Abstract
γ-Aminobutyric acid (GABA) is a natural non-protein amino acid, which broadly exists in many plant parts and is widely used as an ingredient in the food industry. In mammals, it is widely distributed in central nervous system and non-neural tissues. In addition to a primary inhibitory neurotransmitter in the central nervous system, endogenous GABA content has been found to be elevated in neoplastic tissues in colon cancer. However, the effect of extraneous GABA on colon cancer has rarely been reported. In this study, we found the inhibitory effects of GABA on the proliferation of colon cancer cells (CCCs). The amino acid also suppressed metastasis of SW480 and SW620 cells. To further study the correlated mechanism, we analyzed the changes in cell cycle distribution and found that GABA suppressed cell cycle progression through G2/M or G1/S phase. Furthermore, RNA sequencing analysis revealed GABA-induced changes in the mRNA expression of 30 genes, including EGR1, MAPK4, NR4A1, Fos, and FosB, in all the three types of CCC. Importantly, GABA enhanced the anti-tumor efficacy of oxaliplatin (OXA) in subcutaneous xenograft tumor model in nude mice. The data suggest that GABA inhibits colon cancer cell proliferation perhaps by attenuating EGR1-NR4A1 axis, EGR1-Fos axis, and by disrupting MEK-EGR1 signaling pathway. This work reveals the pharmacological value of GABA derived from food and suggests that exogenous GABA might play an auxiliary role in polychemotherapy of colon cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colon cancer is one of the most common types of neoplasia in developed countries [1, 2]; however, the side effects of chemotherapy for colon cancer often result in poor quality of life. A number of studies have demonstrated that certain natural bioactive compounds found in food and herbs can modulate the expression of tumor suppressor genes [3]. Thus, strategies aimed at suppressing tumor growth or metastasis through the consumption of bioactive food components are an excellent approach in cancer prevention and potentially in anti-cancer therapy.
γ-Aminobutyric acid (GABA), a natural non-protein amino acid, is a bioactive constituent of fruits, vegetables, and cereals and is believed to play a role in defense against stress in plants [4]. In animals, it acts as an inhibitory neurotransmitter in brain, while it is also expressed in non-neuronal cells, and studies have shown its relationship with cancer [4–6]. Stimulating GABA signaling induces apoptosis in human neuroblastoma cells [7], and treatment with GABA can attenuate growth of non-small-cell lung cancer cells [8]. Exogenous GABA also demonstrates obvious inhibitory effects on proliferation in other types of cancer cells, including Panc-1 pancreatic cancer cell line and SW480 colon adenocarcinoma cell line [4, 9]. Conversely, significantly high levels of GABA have been found in human colon cancer tissues compared with corresponding para-carcinoma tissues, suggesting that endogenous GABA exerts a colon cancer-promoting effect [10, 11]. Therefore, the influence of GABA on colon cancer remains elusive.
In this study, Cell Counting Kit-8 (CCK-8) assays in vitro and subsequent evaluation of tumor formation in nude mice confirmed the inhibitory effects of exogenous GABA on colon carcinoma cell proliferation. Importantly, this is the first study to report that GABA enhances the anti-cancer effects of OXA. Accordingly, GABA might represent a novel candidate for colon cancer combination therapy.
Materials and methods
Animals
Four-week-old female BALB/c mice were purchased from Shanghai SLAC Laboratory Animal Co., Ltd. (Shanghai, China). All animals were housed under standard conditions of 12-h light/dark cycles with free access to food and water. The experimental protocols were approved by the Institutional Animal Ethics Committee of the Shanghai Institutes for Biological Sciences.
Cells and reagents
SW480, SW620, and HCT116 cells were all obtained from the Shanghai Cell Resource Center, Chinese Academy of Science. SW480 and SW620 were cultured in Dulbecco’s modified Eagle’s medium (DMEM) (Invitrogen, Carlsbad, CA, USA), while HCT116 cells were cultured in MyCoy’s 5 A medium (Basalmedia, Shanghai, China), supplemented with 10 % fetal calf serum (FBS) (Gibco®, Thermo Fisher Scientific, Shanghai, China), and were maintained at 37 °C in an atmosphere of humidified air with 5 % CO2. GABA was purchased from Sigma-Aldrich, Shanghai, China. OXA was from Sanofi-Aventis, Paris, France.
Cell proliferation assay
The cells were seeded at the density of 1300 cells/well into 96-well plates (Corning, Shanghai, China), containing 100 μL of the complete medium. Twenty-four hours later, cells were incubated with drugs for 24–72 h, and then, cell proliferation assay was performed by using CCK-8 (Dojindo, Kumamoto, Japan) according to the manufacturer’s instructions. Briefly, 10 μL of CCK-8 solution was added to each well. After incubation at 37 °C for another 80 min, optical density values at 450 nm (OD 450 nm) were measured by a microplate reader (Multiskan MK3, Thermo Scientific, Shanghai, China).
Cell cycle arrest studies
Cells were seeded in 10-cm dishes, treated with or without GABA for 72 h, and then, trypsinized, harvested, washed twice with ice-cold PBS, and fixed in 70 % ice-cold ethanol and incubated at 4 °C overnight. After washing with ice-cold PBS, cell pellets formed by 1 × 106 cells were incubated with 500 μL of PI/RNase staining buffer (BD Pharmingen, Shanghai, China) for 15 min in the dark at room temperature (RT). Subsequently, DNA content of cells was examined by using a FACSCalibur flow cytometer and analyzed by using ModFit LT software (Becton Dickinson, NJ, USA).
Cell migration and invasion assays
Serum-induced cell migration was examined using 24-well Transwell chambers (Greiner, Frickenhausen, Germany) with 8-μm pores, precoated with or without matrix for the use of performing migration and invasion assays, respectively. The 1.5 × 105 SW480 cells, 1.5 × 105 HCT116 cells, and 5.0 × 105 SW620 cells were incubated with or without GABA, respectively. To evaluate cell migration or invasion, cells were then placed in the upper chamber for 24 h in serum-free medium. The lower chamber contained 10 % serum. After incubation, the upper surface of the Transwell membrane was wiped gently with a cotton swab to remove non-migrating cells. Cells which migrated to the lower surface of the membrane were stained using 0.1 % crystal violet, and photomicrographs of the whole well were captured by using a stereo microscope (Olympus ZX16, Tokyo, Japan).
RNA sequencing
Colon cancer cells were seeded in 10-cm dishes. SW620 and SW480 cells were treated with or without 100 μM of GABA for 72 h, while HCT116 cells were with or without 400 μM of GABA for 48 h. Then, the cells were washed twice with PBS. Subsequently, RNA was extracted using TRIzol reagent and applied to Solexa/Illumina sequencing (Shanghai Biotechnology Co. Ltd., Shanghai, China). Hg19 RefSeq (RNA sequences, GRCh37) was downloaded from the UCSC Genome Browser (http://genome.ucsc.edu). The gene expression was calculated using the RPKM method.
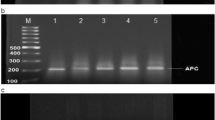
RT-PCR and quantitative real-time PCR
Total RNAs were extracted from cultured cells with TRIzol (Life Technologies, Shanghai, China), and reverse transcription of purified RNA was performed using PrimeScript™ RT Reagent Kit according to the manufacturer’s instructions (TaKaRa, Shanghai, China). Quantification of all gene transcripts was performed by quantitative PCR using the SYBR Premix Kit (TaKaRa, Shanghai, China) and a LightCycler® 480II apparatus (Roche Diagnostics, Mannheim, Germany).
Target gene assay
The primer pairs used for target genes are as follows: human Fos 5′-GTGGCTTCCCTTGATCTGACTG-3′ and 5′-AACAGGAAGTCATCAAAGGGCT-3′, human FosB 5′-CTGCAAGATCCCCTACGAAGAG-3′ and 5′-TGTAAAGAGAGAAGCCGTCAGG-3′, human NR4A1 5′-CCTCCAGCCTTCTTTTCCTTCA-3′ and 5′-GTCACGGGTGTATCCAGTATCC-3′, human EGR1 5′-CTTCGCTAACCCCTCTGTCTAC-3′ and 5′-GTTTGATGAGCTGGGACTGGTA-3′, and human β-actin 5′-AGCCTCGCCTTTGCCGATCC-3′ and 5′-ACCATCACGCCCTGGTGCCT-3′. The gene expressions were all normalized by β-actin.
Statistical analysis
Data were expressed as mean ± SD. The significance of differences between two groups was analyzed using two-tailed Student’s t tests. P values <0.05 were considered to indicate statistical significance.
Results
GABA decreases colon cancer cell proliferation in vitro
Based on reports of opposing biofunctions of GABA on colon cancer, we examined the effect of GABA on colon cancer cell (CCC) proliferation. A phase-contrast microscopy assay showed no obvious changes in the morphology of CCCs treated with GABA (Fig. 1a). However, GABA did significantly slow cell proliferation in a time- and dose-dependent manner (Fig. 1b).
GABA inhibits proliferation of human colon cancer cells. a Images observed under a Olympus IX73 Phase Contrast Microscope (Olympus Corporation, Tokyo, Japan) showing the morphology of cells incubated with or without GABA for 72 h. Cells in the GABA-treated group were exposed to 100 μM (SW480, SW620) or 400 μM (HCT116) GABA. b Cell growth curves of CCCs treated with or without GABA at the indicated concentration for 72 h. The relative number of cells at the indicated time points was determined by the CCK-8 assay, with optical density (OD) measurement at 450 nm. The data are presented as the mean ± SD of quadruplicate samples from one experiment that is a representative of three independent assays. *P < 0.05, **P < 0.01 vs the Ctrl group without GABA treatment
GABA inhibits tumor formation in nude mice
To further confirm the inhibitory effects of GABA on CCC proliferation, SW480 cells were used as a representative cell line to establish a nude mouse model-bearing human colon cancer cells. Compared with mice injected intraperitoneally with distilled water, GABA-treated mice exhibited a much slower rate of tumor growth (Fig. 2).
GABA exhibits anti-tumor activity in a xenograft nude mouse model. a BALB/c mice bearing tumors on 20th day after subcutaneous injection of SW480 cells. SW480 cells were counted and then subcutaneously injected into BALB/c mice (4 × 106 cells/mouse). GABA was dissolved in sterile water and injected intraperitoneally at the dose of 2.5 g/kg from the 6th day (when the average tumor volume was approximately 10–13 mm3), once every 2 days. In the control group, the mice were injected intraperitoneally equal volume of sterile water (100 μL). b Tumors isolated from the corresponding mice in Fig. 2a. c Tumor growth curve. At 8 days after cell injection, the size of tumors was measured every 4 days using vernier calipers. Tumor volume was calculated using the formula V = ab 2 π/6, where “a” represents the length and “b” represents the width. *P < 0.05 vs the Ctrl group. Data shown represent one of two independent experiments
GABA impairs the migration and invasion of SW620 and SW480 cells
In addition to unchecked proliferation, two other characteristic features of malignant cells are the ability to migrate and to invade normal tissues [12, 13]. The capacity of GABA to restrain CCC proliferation led us to examine whether the amino acid could also affect CCC migration and invasion. In order to get the images of all the cells in the whole well, a stereo microscope (Olympus ZX16, Tokyo, Japan) was used to take pictures. Limited by the magnification times of the microscope, cells stained by 0.1 % crystal violet only showed blue dots in the field. However, if observed under the microscope with higher magnification, the migrated/invaded cells could be seen more clearly (Supplementary Fig. 1). We found that compared with a DMEM solvent control group, GABA suppressed the migration activity of both SW480 and SW620 cells during a 24-h period (Fig. 3a, c, e, g), whereas no significant changes in cell migration were observed for HCT116 cells (Fig. 3i, k). Similarly, GABA decreased the invasion ability of both SW480 and SW620 cells but had little impact on HCT116 (Fig. 3b, d, f, h, j, i). These results suggest that GABA possesses the ability to inhibit the metastasis of certain types of CCC lines.
Effects of GABA on CCC migration and invasion. a, e, i Effects of GABA on migration of SW480, SW620, or HCT116 cells. b, f, j Effects of GABA on the invasion of SW480, SW620, and HCT116 cells. In e, f, the shaded parts are magnified on the right, and the migrated/invaded cells were marked by orange arrows. The images shown represent one of two independent experiments. The scale bars are shown. e, d, g, h, k, l Migration/invaded efficacy was represented by relative percentage of migrated/invaded cells, which was calculated by the formula % = 100 × GABA group/Ctrl group, where “Ctrl group” represents the normal culture cells and its migrated/invaded efficacy was defined as 100 %; “GABA group” represents the cells treated with GABA. Data shown in j, f were obtained by cell counting under microscope. While data shown in c, d, g, k were obtained by measuring light absorption. Migration/invaded cells were dissolved in 30 % acetic acid; optical density values at 570 nm (OD 570 nm) were measured by a microplate reader (Multiskan MK3, Thermo Scientific, Shanghai, China). The values represent the mean ± SD of two independent assays. *P ≤ 0.05, **P ≤ 0.01, # P ≥ 0.05 vs the Ctrl group
GABA alters cell cycle distribution
To understand the mechanisms underlying GABA-induced CCC proliferation inhibition, we analyzed changes in cell cycle distribution by flow cytometry. GABA decreased the number of HCT116 cells in G0/G1 phase by a 10 % while increased cell number in G2/M phase by a 30 % (Fig. 4, upper panel). A 30 % increase in G2/M phase indicated that HCT116 cell progression through G2/M phase was retarded. The retardance would directly lead to a decrease production of daughter cells, including the cells in G0/G1 phase. In SW480 and SW620 cells, GABA impeded cell cycle progression at the G1 to S transition because the percentage of cells in G0/G1 increased while the percentage in S decreased (Fig. 4, middle and the lower panels). These data indicate that GABA impairs CCC proliferation perhaps by delaying cell cycle progression through G2/M or G1/S phase. Furthermore, no sub-G1 phase peak, which represents cell death [14], was observed, indicating the failure of GABA to induce cell death and confirming the observation that GABA does not affect cell morphology (Fig. 1a).
GABA affects CCC cycle distribution at 72 h. Both SW480 and SW620 cells were treated with or without 100 μM GABA for 72 h; HCT116 cells were incubated with 400 μM GABA. After fixation, RNA hydrolysis, and DNA staining with PI, the DNA content of the cells was analyzed using a FACSCalibur flow cytometer. a Cell cycle distribution is shown on the left. b The degree to which GABA affected cell cycle distribution. The degree was calculated using the formula effect degree (%) = 100 × (GABA group − Ctrl group)/Ctrl group. The data shown represent one of two independent experiments
Genes differentially expressed in GABA-treated CCC cells
RNA sequencing was performed to further understand the underlying mechanisms by which GABA inhibits CCC proliferation and metastasis. Gene expression profiles were obtained by microarray analysis using Agilent Whole Human Genome Microarray 4 × 44 K, human gene expression arrays with 41,000 probes (Shanghai Biotechnology Co. Ltd., Shanghai, China). After treatment with GABA, 5737 genes were found to be significantly differentially expressed (Fig. 5a), including 30 genes exhibiting different levels of expression in all three types of CCCs (Fig. 5b). Among these 30 genes, 4 closely related to cell proliferation were dramatically down-regulated in GABA-treated cells (Fig. 5c). Consistent with the RNA sequencing results, reduced expression of these four genes was confirmed by real-time quantitative PCR (qPCR) (Fig. 5c, d). The expression of mitogen-activated protein kinase 4 (MAPK4), a member of the mitogen-activated protein kinase (MAPK) family, was also down-regulated in CCC after exposure to GABA (Fig. 5e). Moreover, RNA sequencing revealed reduced expression of MMP-25/MT6-MMP, a member of the matrix metalloproteinase (MMP) family involved in the breakdown of the extracellular matrix in metastasis, in GABA-treated SW480 and SW620 cells but little changes in HCT116 cells (Fig. 5f). These data suggest that GABA may impair CCC metastasis by decreasing MMP25 expression and may inhibit CCC proliferation by down-regulating Fos, FosB, NR4A1, and EGR1 expressions and by attenuating the MAPK signaling pathway.
Differential gene expression induced by GABA in CCCs. RNA sequencing was performed as described in the “Materials and methods” section. a A heatmap showing the differential expression of 5737 genes in response to GABA in CCCs. Genes with fold changes ≥1.5 or ≤−0.25 were counted. b A Venn diagram of the data shown in a. Thirty differentially expressed genes were commonly shared by all three types of CCCs. c A heatmap showing four genes down-regulated in all three types of CCCs treated with GABA. d q-PCR assay for the down-regulated gene expression shown in c. Data represent the mean ± SEM from two independent experiments. e GABA-induced changes in MAPK4 mRNA expression. f GABA-induced changes in MMP25 mRNA expression
Synergistic inhibitory effects of GABA in combination with OXA on colon tumor growth
The observation that GABA inhibits CCC proliferation, migration, and invasion prompted us to evaluate the effects of its combination with chemotherapy drugs. It was observed that GABA significantly enhanced the ability of OXA to suppress tumor growth in nude mice subcutaneously transplanted with SW480 cells (Fig. 6). These data suggest that GABA might be a novel candidate for colon cancer combination therapy.
GABA enhances anti-tumor activity of OXA in a xenograft nude mouse model. The mouse model was established as described in Fig. 2. a BALB/c mice bearing tumors on the 20th day after subcutaneous injection of SW480 cells. OXA was dissolved in sterile water and injected intraperitoneally at the dose of 4 mg/kg, once every 4 days. In the GABA + OXA group, in addition to OXA, the mice were injected intraperitoneally with GABA at the dose of 2.5 g/kg, once every 2 days. b Tumors isolated from the mice in a. c Tumor growth curve. At 8 days after cell injection, the size of tumors was measured every 4 days using vernier calipers. Tumor volume was calculated using the formula V = ab 2 π/6, where “a” represents the length and “b” represents the width. *P < 0.05 vs the mice treated with OXA. The data shown is a representative of two independent experiments
Discussion
GABA is a four-carbon non-protein amino acid, which exists broadly in many plant parts and is also present in human organs and tissues. Besides, the amino acid is widely used as an ingredient in the food industry. It has been reported opposing biofunctions of GABA in the development of various carcinomas. Some studies regard GABA as a tumor-suppressing molecule [8, 15, 16], whereas others consider that it acts as a tumor promoter [17, 18]. In this study, although GABA failed to invoke the death of colon cancer cells, it significantly slowed cell proliferation within 72 h and obviously inhibited tumor growth in BALB/c mice injected subcutaneously with SW480 cells. These data show a tumor-suppressing effect of the molecule on colon cancer.
Several genes that are differentially expressed affect cell growth and proliferation, particularly early growth response gene 1 (EGR1), a transcription factor induced by stress or injury, mitogens, and differentiation factors [19]. Indeed, EGR1 acts as a tumor suppressor in many cell types, and loss of this gene has been proposed to contribute to cancer progression [19, 20]. However, there is a strong new evidence that EGR1 promotes cancer progression; inhibition of EGR1 function via high-affinity and high-specificity anti-sense oligonucleotides blocks cell proliferation and inhibits the transformed phenotype of prostate cancer cells both in vitro and in vivo [19]. Therefore, EGR1 expression results in either the promotion or repression of cell proliferation depending on the cell type and environment [19]. In the present study, EGR1 expression was significantly down-regulated during GABA-induced CCC growth inhibition, suggesting a tumor-promoting effect of the gene on CCCs. Liao et al. reported that EGR1 transcription was not induced in HEK293T cells lacking endogenous MEK activity; in contrast, over-expression of exogenous constitutively active MEK resulted in increased EGR1 expression in HEK293T and HeLa cells, respectively [21]. These data indicate that MEK activation is required for EGR1 expression. In this study, in addition to reducing EGR1 expression in CCCs, GABA also decreased MAPK4 (ERK4) expression. According to the observations described above and previous reports, our data suggest that GABA inhibits CCC growth, perhaps by disrupting the MEK-EGR1 signaling pathway.
As an important transcription factor, EGR1 directly or indirectly regulates the expression of specific genes, such as transcription-regulating genes NR4A1 (Nur77) and Fos [20]. Similar to the reduced expression of EGR1, the expressions of both NR4A1 and Fos were down-regulated by GABA in proliferation-inhibited CCCs, indicating that the attenuated EGR1-NR4A1 axis and EGR1-Fos axis might contribute to GABA-induced CCC growth inhibition. It has been documented that NR4A1 knockdown blocks renal cell carcinoma proliferation and induces apoptosis [22], whereas another report indicates an opposite effect, with NR4A1 hyperexpression inhibiting the growth and cell cycle progression of UM-UC-3 urinary bladder cancer cells [16]. Consistent with the former, our work revealed GABA-induced inhibition of CCC growth via down-regulation of NR4A1 expression, supporting the colon cancer-promoting effects of NR4A1. In addition to Fos, FosB gene expression was also reduced in GABA-treated CCCs, further supporting the view that both FosB and Fos are associated with increased tumor growth [23, 24].
Altered cell cycle distribution is a major cause of suppressed cell proliferation [25], and EGR1 expression is related to the G0-G1 transition or the mitotic spindle assembly checkpoint in a variety of models of cell proliferation [21]. In our study, we observed an obvious increase in the percentage of cells in G0/G1 and a decrease in S in both SW480 and SW620 cells and a 30 % increase in G2/M and a 10 % decrease in G0/G1 in HCT116 cells showing down-regulated EGR1 expression after GABA treatment. These data suggest that down-regulated EGR1 expression following GABA treatment might delay cell progression through G0/G1 checkpoint and M phase.
In addition to positively regulating cell growth, Fos, FosB, and EGR1 drive tumor cell migration and metastasis [24, 26, 27]. In cultured cells and a mouse xenograft model, RNA-binding protein with multiple splicing 1 (RBPMS1) inhibits the growth and migration of breast cancer cells by inhibiting Fos-mediated AP-1 transactivation [26]; additionally, neurobehavioral stress leads to FosB-driven tumor growth and metastasis in ovarian cancer. Moreover, Li et al. found that once activated, EGR1 translocates to nucleus, which results in breast cancer cell proliferation and migration [27]. In the present work, although Fos, FosB, and EGR1 gene expressions were down-regulated by GABA in all of the three types of CCCs, attenuated cell migration and invasion capacities were observed in SW480 and SW620 cells but not in HCT116 cells, which might be attributed to the different overall effects of the changes in gene expression profiles. For example, MMP25/MT6-MMP is a member of the MMP family of potent proteolytic enzymes and participates in tumor invasion and metastasis by directly converting pro-MMP-2 into its active form [28]. After treatment with GABA, both SW480 and SW620 cells showed a decrease in MMP25 expression, whereas expression of this gene was hardly affected in HCT116 cells. These data indicated that down-regulated Fos, FosB, EGR1, and MMP25 expressions might contribute to the impaired metastasis of both SW480 and SW620 cells.
Polychemotherapy is a preferred approach for maximum and rapid tumor remission in patients with symptomatic or acute life-threatening disease [29]. Given the inhibitory effects of GABA on CCCs and the fact that it is a natural amino acid broadly present in many plant parts and more importantly, the combination of GABA with OXA exhibits a significantly synergistic inhibiting effect on tumor growth in nude mice, we speculate that GABA might represent a promising candidate for colon cancer polychemotherapy.
Taken together, although GABA has been reported to have opposing biofunctions in various carcinomas, the present work shows colon cancer-suppressing function of this amino acid perhaps by down-regulating EGR1, NR4A1, Fos, FosB, and MAPK4 gene expressions. Attenuated EGR1-NR4A1 axis, EGR1-Fos axis, and disrupted MEK-EGR1 signaling pathway might contribute to proliferation inhibitory effects of GABA. These findings reveal the pharmacological value of GABA derived from food and suggest that exogenous GABA might play an auxiliary role in polychemotherapy of colon cancer.
References
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300.
Jin K, Gao W, Lu Y, Lan H, Teng L, Cao F. Mechanisms regulating colon cancer cell metastasis into liver (review. Oncol Lett. 2012;3:11–5.
Stefanska B, Karlic H, Varga F, Fabianowska-Majewska K, Haslberger A. Epigenetic mechanisms in anti-cancer actions of bioactive food components—the implications in cancer prevention. Br J Pharmacol. 2012;167:279–97.
Al-Wadei HA, Ullah MF, Al-Wadei M. GABA (gamma-aminobutyric acid), a non-protein amino acid counters the beta-adrenergic cascade-activated oncogenic signaling in pancreatic cancer: a review of experimental evidence. Mol Nutr Food Res. 2011;55:1745–58.
Ippolito JE, Piwnica-Worms DA. Fluorescence-coupled assay for gamma aminobutyric acid (GABA) reveals metabolic stress-induced modulation of GABA content in neuroendocrine cancer. PLoS One. 2014;9:e88667.
Kim JI, Ganesan S, Luo SX, Wu YW, Park E, Huang EJ, et al. Aldehyde dehydrogenase 1a1 mediates a GABA synthesis pathway in midbrain dopaminergic neurons. Science. 2015;350:102–6.
Hackett CS, Quigley DA, Wong RA, Chen J, Cheng C, Song YK, et al. Expression quantitative trait loci and receptor pharmacology implicate Arg1 and the GABA-A receptor as therapeutic targets in neuroblastoma. Cell Rep. 2014;9:1034–46.
Zhang X, Zhang R, Zheng Y, Shen J, Xiao D, Li J, et al. Expression of gamma-aminobutyric acid receptors on neoplastic growth and prediction of prognosis in non-small cell lung cancer. J Transl Med. 2013;11:102.
Joseph J, Niggemann B, Zaenker KS, Entschladen F. The neurotransmitter gamma-aminobutyric acid is an inhibitory regulator for the migration of SW 480 colon carcinoma cells. Cancer Res. 2002;62:6467–9.
Kleinrok Z, Matuszek M, Jesipowicz J, Matuszek B, Opolski A, Radzikowski C. GABA content and GAD activity in colon tumors taken from patients with colon cancer or from xenografted human colon cancer cells growing as s.C. Tumors in athymic nu/nu mice. J Physiol Pharmacol. 1998;49:303–10.
Yan H, G Tang, H Wang, L Hao, T He, X Sun, et al. DNA methylation reactivates GAD1 expression in cancer by preventing CTCF-mediated polycomb repressive complex 2 recruitment. Oncogene. 2015.
Du AY, Zhao BX, Yin DL, Zhang SL, Miao JY. Discovery of a novel small molecule, 1-ethoxy-3-(3,4-methylenedioxyphenyl)-2-propanol, that induces apoptosis in A549 human lung cancer cells. Bioorg Med Chem. 2005;13:4176–83.
Mareel M, Oliveira MJ, Madani I. Cancer invasion and metastasis: interacting ecosystems. Virchows Arch. 2009;454:599–622.
Qian L, Murakami T, Kimura Y, Takahashi M, Okita K, Saikosaponin A. Induced cell death of a human hepatoma cell line (HuH-7): the significance of the “sub-G1 peak” in a DNA histogram. Pathol Int. 1995;45:207–14.
Tian H, Wu JX, Shan FX, Zhang SN, Cheng Q, Zheng JN, et al. Gamma-aminobutyric acid induces tumor cells apoptosis via GABABR1.Beta-arrestins.JNKs signaling module. Cell Biochem Biophys. 2015;71:679–88.
Wu J, Liu J, Jia R, Song H. Nur77 inhibits androgen-induced bladder cancer growth. Cancer Investig. 2013;31:654–60.
Li YH, Liu Y, Li YD, Liu YH, Li F, Ju Q, et al. GABA stimulates human hepatocellular carcinoma growth through overexpressed GABAA receptor theta subunit. World J Gastroenterol. 2012;18:2704–11.
Zhang D, Li X, Yao Z, Wei C, Ning N, Li J. GABAergic signaling facilitates breast cancer metastasis by promoting ERK1/2-dependent phosphorylation. Cancer Lett. 2014;348:100–8.
Baron V, Duss S, Rhim J, Mercola D. Antisense to the early growth response-1 gene (Egr-1) inhibits prostate tumor development in TRAMP mice. Ann N Y Acad Sci. 2003;1002:197–216.
Zhang H, Chen X, Wang J, Guang W, Han W, Zhang H, et al. EGR1 decreases the malignancy of human non-small cell lung carcinoma by regulating KRT18 expression. Sci Rep. 2014;4:5416.
Liao Y, Shikapwashya ON, Shteyer E, Dieckgraefe BK, Hruz PW, Rudnick DA. Delayed hepatocellular mitotic progression and impaired liver regeneration in early growth response-1-deficient mice. J Biol Chem. 2004;279:43107–16.
Hedrick E, Lee SO, Kim G, Abdelrahim M, Jin UH, Safe S, et al. Nuclear receptor 4A1 (NR4A1) as a drug target for renal cell adenocarcinoma. PLoS One. 2015;10:e0128308.
Lu C, Shen Q, DuPre E, Kim H, Hilsenbeck S, Brown PH. cFos is critical for MCF-7 breast cancer cell growth. Oncogene. 2005;24:6516–24.
Shahzad MM, Arevalo JM, Armaiz-Pena GN, Lu C, Stone RL, Moreno-Smith M, et al. Stress effects on FosB- and interleukin-8 (IL8)-driven ovarian cancer growth and metastasis. J Biol Chem. 2010;285:35462–70.
Long XE, Gong ZH, Pan L, Zhong ZW, Le YP, Liu Q, et al. Suppression of CDK2 expression by siRNA induces cell cycle arrest and cell proliferation inhibition in human cancer cells. BMB Rep. 2010;43:291–6.
Fu J, Cheng L, Wang Y, Yuan P, Xu X, Ding L, et al. The RNA-binding protein RBPMS1 represses AP-1 signaling and regulates breast cancer cell proliferation and migration. Biochim Biophys Acta. 2015;1853:1–13.
Li D, Ilnytskyy Y, Kovalchuk A, Khachigian LM, Bronson RT, Wang B, et al. Crucial role for early growth response-1 in the transcriptional regulation of miR-20b in breast cancer. Oncotarget. 2013;4:1373–87.
Nie J, Pei D. Direct activation of pro-matrix metalloproteinase-2 by leukolysin/membrane-type 6 matrix metalloproteinase/matrix metalloproteinase 25 at the asn(109)-Tyr bond. Cancer Res. 2003;63:6758–62.
Huober JB. Thurlimann. The role of combination chemotherapy in the treatment of patients with metastatic breast cancer. Breast Care (Basel). 2009;4:367–72.
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (Grant Nos. 81071680 and 81272280), Shanghai Pujiang Outstanding Young Scientist Project.
Author information
Authors and Affiliations
Corresponding author
Additional information
Lihua Song, Aiying Du,·and Ying Xiong contributed equally to this work.
Electronic supplementary material
Supplementary Fig. 1
Images showing the morphology of migrated or invaded SW620 cells. SW620 cells were planted in the wells of 24-well Transwell chambers and treated with GABA as described in the “Materials and methods” section. Twenty-four hours after treatment, images were obtained by using under an Olympus IX73 Phase Contrast Microscope (Olympus Corporation, Tokyo, Japan). Images in the left panel (a, c, e, g) were magnified on the right (b, d, f, h), respectively. Scale bar 1 mm (DOCX 294 kb)
Rights and permissions
About this article
Cite this article
Song, L., Du, A., Xiong, Y. et al. γ-Aminobutyric acid inhibits the proliferation and increases oxaliplatin sensitivity in human colon cancer cells. Tumor Biol. 37, 14885–14894 (2016). https://doi.org/10.1007/s13277-016-5367-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-016-5367-5