Abstract
Alemtuzumab is a humanized monoclonal antibody that is administered daily for 5 days, and then no further therapy is required for 12 months. It causes rapid and prolonged lymphocyte depletion; the consequent homeostatic reconstitution leads to a radically reformed lymphocyte pool with a relative increase in regulatory T cells and expansion of autoreactive T cells. Although previously licensed for the treatment of B-cell chronic lymphocytic leukemia, it is now been considered for licensing in the treatment of multiple sclerosis (MS). From a disappointing experience with alemtuzumab in progressive MS, Alastair Compston and I argued that immunotherapies should be given early in the course of the disease. In a unique program of drug development in MS, alemtuzumab has been compared in 1 phase 2 trial and 2 phase 3 trials with the active comparator interferon beta-1a. In all trials, alemtuzumab was more effective in suppressing relapses than interferon beta-1a. In one phase 2 and one phase 3 trial, alemtuzumab also reduced the risk of accumulating disability compared with interferon beta-1a. Indeed, alemtuzumab treatment led to an improvement in disability and a reduction in cerebral atrophy. The safety issues are infusion-associated reactions largely controlled by methylprednisolone, antihistamines, and antipyretics; mild-to-moderate infections (with 3 opportunistic infections from the open-label experience: 1 case each of spirochaetal gingivitis, pyogenic granuloma, and Listeria meningitis); and autoimmunity. Usually autoimmunity is directed against the thyroid gland, but causes (1 %) immune thrombocytopenia, and in a few cases antiglomerular basement membrane syndrome. Alemtuzumab is an effective therapy for early relapsing-remitting MS, offering disability improvement at least to 5 years after treatment. Its use requires careful monitoring so that potentially serious side effects can be treated early and effectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alemtuzumab was originally known as Campath-1H because it was the first monoclonal antibody to be made in the University of Cambridge Pathology Department and it was humanized. This was made possible by the Cambridge inventions for producing and humanizing monoclonal antibodies [1, 2]. Although alemtuzumab was originally intended for the treatment of leukemias [3], it was soon tested for autoimmune disease [4–9], and was first used in multiple sclerosis (MS) in 1991.
Alemtuzumab’s Mechanism of Action
Alemtuzumab is given as an intravenous infusion of 12 mg/day for 5 consecutive days in the first cycle and 3 consecutive days in the second cycle. Subsequent cycles are not given electively, but are given in response to a return of disease activity.
Alemtuzumab binds to CD52, a 12-amino acid cell surface protein of unknown function [10–12] that is expressed at high levels on T cells and B cells and at lower levels on monocytes, macrophages, and eosinophils with little found on Natural Killer cells, neutrophils, and hematological stem cells. Cells of the innate immune system are unaffected. Although monocytes carry the CD52 antigen, they are depleted for only a few days. Within minutes of infusing a single dose of alemtuzumab in humans, peripheral lymphocytes are depleted, probably by antibody-dependent, cell-mediated cytotoxicity [13]. Cross-linking of Natural Killer cells causes a rise in serum cytokines, including tumor necrosis factor-α, interleukin-6, and interferon-γ [14], which results in infusion-associated symptoms that are successfully reduced or prevented by pre-treatment with corticosteroids and an antihistamine [15].
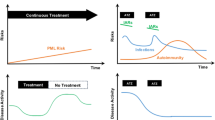
The therapeutic effect of alemtuzumab is mediated by the remolding of the immune repertoire that accompanies homeostatic lymphocyte reconstitution. Recovery of B- and T-lymphocytes to the lower limit of normal after a single course of alemtuzumab takes 8 months and 3 years, respectively [16]. For the first 6 months after treatment, there is a predominance of memory T-cell number cells, especially those with a regulatory phenotype (CD4+ CD25hi FoxP3+), with reduced constitutive cytokine expression [17]. During this time, the B-cell compartment is largely naïve and memory B cells are slow to return [18].
Alemtuzumab Treatment of Progressive MS
The first group of patients to be treated with alemtuzumab in 1991-93, were 36 patients with the progressive disease for a duration of 11 years, a mean Expanded Disability Status Scale (EDSS) score of 6.5 and an average of 0.7 relapses per year, whose disability had worsened by ≥ 1 EDSS point in the preceding year [19]. After alemtuzumab, the mean relapse rate fell to 0.02 per annum, representing a 97 % reduction and new magnetic resonance imaging lesion formation was also demonstrated to be reduced by 90 %. However, the disability of the group of patients continued to deteriorate, just as their cerebral atrophy progressed. At the latest follow-up, a median of 14-years post-treatment, the median disability of the cohort had worsened to an EDSS of 7.5 (range, 4.5-9) [16].
Alemtuzumab Treatment of Relapsing-Remitting MS Disease
Open-Label Trials
The second group of patients to be treated with alemtuzumab had relapsing-remitting MS, with a mean relapse rate of 2.2, which fell after alemtuzumab to 0.14 (equaling a 94 % reduction). This time, unlike the progressive cohort previously discussed, mean disability scores fell after alemtuzumab (by a mean of 1.2 points at 2 years).
This experience led us to conclude that disability accumulation early in MS is driven by inflammation and that anti-inflammatory treatments are effective if given early in the course of the disease [20]. From this analysis, our suggestion emerged that there is a “window of therapeutic opportunity” for immunotherapies in MS [21].
Controlled Trials of Alemtuzumab
A phase 2 trial was published, and the headline results from 2 phase 3 trials have been presented but not yet published (Alasdair Coles at European Committee for the Treatment of MS 2011 for the Comparison of Alemtuzumab and Rebif Efficacy in Multiple Sclerosis trials (CRE-MS) I and of Jeff Cohen at the American Association of Neurology in 2012 for CARE-MS II). All trials have been rater-blinded; the first dose effect of alemtuzumab precludes double-blinding.
After the hypothesis of the “window of therapeutic opportunity,” patients recruited to these trials were selected on the basis of a limited disease duration (restricted to < 3 years in phase 2, 5 in CARE-MS I, and 10 in CARE-MS II); low disability (Expanded Disability Status Score <3 in phase 2 and CARE MSI, and <5 in CAREMSII), but high disease activity (at least 2 relapses in the preceding 2 years) (Table 1). In each trial, alemtuzumab was compared with the active drug interferon beta-1a. In phase 2 and CARE-MS I, alemtuzumab was tested as a first-line therapy. In CARE-MS II, participants had already experienced at least 1 relapse on disease-modifying therapy.
These trials (summarized in Table 2) show that alemtuzumab reduces the relapse rate more effectively than interferon beta-1a. In the phase 2 trial and CARE-MS II, alemtuzumab also reduced the number of patients who acquired sustained accumulation of disability during the trial; indeed, mean disability of alemtuzumab-treated patients actually improved. In CARE-MS I, fewer alemtuzumab-treated patients accumulated disability than those on interferon beta-1a, but this difference was not statistically significant. This trial was inadvertently underpowered because only 11 % of interferon beta-1a patients met the disability endpoint, rather than the expected 20 %. An extension of the phase 2 trial showed sustained superiority of alemtuzumab in comparison with interferon beta-1a for a 5-year duration [22].
Safety
Infusion-Associated Symptoms
An infusion reaction is common at the time of alemtuzumab treatment, with a rash, headache, influenza-like symptoms and less frequently transient recurrence of previous MS symptoms (Table 3). Pre-treatment with corticosteroids, an antihistamine, and paracetemol minimizes these symptoms.
Infections
In all trials, mild-to-moderate infections, especially of the respiratory and urinary tracts, were more frequent among patients receiving alemtuzumab than those receiving interferon beta-1a (Table 3). Serious infections were rare (e.g., occurring in 4 % of patients after alemtuzumab in the CARE MS II trial compared with 1.5 % using interferon beta-1a). Three patients in an open-label experience had opportunistic infections from which they fully recovered (1 case each of spirochaetal gingivitis, pyogenic granuloma, and Listeria meningitis).
Malignancy
Cancers have not been statistically more frequent after alemtuzumab than interferon beta-1a in any of the trials (Table 3), but these studies were not powered to pick up differences in low-frequency events. In the phase 3 trials, there were 3 cases of thyroid papillary carcinoma. These were all detected as a result of thyroid ultrasound scanning of patients with biochemical thyroid dysfunction in which context papillary carcinomas are recognized as “incidental” [23]. In the extension of the phase 2 trial, 1 patient died from non-EBV associated Burkitt’s lymphoma, and another patient who received alemtuzumab developed Castleman’s disease, a pre-lymphomatous condition, and is now in remission after R-CHOP (rituximab, cyclophosphamide, doxyrubicin, prednisolone) [24].
Autoimmunity
The principal adverse effect of alemtuzumab is novel autoimmunity arising months to years after treatment (Table 3). The thyroid gland is the most common target, being affected in 20 to 30 % of patients, most frequently with the development of Grave’s disease. The first person to manifest immune thrombocytopenia died of a brain hemorrhage. Then a careful risk management program was put in place with education for patients and monthly blood counts. This has led to the identification and treatment of all subsequent cases before any significant bleeding events could occur. Most patients have required corticosteroids, and a number of patients had intravenous immunoglobulin, along with some who had rituximab. All of these patients are now well, most are off the treatment and have normal platelet counts.
Other autoimmune diseases have occurred at lower frequency after alemtuzumab. There have been 3 cases of Goodpasture’s disease detected among several thousand people who received alemtuzumab for MS, both in trials (1) and off-label (2); in 2 of the cases, renal transplantation was required, and the remaining cases had stable renal function off treatment. These have been reported several times in the literature [21, 25]. There have also been single cases of autoimmune neutropenia and autoimmune hemolytic anemia.
Autoimmunity is a recognized phenomenon of reconstitution from lymphopenia in a variety of different conditions [26, 27]. We have shown that pre-treatment serum interleukin-21 may serve as a biomarker for the risk of developing autoimmunity for months to years [28].
Immunogenicity
Despite being humanized, alemtuzumab induces anti-alemtuzumab binding and neutralizing antibodies in as much as 30 to 70 % of patients 1 month after the first and second cycles, respectively. However, because the interval between treatment cycles is at least 1 year, such antibodies usually become undetectable before the next cycle [24]. If persistent, neutralizing antibodies become problematic in patients who have received multiple alemtuzumab cycles. We have shown that pre-treatment with an altered version of alemtuzumab, which no longer binds to its target, can effectively induce tolerance to alemtuzumab itself [24].
Discussion
Alemtuzumab is an exploratory treatment for relapsing-remitting MS and is being considered for licensing in the United States and Europe in 2013. A unique development program has tested alemtuzumab with an active comparator in people with early disease in 1 phase 2 and 2 phase 3 trials. In each trial, alemtuzumab offers clinical efficacy superiority in comparison with interferon beta-1a. However, it has potentially serious adverse effects, particularly autoimmune diseases for months or years after alemtuzumab. These require careful monitoring and a high degree of vigilance from patient and physician alike to institute timely therapy. The details of monitoring are currently being reviewed by regulatory authorities, but these are likely to include monthly platelet monitoring and 3 monthly thyroid function monitoring for some years after alemtuzumab treatment.
Several issues involving alemtuzumab treatment of MS remains to be investigated. As an effective treatment with significant adverse effects, opinions vary as to whether alemtuzumab should be considered a “second-line” therapy or if it should be used as a first-line therapy instead. Although, undoubtedly, alemtuzumab has more safety concerns than current first-line therapies, some patients and physicians may feel that this it is a reasonable cost for the superior efficacy of alemtuzumab in this context. After the first 2 annual cycles, it is unclear how subsequent cycles of therapy should be planned. Options include a fixed schedule of re-treatment, re-treatment only with no disease activity or re-treatment with drugs, such as interferon beta in an “induction” program. The long-term safety profile of alemtuzumab, particularly for low frequency events, needs to be established.
References
Riechmann L, et al. Reshaping human antibodies for therapy. Nature 1988;332:323-327.
Kohler G, Milstein C. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 1975;256:495-497.
Waldmann H, Hale G. CAMPATH: from concept to clinic. Phil Trans Roy Soc Lond B Biol Sci 2005;360:1707-1711.
Lockwood CM, et al. Remission induction in Behcet's disease following lymphocyte depletion by the anti-CD52 antibody CAMPATH 1-H. Rheumatology (Oxford) 2003;42:1539-1544.
Dick AD, et al. Campath-1H therapy in refractory ocular inflammatory disease. Br J Ophthalmol 2000;84:107-109.
Isaacs JD, et al. Monoclonal antibody therapy of chronic intraocular inflammation using Campath-1H. Br J Ophthalmol 1995;79:1054-1055.
Isaacs JD, et al. Monoclonal antibody therapy of diffuse cutaneous scleroderma with CAMPATH-1H. J Rheumatol 1996;23:1103-1106.
Isaacs JD, et al. CAMPATH-1H in rheumatoid arthritis — an intravenous dose-ranging study. Br J Rheumatol 1996;35:231-240.
Newman DK, et al. Prevention of immune-mediated corneal graft destruction with the anti-lymphocyte monoclonal antibody. CAMPATH-1H. Eye (Lond) 1995;9(pt 5):564-569.
Hale G. The CD52 antigen and development of the CAMPATH antibodies. Cytotherapy 2001;3:137-143.
Xia MQ, et al. Structure of the CAMPATH-1 antigen, a glycosylphosphatidylinositol-anchored glycoprotein which is an exceptionally good target for complement lysis. Biochem J 1993;293(pt 3):633-640.
Xia MQ, et al. Characterization of the CAMPATH-1 (CDw52) antigen: biochemical analysis and cDNA cloning reveal an unusually small peptide backbone. Eur J Immunol 1991;21:1677-1684.
Hu Y, et al. Investigation of the mechanism of action of alemtuzumab in a human CD52 transgenic mouse model. Immunology 2009;260-270.
Wing MG, et al. Mechanism of first-dose cytokine-release syndrome by CAMPATH 1-H: involvement of CD16 (FcgammaRIII) and CD11a/CD18 (LFA-1) on NK cells. J Clin Invest 1996;98:2819-2826.
Moreau T, et al. Transient increase in symptoms associated with cytokine release in patients with multiple sclerosis. Brain 1996;119(pt 1):225-237.
Hill-Cawthorne GA, et al. Long term lymphocyte reconstitution after alemtuzumab treatment of multiple sclerosis. J Neurol Neurosurg Psychiatry 2012;83:298-304.
Cox AL, et al. Lymphocyte homeostasis following therapeutic lymphocyte depletion in multiple sclerosis. Eur J Immunol 2005;35:3332-3342.
Thompson SA, et al. B-cell reconstitution and BAFF after alemtuzumab (Campath-1H) Treatment of Multiple Sclerosis. J Clin Immunol 2009;99-105.
Kurtzke JF. Rating neurologic impairment in multiple-sclerosis — an Expanded Disability Status Scale (EDSS). Neurology 1983;33:1444-1452.
Coles AJ, et al. Monoclonal antibody treatment exposes three mechanisms underlying the clinical course of multiple sclerosis. Ann Neurol 1999;46:296-304.
Coles AJ, et al. The window of therapeutic opportunity in multiple sclerosis: evidence from monoclonal antibody therapy. J Neurol 2006;253:98-108.
Coles AJ, et al. Alemtuzumab more effective than interferon beta-1a at 5-year follow-up of CAMMS223 Clinical Trial. Neurology 2012;1069-78.
Berker D, et al. Prevalence of incidental thyroid cancer and its ultrasonographic features in subcentimeter thyroid nodules of patients with hyperthyroidism. Endocrine 2011;39:13-20.
Somerfield J, et al. A novel strategy to reduce the immunogenicity of biological therapies. J Immunol 2010;185:763-768.
Clatworthy MR, Wallin EF, Jayne DR. Anti-glomerular basement membrane disease after alemtuzumab. N Engl J Med 2008;359:768-769.
Hsiao LT, et al. Relapse of Graves' disease after successful allogeneic bone marrow transplantation. Bone Marrow Transplant 2001;28:1151-1153.
Gilquin J, et al. Delayed occurrence of Graves' disease after immune restoration with HAART. Lancet 1998;352:1907-1908.
Jones JL, et al. IL-21 drives secondary autoimmunity in patients with multiple sclerosis, following therapeutic lymphocyte depletion with alemtuzumab (Campath-1H). J Clin Invest 2009;119:2052-2061.
Acknowledgments
Alasdair Coles has received honoraria and consulting fees, and his department has received research grants from Ilex Oncology and Genzyme, which are both involved in the commercial development of alemtuzumab. Coles and colleagues have submitted a patent for the prediction of autoimmunity after alemtuzumab. The clinical trials reported here have been funded by Ilex Oncology and Genzyme (a Sanofi company). The scientific work done in Cambridge has been supported by the Medical Research Council, the Wellcome Trust, the Moulton Foundation, the Grand Charity of The Freemasons and the Multiple Sclerosis Society of the UK. Alasdair Coles is supported by the Cambridge Biomedical Research Centre of the National Institute of Health Research. The clinical work was done in the Wellcome Clinical Research Facility. Full conflict of interest disclosures is available in the electronic supplementary material for this article.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 510 kb)
Rights and permissions
About this article
Cite this article
Coles, A.J. Alemtuzumab Therapy for Multiple Sclerosis. Neurotherapeutics 10, 29–33 (2013). https://doi.org/10.1007/s13311-012-0159-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-012-0159-0