Abstract
Background and Objective
Cenobamate is an antiepileptic drug for the treatment of partial-onset seizures. The current study was designed to assess the mass balance and the metabolic profiling of cenobamate in humans.
Methods
Absorption, metabolism, and excretion of cenobamate were investigated in healthy male subjects after a single oral dose of 400 mg of cenobamate containing 50 µCi of [14C]-cenobamate as capsule formulation.
Results
Cenobamate was rapidly (median time to maximum plasma concentration of 1.25 h) and extensively (≥ 88% of dose) absorbed. The mean cenobamate plasma concentration–time profile revealed a multiphasic elimination profile whereas the mean plasma/blood concentration–time curve for total radioactivity did not appear to be multiphasic, suggesting that elimination mechanisms for cenobamate and its metabolites may be different. Blood/plasma ratios observed for the area under the concentration–time curve (AUC) and peak concentration (both ~ 0.60) suggest a limited penetration of cenobamate and metabolites into red blood cells (RBCs). Eight cenobamate metabolites were identified across plasma, urine, and feces. Cenobamate was the main plasma radioactive component and M1 was the only metabolite detected in plasma (> 98% and < 2% total radioactivity AUC, respectively). All detected metabolites were found in urine, with M1 as the major radioactive component (mean cumulative recovery 37.7% of dose); unchanged cenobamate accounted for 6%. Metabolites comprised ~ 88% of the dose recovered in urine, indicating extensive metabolism by the kidneys and/or metabolites formed in the liver were rapidly eliminated from the bloodstream. However, cenobamate metabolites appear to be formed slowly. Minor amounts of cenobamate (0.48%) and five metabolites (≤ 1.75% each; M1, M3, M6, M7, M11) were recovered in feces.
Conclusion
This study indicates that cenobamate is primarily eliminated in urine as metabolites. Cenobamate is the major circulating component in plasma after oral administration and has a limited penetration into RBCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Following oral administration, cenobamate, an antiepileptic drug for the treatment of uncontrolled focal (partial-onset) seizures in adults, is extensively absorbed and is the major circulating component in plasma. |
Cenobamate is primarily eliminated in urine as metabolites with little excretion of the parent drug. |
The present study demonstrates the absence of major circulating metabolites in humans and highlights the need to investigate the effects of hepatic and renal impairment on the disposition of cenobamate. |
1 Introduction
Antiepileptic drugs are often administered in combination and their metabolic profiles frequently lead to drug–drug interactions [1,2,3]. Identification of the metabolic pathway for each new antiepileptic drug is a critical step in their development. Human mass balance studies are usually used to elucidate metabolic pathways of new chemical entities and these data provide key information for preclinical and clinical drug development.
Cenobamate (YKP3089) is a new Food and Drug Administration-approved antiepileptic drug for the treatment of adults with focal (partial-onset) seizures [4]. The precise mechanism by which cenobamate exerts its therapeutic effects in patients with focal seizures is unknown; however, cenobamate reduces repetitive neuronal firing by inhibiting voltage-gated sodium channels, and is also a positive allosteric modulator of the ƴ-aminobutyric acid (GABAA) ion channel [5, 6].
Metabolic stability of cenobamate was studied in rat, dog, monkey, and human liver microsomes. Metabolism was found to be slow in liver microsomes from all species with dog as the fastest (estimated terminal half life [t1/2] was 82 min vs > 100 min for all other species) [data on file]. In vivo, cenobamate has been shown to be extensively metabolized in all animal species. In vitro metabolism studies have shown that cenobamate is primary metabolized by glucuronidation (via UGT2B7 and to a lesser extent by UGT2B4) and by oxidation (via CYP2E1, CYP2A6, CYP2B6, and to a lesser extent by CYP2C19 and CYP3A4/5) [4].
A limited number of transporters have been tested in vitro with cenobamate (P-gp, BCRP, OAT1, OAT3, OCT2, MATE1, and MATE2-K). Cenobamate was not a substrate for these transporters. In addition, cenobamate did not inhibit P-gp, OAT1, OCT1, OCT2, OATP1B3, or BSEP [data on file].
The first phase 1 studies conducted in healthy subjects showed that the pharmacokinetics of cenobamate is complex following oral dosing. After single-dose administration, cenobamate plasma concentrations increase rapidly and reach maximum concentrations between 0.8 and 3.5 h post-dose, plateau for 6–12 h, and then decrease slowly, with a t½ increasing from 30 to 76 h over the 5–750 mg dose range [7]. Increases in cenobamate peak concentration (Cmax) have been shown to be dose proportional, whereas total plasma exposure (area under the concentration–time curve; AUC) increases in a greater than dose-proportional manner over the 5–750 mg dose range. This non-proportionality for AUC has not been observed for multiple dosing between 50 and 500 mg/day. Multiple-dose studies have shown that steady-state plasma concentrations are attained after approximately 2 weeks of once-daily dosing, and an accumulation ratio of approximately 5 has been observed over the 50–300 mg/day dose range. In these studies, cenobamate was generally safe and well tolerated after single doses up to 750 mg and multiple doses from 50 to 500 mg administered once daily [7].
In parallel to the clinical development program, the current human mass balance study was conducted to investigate the absorption, metabolism, and elimination of cenobamate and to identify the major human metabolites as well as any unique human metabolites for toxicological and clinical purposes. In addition, this study will provide the appropriate information to evaluate the need to conduct clinical studies in special populations, e.g., in patients with renal or hepatic impairment.
The aim of this study was to evaluate the metabolic disposition, mass balance, excretion, and pharmacokinetics of cenobamate after a single oral dose of 400 mg containing 50 µCi of [14C]-labeled cenobamate in healthy subjects. The cenobamate dose of 400 mg was selected based on previous clinical studies as safe and within the possible therapeutic range.
2 Subjects and Methods
2.1 Study Design and Population
A phase 1, open-label, single-dose, single-center mass balance study was conducted in healthy male subjects aged 19–55 years. Subjects were screened ≤ 21 days prior to enrollment and were admitted, remaining in-house at the clinic from study day − 1 until completion of all scheduled post-dose procedures on day 14. A single oral dose of 4 capsules containing 12.5 µCi of radiolabeled cenobamate (14C) and 100 mg of cenobamate each (total of 50 µCi 14C/400 mg cenobamate) was administered to each subject on day 1. Labeled cenobamate capsules ([14C]-YKP3089; lot number 65015MAR08-01) were manufactured by ABC Laboratories (Columbia, MO, USA). The allowable [14C] cenobamate radiation levels administered were based on the dosimetry calculations.
All subjects had routine bowel movements (≥ 1 every other day), had not used tobacco- or nicotine-containing products for ≥ 6 months prior to dosing, and had no history of alcoholism or drug abuse for ≥ 2 years prior to study start. Subjects were excluded if they had a history or presence of significant cardiovascular, pulmonary, hepatic, renal, hematologic, gastrointestinal, endocrine, immunologic, dermatologic, neurologic, or psychiatric disease. Subjects who had a history of allergic or serious adverse reactions to benzodiazepines or other anxiolytics, positive urine drug/alcohol testing at screening or check-in, or use of any prescription or over-the-counter medication ≤ 14 days prior to day 1 (except ≤ 2 g acetaminophen/day at the discretion of the investigator) were excluded.
The subjects were not allowed to consume xanthine/caffeine throughout the study, alcohol from 48 h before the start of the study until the end of the study, and grapefruit from 10 days prior to the start of the study until the end of the study. Pertinent study documents were reviewed and approved by the independent MDS Pharma Services Institutional Review Board prior to study initiation, and all subjects reviewed and signed the informed consent form during screening. The study was conducted in compliance with the International Conference on Harmonisation’s Tripartite Guidelines for Good Clinical Practice and the principles enunciated in the Declaration of Helsinki.
2.2 Study Objectives and Assessments
The primary objective of this study was to assess the mass balance of cenobamate following a single oral dose of [14C]-labeled cenobamate. The secondary objectives included determination of pharmacokinetic parameters from total radioactivity in plasma and blood samples, and cenobamate concentrations in plasma samples, to explore the possibility of cenobamate partitioning into red blood cells (RBCs), and to identify cenobamate metabolites in plasma, urine, and feces. Subjects were confined for 312 h after dosing at the clinical unit.
2.2.1 Pharmacokinetic Assessments and Metabolic Profiling
Blood samples were collected prior to dosing (≤ 15 min pre-dose) and at 0.5, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 8, 12, 16, 24, 48, 72, 96, 120, 144, 168, 192, 216, 240, 264, 288, and 312 h post-dose. At each time point, a total of approximately 20 mL of blood was collected (2 × 10 mL sodium heparin tubes). Whole blood (3 mL) was retained to analyze total radioactivity through scintillation counting, and the remainder was centrifuged at approximately 2500 rpm at 4 °C for 15 min for plasma extraction.
Plasma was then aliquoted for scintillation counting (2.5 mL), determination of cenobamate concentration (1.0 mL), and metabolic profiling (3.0 mL), with the remainder stored as back-up samples. The concentrations of cenobamate in human plasma (heparin) were determined using a validated achiral method (study no. ZZ01036-01) with high-performance liquid chromatography (HPLC) and mass spectrometric detection (analytical range 0.080–40.0 μg/mL). Cenobamate stability in plasma was established for 27 h at an ambient temperature and for 281 days at − 20 °C (note: as the assay measured a non-labeled drug, the presented cenobamate concentrations may be approximately 3.6% lower than the actual).
Urine was collected for scintillation counting and metabolic profiling at approximately 1–2 h pre-dose and post-dose at 0–6, 6–12, 12–24 h, and at subsequent 24-h intervals up to 312 h. The urine was refrigerated, and the total volume collected for each time interval was recorded. At the end of each collection interval, the urine was mixed and a 10-mL aliquot (for scintillation counting) and 20-mL aliquot (for metabolic profiling) were transferred to separate storage containers. Urine samples with radioactivity > 500 dpm/g were prepared and used for extraction recovery.
All stools produced from 24 h prior to check-in until dosing were collected and the sample produced nearest to dosing was used as the pre-dose sample. Post-dose stools were collected for scintillation counting and metabolic profiling at 24-h intervals throughout the study. All samples were stored at − 70 °C with an aliquot of approximately 5 g used for metabolic profiling. Homogenate fecal samples with > 800 dpm/g were used for extraction recovery and sample preparation for analysis.
Liquid scintillation counting methods were validated for accuracy and reproducibility of sample processing and [14C] measurement by liquid scintillation counting in four biological matrices—plasma, whole blood, urine, and feces. Samples were processed in duplicate for plasma, whole blood, urine, and feces. Fecal and whole blood samples were oxidized using a Packard Model 307 Oxidizer prior to counting. Quality control samples with two levels of known amounts of radioactivity were prepared in each matrix by spiking with stock solutions of [14C]-labeled glucose. All samples were counted in vials with liquid scintillation cocktail for 5 min and limits of quantification for whole blood, plasma, urine, and feces were 45, 32, 33, and 38 dpm/aliquot (i.e., 0.336 µg-eq/g, 0.239 µg-eq/mL, 0.123 µg-eq/mL, 0.284 µg-eq/g, respectively). The dpm were converted to microgram equivalents (µg-eq) per either milliliter for plasma and urine or per gram for whole blood and feces using the known specific activity. For urine and feces, the data were also converted to the percentage of dose for each time interval. A general assumption that 1 g of whole blood was equal to 1 mL of whole blood was used. Mass balance was calculated as a sum of the percent of total radioactivity recovered in urine and feces.
Metabolite identification was conducted by HPLC/tandem mass spectrometry coupled with a radio flow-through detector, and HPLC fraction collection and counting with TopCount was used for radio quantification of plasma, urine, and fecal samples (QPS, LLC, Newark, DE, USA).
From plasma and whole blood concentration data, pharmacokinetic parameters were calculated using WinNonlin Professional software and included maximum plasma concentration (Cmax), time at maximum plasma concentration (tmax), terminal half-life (t1/2), area under the concentration–time curve from time 0 to the last measurable timepoint (AUC0–t), and AUC from time 0 to infinity (AUC0–∞). AUC0–t was estimated using linear trapezoidal summation from time zero to time t, where t is the time of the last measurable concentration, and AUC0–∞ was calculated as AUC0–t + Ct/kel, where Ct is the time of the last measurable concentration and kel is the terminal rate constant. The ratio of total radioactivity AUC and Cmax in whole blood divided by respective plasma values (AUCblood/AUCplasma and Cmax blood/Cmax plasma) was calculated with the assumption that 1 g of whole blood = 1 mL of whole blood.
All pharmacokinetic data were summarized using descriptive statistics as mean, standard deviation (SD), coefficient of variation, standard error of the mean, median, minimum, and maximum.
2.2.2 Safety Assessments
Safety was assessed via adverse events (AEs) throughout, and vital signs, physical examinations, electrocardiograms (ECGs), and laboratory parameters at various time points. Blood pressure and pulse were monitored pre-dose, at dosing, and at 1, 8, 12, 24, 48, and 312 h post-dose. Physical examinations were performed pre-dose and at the end of the study, ECGs were conducted pre-dose and at 1, 4, 8, 12, 24, and 48 h post-dose, as well as at the end of the study. Laboratory data were collected pre-dose and at the end of the study.
3 Results
3.1 Subject Disposition and Demographics
A total of 6 subjects were enrolled and all completed the study. All subjects were male and Caucasian (Table 1), with an overall mean age of approximately 23 years (range 20–27 years).
3.2 Pharmacokinetic Parameters
Throughout the study, the mean total radioactivity concentration equivalents in plasma were greater than those observed in whole blood (Fig. 1a), with mean Cmax values of 11.6 µg/mL and 7.0 µg/mL in plasma and whole blood, respectively. Additionally, the mean cenobamate radioactivity concentration equivalents in plasma were similar to those of total radioactivity in plasma until both reached peak concentration (Fig. 1b). After peak concentrations were reached (1.25–1.50 h), cenobamate plasma concentrations declined more rapidly than those of total radioactivity for the remainder of the study.
Mean cenobamate plasma concentration (μg/mL) and mean total radioactivity concentration in plasma (μg-equivalents/mL) and whole blood (μg-equivalents/g) over time (312 h). a Linear representation and b semi-logarithmic representation. Subjects received a single oral dose of 4 [14C]-cenobamate capsules, each containing 100 mg cenobamate with 12.5 μCi [14C]-cenobamate. (Note: At 312 h, N = 5 for whole blood total radioactivity concentration and N = 4 for cenobamate plasma concentration due to values below the limit of quantitation for the other subjects)
The ratios of AUC0-t over AUC0–∞ for whole blood and plasma were 91.0% (CV = 2.74%) and 90.9% (CV = 2.60%), respectively, indicating that total radioactivity was well characterized. Exposure to total radioactivity was 65.6% (Cmax) and 66.6% (AUC) greater in plasma than in whole blood (Table 2).
The blood/plasma ratios for both AUC0–∞ and Cmax were ~ 0.600 and remained consistent over time (Fig. 2), suggesting a limited penetration of cenobamate and its metabolites into RBCs. Mean erythrocyte transfer ratios and erythrocyte/plasma partition coefficients were lower than 0.100 and 0.150, respectively, throughout the study, confirming that radiolabeled cenobamate and its metabolites did not significantly penetrate into RBCs.
3.3 Mass Balance
Approximately 93% of the total administered radioactivity was recovered in urine and feces combined over the course of the study (range 78.4%–99.0%; Fig. 3), with > 50% of the radioactivity excreted within approximately 72 h post-dose. Urinary excretion was the primary route of elimination, with approximately 88% of the administered radioactive dose recovered in urine and 5.20% of the dose recovered in feces.
3.4 Metabolite Profiling
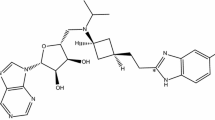
Cenobamate and metabolite M1 were detected in the plasma radiochromatograms while analysis of the urine radiochromatograms revealed cenobamate, eight identifiable metabolites, denoted as M1, M2a, M2b, M3, M5, M6, M7, M11, and two trace unidentifiable metabolites, P2 and P5 (Table 3). A total of six radioactive components were observed in fecal samples (cenobamate, M1, M3, M6, M7, and M11). The M1 and M11 metabolites were identified as two N-glucuronides of cenobamate with glucuronidation at different positions. Through radiochromatograms, two non-overlapping peaks were visualized indicating that M1 and M11 are distinct metabolites (Supplemental Fig. 1). M1 was detected in plasma, urine, and feces while M11 was only detected in fecal extracts. M2a and M2b were two glucuronides formed from cenobamate hydroxylation products, M3 was an ether glucuronide formed from the hydrolysis product of cenobamate, M6 and M7 were two cenobamate dihydrodiol metabolites, and M5 was identified as a glucuronide of either M6 or M7. Trace metabolites P2 and P5 were very minor radioactive components detected in urine and no reasonable molecular ions for these were identified.
Cenobamate was the major radioactive component in plasma, with > 98% of the total radioactivity AUC; the only other metabolite detected in plasma was M1, which accounted for < 2% of total radioactivity AUC (Table 4). The mean Cmax of cenobamate was 11.5 μg/mL, while that of the M1 metabolite was 0.290 μg/mL.
M1 was the major radioactive component found in urine, with a mean cumulative recovery of 37.7% (range 27.8–49.8%), followed by M2b and M7 (mean cumulative recovery 17.5% and 7.88%, respectively) (Supplemental Tables). The mean cumulative recovery of cenobamate in urine was 6.36% and was < 7% each for all other metabolites detected. Total cumulative recovery in feces was between 1.72% and 6.98%, with M1 as the major radioactive component (mean cumulative recovery 1.75%). Very little cenobamate was recovered in feces (mean cumulative recovery 0.480%).
Analysis of plasma with a chiral HPLC column confirmed that there was no chiral inversion for cenobamate (R-enantiomer) in this study after a single oral dose. This lack of chiral inversion was confirmed at steady state using a validated assay to measure both R- and S-forms of cenobamate in a separate study (data on file). Based on the metabolites identified in this study, the proposed biotransformation pathway for cenobamate is shown in Fig. 4.
3.5 Safety
No AEs or deaths occurred in any subjects throughout the study. One clinically significant laboratory result in creatinine kinase occurred in one subject. At hour − 14.5 (day − 1, check-in), a higher than normal value of 621 U/L creatinine kinase was recorded (reference range 43–350 U/L), which remained out of range at recheck (448 U/L) and returned to normal by the end of the study (165 U/L). No individual out-of-range clinically significant hematology or urinalysis values were observed throughout the study. Additionally, all post-dose mean vital signs were within normal limits, and changes from baseline in systolic blood pressure, diastolic blood pressure, and pulse were minor. Overall, cenobamate was safe and well tolerated throughout this study in healthy male subjects.
4 Discussion
The present study was conducted to evaluate the mass balance of radiolabeled cenobamate administration in six healthy male subjects. A single 400 mg oral dose of cenobamate with 50 µCi of [14C]-cenobamate was administered to each subject. Cenobamate was rapidly absorbed with comparable tmax values of 1.25 to 1.50 h in plasma and whole blood, respectively. The maximum mean plasma cenobamate concentration (Cmax) and plasma exposure (AUC) were comparable to those observed in a previous pharmacokinetic study following oral administration of a single 400 mg dose of cenobamate in healthy subjects [7].
The plasma concentration–time profile of cenobamate (Fig. 1a, b) revealed an apparent multiphase elimination of cenobamate up to 288 h post-dose with the first phase occurring prior to 24 h post-dose, the second phase occurring between 24 and 144 h post-dose, and the third phase occurring after 144 h post-dose. This non-linearity in the elimination phase was observed in 5 of the 6 subjects (Supplemental Fig. 2) and may be attributable to a possible saturation in the elimination processes of cenobamate up to approximately 144 h (at which point the elimination processes are no longer saturated, and the apparent rate of systemic elimination is increased). The concentration–time profiles for unchanged cenobamate and total radioactivity were nearly superimposable up to about 24 h, indicating that the parent drug is the predominant quantifiable moiety present in the plasma up to that time point. The divergence between total radioactivity and parent drug concentration–time profiles indicated a slow appearance of the metabolite(s) in the systemic circulation. Interestingly, the multiphasic nature of the unchanged cenobamate concentration–time profile was not clearly apparent for the total radioactivity concentration–time profile, suggesting distinct elimination mechanisms for the parent drug and its metabolites. Possible explanations for these findings include a slow formation of the metabolites and a limited tissue distribution. In addition, the involvement of concentration- or time-dependent inhibition of hepatic efflux transporters (i.e., OATPs, MRPs, and BCRP) and/or concentration- or time-dependent saturation of kidney influx transporters (i.e., OATs, OCTs, and URAT1) on the disposition of cenobamate can also lead to a slow elimination of this compound.
The concentration–time profile for total radioactivity in blood and plasma showed low penetration of cenobamate and its metabolite(s) into the RBCs as indicated by the radioactivity exposure in plasma being 65% greater than whole blood, with a blood to plasma ratio for both AUC0–∞ and Cmax of 0.60.
Despite approximately 80% of the dose being recovered as metabolites in the urine, only trace amounts of metabolites were seen in the plasma as illustrated in Table 4. These results suggest that cenobamate may either be metabolized by the kidneys and/or its metabolites are formed in the liver and rapidly eliminated from the bloodstream. Kidney-mediated metabolism has been previously identified as a significant metabolizing system for some xenobiotics [8]. Further studies are required to elucidate the exact mechanism of elimination for cenobamate.
This study demonstrates the absence of major circulating metabolites (> 10% of total radioactivity in plasma) after oral administration of cenobamate. Because cenobamate is extensively metabolized and excretion of these metabolites is primarily through the kidneys, further study of the effects of renal and hepatic impairment on the disposition of cenobamate is necessary.
5 Conclusion
In summary, the current data demonstrated that oral radiolabeled cenobamate was absorbed quickly and almost completely. Cenobamate was extensively metabolized through glucuronidation, hydrolysis, and hydroxylation and seemed to follow multiple phases of elimination. The major route of elimination of cenobamate and its metabolites was through urine. The parent drug was the primary circulating moiety in plasma and the formation of its metabolites was apparently slow. The blood/plasma ratio suggests a limited penetration of cenobamate and its metabolites into RBCs. The elimination pathways for cenobamate and its metabolite(s) appear to be uniquely different.
References
Patsalos PN, Perucca E. Clinically important drug interactions in epilepsy: interactions between antiepileptic drugs and other drugs. Lancet Neurol. 2003;2:473–81.
Perucca E. Clinically relevant drug interactions with antiepileptic drugs. Br J Clin Pharmacol. 2006;61:246–55.
Johannessen Landmark C, Patsalos PN. Drug interactions involving the new second- and third-generation antiepileptic drugs. Expert Rev Neurother. 2010;10:119–40.
XCOPRI® (cenobamate tablets), for oral use [prescribing information]. Paramus, NJ: SK Life Science, Inc.; 2019.
Nakamura M, Cho JH, Shin HS, Jang IS. Effects of cenobamate (YKP3089), a newly developed anti-epileptic drug, on voltage-gated sodium channels in rat hippocampal CA3 neurons. Eur J Pharmacol. 2019;855:175–82.
Sharma R, Song WS, Nakamura M, et al. Effects of cenobamate on GABA-A receptor modulation [abstract]. American Epilepsy Society Annual Meeting, November 30–December 4, 2018, New Orleans, LA; Abstract 3.306.
Vernillet L, Greene SA, Kamin M. Pharmacokinetics of cenobamate: results from single and multiple oral ascending dose studies in healthy subjects. Clin Pharmacol Drug Dev. 2020. https://doi.org/10.1002/cpdd.769.
Knights KM, Rowland A, Miners JO. Renal drug metabolism in humans: the potential for drug-endobiotic interactions involving cytochrome P450 (CYP) and UDP-glucuronosyltransferase (UGT). Br J Clin Pharmacol. 2013;76:587–602.
Acknowledgements
The authors would like to thank Staci J. McDonald, PharmD, Robert A. Earl, PhD, Ian Malloch Davis, MS, Elliot Offman, BSc Pharm, MSc, S. James Lee, PhD, Martin Brecher, MD, Palanichamy Ilankumaran, PhD and Zhaoping Yan, for study contribution. Additionally, the authors thank the staff and volunteers who participated in this study. The authors also thank Debika Chatterjea, PhD, MedVal Scientific Information Services, LLC for providing medical writing support, which was funded by SK Life Science, Inc. This manuscript was prepared according to the International Society for Medical Publication Professionals’ “Good Publication Practice for Communicating Company-Sponsored Medical Research: The GPP3 Guidelines.”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by SK Life Science, Inc.
Conflict of Interest
LV, employee of SK Life Science, Inc.; SAG, employee of SK Life Science, Inc.; HWK, employee of SK Life Science, Inc.; SMM, employee of SK Life Science, Inc.; KG, employee of SK Life Science, Inc.
Data Availability Statement
The authors confirm that the data supporting the main findings of this study are available within the article [and/or] its supplementary materials. Any additional data, noted as ‘data on file’ within the text, are available from the corresponding author [LV] upon reasonable request.
Ethical Approval
This research was conducted in accordance with the clinical research guidelines established by the Medical Research Council of Canada, the Basic Principles defined in U.S. 21 CFR Part 312.20, the requirements of Directive 2001/20/EC (Europe), the principles enunciated in the Declaration of Helsinki and the ICH-harmonised tripartite guideline regarding Good Clinical Practice (GCP). The study was approved by the independent MDS Pharma Services Institutional Review Board.
Informed Consent
Informed consent was given by all subjects who participated in the study.
Previous Presentation
This data was previously presented at the 12th International Society for the Study of Xenobiotics Meeting, July 28–July 31, 2019.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vernillet, L., Greene, S.A., Kim, H.W. et al. Mass Balance, Metabolism, and Excretion of Cenobamate, a New Antiepileptic Drug, After a Single Oral Administration in Healthy Male Subjects. Eur J Drug Metab Pharmacokinet 45, 513–522 (2020). https://doi.org/10.1007/s13318-020-00615-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-020-00615-7