Abstract
As the world population is aging rapidly, emergency abdominal surgery for acute abdomen in the elderly represents a global issue, both in developed and developing countries. Data regarding all the elderly patients who underwent emergency abdominal surgery from January 2017 to December 2017 at 36 Italian surgical departments were analyzed with the aim to appraise the contemporary reality regarding the use of emergency laparoscopy for acute abdomen in the elderly. 1993 patients were enrolled. 1369 (68.7%) patients were operated with an open technique; whereas, 624 (31.3%) underwent a laparoscopic operation. The postoperative morbidity rate was 32.6%, with a statically significant difference between the open and the laparoscopic groups (36.2% versus 22.1%, p < 0.001). The reported mortality rate was 8.8%, with a statistically significant difference between the open and the laparoscopic groups (11.2% versus 2.2%, p < 0.001). Our results demonstrated that patients in the ASA II (58.1%), ASA III (68.7%) and ASA IV (88.5%) groups were operated with the traditional open technique in most of the cases. Only a small percentage of patients underwent laparoscopy for perforated gastro-duodenal ulcer repair (18.9%), adhesiolyses with/without small bowel resection (12.2%), and large bowel resection (10.7%). Conversion to open technique was associated with a higher mortality rate (11.1% versus 2.2%, p < 0.001) and overall morbidity (38.9% versus 22.1%, p = 0.001) compared with patients who did not undergo conversion. High creatinine (p < 0.001) and glycaemia (p = 0.006) levels, low hemoglobin levels (p < 0.001), oral anticoagulation therapy (p = 0.001), acute respiratory failure (p < 0.001), presence of malignancy (p = 0.001), SIRS (p < 0.001) and open surgical approach (p < 0.001) were associated with an increased risk of postoperative morbidity. Regardless of technical progress, elderly patients undergoing emergency surgery are at very high risk for in-hospital complications. A detailed analysis of complications and mortality in the present study showed that almost 9% of elderly patients died after surgery for acute abdomen, and over 32% developed complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the world population is aging rapidly, emergency abdominal surgery for acute abdomen in the elderly represents a global issue, both in developed and developing countries.
The number of people worldwide over 65 years of age is estimated to rise from 5234 million in 2010 to over 1.5 billion in 2050, and actually approximately 33% of hospital stays and 41% of hospital costs are attributed to patients older than 65 years [1].
More than 20% of the Italian population is over the age of 65 and, by the year 2050, this percentage is expected to grow to 34%. Over the last 20 years, country’s life expectancy has increased from 78 to 80 years for men and from 84 to 85 years for women. About 20% of the senior citizens and 6% of the country’s total population are currently over the age of 80 [2].
It is estimated that 21% of the total population older than 60 years will require surgery, compared with only 12% of people in the 45–60 age group. Demographic changes in the population have also modified the profile of emergency abdominal surgery, where typical causes of acute abdomen in the elderly include acute cholecystitis, incarcerated hernia, bowel obstruction and appendicitis [3,4,5].
In the elderly population, recovery from surgery is considered more often complicated and burdened by longer hospital stay compared with the younger population. People over the age of 70 who undergo an emergency laparotomy have an inpatient mortality of 21.4%, and older patients, in particular octogenarians, have poorer outcomes with up to 44% mortality reported [6, 7].
Patients undergoing major abdominal surgery in the elective setting should be adequately assessed preoperatively to identify modifiable risk factors that can be addressed before surgery. In the emergency setting as well, overall risk should still be assessed to optimize physiology, even if the opportunity to do so is limited.
Despite the urgent need for knowledge in the surgical treatment of acute abdomen in the elderly, only few population-based studies have been published to date, reporting an overall morbidity rate of 26%, and mortality of 22% following urgent laparotomy in patients > 65 years of age [8,9,10].
The primary aim of this multicenter prospective cohort study conducted in Italy was to analyze the clinical–pathological data, the management strategies, and the short-term outcomes of emergency surgery for acute abdomen in the elderly, with particular regard to the use of laparoscopy.
Methods
The Frailty and Emergency Surgery in the Elderly (FRAILESEL) study has been designed and developed by the ERASO (Elderly Risk Assessment And Surgical Outcome) Collaborative Study Group, on behalf of the Italian Association of Hospital Surgeons (ACOI), the Italian Society of Surgery (SIC), the Italian Society of Emergency Surgery and Trauma (SICUT), the Italian Society of Geriatric Surgery (SICG), the Italian Society of Endoscopic Surgery and new technologies (SICE), and the Italian Chapter of the World Society of Emergency Surgery (WSES).
The FRAILESEL is a large, nationwide, multicenter, prospective, cohort, study that investigated the perioperative outcomes of patients aged ≥ 65 years who underwent emergency abdominal surgery between January 2017 and December 2017 (main study data collection period) at the study hospitals. One hundred and forty hospitals registered in the database of the Italian Ministry of Health in Italy that provide emergency general surgery were invited to participate and 36 surgical units accepted to take part in the study. Centers were included on a volunteer basis, and neither investigators nor participating hospitals were paid for their collaboration.
Data regarding elderly patients discharged from the participating centers who underwent any type of emergency abdominal surgical intervention were prospectively collected. Vascular, gynecological, and urological procedures were considered eligible for the study if performed by general or emergency surgeons in a general or trauma surgery setting.
Emergency procedures were defined as unforeseen, non-elective operations according to the NCEPOD Classification of Interventions [11].
The investigators were informed of the objectives of the study and asked to complete details about the surgical management of acute abdomen in the elderly following standard methods and collection protocols, as we described in the study protocol [12]. Clinical decisions, including operative technique (open or laparoscopic), were based on the criteria of individual centers and surgeons. Surgical procedures were sorted in accordance with the 9th revision of the International Classification of Disease Clinical Modification (ICD-9-CM).
The final FRAILESEL Study protocol was approved by the Ethics Committee of La Sapienza University of Rome and by the boards of all the societies involved. All the parts of the study and the present manuscript have been checked and presented according to the checklist for Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [13].
Postoperative complications were reported and categorized according to the Clavien–Dindo classification system by the study leader in each of the participating centers [14], and morbidity and mortality within 30 days from the date of surgery were evaluated regardless of the time elapsed from the surgical procedure if reasonably related to it.
Exclusion criteria
Exclusion criteria were the following: patients younger than 65 years old at the day of surgery; diagnostic laparoscopy/laparotomy with no further surgical procedures performed; lack of informed consent for the study participation; endoscopic procedures and emergency reoperations after elective surgery; patients already hospitalized and scheduled for the same procedure; patients participating in another trial.
Patients characteristics, preoperative variables and objectives of the study
Demographic data and pre-existing comorbidity and conditions were registered. Comorbidity was recorded if the condition was being medically treated at the time of admission, or if previous treatment for the condition was described in the admission report.
Collected patient variables included: age, BMI, heart rate, systolic blood pressure, WBC count, creatinine, glycaemia, and hemoglobin values, oral anticoagulation therapy, and comorbidity (diagnosis of acute myocardial infarction < 6 months, heart failure, peripheral vascular disease, chronic respiratory disease, malignancy). Furthermore, the American Society of Anesthesiologists (ASA) class as well as data on the presence of systemic inflammatory response syndrome (SIRS), operative records, type of surgical procedure, and intra-operative diagnosis were collected.
The primary aim of this study was to critically appraise the contemporary Italian reality regarding the surgical approach to acute abdomen in the elderly, through the analysis of a large cohort of patients aged ≥ 65 years. Within this context, the main outcomes were the occurrence of major complications and death from any cause within 30 days after the operation, stratified by the type of surgery (appendectomy, cholecystectomy, gastro-duodenal ulcer repair, small bowel resection/adhesiolysis, large bowel resection, abdominal wall reconstruction) and the age group (65–74 years old; 75–84 years old; > 84 years old). We critically reviewed the clinical–pathological data, the management strategies, and the conversion rate from laparoscopic to open surgery of elderly patients submitted to emergency abdominal surgery.
Statistical analysis
Statistical analysis was performed with SPSS software, version 22 (IBM, New York, NY, USA) for MacOSX. Data normality was tested using the Shapiro–Wilk or Kolmogorov–Smirnov tests. Dichotomous data and counts were presented in frequencies; whereas, continuous data were presented as mean values ± standard deviations. Differences between means were compared using the independent sample Student’s t test, the pairwise comparison Student’s t test, the Mann–Whitney U test, the Kruskal–Wallis test or other analysis of variance (ANOVA) tests when indicated.
Fisher’s exact test or χ2 test, with or without Yates correction, was implemented to compare differences in frequencies.
Thirteen independent clinical variables were analyzed. Variables associated with complications (conversion to open surgery, morbidity and mortality) following surgical interventions with P < 0.20 were selected for inclusion in the multivariate logistic regression analyses.
The Hosmer–Lemeshow test was performed to assess the value of the logistic regression model in predicting the risk of conversion. Two further multivariate logistic regression analyses were performed to assess perioperative risk factors for morbidity and mortality in the entire elderly cohort of patients submitted to emergency surgery. A p value ≤ 0.05 was considered statistically significant.
Results
Clinical characteristics of patients enrolled in the FRAILESEL Study
During the study period, a total of 1993 patients satisfying the inclusion criteria were identified (Fig. 1). The clinical characteristics of the patients enrolled in the study are summarized in Table 1.
1369 (68.7%) patients underwent open surgery (open group); whereas 624 (31.3%) underwent laparoscopic surgery (laparoscopic group). A conversion rate of 14.4% was reported (converted group). The mean age of patients in the open group and laparoscopic group was 78.6 ± 7.9 years and 76.0 ± 7.3 years, respectively (p < 0.001).
The analysis of preoperative variables showed that patients in the laparoscopic group had significantly higher BMI (27.2 ± 6.3 versus 26.2 ± 6.5, p < 0.010) compared with patients in the open group.
The analysis of the ASA class showed that the vast majority of the enrolled patients were classified as ASA III (54.3%), followed by ASA II (24.8%) and ASA IV (12.9%).
The vast majority of patients in the ASA II (58.1%), ASA III (68.7%) and ASA IV (88.5%) groups were operated with the traditional open technique.
The univariate analysis of preoperative variables demonstrated that patients in the converted group had similar mean age, BMI, heart rate, creatinine level, blood sugar level, hemoglobin level, rates of acute myocardial infarction across the 6 months prior to surgery and other cardiovascular diseases in comparison with the open group and the laparoscopic group. Instead, lower systolic blood pressure mean values (129.4 ± 34.6 versus 138.1 ± 22.4, p = 0.040), and higher WBC count (12.9 ± 5.3 versus 11.5 ± 5.7, p = 0.040) were found in the converted group compared with the laparoscopic group (Table 2).
Analysis of the surgical procedures
Large bowel resection was the most frequently performed emergency surgical operation (n = 524), followed by cholecystectomy (n = 452), hernia repair with or without small bowel resection (n = 328), adhesiolysis with or without small bowel resection (n = 327), appendectomy (n = 108), and surgery involving the stomach and/or the duodenum for perforated gastro-duodenal ulcer repair (n = 106).
Laparoscopy was implemented for cholecystectomy (71.0% of cases), appendectomy (51.8% of cases), perforated gastro-duodenal ulcer repair (18.9% of cases), adhesiolyses with/without small bowel resection (12.2% of cases), large bowel resection (10.7% of cases), hernia repair (5.8% of cases), and other vascular, gynecological and urological surgical procedures (14.9% of cases).
The conversion rate was 7.5% for appendectomy and 8.2% for cholecystectomy. Although limited by the small sample size, conversion rate was low for patients who underwent surgical interventions for perforated gastro-duodenal ulcer repair stomach and duodenum (4.7%), adhesiolysis with or without small bowel resection (6.1%), large bowel resection (3.2%), and other vascular, urological and gynecological emergency procedures (2.0%) (Table 3).
Analysis of morbidity and mortality
The overall morbidity rate following surgery was 32.6%, with a statically significant difference between the open group and the laparoscopic group (36.2% versus 22.1%, p < 0.001). Patients in the converted group showed similar rates of complications compared with patients in the open group (38.9% versus 36.2%, p = 0.651), but higher rates of complications compared with patients in the laparoscopic group (38.9% versus 22.1%, p = 0.001).
The reported mortality rates for patients who underwent any type of surgical intervention were 8.8%, with a statistically significant difference between the open group and the laparoscopic group (11.2% versus 2.2%, p < 0.001). No statically significant difference in terms of mortality was found comparing patients in the converted group with patients in the open group (11.1% versus 11.2%, p = 1.000). Conversely, a higher mortality rate was found in the converted group compared with the laparoscopic group (11.1% versus 2.2%, p < 0.001) (Table 4).
Patients in the laparoscopic group showed lower rates of grade I (7.1% versus 11.5%, p < 0.001), grade II (9.2% versus 15.0%, p < 0.001), and grade IVa Clavien–Dindo complications (1.1% versus 2.4%, p = 0.029) compared with patients in the open group.
Grade IIIa (4.4% versus 0.9%, p = 0.028) and IVb (1.2% versus 0.4%, p = 0.023) complications were higher in the converted group compared with the laparoscopic group.
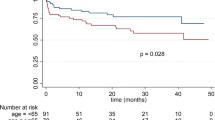
The overall procedure-related 30-day mortality and morbidity rates, stratified by the type of procedure and patients’ age are shown in Table 5. The overall 30-day mortality rate was 8.8% (by procedure: 1.9% appendectomy, 1.8% cholecystectomy, 20.8% perforated gastro-duodenal ulcer repair, 10.7% small bowel resection/adhesiolysis, 13.5% large bowel resection, 3.4% abdominal wall reconstruction, 18.2% other), whereas the overall 30-day morbidity rate was 32.6% (by procedure: 23.1% appendectomy, 24.8% cholecystectomy, 42.5% perforated gastro-duodenal ulcer repair, 36.9% small bowel resection/adhesiolysis, 41.0% large bowel resection, 26.5% abdominal wall reconstruction, 36.5% other). Subgroup analyses, conducted through the stratification of the cohort by age groups showed a general trend towards increased mortality and morbidity rates with increasing age.
Multivariate analyses
The logistic regression analysis showed that decreased values of systolic blood pressure (OR 0.987, 95% CI 0.978–0.995, p = 0.002), increased WBC count (OR 1.040, 95% CI 1.001–1.080, p = 0.043), and presence of respiratory failure (OR 1.578, 95% CI 1.127–2.211, p = 0.039) were the three independent factors associated with the risk of conversion from laparoscopic to open procedures (Table 6).
To estimate the risk factors behind postoperative morbidity and mortality, two separate multivariate analyses were performed after bivariate correlation analysis. All the statistically significant variables were inserted into the regression analysis model.
The results of the multivariate analysis showed that patients with increased postoperative morbidity had higher creatinine (OR 1.348, 95% CI 1.200–1.514, p < 0.001) and glycaemia (OR 1.002, 95% CI 1.001–1.004, p = 0.006) levels, as well as low hemoglobin levels (OR 0.904, 95% CI 0.871–0.939, p < 0.001) compared with patients who did not experience any complications. They were also more frequently under oral anticoagulation therapy (OR 1.462, 95% CI 1.167–1.832, p = 0.001), presented with higher rates of respiratory failure (OR 1.312, 95% CI 1.146–1.503, p < 0.001), and SIRS (OR 1.728, 95% CI 1.344–2.222, p < 0.001), had an established diagnosis of malignancy (OR 1.601, 95% CI 1.206–2.126, p = 0.001), and underwent an open surgical operation (p < 0.001) (Table 7).
Patients with increased postoperative mortality rates had higher creatinine (OR 1.496, 95% CI 1.318–1.697, p < 0.001) and glycaemia (OR 1.003, 95% CI 1.001–1.006, p = 0.003) levels, low hemoglobin levels (OR 0.890, 95% CI, p < 0.001), and a previous history of acute myocardial infarction (OR 2.359, 95% CI 1.171–4.752, p = 0.016) and heart failure (OR 1.959, 95% CI 1.389–2.763, p < 0.001) were independently associated with an increased risk of postoperative mortality (Table 8).
Discussion
Life expectancy in economically developed countries has sensibly increased due to improvements in hygienic conditions, better dietary regimens and medical advancements [15].
Italy has one of the oldest aging population, with a mean age of 80.6 years for men and 84.9 years for women [16]. According to the Italian National Institute for Statistics (ISTAT), for every 100 persons younger than 15 years of age, there are 81 who are older than 60 years [2].
While elective surgical procedures in the elderly provide satisfactory results compared with the younger population, this does not seem true for emergency general surgery, where significantly higher morbidity and mortality rates are reported [4, 17, 18]. Emergency laparotomy is considered a high-risk procedure, with significant mortality rates ranging from 14 to 20%. In the presence of comorbidity and perioperative conditions like sepsis, mortality the rate increases to over 50% in elderly patients [19, 20].
The use of the laparoscopic approach in the emergency setting is well established and has some advantages to the open approach by reducing the postoperative pain, length of hospital stay and complication rates [21,22,23,24].
According to some authors, laparoscopy carries particular risk via carbon dioxide insufflation in elderly patients with reduced cardiopulmonary reserve, causing diaphragmatic splinting, reducing venous return and cardiac output, and predisposing the patient to myocardial infarction and basal atelectasis.
In the present study, laparoscopy for acute abdomen was performed in only 31.3% of the cases, similar to other national series [22, 25,26,27].
Laparoscopy for acute abdomen in Italy gained an increasing diffusion during the last 10 years, as shown by the increased rate of abdominal emergencies approached by laparoscopy reported by Agresta et al. In particular, significant changes have been recorded in the penetration of laparoscopic surgery for acute diverticulitis; whereas, other conditions such as small bowel obstruction and perforated peptic ulcer are still approached by laparotomy in about 70% of cases [22].
More than 70% of patients with acute cholecystitis underwent laparoscopic cholecystectomy in the present study. In young and otherwise healthy patients, early cholecystectomy represents the standard of care for acute cholecystitis, as it is related to lower complication rate, shorter hospital stay and lower costs compared with delayed cholecystectomy. A recent systematic review and meta-analysis comparing early and delayed cholecystectomy for acute cholecystitis in the elderly population demonstrated that early cholecystectomy seems to be a feasible treatment, being the procedure associated with a conversion rate of 23%, perioperative morbidity of 24%, and mortality of 3.5% [28]. However, these rates are higher than those reported for non-elderly patients undergoing emergency cholecystectomy, being approximately 15% and < 1%, respectively [29].
Another meta-analysis by Antoniou et al. comparing open and laparoscopic cholecystectomy in elderly patients showed that odds ratios for mortality (1.0% vs 4.4%), morbidity (11.5% vs 21.3%), cardiac (0.6% vs 1.2%) and respiratory complications (2.8% vs 5.0%) were constantly in favor of laparoscopic surgery [30].
Emergency laparoscopic colorectal resection, where technically feasible, has demonstrated to improve the postoperative outcomes in comparison to open surgery, especially in terms of median length of hospital stay and overall complication rate [31].
Likewise, a recent meta-analysis by Cirocchi et al. exploring the role of emergency laparoscopic colectomy for complicated sigmoid diverticulitis showed that laparoscopy improves the rates of overall postoperative complications (RR 0.62, 95% CI 0.49–0.80) and postoperative hospital stay (MD − 6.53, 95% CI − 16.05 to 2.99). Conversely, laparoscopy did not seem to improve the other clinical outcomes, such as the rate of primary anastomosis, operating time, reoperation rate and postoperative 30-day mortality [32]. Results coming from the large prospective, observational study by Santacruz et al. showed that laparoscopic colon cancer resections decrease wound infection rate, postoperative complications, and length of hospital stay, especially in ASA III–IV patients [27].
Moreover, recent randomized controlled trials, such as the COST, COLOR and CLASSIC have demonstrated the efficacy and safety of minimally invasive colectomy in patients with colorectal cancer [33,34,35]. Unfortunately, all these trials have underrepresented the elderly and failed to account for frailty.
We found that emergency colorectal resections were performed laparoscopically in almost 11% of cases in our study. In the same way, contemporary data show that in developed countries, less than 17% of emergency colorectal resections for any cause and less than 5% for cancer are performed by laparoscopy [31, 36].
Previous studies have highlighted the role of laparoscopy also in surgical management of small bowel obstruction, since laparoscopic adhesiolysis has become a widely adopted technique with a substantial reduction in the overall complication rate compared with open surgery [37, 38]. However, as also demonstrated in our study, when a resection is necessary, the literature shows that a minority of cases are done entirely laparoscopically. If an indication for resection is found during an explorative laparoscopy for small bowel obstruction, the majority of resections are done after conversion to laparotomy [39, 40]. This attitude has been confirmed by the large analysis of over 4000 patients undergoing small bowel resection associated with obstruction from adhesive disease, where only 2.9% were approached laparoscopically [38].
It appears that laparoscopy is still relatively uncommon also for perforated gastro-duodenal ulcer, which is one of the most common surgical emergencies worldwide occurring in approximately 2–10% of patients hospitalized for peptic ulcer disease [41].
Different studies have demonstrated that there has been a shift in the overall population of emergency repair for perforated peptic ulcer to a more elderly cohort [42, 43]. Factors related to comorbidity, shock on admission, delayed surgery and postoperative infections have been associated with increased mortality and morbidity rates of up to 40% and 50%, respectively, for perforated peptic ulcer in the elderly [44].
Less than 20% of patients with perforated gastro-duodenal ulcer were treated with laparoscopy in our study. Putting these results in the context of emergency abdominal surgery in the elderly, Testini et al. reported that patients over 65 years have significantly higher mortality rate after surgery for perforated peptic ulcer [45].
Recent statistics show that acute appendicitis currently accounts for 15% of all emergency room visits for acute abdominal pain in patients over 60 years of age, and appendectomy is actually the third most common reason for abdominal surgery in geriatric patients [46]. The risk of death from acute appendicitis in older patients is up to 14 times that of this disease in the general adult population.
In 2013, Moazzez et al. reported that 75% of operations performed on patients aged > 65 years with acute appendicitis were laparoscopic in the USA, a significantly higher percentage compared with that reported by Guller et al. in 2003 [47, 48].
This confirmed that laparoscopic appendectomy is becoming the gold standard approach even in older age group patients owing to the well-demonstrated benefits of laparoscopy, especially as regards the decreased rates of postoperative complications.
Elderly patients are uniquely vulnerable to poor outcomes after emergency surgical procedures.
Regardless of clinical and technical progress, mortality and morbidity among elderly patients requiring emergency abdominal surgery are still high. In our study, the overall morbidity rate following surgery was 32.6%, with a significant difference between the open (32%) and laparoscopic groups (22.1%).
The reported mortality rates for patients submitted to any type of surgical intervention were 8.8%, with a lower rate for the laparoscopic procedures (2.2%) compared to open (11.2%). Similar studies reported higher mortality rates approaching 15%, with comparable overall morbidity rates [49]. It is important to highlight that 84.2% of our cohort had an ASA score ≤ 3. Therefore, our population lower morbidity may also be related to a lower baseline prevalence of comorbidity than prior studies which enrolled overall sicker patients.
Our data support laparoscopy as the standard choice for the treatment of acute cholecystitis and appendicitis. However, its adoption is sensibly lower when there is involvement of small and large intestine and, at the same time, the ratio of laparoscopic procedures converted to open increases following emergency operations which involve the bowel [50, 51].
A very limited number of studies investigating the preoperative risk factors associated with emergency surgery for acute abdomen in patients ≥ 65 years of age have been published to date. The results of the multivariate analyses in the present study showed that patients with increased postoperative mortality rates had higher creatinine and blood sugar levels, low hemoglobin values, and had a previous history of acute myocardial infarction and heart failure.
Moreover, high creatinine and blood sugar levels, low hemoglobin values, oral anticoagulation therapy, acute respiratory failure, the presence of SIRS, an established diagnosis of malignancy and an open surgical approach were independently associated with an increased risk of postoperative morbidity. Recently, Poillucci et al. demonstrated that, in elderly patients with acute appendicitis, perioperative risk assessment in the emergency setting must be as accurate as possible to identify modifiable risk factors that can be addressed before surgery, such as preoperative hemoglobin and creatinine levels [5].
Other population-based studies conducted on the general population found the presence of cerebrovascular disease, cardiopulmonary comorbidities, chronic nephropathy, cirrhosis of the liver, and malignancy to influence the 30-day and 90-day mortality [52].
Among the secondary objectives of the study, we analyzed the conversion rate from laparoscopic to open surgery, and short-term outcomes of elderly patients submitted to emergency abdominal surgery.
Our data on conversion rate (14.4%) are similar to the 11% from the literature and is highly variable according to the different complexity of procedures, with the lowest conversion rates for cholecystectomies and appendectomies.
After multivariate analyses of our data, lowest blood pressure and white blood cell count were associated with conversion to laparotomy and co-morbidities associated with higher conversion rates were only chronic pulmonary conditions.
Our study results must be interpreted within the context of a number of limitations. There is a huge variation in the organization of the emergency surgical departments across the country, and the most relevant source of bias is probably the heterogeneity of care in the various centers involved. This probably derives from the lack of clear recommendations specifically tailored for the evaluation and management of elderlies in need of an emergency surgical operation.
Another limitation is the non-randomized nature associated with any large database. Conclusions from non-randomized studies can be misleading because there is always a chance for selection bias, thus leading to the risk of underestimation or overestimation of the true intervention effect. Patient selection may play a significant role in outcome differences, as more complex patients may be more likely to undergo open intervention, and this may skew the results in favor of laparoscopic surgery.
Finally, a limitation of our data source is that FRAILESEL only recorded 30-day postoperative outcomes. With a large amount of medical expenditures occurring in the last year of life, it would be of extreme interest to better understand longer-term adverse outcomes to aid in decision-making for the opportunity of surgical intervention with the family.
Regardless of technical progress, elderly patients undergoing emergency surgery are at very high risk for in-hospital complications. A detailed analysis of complications and mortality in the present study showed that almost 9% of elderly patients died after surgery for acute abdomen, and over 32% developed complications.
Appropriate patient selection is essential for achieving adequate outcomes in laparoscopic emergency surgery in the elderly. Laparoscopy may be not practicable in case of cardiovascular and respiratory impairment, or in cases where local complexity (extensive adherences, marked small bowel dilatation, severe sepsis, obstructing colorectal cancer, etc.) makes the availability of experienced laparoscopic surgical and nursing staffs mandatory.
In conclusion, the FRAILESEL study demonstrated that emergency operations for acute abdomen in the elderly are basically performed through open surgery, preventing these patients from the benefits of mini-invasive procedures. However, little is known about the reasons for that. Limitations of laparoscopic surgery in these patients could be related to the poor clinical conditions of the patients or to the lack of expertise during night-time or weekend shifts when emergency surgery is usually performed.
References
National Institute on Aging (NIA) (2018) Available at: https://www.nia.nih.gov. Accessed 22 May 2019
ISTAT: Stime per l’anno 2016. 2017, Available at: http://www4.istat.it/it/anziani. Accessed April 1, 2019
Pisano M, Ceresoli M, Cimbanassi S, Gurusamy K, Coccolini F, Borzellino G, Costa G, Allievi N, Amato B, Boerma D, Calcagno P, Campanati L, Campanile FC, Casati A, Chiara O, Crucitti A, di Saverio S, Filauro M, Gabrielli F, Guttadauro A, Kluger Y, Magnone S, Merli C, Poiasina E, Puzziello A, Sartelli M, Catena F, Ansaloni L (2019) 2017 WSES and SICG guidelines on acute calcolous cholecystitis in elderly population. World J Emerg Surg. https://doi.org/10.1186/s13017-019-0224-7
Costa G, Tomassini F, Tierno SM, Venturini L, Frezza B, Cancrini G, Mero A, Lepre L (2009) Emergency colonic surgery: analysis of risk factors predicting morbidity and mortality. Chir Ital 61:565–571
Poillucci G, Podda M, Pisanu A, Mortola L, Dalla Caneva P, Massa G, Costa G, Savastano R, Cillara N, ERASO (Elderly Risk Assessment And Surgical Outcome) Collaborative Study Group (2019) Risk factors for postoperative morbidity following appendectomy in the elderly: a nationwide prospective cohort study. Eur J Trauma Emerg Surg 69:531–540
Saunders DI, Murray D, Pichel AC, Varley S, Peden CJ, Emergency Laparotomy Network UK (2012) Variations in mortality after emergency laparotomy: the first report of the UK Emergency Laparotomy Network. Br J Anaesth 109:368–375
Green G, Shaikh I, Fernandes R, Wegstapel H (2013) Emergency laparotomy in octogenarians: a 5-year study of morbidity and mortality. World J Gastrointest Surg 5:216–221
Kettunen J, Paajanen H, Kostiainen S (1995) Emergency abdominal surgery in the elderly. Hepatogastroenterology 42:106–108
McGillicuddy EA, Schuster KM, Davis KA, Longo WE (2009) Factors predicting morbidity and mortality in emergency colorectal procedures in elderly patients. Arch Surg 144:1157–1162
Iversen LH, Bülow S, Christensen IJ, Laurberg S, Harling H, Danish Colorectal Cancer Group (2008) Postoperative medical complications are the main cause of early death after emergency surgery for colonic cancer. Br J Surg 95:1012–1019
NCEPOD Classification of Intervention (2004) Reference Source
Costa G, Massa G, ERASO (Elderly Risk Assessment for Surgical Outcome) Collaborative Study Group (2018) Frailty and emergency surgery in the elderly: protocol of a prospective, multicenter study in Italy for evaluating perioperative outcome (The FRAILESEL Study). Updates Surg 70:97–104
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative STROBE (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 12:1495–1499
Dindo D, Demartines N, Clavien PA (2004) Classification of Surgical Complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Office for National Statistics (ONS) (2018) National population projections 2014-based statistical bulletin 2015. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/bulletins/nationalpopulationprojections/2015-10-292015. Accessed 1 Apr 2019
ISTAT. Noi Italia 2019. Available at: http://noi-italia.istat.it. Accessed December 22, 2019
Desserud KF, Veen T, Søreide K (2016) Emergency general surgery in the geriatric patient. Br J Surg. https://doi.org/10.1002/bjs.10044
McLean RC, McCallum IJ, Dixon S, O’Loughlin P (2016) A 15-year retrospective analysis of the epidemiology and outcomes for elderly emergency general surgical admissions in the North East of England: a case for multidisciplinary geriatric input. Int J Surg 28:13–21
Stoneham M, Murray D, Foss N (2014) Emergency surgery: the big three–abdominal aortic aneurysm, laparotomy and hip fracture. Anaesthesia 69(Suppl 1):70–80. https://doi.org/10.1111/anae.12492
Al-Temimi MH, Griffee M, Enniss TM, Preston R, Vargo D, Overton S, Kimball E, Barton R, Nirula R (2012) When is death inevitable after emergency laparotomy? Analysis of the American College of Surgeons National Surgical Quality Improvement Program database. J Am Coll Surg 215:503–511
Jimenez Rodriguez RM, Segura-Sampedro JJ, Flores-Cortés M, López-Bernal F, Martín C, Diaz VP, Ciuro FP, Ruiz JP (2016) Laparoscopic approach in gastrointestinal emergencies. World J Gastroenterol 22:2701–2710
Agresta F, Campanile FC, Podda M, Cillara N, Pernazza G, Giaccaglia V, Ciccoritti L, Ioia G, Mandalà S, La Barbera C, Birindelli A, Sartelli M, Di Saverio S, Joined Italian Surgical Societies Working Group (2017) Current status of laparoscopy for acute abdomen in Italy: a critical appraisal of 2012 clinical guidelines from two consecutive nationwide surveys with analysis of 271,323 cases over 5 years. Surg Endosc 31:1785–1795
Mandrioli M, Inaba K, Piccinini A, Biscardi A, Sartelli M, Agresta F, Catena F, Cirocchi R, Jovine E, Tugnoli G, Saverio Di (2016) Advances in laparoscopy for acute care surgery and trauma. World J Gastroenterol 22:668–680
Pucher PH, Carter NC, Knight BC, Toh S, Tucker V, Mercer SJ (2018) Impact of laparoscopic approach in emergency major abdominal surgery: single-centre analysis of 748 consecutive cases. Ann R Coll Surg Engl 100:279–284
Cocorullo G, Falco N, Tutino R, Fontana T, Scerrino G, Salamone G, Licari L, Gulotta G (2016) Open versus laparoscopic approach in the treatment of abdominal emergencies in elderly population. G Chir 37:108–112
Kannan U, Reddy VS, Mukerji AN, Parithivel VS, Shah AK, Gilchrist BF, Farkas DT (2015) Laparoscopic vs open partial colectomy in elderly patients: insights from the American College of Surgeons—National Surgical Quality Improvement Program database. World J Gastroenterol 21:12843–12850
Cerdán Santacruz C, Frasson M, Flor-Lorente B, Ramos Rodríguez JL, Trallero Anoro M, Millán Scheiding M, Maseda Díaz O, Dujovne Lindenbaum P, Monzón Abad A, García-Granero Ximenez E, ANACO Study Group (2017) Laparoscopy may decrease morbidity and length of stay after elective colon cancer resection, especially in frail patients: results from an observational real-life study. Surg Endosc 31:5032–5042
Loozen CS, van Ramshorst B, van Santvoort HC, Boerma D (2017) Early Cholecystectomy for acute cholecystitis in the elderly population: a systematic review and meta-analysis. Dig Surg 34:371–379
Cao AM, Eslick GD, Cox MR (2016) Early laparoscopic cholecystectomy is superior to delayed acute cholecystitis: a meta-analysis of case-control studies. Surg Endosc 30:1172–1182
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA (2014) Meta-analysis of laparoscopic vs open cholecystectomy in elderly patients. World J Gastroenterol 20:17626–17634
Harji DP, Griffiths B, Burke D, Sagar PM (2014) Systematic review of emergency laparoscopic colorectal resection. Br J Surg 101:e126-33. https://doi.org/10.1002/bjs.9348
Cirocchi R, Fearnhead N, Vettoretto N, Cassini D, Popivanov G, Henry BM, Tomaszewski K, D’Andrea V, Davies J, Di Saverio S (2019) The role of emergency laparoscopic colectomy for complicated sigmoid diverticulits: a systematic review and meta-analysis. Surgeon 17:360–369
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy AM, COlon cancer Laparoscopic or Open Resection Study Group (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, Bonjer HJ, COlorectal cancer Laparoscopic or Open Resection II (COLOR II) Study Group (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM, MRC CLASICC trial group (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726
Keller DS, Senagore AJ, Fitch K, Bochner A, Haas EM (2017) A new perspective on the value of minimally invasive colorectal surgery-payer, provider, and patient benefits. Surg Endosc 31:2846–2853
Szomstein S, Lo Menzo E, Simpfendorfer C, Zundel N, Rosenthal RJ (2006) Laparoscopic lysis of adhesions. World J Surg 30:535–540
Sharma R, Reddy S, Thoman D, Grotts J, Ferrigno L (2015) Laparoscopic versus open bowel resection in emergency small bowel obstruction: analysis of the national surgical quality improvement program database. J Laparoendosc Adv Surg Tech A 25:625–630
Johnson KN, Chapital AB, Harold KL, Merritt MV, Johnson DJ (2012) Laparoscopic management of acute small bowel obstruction: evaluating the need for resection. J Trauma Acute Care Surg 72:25–31
Nagle A, Ujiki M, Denham W, Murayama K (2004) Laparoscopic adhesiolysis for small bowel obstruction. Am J Surg 187:464–470
Byrge N, Barton RG, Enniss TM, Nirula R (2013) Laparoscopic versus open repair of perforated gastroduodenal ulcer: a National Surgical Quality Improvement Program analysis. Am J Surg 206:957–963
Wang YR, Richter JE, Dempsey DT (2010) Trends and outcomes of hospitalizations for peptic ulcer disease in the United States, 1993 to 2006. Ann Surg 251:51–58
Bertleff MJ, Lange JF (2010) Laparoscopic correction of perforated peptic ulcer: first choice? A review of literature. Surg Endosc 24:1231–1239
Møller MH, Larsson HJ, Rosenstock S, Jørgensen H, Johnsen SP, Madsen AH, Adamsen S, Jensen AG, Zimmermann-Nielsen E, Thomsen RW, Danish Clinical Register of Emergency Surgery (2013) Quality-of-care initiative in patients treated surgically for perforated peptic ulcer. Br J Surg 100:543–552
Testini M, Portincasa P, Piccinni G, Lissidini G, Pellegrini F, Greco L (2003) Significant factors associated with fatal outcome in emergency open surgery for perforated peptic ulcer. World J Gastroenterol 9:2338–2340
Sheu BF, Chiu TF, Chen JC, Tung MS, Chang MW, Young YR (2007) Risk factors associated with perforated appendicitis in elderly patients presenting with signs and symptoms of acute appendicitis. ANZ J Surg 77:662–666
Moazzez A, Mason RJ, Katkhouda N (2013) Thirty-day outcomes of laparoscopic versus open appendectomy in elderly using ACS/NSQIP database. Surg Endosc 27:1061–1071
Guller U, Jain N, Peterson ED, Muhlbaier LH, Eubanks S, Pietrobon R (2004) Laparoscopic appendectomy in the elderly. Surgery 135:479–488
Ukkonen M, Kivivuori A, Rantanen T, Paajanen H (2015) Emergency Abdominal operations in the elderly: a multivariate regression analysis of 430 consecutive patients with acute abdomen. World J Surg 39:2854–2861
Bala M, Kashuk J, Moore EE, Kluger Y, Biffl W, Gomes CA, Ben-Ishay O, Rubinstein C, Balogh ZJ, Civil I, Coccolini F, Leppaniemi A, Peitzman A, Ansaloni L, Sugrue M, Sartelli M, Di Saverio S, Fraga GP, Catena F (2017) Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery. World J Emerg Surg. https://doi.org/10.1186/s13017-017-0150-5
Di Saverio S, Coccolini F, Galati M, Smerieri N, Biffl WL, Ansaloni L, Tugnoli G, Velmahos GC, Sartelli M, Bendinelli C, Fraga GP, Kelly MD, Moore FA, Mandalà V, Mandalà S, Masetti M, Jovine E, Pinna AD, Peitzman AB, Leppaniemi A, Sugarbaker PH, Goor HV, Moore EE, Jeekel J, Catena F (2013) Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2013 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. https://doi.org/10.1186/1749-7922-8-42
Tolstrup MB, Watt SK, Gögenur I (2017) Morbidity and mortality rates after emergency abdominal surgery: an analysis of 4346 patients scheduled for emergency laparotomy or laparoscopy. Langenbecks Arch Surg 402:615–623
Acknowledgements
List of the Elderly Risk Assessment and Surgical Outcome (ERASO) Collaborative Study Group members (endorsed by SICUT, ACOI, SICG, SICE, and the Italian Chapter of the WSES): F. Agresta, G. Alemanno, G. Anania, M. Antropoli, G. Argenio, J. Atzeni, N. Avenia, A. Azzinnaro, G. Baldazzi, G. Balducci, G. Barbera, G. Bellanova, C. Bergamini, L. Bersigotti, P. P. Bianchi, C. Bombardini, G. Borzellino, S. Bozzo, G. Brachini, G. M. Buonanno, T. Canini, S. Cardella, G. Carrara, D. Cassini, M. Castriconi, G. Ceccarelli, D. Celi, M. Ceresoli, M. Chiarugi, N. Cillara, F. Cimino, L. Cobuccio, G. Cocorullo, E. Colangelo, G. Costa, A. Crucitti, P. Dalla Caneva, M. De Luca, A. de Manzoni Garberini, C. De Nisco, M. De Prizio, A. De Sol, A. Dibella, T. Falcioni, N. Falco, C. Farina, E. Finotti, T. Fontana, G. Francioni, P. Fransvea, B. Frezza, G. Garulli, M. Genna, S. Giannessi, A. Gioffrè, A. Giordano, D. Gozzo, S. Grimaldi, G. Gulotta, V. Iacopini, T. Iarussi, E. Laterza, A. Leonardi, L. Lepre, G. Luridiana, A. Malagnino, G. Mar, P. Marini, R. Marzaioli, G. Massa, V. Mecarelli, A. Mingoli, G. Nigri, S. Occhionorelli, N. Paderno, G. M. Palini, D. Paradies, M. Paroli, F. Perrone, L. Petruzzelli, A. Pezzolla, D. Piazza, V. Piazza, M. Piccoli, A. Pisanu, M. Podda, G. Poillucci, R. Porfidia, G. Rossi, P. Ruscelli, A. Spagnoli, R. Sulis, D. Tartaglia, C. Tranà, A. Travaglino, P. Tomaiuolo, A. Valeri, G. Vasquez, M. Zago, E. Zanoni.
Author information
Authors and Affiliations
Consortia
Contributions
GC: Study conception and design, literature search, acquisition, interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. PF: Study conception and design, literature search, acquisition, interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. MP: Interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. AP: Interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. Francesco MC: Interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. AI: Interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published. GB: Interpretation and analysis of data; critically revising the article for important intellectual content; and final approval of the version to be published. FA: Study conception and design, literature search, interpretation and analysis of data; drafting and critically revising the article for important intellectual content; and final approval of the version to be published.
Corresponding author
Ethics declarations
Conflicts of interest and source of funding
Gianluca Costa, Pietro Fransvea, Mauro Podda, Adolfo Pisanu, Francesco Maria Carrano, Angelo Iossa, Genoveffa Balducci, and Ferdinando Agresta, have no conflict of interest to declare. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
The study has been approved by the Ethics Committee of the University “La Sapienza” (Rome, Italy. Protocol ID: Rif_CE_452_2016). Secondary approval was obtained from all ethics committees of the other participating centers. The study protocol was registered at ClinicalTrials.gov (ClinicalTrials.gov identifier: NCT02825082).
Research involving human participants and/or animals
The study has been performed in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the ERASO (Elderly Risk Assessment and Surgical Outcome) Collaborative Study Group mentioned in “Acknowledgements” section.
Rights and permissions
About this article
Cite this article
Costa, G., Fransvea, P., Podda, M. et al. The use of emergency laparoscopy for acute abdomen in the elderly: the FRAILESEL Italian Multicenter Prospective Cohort Study. Updates Surg 72, 513–525 (2020). https://doi.org/10.1007/s13304-020-00726-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00726-5