Abstract
The purpose of the present investigation was to explore the effect of cyclodextrin (CD) as permeation enhancer through rat skin in the form of a valuable and stable transdermal drug delivery system by exploiting its favorable properties. Phase-solubility studies demonstrated that the CD:drug ratio 1:2 was employed in complexation. Solid-state characterizations of complexes was performed by differential scanning calorimetry, X-ray diffractometry, Fourier transform infrared, nuclear magnetic resonance spectrophotometry analysis, and scanning electron micrograph. The HP-β-CD by virtue of its greater stability than the pure curcumin (CMN), allowed greater transdermal flux of CMN indicative of enhanced permeation via CMN-2-hydroxy propyl β cyclodextrins (HP-β-CD). Permeability studies of drug, complex, and with various penetration enhancers (PEs), were performed through rat skin, highlighted a favorable effect of CDs on drug permeation rate, due to its solubilizing action; in contrast with unpredictably poor skin permeation of pure drug. The complexes were found to cause relatively less irritation as compared to the pure drug and drug with PEs in skin irritation studies. The anti-inflammatory activity using paw odema model showed that the formulations of CMNCur–HP-β-CD complex exhibited significant (p < 0.001) decrease in paw edema volume than its pure CMN gel demonstrating enhanced biological activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Transdermal drug delivery systems (TDDS) provide a variety of advantages such as high patient compliance, bypassing gastrointestinal and hepatic elimination pathways and easily administered portable and economical dosage form. Thereby, TDDS are beneficial over oral and intravenous dosage forms and show pattern of sustained release of drug directly in the blood circulation over a long period of time. Skins PEs are employed to optimize TDDS for drugs that are otherwise inadequately skin permeable [1]. Mechanistic approach and activity of skin PE depend on the physicochemical properties of the penetrant as well as the enhancer. The fabrication of TDDS is based on a selection of suitable skin PEs that would be facilitated by an understanding of their mode of action within the target tissue. 2-hydroxy propyl β cyclodextrins (HP-β-CDs) represent one of the favorable PE groups due to their biocompatibility, low toxicity, and irritability profile [2].
Cyclodextrins (CDs) are oligosaccharides composed of glucose molecules with torus-shaped cyclic fashion. They have tendency to form inclusion complexes with drugs thereby alter their physico-pharmaceutical properties. In order to improvise carrier properties, CDs have been chemically modified to alter their water solubility, hygroscopicity, and surface activity, etc. CDs and their derivatives have been utilized for enhancing the solubility and stability against acid/alkali/enzyme hydrolysis of drugs [3, 4]. This makes CDs as a supermolecular structure employed for rapid, sustained and targeted delivery of drugs by oral, nasal and parenteral routes [5]. Effects of CDs on topical bioavailability of drugs have been explored since decades but possible mechanism of skin permeability by CDs is not understood. Some researchers have explained availability of drug in a more diffusible form due to solubilization by CDs at the barrier exterior and thus partitioning from the CDs cavity into the lipophilic barrier as one of the mechanism [6], whereas others have illustrated extraction of lipophilic components from stratum corneum as a probable concept [7]. Transdermal applications of CDs inclusion complex have been investigated and its potential explained as one of the emerging skin penetration tool including dexamethasone [8], ethyl-4-biphehnyl acetate (1) ethyl-4-biphenyl acetic acid a prodrug [9], piroxicam [8], diclofenac [9], bupranolol [10], ketoprofen [11], avobenzone [12]. However, hydrophilic CD drug complexes showed limited permeability contrary to the above-mentioned reports due to lack in understanding of mechanistic approach of permeation through transdermal delivery system being not fully exploited [13]. Klang et al. [14] could enhance the stability and skin permeation of progesterone nanoemulsions by sucrose stearate and cyclodextrins. Ungaro et al. [15] have demonstrated the use of cyclodextrins as solubilizing agents for simvastatin and effect of hydroxypropyl-β-cyclodextrin on lactone/hydroxyacid aqueous equilibrium and confirmed CD-based formulations as effective and beneficial for a specific therapeutic use.
Curcumin (CMN) is a poor water-soluble alkaloidal anti-inflammatory drug, broadly used as analgesic and for the treatment of rheumatoid arthritis and osteoarthritis [16] and has antioxidant properties [17]. It also has beneficial effects on platelet aggregation and vascular prostaglandin synthesis [18]. Upon oral administration, it undergoes an extra-ordinary first-pass metabolism (>90 % in humans) and is rapidly eliminated with a biological half-life of (1.5–2.0 h). It has been associated with poor gastro-intestinal absorption and extensive first pass metabolism and, consequently, leads to poor oral bioavailability; these shortcomings can be surmounted by its transdermal administration. However, it is well known that, owing to the strong barrier function of the skin, transdermal permeation of drugs has to be aptly enhanced [19].
Since CMN is a wonder herbal drug, which has potential to eradicate various diseases, various scientific data would be desirable to help further investigations. The use of CMN is limited due to its inadequate stability, very poor water solubility, and low oral bioavailability. Our investigation suggests that the developed HP-β-CD complex of CMN may help alleviate the inherent problems and thus prove to be a promising alternative to traditional formulations of CMN.
Purpose of the current study was to investigate the possible effectiveness and prospective of cyclodextrins' tailored TDDS. In the present study, cyclodextrin complexes were synthesized and characterized by various techniques. The CD complexes were extensively studied as an effective tool for skin permeation and were compared with various PEs by analyzing release kinetic profiles and calculating permeation through hairless mouse skin model. The developed formulation can serve as an efficient, safe, and biocompatible drug delivery vehicle for transdermal applications.
Materials and methods
Materials
CMN, Carbopol 940, polyethylene glycol (PEG 400), Triethanolamine (TEA), propylene glycol, and sodium lauryl sulphate (SLS) were purchased from Central Drug House Pvt. Ltd. (Mumbai, India). 2-HP-β-CD, dimethyl sulphoxide (DMSO), methanol (HPLC grade), 0.45 μm Millipore filter and cellulose dialysis membrane (pore diameter 2.4 nm) were purchased from Himedia Laboratories Ltd. (Mumbai, India).
Phase-solubility studies
Phase-solubility studies of CMN with HP-β-CD were carried out according to previously reported method [20]. CMN in excess of its solubility was weighed into a series of screw-capped vials containing aqueous phosphate buffer solution (pH 5) of HP-β-CD, concentration ranging from 2 to 14 mM. The vials were agitated on a water bath incubator shaker for 1 week at RT (27 ± 0.5 °C) and equilibrated for further 24 h. The resultant mixture was centrifuged (4,000 rpm for 30 min), and the clear supernatant was passed through 0.45-μm Millipore filter. The drug content of samples was determined spectrophotometrically at 420 nm [21]. The apparent stability constant and thermodynamic parameters were calculated for 1:2 drug:HP-β-CD complex. Apparent stability constants (KC) of HP-β-CD complex with CMN were calculated from UV–visible spectra according to Benesi–Hildebrand equation [22].
Preparation of solid complexes of CMN–HP-β-CD
The solid complexes of CMN with HP-β-CD in a molar ratio of 1:2 (drug: HP-β-CD) were prepared as (1) inclusion complex prepared by physical mixture (ICPPM), (2) inclusion complex prepared by lyophilization method (ICPLM), and (3) inclusion complex prepared by solvent evaporation method (ICPSEM), reported previously [23]. The overview of project is summarized in Fig. 1.
Physical mixture
CMN complex was prepared according to the method reported elsewhere [24]. Briefly, an appropriate amount of CMN was weighed and triturated with HP-β-CD, in 1:2 molar ratios in a mortar for 10 min at RT and the final product was used for further studies.
Solvent evaporation method
In this method, CMN and HP-β-CD were taken in molar ratio of 1:2. CMN was dissolved in minimum quantity of methanol at 60 °C, HP-β-CD was dissolved in aqueous buffer (pH 5), and then dissolved CMN was added dropwise into 2:5 equivalent of HP-β-CD aqueous buffer solution (pH 5) at 60 °C with continuous stirring and was refluxed with continuous agitation at 70 °C for about 4 h. The reaction mixture was again stirred for 1 h at 70 °C to remove residual methanol without reflux. Resulting solution was cooled at RT. After stirring for 8 h at RT, the reaction mixture was stored overnight at 4 °C and then filtered off in a sintered glass filter. The product was dried in a vacuum oven at temperature (50–55 °C), and the dried crystalline product was obtained [23].
Lyophilization method
Complex was prepared by lyophilization method as reported previously [24]. Briefly, 1:2 concentrations of CMN and HP-β-CD (8 mM for HP-β-CD) were dissolved in aqueous buffer solution (pH 5) containing 5 % glucose as a cryoprotectant. The mixture was agitated for 1 week at RT (27 ± 0.5 °C) and filtered through 0.45-μm Millipore filter, and the filtrate was lyophilized in a lyophilizer Hetero Dry Winner, Germany.
Solubility measurement
The aqueous solubility of the compounds, i.e., plain CMN and its complex (1:2:: CMN: HP-β-CD) was determined in PBS buffer (pH 5) at RT (27 ± 5 °C) according to the reported method [25].
Differential scanning calorimetry
The differential scanning calorimetry (DSC) curves of the different samples were measured with TA Instrument 2910 MDSC V4.4E, Shin, Osaka, Japan) under flow of nitrogen at a scanning rate of 10 °C per minute, heating rate of 20 °C/min and temperature range of 100–200 °C for sample size 0.5–3 mg.
Powder X-ray diffraction
X-ray diffractrograms were obtained with an X-ray diffractometer (Rigaku D/Max-1200; Rigaku Denki Co., Tokyo, Japan) using Ni-filtered CuKa radiation (35 kV, 15 mA).
Fourier transform infrared spectroscopy
The FTIR spectra of the samples were recorded on Thermo Nicolet Corporation, USA instrument, IR 200 with DTGS detector assembly and ZnSe Crystal as sample holder. Transmission range was 20,000 to 650 cm−1. The FTIR spectra of the CMN–HP-β-CD complex prepared by solvent evaporation were recorded on Testscan Shimadzu FTIR 8000 series.
Nuclear magnetic resonance
Nuclear magnetic resonance (NMR) spectroscopy of the complex sample was carried out at 300 MHz, in D2O as solvent (Bruker DRX 300 MHz, Billerica, MA).
Scanning electron micrograph
The shape and surface morphology of HP-β-CD, CMN, their physical mixtures and complexes were investigated using SEM. The samples were prepared by lightly sprinkling the formulation on a double-adhesive tape stuck to an aluminum stub. The stubs were then coated with gold to a thickness of ∼300 Å under an argon atmosphere using a gold sputter module in a high-vacuum evaporator. The coated samples were then randomly scanned and photomicrographs were taken with a SEM (Jeol JSM-1600, Tokyo, Japan).
Formulation and characterization of carbopol gel
Carbopol gel was prepared according to the method reported elsewhere [26]. Briefly, Carbopol 940 (1 g) was dispersed in distilled water (88 g) by mechanical stirring at 800 rpm for 60 min at RT. Propylene glycol (10 g) was added to this solution and the resulting mixture was neutralized by dropwise addition of triethanolamine. Mixing was continued until a transparent gel appeared, while the amount of the base was adjusted to achieve a gel with pH 5.0, optimum for the transdermal preparation and the physicochemical properties of gel such as pH, viscosity and percentage drug content. The data of physicochemical properties of optimized gel is shown in Table 1.
Skin permeation studies
Male albino rats (160 ± 20 g) were treated with an overdose of chloroform by inhalation and were sacrificed. After clipping of the hair dorsal skin was excised and subcutaneous fat was removed by means of subcutaneous blunt dissection. The in vitro skin permeation of Carbopol gel of plain drug (ICPLM) was studied using locally fabricated Franz diffusion cell with an effective permeation area and receptor cell volume of 1.0 cm2 and 10 mL, respectively, at RT (27 ± 0.5 °C). The full thickness skin was clamped by an “O” ring between the donor and the receptor chambers of a Franz diffusion cell, with the stratum corneum side facing upward into the donor compartment. The receptor compartment contained 10 mL PBS (pH 5.0) and was constantly stirred in a magnetic stirrer (Expo India Ltd., Mumbai, India) at 100 rpm. The Carbopol gel of ICPLM (250 μl) was applied on to the skin in donor compartment, which was then covered with parafilm to avoid any evaporation process. Samples were withdrawn through the sampling port of the diffusion cell at predetermined time intervals over 24 h and analyzed for drug content by UV spectroscopy [27]. The receptor phase was immediately replenished with equal volume of fresh diffusion buffer. Similar experiments were performed with plain CMN-Carbopol gel. Sink conditions were maintained throughout the experiment. The amount of CMN retained in the skin was determined at the end of the in vitro permeation experiment (24 h). The skin was washed with methanol and homogenized for 5 min in a stirrer. The resulting solution was centrifuged for 10 min at 7,000 rpm. The supernatant was analyzed for drug content by UV spectroscopy. The cumulative amount of drug permeated per unit area was plotted as a function of time; the steady-state permeation rate (Jss) and lag time (LT, h) were calculated from the slope and x intercept of the linear portion, respectively.
Anti-inflammatory activity
The formulations of CMN, ICPLM, CMN-SLS, and CMN-DMSO gel were selected for screening for anti-inflammatory activity and compared with marketed Whitefield Ointment I.P. (Kremoint Pharma Pvt. Ltd., India), containing benzoic acid I.P. (6 % w/w) and salicylic acid I.P. (3 % w/w).
Total 36 albino rats of either sex weighing 100–150 g, were selected and divided into six groups of six animals each. The experimental protocol was duly approved by the Institutional Animal Ethical Committee by letter number Animal Eths. Comm./DB/304 of Dr. H. S. Gour University, Sagar, M.P. India. The first group served as control and was treated with plain Carbopol gel. Second group was treated with marketed formulation. The animals of the third, fourth, fifth, and sixth groups were treated with different formulations of CMN, such as plain CMN gel, gel of ICPLM, CMN-SLS, and CMN-DMSO, respectively. After weighing the rats individually, they were marked. The initial paw volume of each animal at the start of the experiment was measured by plethysmometer (Ugo Basile, 7140, Italy). One hour post-topical application, 0.1 mL of 1 % w/v carrageenan suspension in distilled water was injected in the sub-planter tissue of left hind paw of each animal using 27-gauge needle. A mark was made on the left hind foot just below the tibio-torsal junction so that every time the paw was dipped in the column of plethysmograph to same level to ensure constant paw volume. After 2 h administration of carrageenan suspension, the paw volumes were measured at regular time intervals up to 24 h using plethysmometer, and percent inhibition of edema was calculated. The results were compared by one-way ANOVA followed by Dunnett's t test and was considered as significant with respect to plain drug.
Skin irritation study
Skin irritation study of different formulations was conducted in male albino rats (160 ± 20 g) according to the reported method [28]. The animals were housed in an air-conditioned room (20 °C) and hair of the back was trimmed short, 24 h before the beginning of the assay. The animals were divided into four groups of five each. First group of rats received plain drug gel and served as control, while second, third, and fourth groups of rats received ICPLM gel, CMN-SLS, and CMN-DMSO, respectively. Three squares were drawn on each side of the back of each rat and 0.5 g of each formulation was applied on each square. Using nylon mesh, supported by the plastic squares having small pores kept above the treated area, protected the treated area of the animals. The formulation was removed after exposure for 32 h and exposed skin was scored for the formation of edema (graded 0–3) and erythema (graded 0–3).
Storage-physical stability of CMN formulation
Stability studies were performed for 3 months using CMN gel prepared of ICPLM and with PEs. Gel formulations were evaluated for drug retentive potential at three different temperature conditions, i.e., 4–8 °C (refrigerator), 25 ± 2 °C/60 % RH (RT), 40 ± 2 °C/75%RH (accelerated temperature) as per ICH Guideline Q1A (R2) [29]. Stability samples were analyzed for drug assay and ex vivo permeation through rat skin at each sampling point of 1, 2, and 3 months [30, 31].
Statistical analysis
Data are expressed as the mean ± standard deviation (SD), and statistical analysis was carried out by one-way ANOVA following Tukey–Kramer multiple comparison test. p > 0.05 was considered statistically insignificant, while p < 0.001 was considered very significant.
Results
Phase-solubility studies
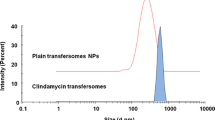
The phase-solubility diagram of CMN as a function of HP-β-CD concentration in an aqueous buffer solution (pH 5) at RT is shown in Fig. 2. The phase-solubility plot for CMN-HP-β-CD was found to be “Bs type” solubility curve [32].
Thermodynamic parameters
Stability constant was found to be 6.2 × 105, and other thermodynamic parameter were also determined; ΔG = −1.88 kJ/mole, ΔH = 3.766 kJ/mole, and ΔS = 0.0189.
Solubility measurement
Solubility of ICPPM, ICPLM, and ICPSEM was found to show 100.71-, 1051.76-, and 1026.47-folds increase, respectively, as compared to pure CMN.
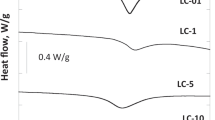
DSC studies
Inclusion complex formation was confirmed by DSC thermograms (Fig. 3). CMN exhibited a sharp endothermic melting peak (Tm) at 177.19 °C, whereas HP-β-CD shows peak at 135.43 °C. Thermogram of ICPPM shows the characteristic peak similar to that of CMN. Thermogram of ICPSEM shows the endotherm peak shift from 177.19 °C to 160.59 °C of the pure CMN. In contrast, thermogram of ICPLM showed complete disappearance of the characteristic endothermic peak of CMN.
X-ray powder diffraction analysis
The X-ray diffraction patterns of drug, polymer, and complexes are shown in Fig. 4. Characteristic high intensity diffraction peaks for CMN were detected at: 2θ = 12.227, 14.561, 17.338, 18.194, 23.429, 25.639, 25.660; for ICPPM 2θ = 10.744, 12.551, 12.740, 15.454, 17.176, 18.857, 20.835, 22.968, and for ICPSEM 2θ = 16.640, 17.418, 23.873, 29.250, 29.734, 30.784, 34.002. CMN has well-defined crystalline X-ray patterns, whereas HP-β-CD is amorphous. X-ray pattern of ICPPM appears to represent the superimposed peaks of parent compounds. The patterns of ICPSEM showed that the peaks ascribed to CMN are significantly diminished. In contrast, ICPLM showed remarkable disappearance of peaks with no measurable X-ray patterns.
X-ray diffractogram of parent compound and different complex (ICPPM = inclusion complex prepared by physical mixture; ICPLM = inclusion complex prepared by lyophilization method; ICPSEM = inclusion complex prepared by solvent evaporation method; CMN = curcumin; HP-β-CD = 2-hydroxy propyl-β-cyclodextrins)
FTIR spectra
FTIR spectra of pure CMN, HP-β-CD and their complex are presented in Fig. 5. FTIR spectrum of HP-β-CD showed prominent absorption bands at 3,622.35 cm−1 due to O–H stretching vibration; at 2,714.81 cm−1 due to the C–H stretching vibrations; at 1,495.198 cm−1 due to C=C ring stretch; at 1,101.93 and 1,042.48 cm−1 corresponding to asymmetrical C–O–C stretching vibrations and symmetric C–O–C stretch, respectively. The characteristic bands of pure CMN occurred at 3,731.51 cm−1 due to p-OH stretching vibration, non-hydrogen bonding; at 2,882.19 cm−1, they were assigned to the asymmetric methyl –O-CH3 stretching vibration. Other bands were observed at 1,561.54 and 1,265.75 cm−1 corresponding to strong asymmetric C=O band stretching vibration and asymmetric C–O–C stretching vibration, respectively. Shift of characteristic bands, disappearance or reduction in intensity, and appearance of new bands in the FTIR spectra might be associated to possible drug–CD interaction and/or amorphization of the product [33]. The spectral pattern of ICPPM corresponds to the sum of the band positions of the FTIR spectra of both CMN and HPβCD, whereas spectrum of ICPSEM showed asymmetric methyl stretch shifting to 2,837.1 cm−1 and the C=C stretching vibration of benzene ring shifted to 1,593.1 cm−1. In contrast, the spectrum of ICPLM demonstrated complete disappearance of the CMN characteristic bands that were seen in the spectrum of physical mixture. The most notable band disappearance occurred at 1,506.85 cm−1, C=C stretching vibration of benzene ring, 1,265.75 cm−1 absorption peak assigned to the asymmetric C–O–C stretching vibration, and 2,882.19 cm−1 absorption peak for asymmetric methyl stretch.
1H-NMR spectroscopy
Chemical shifts (parts per million) for the protons of CMN and HP-β-CD in its free state and in ICPLM are summarized in Table 2. Results are summarized with signals that are less or appreciably shifted either downfield for H3, H4, and H5 and upfield for H1 and H2.
SEM
Results of SEM analysis, performed to investigate the morphologies of pure drug and complexes prepared by various methods, were consistent with these findings, showing that the polyhedron-shaped drug crystals, still recognizable in both ICPPM and ICPSEM, were no longer detectable in ICPLM (Fig. 6).
In vitro permeation studies
Permeability profiles of Carbopol gel of plain CMN, ICPLM, CMN-SLS, and CMN-DMSO as PEs across rat skin are reported in Fig. 7. The plain gel of CMN, ICPLM, CMN-SLS, and CMN-DMSO showed cumulative percentage release of 13.22 %, 76.98 %, 34.22 %, and 72.34 %, respectively. The amount of drug permeated was in the order ICPLM > CMN-DMSO > CMN-SLS > CMN. Percentage cumulative amount of ICPLM permeated was found to be 5.8-fold greater than CMN alone after 10 h. The permeation measured by the amount of transferred drug was remarkably enhanced of ICPLM (p < 0.05) possibly due to complexation.
Flux of different formulations through hairless rat skin is shown in Fig. 8. There is a significant enhancement (p < 0.05) of flux between pure drug and ICPLM. The determined flux followed the order ICPLM > CMN-DMSO > CMN-SLS > CMN.
Skin irritancy studies
In regular transdermal studies, PEs for enhancing passive permeation of drug molecule are usually employed. However, regulatory authorities have also given importance to the irritation potential of PEs. The skin irritations scores defined by the Code of Federal Regulation, 1976 following application of different formulation at 32 h are shown in Fig. 9. In this histopathological evaluation, score of edema and erythema were considered as the key criteria to distinguish the effect of drug. No apparent change was observed in skin morphology after the application of control sample containing Carbopol gel without drug. However, when compared with the skin treated with gel containing CMN, CMN-SLS, and CMN-DMSO, mild to well-defined erythema exhibiting mean score of 0.4, 0.4, and 0.6, respectively, was observed. Gel of ICPLM caused relatively less irritation showing mean score of 0.2. Edema was almost absent in all cases.
Anti-inflammatory activity
Anti-inflammatory activity of different formulations was determined following the carrageenan-induced rat paw edema model and was found to be in the order of ICPLM > CMN-DMSO > CMN-SLS > marketed formulation > CMN, as signified by percent edema inhibition of 81 %, 51 %, 49 %, 46 %, and 10 % after 12 h, respectively, shown in Fig. 10.
Stability study
The formulations were subjected to accelerated stability testing, as per ICH guidelines for semi-solid preparations, at three different temperature conditions, i.e., 4–8 °C (refrigerator), 25 ± 2 °C/60 % RH (RT), 40 ± 2 °C/75 % RH (accelerated temperature) for a period of 3 months [30]. The ICPLM formulation was found to be stable with respect to CMN assay when analyzed by UV spectroscopy of different formulations (Fig. 11).
Further, in order to assess the integrity of PE system, ICPLM, SLS, and DMSO were employed; the transdermal permeation was studied through the rat skin. Flux for CMN permeation through ICPLM was not altered significantly in the 3-month long study at all the stability conditions, establishing the integrity of PE system. On the contrary, permeation data of other formulations were found to be greatly diminished over time due to degradation of CMN in the formulations (Fig. 12).
Discussion
The major aim of this investigation was the development of stable formulations with the application of HP-β-CD which imparts drug solubilization, stabilization, and improved transdermal permeation. In order to plan the synthesis of cyclodextrin complex, phase-solubility curve was determined and was found to be “Bs type”, which demonstrates the complex formation between one molecule of CMN and two molecules of HP-β-CD, i.e., in the ratio of 1:2. This can be further confirmed by the molecular dimension of CMN which is too large (ca. 19 Å long, 6 Å wide) to be entrapped entirely into one HP-β-CD cavity (ca. 7.8 Å wide), thus two molecules are required for the complexation phenomenon. Thermodynamic parameters were also determined with positive ΔH confirmed endothermic binding process, which further lead to increase in enthalpy of the system. ΔG value for the complex was determined to be negative assuring their stability. According to Vant's Hoff equation, the higher the complexation constant, the lower will be the Gibbs free energy of complexation. Further ΔS was found to be positive, confirming the complexation phenomenon. During complexation, when guest molecule enters the cavity of HP-β-CD, some water molecules get released which lead to higher entropy. Involvement of electrostatic or hydrophobic interactions in complex formation was verified by these thermodynamic parameters [32].
First off, we achieved formulation of complex and were validated by various mentioned evaluation parameters. Solubility data of ICPPM, ICPLM, and ICPSEM was compared with pure CMN. This proved that complexation with hydrophilic polymer leads to overwhelming increase in the solubility of insoluble or poorly aqueous soluble drug. DSC thermogram of ICPPM shows the characteristic peak similar to that of CMN, thus revealing that no complex formation occurred by physical mixture. Thermogram of ICPSEM shows the endotherm peak shift depicting partial complexation. In contrast, thermogram of ICPLM showed complete disappearance of the characteristic endothermic peak of CMN that clearly proved the formation of inclusion complex with reduced crystallinity due to the absence of endothermic peak of drug and that may be attributed to the amorphous state of inclusion complex. The X-ray pattern of ICPPM shows crystalline nature with superimposed peaks of parent compounds. The patterns of ICPSEM showed significantly diminished peaks ascribed to CMN, suggesting lower degree of crystalinity. In contrast, ICPLM showed remarkable disappearance of peaks, suggesting the amorphous characteristic. FTIR spectral pattern of ICPPM indicates no or minor interaction between CMN and HP-β-CD molecules in the physical mixture, whereas spectrum of ICPSEM showed partial interaction of peaks of parent compound, thus revealing partial complexation. FTIR spectral pattern of ICPLM demonstrated complete disappearance of the CMN characteristic bands. The most notable band disappearance of C=C stretching vibration of benzene ring, absorption peak assigned to the asymmetric C–O–C stretching vibration, and absorption peak for asymmetric methyl stretch implied masking of aromatic structures possibly by inclusion into CD cavities. Alkene part of CMN showed some changes in their absorption frequency assuring the delocalization of π electron of olefinic double bond and thus proved immersion of aromatic ring in the HP-β-CD cavity. From the data of phase-solubility studies, the complexation ratio of CMN: HP-β-CD is found to be 1:2 showing entrapment of aromatic ring in each side of CMN in the cavity of two HP-β-CD. Chemical shifts (parts per million) for the protons of ICPLM clearly demonstrated that signals are less or appreciably shifted (either downfield for H3, H4, and H5 or upfield for H1 and H2), assuring formation of the complex. In NMR study of pure drug, chemical shifts are prominent in case of –OH and –CH3 protons. This fashion of shifting of signals along with changes occurred for pure HP-β-CD protons reveal the mode of interaction of HP-β-CD with CMN. Possibly aromatic ring containing –OH and –CH3 is immersed in the cavity of HP-β-CD probably due to the remarkably shifted H3 and H5 protons located inside the cavity of HP-β-CD. SEM analysis clarify the morphologies of pure drug and complexes prepared by various methods and found amorphous aggregates of ICPLM showing complete complexation.
A subsequent aim of this study was to explore the influence of HP-β-CD and different permeation enhancers on skin permeation of CMN. Indeed, these compounds led to improved skin permeation rates of the drug. The best performance shown by ICPLM is attributable to the greater solubilizing power towards the practically insoluble drug, which allowed a greater amount of drug in solution, available for permeation. On the contrary, with other permeation enhancers, the faster drug release obtained from ICPLM is attributable to their complex formation, which further increases the drug permeation. This finding corroborated the importance of the different mode of drug interaction with different PEs in determining its penetration rate as well as the possibility of better modulating it by CD complexation. The permeation was measured by the amount of transferred drug was remarkably enhanced of ICPLM (p < 0.05) possibly due to complexation. There is a significant enhancement (p < 0.05) of flux between pure drug and ICPLM because of the improved penetration through rat skin possibly due to the presence of solubilized drug at the site.
The skin irritation scores showed decrease in irritation, assuring complexation of drug with HP-β-CD, which alleviates drug-induced local irritation and improves the safety of the drug. Anti-inflammatory activity of different formulations was determined by carrageenan-induced rat paw edema model and verified that complexation of CMN with HP-β-CD increases its biological activity. The accelerated stability testing demonstrated that complexation of CMN improves its stability and needs to be further explored for its biomedical applications.
Conclusion
The transdermal formulation of CD complex was shown to be efficacious, safe, stable and non-irritant to skin. CMN is widely used as potent anti-inflammatory drug. It is advantageous over NSAIDs, being devoid of any side effect such as GIT bleeding, hepatotoxicity, etc., yet suffers from its inherent drawbacks such as poor bioavailability and less permeability through skin. Therefore, it is envisaged to formulate cyclodextrin complex. HP-β-CD formed true inclusion complexes with CMN, indicating a stoichiometry of 1:2 (CMN:HP-β-CD). CDs have been studied as a possible vehicle for transdermal delivery of CMN, an anti-arthritic, anti-inflammatory agent. The study confirmed that CDs are very promising, safe, and biocompatible PEs for transdermal delivery of CMN as revealed from an enhanced transdermal flux. Finally, we conclude that CMN–CD complex gel provides better permeation as compared to plain drug gel. Since transdermal drug deliver entails higher permeability, CD complex formulation is a better option for transdermal drug delivery for the CMN.
References
Drakulic BJ, Juranic IO, Eric S, Zloh M. Role of complexes formation between drugs and penetration enhancers in transdermal delivery. Int J Pharm. 2008;363(1–2):40–9.
Loftsson T, Masson M. Cyclodextrins in topical drug formulations: theory and practice. Int J Pharm. 2001;225(1–2):15–30.
Lopez RFV, Collett JH, Bentley MVLB. Influence of cyclodextrin complexation on the in vitro permeation and skin metabolism of dexamethasone. Int J Pharm. 2000;200(1):127–32.
Uekama K, Adachi H, Irie T, Yano T, Saita M, Noda K. Improved transdermal delivery of prostaglandin E1 through hairless mouse skin: combined use of carboxy methyl-ethyl-beta- cyclodextin and penetration enhancers. J Pharm Pharmacol. 1992;44(2):119–21.
Yang W, Chow KT, Lang B, Wiederhold NP, Johnston KP, Williams 3rd RO. In vitro characterization and pharmacokinetics in mice following pulmonary delivery of itraconazole as cyclodextrin solubilized solution. Eur J Pharm Sci. 2010;39(5):336–47.
Felton LA, Wiley CJ, Godwin DA. Influence of hydroxylpropyl- beta- cyclodextrin on the transdermal permeation and skin accumulation of oxybenzone. Drug Dev Ind Pharm. 2002;28(9):1117–24.
Vitroria M, Bentley LB, Vianna RF, Wilson S, Collett JH. Characterization of the influence of some cyclodextrins on the stratum corneum from the hairless mouse. J Pharm Pharmacol. 1997;49(4):397–402.
Doliwa A, Santoyo S, Ygartua P. Influence of Piroxicam: hydroxypropyl-beta-cyclodextrin complexation on the in vitro permeation and skin retention of Piroxicam. Skin Pharmacol Appl Skin Physiol. 2001;14:97–107.
Dias MMR, Raghavan SL, Pellett MA, Hadgraft J. The effect of β-cyclodextrins on the permeation of diclofenac from supersaturated solutions. Int J Pharm. 2003;263(1–2):173–81.
Babu RJ, Pandit JK. Effect of cyclodextrins on the complexation and transdermal delivery of bupranolol through rat skin. Int J Pharm. 2004;271(1–2):155–65.
Maestrelli F, Gonzalez-Rodrıguez ML, Rabasco AM, Mura P. Effect of preparation technique on the properties of liposomes encapsulating ketoprofen–cyclodextrin complexes aimed for transdermal delivery. Int J Pharm. 2006;312(1–2):53–60.
Yang J, Wiley CJ, Godwin DA, Felton LA. Influence of hydroxypropyl-b-cyclodextrin on transdermal penetration and photostability of avobenzone. Eur J Pharm Biopharm. 2008;69(2):605–12.
Rajewski RA, Stella VJ. Pharmaceutical applications of cyclodextrins. 2. In vivo drug delivery. J Pharm Sci. 1996;85(11):1142–69.
Klang V, Matsko N, Zimmermann AM, Vojnikovic E, Valenta C. Enhancement of stability and skin permeation by sucrose stearate and cyclodextrins in progesterone nanoemulsions. Int J Pharm. 2010;393(1–2):152–60.
Ungaro F, Giovino C, Catanzano O, Miro A, Mele A, Quaglia F, La Rotonda MI. Use of cyclodextrins as solubilizing agents for simvastatin: effect of hydroxypropyl-β-cyclodextrin on lactone/hydroxyacid aqueous equilibrium. Int J Pharm. 2011;404(1–2):49–56.
Arora RB, Basu N, Kapoor V, Jain AP. Anti-inflammatory studies on Curcuma longa (turmeric). Ind J Med Res. 1971;59(8):1289–95.
Sharma OP. Antioxidant activity of curcumin and related compounds. Biochem Pharmacol. 1976;25(15):1811–2.
Deodhar SD, Sethi R, Srimal RC. Preliminary study on anti-rheumatic activity of curcumin (diferuloyl methane). Ind J Med Res. 1980;71:632–4.
Cho YI, Choi HK. Enhancement of percutaneous absorption of ketoprofen: effect of vehicles and adhesive matrix. Int J Pharm. 1998;169:95–104.
Higuchi T, Connors KA. Phase Solubility techniques. Adv Anal Chem Instrum. 1965;4:117–210.
Jayaprakasha GK, Jagan Mohan RL, Sakariah KK. Improved HPLC method for the determination of curcumin, demethoxy curcumin and bisdemethoxy curcumin. J Agric Food Chem. 2002;50(13):3668–72.
Benesi HA, Hildebrand JH. A spectrophotometric investigation of the interaction of Iodine with aromatic hydrocarbons. J Am Chem Soc. 1949;71(8):2703–7.
Zhang GY, Wang HY, Tang B. Study on the supramolecular interaction of curcumin and beta-cyclodextrin by spectrophotometry and its analytical application. J Agric Food Chem. 2002;50(6):1355–61.
Tenjarla S, Puranajoti P, Kosina R, Mandal T. Preparation, characterization and evaluation of Miconazole–cyclodextrin complexes for improved oral and topical delivery. J Pharm Sci. 1998;87(4):425–9.
Indian Pharmacopoeia: Controller of Publication, Ministry of Health and Family Welfare, Govt. of India, New Delhi 1996
Gondaliya DP, Pundarikakshudu K. Studies in formulation, characterization of transdermal permeation of nimesulide from aqueous and emulgel. Indian Drugs. 2002;39:465–73.
Dubey V, Mishra D, Dutta T, Nahar M, Saraf DK, Jain NK. Dermal and transdermal delivery of an anti-psoriatic agent via ethanolic liposomes. J Contr Rel. 2007;123(2):148–54.
Draize JH, Woodward G, Calvery HO. Methods for the study of irritation and toxicity of substances applied topically to the skin and mucous membranes. J Pharmacol Exp Ther. 1944;82:377–90.
ICH Harmonised Tripartite Guideline, stability testing of new drug substances and products Q1A (R2), 2003.
Tiwari SB, Udupa N, Rao BSS, Puma D. Thermosensiitive liposomes and localized hyperthermia—an effective bimodality approach for tumour management. Int J Pharm. 2000;32:214–20.
Krishna G, Hodrick WF, Lang W, Lin X, Karra S, Mao J, Almassian B. Pharmaceutical development and manufacturing of a parenteral formulation of a novel antitumor agent, VNP40101M. AAPS Pharm Sci Tech. 2001;2(3):E14.
Lachman L, Lieberman HA, Kanig JL, editors. The theory and practice of industrial pharmacy. 3rd ed. Bombay: Varghese Publishing House; 1991. p. 171.
Al-Marzouqi AH, Elwy HM, Shehadi I, Adem A. Physicochemical properties of antifungal drug–cyclodextrin complexes prepared by supercritical carbon dioxide and by conventional techniques. J Pharm Biomed Anal. 2009;49(2):227–33.
Acknowledgements
The authors (Raksha Ghanghria and Prashant Kesharwani) are thankful to IUC-DAE (Indore, India) and SAIF, Lucknow for extending their facilities to carry out characterization studies. The financial support of University Grant Commission and Indian Council of Medical Research (ICMR), New Delhi, India, is gratefully acknowledged.
Disclosures
There is no conflict of interest and disclosures associated with the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghanghoria, R., Kesharwani, P., Agashe, H.B. et al. Transdermal delivery of cyclodextrin-solubilized curcumin. Drug Deliv. and Transl. Res. 3, 272–285 (2013). https://doi.org/10.1007/s13346-012-0114-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-012-0114-y