Abstract
Acute appendicitis (AA) is among the most common causes of acute lower abdominal pain leading patients to the emergency department. Significant debate remains on whether AA should be operated or not. A propensity score-matched analysis was performed in seven Italian Hospitals, with the aim to assess safety and feasibility both nonoperative management with antibiotics (AT) and surgical therapy with appendectomy (ST) for patients with AA. Data regarding all patients discharged from the participating centers with a diagnosis of appendicitis from January 1st, 2014 to December 31st, 2014 were collected retrospectively. Follow-up data were collected from January 1st, 2015 to December 31st, 2016. The complication-free treatment success of AT (53.7%) was significantly inferior to that of ST (86.4%) (P < 0.0001). Patients initially treated with antibiotics reported an index admission AT failure rate of 20.9% and a recurrence rate at 1-year follow-up of 20.3%. No statistically significant difference was found when comparing AT and ST groups for the outcome of interest post-operative complications (13.5 vs 13.6%, P = 0.834). Patients treated with AT were discharged home earlier than patients in the ST group (3.38 ± 1.89 vs 4.84 ± 2.69 days, P < 0.0001). Due to the low rates of complications occurred in the ST group and the high efficacy of the surgical therapy, laparoscopic appendectomy still represents the most effective treatment for patients with AA. AT is associated with shorter hospital stay and faster return to normal activity, and may prevent from appendectomies around 80% of patients who leave the hospital with clinical recovery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute appendicitis (AA) is among the most common causes of acute lower abdominal pain leading patients to the emergency department, with a lifetime prevalence of about 7% and highest incidence in the second decade of life [1].
AA is heterogeneous in terms of presentation, clinical evolution, and pathological aspects. Most cases are uncomplicated. However, in about 20% of cases, AA is presenting on clinical onset with gangrene, abscesses, localized or diffuse peritonitis [2].
Despite all the improvements in the diagnostic process, significant debate remains on whether AA should be operated or not [3].
Since Lawson Tait performed successfully the first appendectomy in 1880, surgery has been the most widely accepted treatment of choice. Approximately 300,000 people undergo appendectomy each year in the US [4]. Current evidence suggests laparoscopic appendectomy (LA) be the most effective surgical treatment, being associated with lower incidence of wound infections and post-operative morbidity, a shorter hospital stay and better quality of life scores when compared to open surgery [5].
In 1886, Fitz reported that many autopsies specimens were showing pathologic signs consistent with AA, therefore, hypothesizing that in some patients, the disease could resolve without any surgery [6]. In 1953, Harrison reported 42 of 47 cases of AA being successfully treated using antibiotics and Coldrey in 1956 published the data on 471 patients with AA treated conservatively, with low morbidity, mortality (0.2%), and recurrence rates (14.4%) [7, 8].
Over the past 20 years, there has been a renewed interest in the conservative management both uncomplicated (non-perforated) and complicated (gangrenous and perforated) forms of AA, probably due to a more precise analysis of the incidence of post-operative complications and the increasing costs of surgical interventions, which are mostly related to the spreading use of laparoscopic approach [9,10,11,12].
Several studies have been published on conservative management of AA to date [10, 13,14,15]. However, in the vast majority of cases, they compared outcomes achieved by either open appendectomy (OA) and antibiotic treatment (AT). Open procedures accounted for 81.4% of all appendectomies analyzed in the randomized controlled trials published to date [16].
As we are currently in the “laparoscopic era”, applying the findings of these studies in the daily practice would be difficult. In Italy, more than 75% of acute appendicitis are nowadays approached by laparoscopy, and the clinical outcomes achieved by an open approach (length of hospital stay, time to return to normal activities, complication rates, etc.) cannot be applied to our usual practice [17].
Since several relevant questions remain unanswered about nonoperative management of AA, we carried out a propensity score-matched analysis from the data of a multicenter retrospective cohort study, with the aim to assess safety and feasibility both nonoperative management with antibiotics (AT) and surgical therapy with appendectomy (ST) through the analysis of efficacy rates, incidence of recurrence, complications, length of hospital stay, and time to return to normal activity.
Methods
This propensity score-matched analysis comparing AT and ST for patients with acute appendicitis was performed in seven Italian Hospitals registered in the database of the Italian Ministry of Health.
Approval of Ethical Committee was obtained (Acceptance Code: Independent Ethical Committee of the University of Cagliari, PG/2016/7825, 31/05/2016).
The study has been approved by the board of all the hospitals involved and carried out in agreement with the Helsinki Declaration. All parts of the study and the present manuscript have been checked and presented according to the checklist for Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [18]. A written informed consent for the treatment of personal and sensible data was obtained from all patients prior to the data collection and evaluation.
Data regarding all patients discharged from the participating centers with a diagnosis of appendicitis from January 1st, 2014 to December 31st, 2014 were collected retrospectively. Follow-up data were collected from January 1st, 2015 to December 31st, 2016.
Every patient with a clinical suspicion of AA was assessed first through physical examination performed by the on-call general surgeon, second through blood tests, including white blood cell count, polymorphonuclear cells count, C-Reactive Protein levels, and calculation of the Appendicitis Inflammatory Response (AIR) score [19]. Abdominal US and/or CT scan was performed in selected patients, depending on the on-call surgeon’s clinical judgement.
Patients without a direct surgical indication were initially managed conservatively with antibiotics, serial abdominal examinations, and blood tests. Patients were assigned to the surgical treatment group if they received immediate surgical treatment (laparoscopic or open appendectomy, depending on the on-call surgeon’s decision) or were treated with a surgical approach within the first 12 h, based on clinical discretion of the on-call surgeon, according to current good surgical practice and availability of the operating theatre. Patients managed conservatively received one of the following parenteral antibiotic treatments: Piperacillin/Tazobactam (4.5 g) three intravenous administration per day; Ceftriaxone (2 g) once per day or Ciprofloxacin (500 mg) twice per day plus Metronidazole (500 mg) three times per day; Amoxicillin/Clavulanic acid (2 g) four times per day for a length depending on the clinical conditions; and Ertapenem (1 g) one administration per day for 3 days. Patients were discharged with oral antibiotics (amoxicillin/clavulanic acid or ciprofloxacin) for at least 4 days.
Inclusion criteria
-
Signed informed consent for the treatment of personal and sensible data.
-
Age range 18–65 years.
-
Diagnosis of AA made using the appendicitis inflammatory response (AIR) score, eventually confirmed by ultrasound and/or CT scan in selected patients, depending on the on-call surgeon’s judgement.
Exclusion criteria
-
Pregnant or lactating.
-
Non-consenting patients.
-
Positive diagnosis for inflammatory bowel disease (IBD).
-
Clinical diagnosis of diffuse peritonitis, confirmed by CT scan.
-
Appendectomy performed as an elective procedure.
-
Appendectomy performed during other abdominal surgical procedures.
-
Previous hospitalization for acute appendicitis treated conservatively.
Definition of outcomes
Primary outcome
-
Treatment efficacy was defined as “complication-free treatment success based on 1-year follow-up” (success of the initial treatment with uncomplicated course: no post-operative complications, adverse events, or treatment failure occurring).
Secondary outcomes
-
Index admission antibiotic therapy failure: failure of AT during initial hospitalization (lack of efficacy in the AT group intended as non-resolving AA).
-
Recurrence at 1-year follow-up. Recurrence of AA was defined as an episode of appendicitis being diagnosed again after the initial antibiotic treatment was completed and the patient had been discharged home.
-
Analysis of treatment modality for index admission antibiotic failures and recurrences (further cycles of AT or ST).
-
Overall post-intervention complications, assessed by the Dindo–Clavien Classification. The number and rate of abscesses, post-operative peritonitis, surgical site infections, incisional hernias, incisional pain, or obstructive symptoms and other general complications. Complications were analyzed both for patients who underwent ST as primary treatment and for those who underwent surgery as second line approach, after the failure of AT.
-
Length of primary hospital stay.
-
Time to return to normal activities: rates of patients who returned to normal activities within 2 weeks from the treatment.
Theory/calculation
Statistical Package for the Social Sciences (SPSS), version 22 (SPSS Inc., Chicago, IL, USA) has been used to carry out the statistical analysis. Dichotomous variables have been expressed as numbers and percentages, while continuous variables as mean and standard deviation (SD). Student’s t test or ANOVA have been used for comparisons of continuous variables between groups. Chi-square test or Fisher’s exact test, as appropriate, have been used for analysis of categorical data. Results of univariate analysis were expressed as follows: odd ratios (OR) for dichotomous outcomes and β-coefficients for continuous outcomes, both with the correspondent 95% confidence intervals (95% CI). The Propensity Score (PS) model was calculated considering the following variables as covariates: age, sex, AIR score on admission and pre-intervention diagnosis [20]. Treated patients (AT group) and controls (ST group) were matched using “nearest neighbour matching” based on the individual PS with a caliper set at 0.2 and with a 1:1 matching model with replacement.
A multiple logistic regression model has been used to investigate clinical, laboratory, and radiologic variables (independent variables) predictive of conservative treatment failure and success (dependent variable) using the STATA/SE, version 14 (StataCorp LP, College Station, TX, USA). A value of P < 0.05 was considered statistically significant.
Sample size calculation
Prior similar studies found a complication-free treatment success rate of approximately 68% in the antibiotic-first therapy group and of 89% in the surgical group [21]. We estimated that a minimum of 76 patients per group would yield a power of 0.90 (1 − β) to establish whether appendectomy was superior to antibiotic-first treatment using a one-sided significance ɑ level of 0.05 (5%) with Power Sample Size Calculator (sealedenvelope.com). We anticipated a 15% loss to follow-up, resulting in our plan to enroll at least 175 patients.
Results
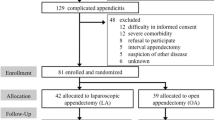
A total of 502 clinical records were identified and reviewed. 46 patients had a diagnosis of diffuse peritonitis from ruptured appendicitis confirmed by CT scan, and were excluded from the analysis. Of the 456 patients who met the inclusion criteria, 78 (17.1%) were lost to follow-up or excluded because of incomplete/incongruous follow-up data availability. Mean follow-up period was 20 ± 4 months. According to our selection criteria, 378 patients were available in our database for complete follow-up. Matching was not possible for 32 patients of the surgical group.
The matched group was composed of 162 patients (46.8%) submitted to AT and 184 patients (53.2%) to ST. Within the latter group, 157 patients (85.6%) and 27 patients (14.4%) underwent LA and OA. No statistically significant difference was found in the rate of LA when comparing the surgical technique adopted in ST group and in the subgroup of patients who underwent surgery after failure of the antibiotic strategy (LA 80.3% and OA 19.7%).
The rate of complicated appendicitis identified at the time of surgical operation did not show any statistically significant difference between the two groups (29.4 and 23.8% in the AT and ST groups, respectively; P = 0.519).
The general characteristics of patients enrolled in the study (pre-matching and post-matching groups) are shown in Tables 1 and 2.
Treatment efficacy
A higher rate of efficacy was found in the ST group when compared with the AT group. Taking into account any kind of post-interventional complication (post-operative complications, adverse events, and treatment failure), the post-matching analysis showed that the complication-free treatment success of AT (53.7%) was significantly inferior to that of ST (86.4%) (OR 5.482, 95% CI 3.250:9.247, P < 0.0001).
Patients initially treated with antibiotics reported an index admission AT failure rate of 20.9% and a recurrence rate at 1-year follow-up of 20.3%.
The post-matching analysis of treatment modality for index admission antibiotic failures and recurrences showed that all patients who reported an index admission failure were subsequently treated with surgery, whereas 33.3% of patients diagnosed with a recurrence was successfully managed with a further cycle of antibiotics. Results are shown in Table 3.
Post-operative complications
At the post-matching analysis, no statistically significant difference was found when comparing AT and ST groups for the outcome of interest post-operative complications (13.5 vs 13.6%, OR 1.06, 95% CI 0.449:2.502, P = 0.834). Complications after surgery for patients who experienced an index admission AT failure accounted for 2.9%, whereas 8.7% of patients reported a complication after appendectomy performed for a recurrence of acute appendicitis (Table 3). Complications following appendectomy as the first-line approach were 4 abscesses, 1 cardiovascular complication, 3 hemorrhages from the trocar sites insertion, 6 surgical site infections, and 11 other general complications. According to the Dindo–Clavien classification of surgical complications, 15 grade I (8.15%), 5 grade II (2.72%), 2 grade IIIa (1.09%), and 3 grade IIIb (1.63%) complications were reported. Conversely, in the AT group patients who were submitted to surgery, 3 grade I (3.57%), 2 grade II (1.78%), and 3 grade IIIb (3.57%) complications were recorded.
Length of hospital stay and return to normal activity in 2 weeks
Data on length of primary hospital stay demonstrated that patients successfully treated with AT were discharged home earlier than patients in the ST group, with a statistically significant difference (3.38 ± 1.89 vs 4.84 ± 2.69 days, β − 2.17, 95% CI − 2.60:− 1.73, P < 0.0001). Conversely, the length of hospital stay in the subgroup of patients who underwent surgery for index admission antibiotic-first strategy failure was 5.32 ± 3.02 days, with no statistically significant difference when compared to the outcome in the ST group (5.32 ± 3.02 days, β − 0.480, 95% CI − 1.489:0.529, P = 0.437).
Similarly, at the post-matching analysis, patients successfully treated with antibiotics had a faster return to normal daily life. In fact, 93.7% of them returned to normal activities in 2 weeks, whereas only 76.1% of patients in the ST did (OR 5, 95% CI 3.146:7.945, P < 0.0001), as shown in Table 3.
Multiple logistic regression analysis
Age, sex, AIR score, classification of the disease (uncomplicated or complicated), time from the onset of symptoms to the administration of antibiotic therapy, and the type of antibiotics used were included as variables in a multiple logistic model. Among these variables, it was possible to include only age and AIR score (in two classes: < 5 and ≥ 5). Sex, classification of the disease, and duration of the symptoms considered individually were not associated with the identified outcome variable (success vs failure of antibiotic therapy). The results of the multiple logistic regression analysis showed that the risk of the antibiotic-first strategy failure increased with increasing age (OR 1.027; P = 0.018; 95% CI 1.004–1.049), and with AIR scores ≥ 5 (OR 3.236; P = 0.006; 95% CI 1.405–7.458), although a specific age interval related to an augmented risk of AT failure was not identified.
Discussion
Several questions remain unanswered when talking about safety and feasibility of nonoperative treatment with antibiotics for patients with acute appendicitis.
The first question concerns efficacy.
The choice of the primary outcome measure used to compare such different treatment strategies may represent a difficult step.
In the trial published by Hansson et al., efficacy for AT was defined as achieving a definitive improvement without requiring surgery within a median follow-up of 1 year. Lack of efficacy in the AT group included both index admission treatment failure of antibiotic therapy during the hospitalization and recurrences. On the other hand, efficacy for the ST was defined as AA confirmed at the time of the surgical operation and resolution of symptoms after surgical treatment [22]. Allievi et al. recently published the results from a propensity score-based outcome analysis of conservative vs surgical management for patients with AA in which the primary outcome (failure rate) was evaluated using different definitions for the two groups of treatment. For the surgical group, failure was defined as the occurrence of pre- and post-operative complications, eventually associated with negative appendectomy. With regard to failure within the medical group, all patients who needed surgical therapy after 72 h of conservative management were accounted for as failure cases [23].
However, to allow a reliable analysis of the efficacy of the two therapeutic strategies, in our personal opinion, the primary outcome should be identical for both the branches of treatment, and combine endpoints of efficacy and safety at the same time.
The definitions of “Efficacy” and “Safety” provided by Harnoss et al. in their recent systematic review and meta-analysis met the above-mentioned criteria. “Efficacy” was defined by the success of the initial treatment with uncomplicated course (no post-intervention complications, adverse events, or treatment failure occurring); “Safety” was defined by the absence of post-operative complications, adverse events of antibiotic treatment, and complicated progress of the disease [21].
Although in the past, the common behavior suggested that the proportion of perforations increased with the duration of symptoms and progression from an uncomplicated form of AA to perforation was considered dogmatic, an increasing amount of evidence suggests not only that not all patients with appendicitis will progress to perforation, but even that the resolution may be a common event [24]. The increasing proportion of perforations with duration of symptoms may at least partly be explained by selection of patients with perforated appendicitis because of spontaneous resolution of the non-perforated cases [25].
Regarding efficacy outcomes, the results of the present study, conducted on 346 patients with acute appendicitis, have confirmed the superiority of the ST approach, which has shown a complication-free treatment success rate of 86.4% at the post-matching analysis. Conversely, AT resulted in a 53.7% of cases successfully treated (P < 0.0001). 20.9% of patients initially treated with antibiotics experienced an index admission failure of the conservative treatment, whereas 20.3% presented with an episode of recurrence during the follow-up period.
It is worth noting that around 80% of patients who left the hospital with clinical recovery did not experience appendectomy within a median follow-up time close to 2 years. The same results have been recently published by Lundholm et al. in a large series of 710 patients with a mean follow-up of over 9 years [26].
To date, several meta-analyses, randomized controlled trials, and propensity score-based analysis comparing AT and ST for AA have been published in the literature [10, 12, 15, 21, 23, 27, 28]. Although these studies support the evidence that the majority of patients can be treated with an antibiotic-first therapy avoiding appendectomy, contrasting data about rates of the efficacy of antibiotic therapy, especially regarding long-term outcomes, have been obtained [22, 29].
When performing a pooled analysis of the trials published up to the current date, our group found that AT management was associated with a significantly lower treatment efficacy based on the 1-year follow-up when compared to ST (75.9 vs 98.3%). In particular, the recurrence rate was 22.5% with a mean length of time to recurrence of 4.65 months [16].
However, each trial published in the literature shows limitations in terms of patient selection bias, definition of primary endpoints, lack of a standardized computed tomography, or ultrasound scan diagnosis. Furthermore, the majority of the appendectomies performed for patients enrolled in RCTs published so far were performed by open approach, whereas laparoscopic appendectomy is being increasingly performed worldwide and will likely be elected as the gold standard surgical approach in the near future [5, 17].
Recently, the ACTUAA study has been launched, with the aim to test the hypothesis that surgical treatment with appendectomy is superior to the conservative approach with antibiotics for patients with uncomplicated acute appendicitis. It is designed as a prospective, non-randomized, controlled, open label, superiority multi-institutional trial to compare conservative treatment with antibiotics and appendectomy for patients with uncomplicated acute appendicitis confirmed by US and/or CT or MRI scan [30].
The second question is how to distinguish during patients’ assessment those who might respond well to AT alone from those who would require surgery. Our attempt to identify a subgroup of patients who might be treated with antibiotics through a multivariate analysis showed that the risk of the AT strategy failure increased with increasing age and AIR scores ≥ 5, although a specific age interval related to an increased risk of AT failure was not identified. Sex, classification of the disease (uncomplicated or complicated), time from the onset of symptoms to the administration of antibiotic therapy, and the type of antibiotics were not directly related to failure or success of the conservative treatment.
Hansson et al. in their study on 581 patients with acute appendicitis published in 2014 found that patients with assumed appendicitis who fulfilled all criteria with CRP < 60 g/L, WBC < 12 × 109/L, and age < 60 years had 89% of chance to recover with antibiotics without surgery [31].
A further issue concerns the treatment modality of recurrent episodes of appendicitis for patients previously treated with antibiotics. The NOTA study stated that a second attempt with AT could be a successful option for over 60% of patients who present with a recurrent episode of appendicitis at follow-up [32]. In our experience, 33.3% of patients who presented with a recurrence at follow-up were successfully treated with a further cycle of antibiotics, whereas 66.7% underwent surgery.
A further matter of debate is whether the diagnosis of AA should be necessarily performed by the US or CT scan. The WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis stated that the use of imaging techniques in the diagnostic workup should be linked to risk stratification such as AIR or Alvarado scores. Intermediate-risk classification identifies patients likely to benefit from systematic diagnostic imaging, whereas high-risk patients may not require pre-operative imaging [5].
In our study, the great majority of patients were classified with an AIR score of 5–8 (intermediate), and the diagnosis was carried out via diagnostic imaging in 63% of the patients enrolled in the study.
In the EU, only around 13% of patients undergo pre-operative imaging, which is typically reserved for elderly patients who might have cancer, atypical or delayed presentations or those who have suspected appendicular masses or abscesses [33]. Young males with typical clinical histories and examination findings go straight to surgery-first without any imaging. Conversely, in the USA, 86% of patients actually undergo pre-operative imaging, 91% of whom undergo CT [34].
The most common post-operative complications following an appendectomy, such as wound infections, intra-abdominal abscess, and ileus caused by adhesions may vary in frequency between open (overall complication rates 11.1%) and laparoscopic (8.7%) appendectomy [35, 36].
No statistically significant difference was found when comparing patients submitted to surgery after AT and ST for post-operative complications in our study (13.5 vs 13.6). Complications after surgery for patients who experienced an index admission AT failure accounted for 2.9%, whereas 8.7% of patients reported a complication after appendectomy performed for a recurrence of acute appendicitis.
The shorter length of hospital stay and early return to daily normal activity are two well-known advantages of the antibiotic-first management, especially in terms of cost-effectiveness. In our study, patients successfully treated with AT were discharged much earlier, with a mean length of primary hospital stay of 3.38 ± 1.89 vs 4.84 ± 2.69 of the ST group, with a statistically significant difference. In the same way, patients treated with antibiotics without surgery returned earlier to normal activity. Indeed, our results demonstrated that 93.7% of patients successfully treated conservatively returned to normal activity in 2 weeks, whereas only 76.1% of the ST group achieved the same result. Therefore, the conservative treatment may be considered advantageous from a socio-economic point of view.
Possible limitations of this study are related to its retrospective design, which carries a high risk of selection bias. In fact, we cannot exclude that AT was preferred for selected patients expected to have better chances of successful conservative treatment and better outcomes.
Moreover, although CT and US scans are thought to be the best tools, not only to diagnose acute appendicitis, but even to distinguish between uncomplicated and complicated forms, only 60 and 65% of patients in the AT and ST groups, respectively, underwent diagnostic imaging before the treatment choice. Therefore, the question is whether the rate of patients, initially treated with antibiotics and subsequently operated on during the index admission for the persistence of symptoms, was affected by a complicated form ab initio, or the natural history of the disease was more aggressive in this subgroup of patients. However, to overcome this limitation, a propensity score analysis with a “nearest neighbour” matching allowed us to obtain two balanced groups in terms of age, sex, laboratory variables, and pre-intervention diagnosis.
Based on this study, due to the low rates of complications occurred in the ST group and the high efficacy of the surgical therapy, laparoscopic appendectomy still represents the most effective treatment for patients with AA. However, AT is associated with shorter hospital stay and faster return to normal activity, and may prevent from appendectomies around 80% of patients who leave the hospital with clinical recovery. When a conservative treatment is attempted, surgeons must appropriately inform patients about the current evidence of the efficacy related to an antibiotic-first strategy, as well as inform about the uncertainties.
Further large prospective multicenter trials with adequate multivariate analysis are needed to identify a subgroup of patients with AA for whom antibiotic treatment can be highly effective.
Abbreviations
- AA:
-
Acute appendicitis
- LA:
-
Laparoscopic appendectomy
- OA:
-
Open appendectomy
- AT:
-
Antibiotic therapy
- ST:
-
Surgical therapy
- AIR:
-
Appendicitis inflammatory response
- US:
-
Ultrasound scan
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- RCTs:
-
Randomized controlled trials
References
Humes DJ, Simpson J (2006) Acute appendicitis. BMJ 333:530–534
Livingston EH, Woodward WA, Sarosi GA et al (2007) Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg 245:886–892
Podda M, Cillara N, Balestra F et al (2017) A short commentary on “Nonoperative management of uncomplicated appendicitis in adults: what do we need to get certainty?”. Int J Surg. 40:109–111
Addiss DG, Shaffer N, Fowler BS et al (1990) The epidemiology of appendicitis and appendectomy in the US. Am J Epidemiol 132:910–925
Di Saverio S, Birindelli A, Kelly MD et al (2016) WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg. https://doi.org/10.1186/s13017-016-0090-5 (eCollection 2016; Review)
Fitz R (1886) Perforating inflammation of the vermiform appendix. Am J Med Sci 92:321–346
Harrison PW (1953) Appendicitis and antibiotics. Am J Surg 85:160–163
Coldrey E (1956) Treatment of acute appendicitis. Br Med J 2:1458–1461
Flum DR (2015) Acute appendicitis—appendectomy or the “Antibiotics first” strategy. N Engl J Med 372:1937–1943
Salminen P, Paajanen H, Rautio T et al (2015) Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis. The APPAC randomized clinical trial. JAMA 313:2340–2348
Findlay JM, Kafsi JE, Hammer C et al (2016) Nonoperative management of appendicitis in adults: a systematic review and meta-analysis of randomized controlled trials. J Am Coll Surg 223:814–824
Mentula P, Sammalkorpi H, Leppaniemi A (2015) Laparoscopic surgery or conservative treatment for appendiceal abscess in adults? A randomized controlled trial. Ann Surg 262:237–242
Vons C, Barry C, Maitre S et al (2011) Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet 377:1573–1579
Styrud J, Eriksson S, Nilsson I et al (2006) Appendectomy versus antibiotic treatment in acute appendicitis. A prospective multicenter randomized controlled trial. World J Surg 30:1033–1037
Talan DA, Saltzman DJ, Mower WR et al (2016) Antibiotics-first versus surgery for appendicitis: a US pilot randomized controlled trial allowing outpatient antibiotic management. Ann Emerg Med. https://doi.org/10.1016/j.annemergmed.2016.08.446 (Epub ahead of print)
Podda M, Cillara N, Di Saverio S et al (2017) Antibiotics-first strategy for uncomplicated acute appendicitis in adults is associated with increased rates of peritonitis at surgery: a systematic review with meta-analysis of randomized controlled trials comparing appendectomy and non-operative management with antibiotics. Surgeon. https://doi.org/10.1016/j.surge.2017.02.001 [(Epub ahead of print) Review]
Agresta F, Campanile FC, Podda M et al (2016) Current status of laparoscopy for acute abdomen in Italy: a critical appraisal of 2012 clinical guidelines from two consecutive nationwide surveys with analysis of 271,323 cases over 5 years. Surg Endosc 31:1785–1795
von Elm E, Altman DG, Egger M et al (2008) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61:344–349
Andersson M, Andersson RE (2008) The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World J Surg 32:1843–1849
D’Agostino RB (1998) Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 17:2265–2281
Harnoss JC, Zelienka I, Probst P et al (2016) Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015: CRD42015016882). Ann Surg. https://doi.org/10.1097/SLA.0000000000002039 (Epub ahead of print)
Hansson J, Körner U, Khorram-Manesh A et al (2009) Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg 96:473–481
Allievi N, Harbi A, Ceresoli M et al (2017) Acute appendicitis: still a surgical disease? Results from a propensity score-based outcome analysis of conservative versus surgical management from a prospective database. World J Surg. https://doi.org/10.1007/s00268-017-4094-4
Andersson RE (2007) The natural history and traditional management of appendicitis revisited: spontaneous resolution and predominance of prehospital perforations imply that a correct diagnosis is more important than a early diagnosis. World J Surg 31:86–92
Luckmann R (1989) Incidence and case fatality rates for acute appendicitis in California. A population-based study of the effects of age. Am J Epidemiol 129:905–918
Lundholm K, Hansson-Assarsson J, Engström C et al (2017) Long-term results following antibiotic treatment of acute appendicitis in adults. World J Surg. https://doi.org/10.1007/s00268-017-3987-6 (Epub ahead of print)
Ehlers AP, Talan DA, Moran GJ et al (2016) Evidence for an antibiotics-first strategy for uncomplicated appendicitis in adults: a systematic review and gap analysis. J Am Coll Surg 222:309–314
Lima Rocha L, Bianco Rossi FM, Souza Pessoa CM et al (2015) Antibiotics alone versus appendectomy to treat uncomplicated acute appendicitis in adults: what do meta-analyses say? World J Emerg Surg. https://doi.org/10.1186/s13017-015-0046-1 (ECollection)
Eriksson S, Granström L (1995) Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg 82:166–169
Podda M, Serventi F, Mortola L et al (2017) A prospective non-randomized controlled, multicenter trial comparing Appendectomy and Conservative Treatment for patients with Uncomplicated Acute Appendicitis (the ACTUAA STUDY). Int J Colorect Dis. https://doi.org/10.1007/s00384-017-2878-5
Hansson J, Khorram-Manesh A, Alwindawe A et al (2014) A model to select patients who may benefit from antibiotic therapy as the first line treatment of acute appendicitis at high probability. J Gastrointest Surg 18:961–967
Di Saverio S, Sibilio A, Giorgini E et al (2014) The NOTA study (Non Operative Treatment for Acute Appendicitis): prospective study on the efficacy and safety of antibiotics (amoxicillin and clavulanic acid) for treating patients with right lower quadrant abdominal pain and long-term follow-up of conservatively treated suspected appendicitis. Ann Surg 260:109–117
National Surgical Research, C (2013) Multicentre observational study of performance variation in provision and outcome of emergency appendicectomy. Br J Surg 100:1240–1252
Collaborative S et al (2008) Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Ann Surg 248:557–563
Nakhamiyayev V, Galldin L, Chiarello M et al (2010) Laparoscopic appendectomy is the preferred approach for appendicitis: a retrospective review of two practice patterns. Surg Endosc 24:859–864
Wilms IM, de Hoog DE, de Visser DC et al (2011) Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD008359.pub2
Acknowledgements
The authors would like to thank and express gratitude to Professor Silvio Garattini and Doctor Vittorio Bertele’ (Mario Negri Institute for Pharmacological Research, Milan, Italy) for the intellectual review of the ACTUAA-R Study Project on Acute Appendicitis, and Mr. Christian Raffinetti for the English language editing. The study has been possible mainly thanks to all the colleagues of the ACTUAA-R study group on Acute Appendicitis and the Italian Surgical Units involved, which have taken the time to give their unique contribution.
Francesco Balestra: General, Emergency and Robotic Surgical Unit, San Francesco Hospital, Nuoro (Italy). Fernando Serventi: General and Emergency Surgical Unit, Civile Hospital, Alghero (Italy). Stefania Fiume: Emergency Surgical Unit, Brotzu Hospital, Cagliari (Italy). Antonio Lai: General and Emergency Surgical Unit, San Marcellino Hospital, Muravera (Italy). Simona Ledda: General and Emergency Surgical Unit, Nostra Signora di Bonaria Hospital, San Gavino (Italy). Fabio Pulighe: General, Emergency and Robotic Surgical Unit, San Francesco Hospital, Nuoro (Italy). Sara Gobbi: Department of Surgery, Giovanni Paolo II Hospital, Olbia (Italy). Carlo De Nisco: General, Emergency and Robotic Surgical Unit, San Francesco Hospital, Nuoro (Italy). Giulio Argenio: General, Emergency and Robotic Surgical Unit, San Francesco Hospital, Nuoro (Italy). Giorgio Norcia: General and Emergency Surgical Unit, Civile Hospital, Alghero (Italy). Sergio Gemini: Emergency Surgical Unit, Brotzu Hospital, Cagliari (Italy). Raffaele Sechi: General and Emergency Surgical Unit, Nostra Signora di Bonaria Hospital, San Gavino (Italy). Miriam Pala: Department of Surgery, Santissima Trinità Hospital, Cagliari (Italy). Renata Pau: Department of Surgery, Santissima Trinità Hospital, Cagliari (Italy). Roberto Ottonello: General and Emergency Surgical Unit, San Marcellino Hospital, Muravera (Italy). Marcello Pisano: General and Emergency Surgical Unit, San Marcellino Hospital, Muravera (Italy). Simona Aresu: General and Emergency Surgical Unit, Nostra Signora della Mercede Hospital, Lanusei (Italy). Massimiliano Coppola: General and Emergency Surgical Unit, Nostra Signora della Mercede Hospital, Lanusei (Italy). Antonio Tuveri: Department of Surgery, CTO Hospital, Iglesias (Italy). Francesco Madeddu: Department of Surgery, CTO Hospital, Iglesias (Italy). Antonella Piredda: Department of Surgery, Sirai Hospital, Carbonia (Italy). Giovanni Pinna: Department of Surgery, Sirai Hospital, Carbonia (Italy). Fabrizio Scognamillo: Surgical Pathology Institute, University Hospital, Sassari (Italy). PierLuigi Tilocca: Surgical Pathology Institute, University Hospital, Sassari (Italy). Leonardo Delogu: General Surgery Department, A. Segni Hospital, Ozieri (Italy). Gian Marco Carboni: General Surgery Department, A. Segni Hospital, Ozieri (Italy). Gianfranco Porcu: Department of Surgery, San Martino Hospital, Oristano (Italy). Danilo Piras: Department of Surgery, San Martino Hospital, Oristano (Italy)
Author information
Authors and Affiliations
Consortia
Contributions
Gaetano Poillucci, Lorenzo Mortola, Mauro Podda, Salomone Di Saverio, Chiara Gerardi, Nicola Cillara, and Luigi Presenti: study conception and design, acquisition, analysis and interpretation of data, drafting and critically revising the manuscript for important intellectual content, and final approval of the version to be published; Laura Casula: analysis and interpretation of data, critically revising the manuscript for important intellectual content, and final approval of the version to be published.
Corresponding author
Ethics declarations
Ethical approval
Independent Ethical Committee of the University of Cagliari (Acceptance Code: PG/2016/7825, 31/05/2016).
Conflict of interest
Gaetano Poillucci, Lorenzo Mortola, Mauro Podda, Salomone Di Saverio, Laura Casula, Chiara Gerardi, Nicola Cillara, and Luigi Presenti have no conflicts of interest or financial ties to disclose.
Research involving human participants and/or animals
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (Independent Ethical Committee of the University of Cagliari) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from all patients for being included in the study. Additional written informed consent for the treatment of personal and sensible data was obtained from all patients prior to the data collection and evaluation.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Additional information
Members of the ACTUAA-R Collaborative Working Group on Acute Appendicitis are listed in the Acknowledgement section at the end of the article.
Rights and permissions
About this article
Cite this article
Poillucci, G., Mortola, L., Podda, M. et al. Laparoscopic appendectomy vs antibiotic therapy for acute appendicitis: a propensity score-matched analysis from a multicenter cohort study. Updates Surg 69, 531–540 (2017). https://doi.org/10.1007/s13304-017-0499-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-017-0499-8