpensive substance, which is important considering that most burn-related deaths occur in low- and middle-income countries.
It has been previously reported that the interaction between Cb and basic drugs yields a high proportion of counterionic condensation. The presence of non-electrolytes does not affect the equilibrium of ion-pair formation, whereas the addition of ions to the system generates ion exchanges and regrouping of charges, causing a partial dissociation of the ion pairs [35, 36]. In agreement, the release of Cip and Lid from the hydrogel was minimal in water but increased significantly in the presence of a biological like-fluid, as a consequence of ion exchange. This rise in the rate of delivery have been attributed mainly to the diffusion of Na+ and Cl− ions from the receptor to the hydrogel compartment, thereby promoting ionic exchange with Cip- or Lid-charged species attached to Cb. This result is consistent with the view that a high proportion of both drugs are under the form of ionic pairs. Thus, if delivery occurred through the Fickian diffusion of free species, and their concentrations were low because of the high proportion of ionic pairs, then the rate of delivery should have remained slow, as was observed when water was the receptor medium. This result also suggests that the dissociation of ion pairs is the slow step that controls the delivery rate. In this way, as Na+ and Cl− diffused into the hydrogel, Na+ promoted the exchange of cationic and zwiterionic species of Lid and Cip, respectively, attached to Cb, while Cl− acted as a counterion that diffused with them. Both these mechanisms would contribute to raising the release rate, as observed. These results are in agreement with previous reports for binary polyelectrolyte-drug systems [15, 35, 37, 38].
It is known that for an antibacterial to be effective and to exert its bactericidal action, it must reduce the number of colony forming units per milliliter by at least 99.9% compared with the initial inoculum count [39]. Considering the bactericidal concentration values of Cip against Pseudomonas aeruginosa ATCC® 27853 and Staphylococcus aureus ATCC® 29213 [40], it can be inferred that this values were achieved in vitro in the first 30–45 min of Cip release and were maintained for at least 24 h. Although the release of both drugs increases when the receptor medium is NaCl, at 24 h still not 100% of the dose was released. This may be because the Franz cells are a closed system. However, it would be expected that the permanent flow dynamics of the wounds would allow the total dose to be led from the CbCipLid hydrogel, which would act as a reservoir. Thus, the low amount of antibiotic released should not be interpreted as a drawback of the formulation. Indeed, previous studies have shown the reversibility of the interaction in several polyelectrolyte-drug systems [37, 38, 41].
In addition, a significant anesthetic effect was observed from 5 min, suggesting that the system provides an immediate anesthetic effect in spite of the controlled release. This aspect, combined with the cooling effect produced by hydrogels could provide a favorable feeling for the patient. The higher anesthetic effect produced by the CbCipLid hydrogel can be attributed to the viscosity of the system and the mucoadhesiveness of Cb which would increase drug retention at the site of application with a better efficacy. The sustained release of the drugs has advantages from the clinical point of view, because it requires lower frequencies of application, which translate into less pain and stress for the patient [5].
The rheological behavior of CbCipLid hydrogel was tested at body temperatures (35 and 37 °C) as well as at room temperature (25 °C). The results obtained are consistent with those reported by Barry and Meyer [42] and Pena [43], who established that Cb hydrogels possess good stability properties where viscosity, critical stress value, and plastic flow characteristics are not affected by temperature. Plasticity is a desirable consistency feature of topical formulations [44], because they have a low resistance to flow at high-speed conditions, considering that at rest the flow is zero [45]. This rheological behavior is of great importance, as it helps applications to stay on the skin without slipping. In addition, plasticity is an advantage from the point of view of packaging, since the hydrogel would maintain its consistency in the container, but at the moment of applying an external force, it would begin to flow [46, 47]. The absence of thixotropy permits the immediate recovery of viscosity when shear is arrested and both the high yield value and quick break make the CbCipLid hydrogel ideal for dispensing [43]. In addition, due to the biomucoadhesive properties of the Cb, the hydrogel would remain on the surface of application for a reasonable time and, if necessary, could be removed from the skin by a simple washing.
It is well known that the body tends to repair wounds and to re-establish the normal continuum of the structures in the shortest time possible [7]. Immediately after an injury, there is an increased synthesis of extracellular matrix components in the wound area. The treatment with CbCipLid hydrogel decreased the wound-healing period compared with the current gold standard treatment (SSD cream). In fact, the presence of the hydrogel was associated with a greater number of fibroblasts, which generated an extracellular matrix in the damaged areas, after which, fibroblast number can return to basal levels. As a consequence, the epithelia could grow on top, due to the supportive effect of dermal connective tissue on the epidermal biology [48]. Therefore, epidermal continuity and integrity was installed early by the CbCipLid hydrogel. This accelerated effect on wound healing compared with the SSD cream is consistent with a previous study performed on pigs with second-degree burns infected and treated with a keratin hydrogel and Cip [49].
The faster healing observed not only in the case of CbCipLid hydrogel but also in the CbNa hydrogel group may be related to the moist environment provided by the hydrogels, which is convenient for cell viability and physiology and promotes initial cooling and subsequent healing of burn wounds [50, 51]. The faster epithelization observed with the CbCipLid hydrogel respect to CbNa hydrogel might also be attributed to the presence of Cip, which prevent deleterious bacterial invasion [5, 52].
Current data available about Cb derive from contradictory in vitro studies with scarce in vivo information [52, 53]. However, Jettanacheawchankit et al. [54] studied in vivo wound healing and found that Cb hydrogel significantly enhanced wound healing compared with normal saline, with this effect resulting from its mucoadhesive properties that acted as a wound dressing to prevent contamination and irritation.
The birefringence of extracellular collagen fibers under polarized light has been used as a marker of their structural integrity, with their luminescence being reduced due to protein denaturalization associated with heat [55]. Hence, the increase in luminescence of damaged skin over time represents a marker of protein structure recovery in a burned skin [56]. The luminescence value of CbCipLid hydrogel at day 21 was significantly higher than that observed for SSD cream, because of the increased fibroblast proliferation on day 7, which promoted collagen deposition. In agreement with the wound-healing test, the higher luminescence values presented by the CbCipLid hydrogel compared with CbNa hydrogel may be explained by the faster healing rate provided by the antimicrobial properties of Cip. In contrast, SSD cream showed the lowest luminescence values, which might have been related to SSD cytotoxicity on fibroblasts [8], the cream composition, or a combination of both.
Since the rabbit eye is a mucosa with permanent fluid flow, it can simulate conditions similar to those present in an open wound or exudative burn. It is known that an anesthetized cornea decreases its sensitivity to a stimulus and different techniques and instruments have been developed over the years to quantify the sensitivity of the cornea. Several authors have used corneal aesthesiometer methodologies to determine the ability of different drugs to inhibit corneal sensitivity, such as anesthetics [25,25,27, 57]. According to the data obtained, CbCipLid hydrogel yielded an anesthetic effect significantly more intense than that produced by the Lid solution. This might have occurred because of the ability of Cb to generate viscous hydrogels that are capable of interacting with the mucus layer or tissues of the eye [58], which can lead to an increase in the pre-corneal residence time and thus augment the anesthetic effect. Therefore, these results can be compared with the ability of the system to produce an anesthetic effect after being applied to the wound injury.
Several new systems containing peptides, growth factors, and cells [59,59,61] have shown the ability to increase wound healing and improve burn treatment. Compared with these, the CbCipLid hydrogel presents several advantages such as low cost, stability, ease of preparation, and a sustained release that require lower frequencies of application. In fact, the hydrogel may be obtained in other forms, such as film or powder which will be explored in future studies.
Collectively, the results obtained demonstrate that the CbCipLid hydrogel could be a versatile new platform for the controlled topical delivery of antimicrobial-anesthetic agents in the treatment of second degree burns.
References
World Health Organization. Burns [Internet]. Fact sheet No. 365. 2017. Available from: http://www.who.int/mediacentre/factsheets/fs365/en/
Li J, Zhang Y-P, Zarei M, Zhu L, Sierra JO, Mertz PM, et al. A topical aqueous oxygen emulsion stimulates granulation tissue formation in a porcine second-degree burn wound. Burns [Internet]. Elsevier Ltd and International Society of Burns Injuries. 2015;41(5):1049–57. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25554261
Wasiak J, Cleland H, Campbell F, Spinks A. Dressings for superficial and partial thickness burns. Cochrane database Syst Rev. England; 2013;(3):CD002106.
Alemdaroǧlu C, Deǧim Z, Çelebi N, Zor F, Öztürk S, Erdoǧan D. An investigation on burn wound healing in rats with chitosan gel formulation containing epidermal growth factor. Burns. 2006;32(3):319–27.
Roy DC, Tomblyn S, Isaac KM, Kowalczewski CJ, Burmeister DM, Burnett LR, et al. Ciprofloxacin-loaded keratin hydrogels reduce infection and support healing in a porcine partial-thickness thermal burn. Wound Repair Regen [Internet]. 2016;24(4):657–68. https://doi.org/10.1111/wrr.12449.
ANMAT. Vademécum Nacional de Medicamentos: Platsul A [Internet]. 2018. Available from: http://anmatvademecum.servicios.pami.org.ar/index.html. Accessed 12 Feb 2018
Yaman I, Durmus a S, Ceribasi S, Yaman M. Effects of Nigella sativa and silver sulfadiazine on burn wound healing in rats. Vet Med (Praha) 2010. 55(12):619–24.
Tarameshloo M, Norouzian M, Zarein-Dolab S, Dadpay M, Gazor R. A comparative study of the effects of topical application of Aloe vera, thyroid hormone and silver sulfadiazine on skin wounds in Wistar rats. Lab Anim Res [Internet]. 2012;28(1):17–21. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3315193&tool=pmcentrez&rendertype=abstract
Hoeksema H, Vandekerckhove D, Verbelen J, Heyneman A, Monstrey S. A comparative study of 1% silver sulphadiazine (Flammazine) versus an enzyme alginogel (Flaminal) in the treatment of partial thickness burns. Burns [Internet]. Elsevier Ltd Int Soc Burns Injuries. 2013;39(6):1234–41. https://doi.org/10.1016/j.burns.2012.12.019.
Bagri LP, Bajpai J, Bajpai AK. Evaluation of starch based cryogels as potential biomaterials for controlled release of antibiotic drugs. Bull Mater Sci. 2011;34(7):1739–48.
Abdelkader H, Mansour HF. Comparative studies for ciprofloxacin hydrochloride pre-formed gels and thermally triggered (in situ) gels: in vitro and in vivo appraisal using a bacterial keratitis model in rabbits. Pharm Dev Technol England. 2015;20(4):410–6.
Olivera ME, Manzo RH, Junginger HE, Midha KK, Shah VP, Stavchansky S, et al. Biowaiver monographs for immediate release solid oral dosage forms: ciprofloxacin hydrochloride. J Pharm Sci United States. 2011;100(1):22–33.
Cassens J, Prudic A, Ruether F, Sadowski G. Solubility of pharmaceuticals and their salts as a function of pH. Ind Eng Chem Res. 2013;2731(1):2721–31.
Lubrizol. Carbopol® Polymer Products [Internet]. 2018. Available from: https://www.lubrizol.com/Life-Sciences/Products/Carbopol-Polymer-Products
Vilches AP, Jimenez-Kairuz A, Alovero F, Olivera ME, Allemandi DA, Manzo RH. Release kinetics and up-take studies of model fluoroquinolones from carbomer hydrogels. Int J Pharm. 2002;246(1–2):17–24.
Bermúdez JM, Jimenez-Kairuz AF, Olivera ME, Allemandi DA, Manzo RH. A ciprofloxacin extended release tablet based on Swellable drug polyelectrolyte matrices. AAPS PharmSciTech [Internet]. 2008;9(3):924–30. Available from:. https://doi.org/10.1208/s12249-008-9098-9.
Ministerio de Salud; Secretaría de Políticas Regulación e Institutos; Administración Nacional de Medicamentos Alimentos y Tecnología Médica; Instituto Nacional de Medicamentos. Farmacopea Argentina [Internet]. 7th ed. Comisión Permanente de la Farmacopea Argentina, editor. Ciudad Autónoma de Buenos Aires; 2003. Available from: http://www.anmat.gov.ar/webanmat/fna/fna.asp
ANMAT. Vademecum Nacional de Medicamentos: fotamicin [Internet]. 2018. Available from: http://anmatvademecum.servicios.pami.org.ar/index.html. Accessed 12 Feb 2018
Dash S, Murthy PN, Nath L, Chowdhary P. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol Pharm. 2010;67(3):217–23.
The United States Pharmacopeial Convention. The United States Pharmacopeia and The National Formulary. The United States Pharmacopeia 40 The National Formulary 35 [Internet]. USP40 NF35. United States Pharmacopoeial Convention, Washington, DC; 2017. Accessed 12 Feb 2018. Available from: http://www.uspnf.com/uspnf/pub/index?usp=37&nf=32&s=2&officialOn=December 1, 2014.
International Conference on Harmonization (ICH). ICH topic Q2 (R1) validation of analytical procedures: text and methodology. Int Conf Harmon. 2005;4:1–13.
Gomes MT, Campos GRS, Piccolo N, França CM, Guedes GH, Lopes F, et al. Experimental burns: comparison between silver sulfadiazine and photobiomodulation. Rev Assoc Med Bra. 2017;63(1):29–34.
Turatti Pessolato AG, dos SantosMartins D, Ambrósio CE, Mananares CAF, de Carvalho AF. Propolis and amnion reepithelialise second-degree burns in rats. Burns. 2011;37(7):1192–201.
Han M, Durmus A, Karabulut E, Yaman I. Effects of Turkish Propolis and silver sulfadiazine on burn wound healing in rats. Rev Méd Vét. 2005;156(12):624–7.
McAlvin JB, Zhan C, Dohlman JC, Kolovou PE, Salvador-Culla B, Kohane DS. Corneal anesthesia with site 1 sodium channel blockers and dexmedetomidine. Investig Ophthalmol Vis Sci. 2015;56(6):3820–6.
Sharrow-Reabe KL, Townsend WM. Effects of action of proparacaine and tetracaine topical ophthalmic formulations on corneal sensitivity in horses. J Am Vet Med Assoc [Internet] 2012;241(12):1645–1649. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L366342142%5Cnhttp://avmajournals.avma.org/doi/pdf/https://doi.org/10.2460/javma.241.12.1645%5Cnhttp://dx.doi.org/10.2460/javma.241.12.1645%5Cnhttp://novacat.nova.edu:4550/resserv?sid=EMBASE&issn=00031488.
Wang L, Shankarappa S, Tong R, Ciolino J, Tsui J, Chiang H, et al. Topical drugs formulations for prolonged corneal anesthesia. Cornea. 2013;32(7):1040–5.
Golberg A, Khan S, Belov V, Quinn KP, Albadawi H, Felix Broelsch G, et al. Skin rejuvenation with non-invasive pulsed electric fields. Sci Rep [Internet]. 2015;5:10187. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4428072&tool=pmcentrez&rendertype=abstract
Boateng J, Catanzano O. Advanced therapeutic dressings for effective wound healing—a review. J Pharm Sci [Internet]. 2015;104(11):3653–80. https://doi.org/10.1002/jps.24610.
Sinha M, Banik RM, Haldar C, Maiti P. Development of ciprofloxacin hydrochloride loaded poly(ethylene glycol)/chitosan scaffold as wound dressing. J Porous Mater. 2013;20(4):799–807.
World Health Organization (WHO). Antimicrobial resistance. Global report on surveillance [Internet]. Switzerland. World Health Organization (WHO). 2014. 232 p. Available from: http://www.who.int/drugresistance/en/%0AISBN
Zilberman M, Elsner JJ. Antibiotic-eluting medical devices for various applications. J Control Release. 2008;130(3):202–15.
Dua K, Malipeddi VR, Madan J, Gupta G, Jesus TDE, Pinto A. Norfloxacin and metronidazole topical formulations for effective treatment of bacterial infections and burn wounds. Interv Med Appl Sci. 2016;8(2):68–76.
Jacobsen F, Fisahn C, Sorkin M, Thiele I, Hirsch T, Stricker I, et al. Efficacy of topically delivered moxifloxacin against wound infection by Pseudomonas aeruginosa and methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2011;55(5):2325–34.
Jimenez-kairuz A, Allemandi D, Manzo RH. Mechanism of lidocaine release from carbomer ± lidocaine hydrogels. J Pharm Sci. 2002;91(1):267–72.
Esteban SL, Manzo RH, Alovero FL. Azithromycin loaded on hydrogels of carbomer: chemical stability and delivery properties. Int J Pharm. 2009;366:53–7.
Guzmán ML, Soria EA, Laino C, Manzo RH, Olivera ME. Reduced food interaction and enhanced gastrointestinal tolerability of a new system based on risedronate complexed with eudragit e100. Mechanistic approaches from in vitro and in vivo studies. Eur J Pharm Biopharm. 2016;107:263–72.
Battistini FD, Boiero C, Palma SD, Allemandi DA, Manzo RH, Olivera ME, et al. The role of hyaluronan as a drug carrier to enhance the bioavailability of extended release ophthalmic formulations. Hyaluronan-timolol ionic complexes as a model case. Eur J Pharm Sci. 2017;49(4):588–94.
Alovero FL, Olivera ME, Manzo RH. In vitro pharmacodynamic properties of a fluoroquinolone pharmaceutical derivative: hydrochloride of ciprofloxacin-aluminium complex. Int J Antimicrob Agents. 2003;21(5):446–51.
Clinical and Laboratory Standars Institute (CLSI). EM100 Connect-CLSI M100 S27:2017 [Internet]. 2017. Available from: http://em100.edaptivedocs.info/GetDoc.aspx?doc=CLSI M100 S27:2017&scope=user.
Quinteros DA, Rigo VR, Kairuz AFJ, Olivera ME, Manzo RH, Allemandi DA. Interaction between a cationic polymethacrylate (Eudragit E100) and anionic drugs. Eur J Pharm Sci Netherlands. 2008;33(1):72–9.
Barry BW, Meyer MC. Rheological properties of carbopol gels: 1. Continuous shear and creep properties of carbopol gels. Int J Pharm. 1979;2:1–25.
Pena LE. Gel dosage forms: theory, formulation and processing. In: Oborne D, Amann A, editors. Drug and the pharmaceutical sciences. New York: Marcel Dekker; 1990. p. 381–8.
Bousmina M. Rheology of polymer blends: linear model for viscoelastic emulsions. Rheol Acta. 1999;38(1):73–83.
Ruiz Martinez MA, Lopez-Viota Gallardo J, de Benavides MM, de Dios Garcia Lopez-Duran J, Gallardo Lara V. Rheological behavior of gels and meloxicam release. Int J Pharm. 2007;333(1–2):17–23.
Kutschmann E, Haake G, Karlsruhe D. Rheological analysis of the stability of pharmaceutical suspensions [Internet]. Vol. V98–154E. 2004. Available from: http://www.rhl.pl/files/17905/Pomiary_i_analiza_stabilnosci_dodatkow_farmaceutycznych.pdf.
Kutschmann E, Gmbh GH, Karlsruhe D. Yield point determination—a critical discussion of different methods [Internet]. 2000. Available from: http://www.rhl.pl/files/17736/Pomiary_punktu_plyniecia.pdf.
Rosin NL, Agabalyan N, Olsen K, Martufi G, Gabriel V, Biernaskie J, et al. Collagen structural alterations contribute to stiffening of tissue after split-thickness skin grafting. Wound Repair Regen [Internet]. 2016;24(2):263–74. Available from: http://doi.wiley.com/10.1111/wrr.12402
Wang XQ, Kravchuk O, Liu PY, Kempf M, Boogaard CVD, Lau P, et al. The evaluation of a clinical scar scale for porcine burn scars. Burns. 2009;35(4):538–46.
Martineau L, Shek PN. Evaluation of a bi-layer wound dressing for burn care: I. Cooling and wound healing properties. Burns. 2006;32(1):70–6.
Caron I, Rossi F, Papa S, Aloe R, Sculco M, Mauri E, et al. A new three dimensional biomimetic hydrogel to deliver factors secreted by human mesenchymal stem cells in spinal cord injury. Biomaterials. 2016;75:135–47.
Chen X, Peng LH, Shan YH, Li N, Wei W, Yu L, et al. Astragaloside IV-loaded nanoparticle-enriched hydrogel induces wound healing and anti-scar activity through topical delivery. Int J Pharm. 2013;447(1–2):171–81.
Guo X, Huang S, Sun J, Wang F. Comparison of the cytotoxicities and wound healing effects of hyaluronan, carbomer, and alginate on skin cells in vitro. Adv Skin Wound Care. 2015;28(9):410–4.
Jettanacheawchankit S, Sasithanasate S, Sangvanich P, Banlunara W, Thunyakitpisal P. Acemannan stimulates gingival fibroblast proliferation; expressions of keratinocyte growth factor-1, vascular endothelial growth factor, and type I collagen, and wound healing. J Pharmacol Sci. 2009;109(4):525–31.
Huang Y, Meek KM, Ho MW, Paterson CA. Anaylsis of birefringence during wound healing and remodeling following alkali burns in rabbit cornea. Exp Eye Res [Internet]. 2001;73(4):521–32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11825023
Le V-H, Lee S, Kim B, Yoon Y, Yoon CJ, Chung WK, et al. Correlation between polarization sensitive optical coherence tomography and second harmonic generation microscopy in skin. Biomed Opt Express [Internet]. 2015;6(7):2542. Available from: https://www.osapublishing.org/boe/abstract.cfm?uri=boe-6-7-2542
Lawrenson JG, Ruskell GL. Investigation of limbal touch sensitivity using a Cochet-Bonnet aesthesiometer. Br J Ophthalmol [Internet]. 1993;77(6):339–43. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=504526&tool=pmcentrez&rendertype=abstract
Boddeda B, Ratna JV, Battu H. A review on mucoadhesive polymers in ophthalmics. Int J Pharm Sci Rev Res. 2014;24(1):237–45.
Yergoz F, Hastar N, Cimenci CE, Ozkan AD, Tekinay T, Guler MO, et al. Heparin mimetic peptide nanofiber gel promotes regeneration of full thickness burn injury. Biomaterials. 2017;134:117–27.
Volkova N, Yukhta M, Pavlovich O, Goltsev A. Application of cryopreserved fibroblast culture with au nanoparticles to treat burns. Nanoscale Res Lett. 2016;11(1):22.
Jin G, Prabhakaran MP, Kai D, Ramakrishna S. Controlled release of multiple epidermal induction factors through core—shell nanofibers for skin regeneration. Eur J Pharm Biopharm. 2013;85(3, part A):689–98.
Acknowledgements
María Florencia Sanchez thanks for the CONICET fellowship. We thank Dr. Paul Hobson, native speaker, for revision of the manuscript.
Funding
This work was supported by Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET, grant number PIP 2013-2015, 11220120100461), the Fondo para la Investigación Científica y Tecnológica (FonCyT, grant number PICT 0173), and the Universidad Nacional de Córdoba (SECYT-UNC, grant number 162/12).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sanchez, M.F., Breda, S.A., Soria, E.A. et al. Ciprofloxacin-lidocaine-based hydrogel: development, characterization, and in vivo evaluation in a second-degree burn model. Drug Deliv. and Transl. Res. 8, 1000–1013 (2018). https://doi.org/10.1007/s13346-018-0523-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-018-0523-7







 ) 25, (
) 25, ( ) 35, (
) 35, ( ) 37 °C, and CbNa hydrogel (
) 37 °C, and CbNa hydrogel ( ) at 25 °C. All measurements were taken in triplicate
) at 25 °C. All measurements were taken in triplicate



