Abstract
Recently, microRNAs (miRNAs), a kind of small and non-coding RNA, can target the downstream molecules. Increasing evidence demonstrates that miRNAs meditate the onset and progression of a variety of tumors. In the present study, we carried out gene transfection, western blot, and reverse transcription PCR (RT-PCR) to explore the role of miR-22 in glioblastoma tissues and cell lines. Here, we verified that the expression of miR-22 was downregulated in glioblastoma tissues and cells rather than matched non-tumor tissues and normal human astrocyte (NHA) cells (p < 0.001). By contrast, SIRT1 messenger RNA (mRNA) and protein were upregulated in glioblastoma tissues and cells (p < 0.001). In vitro miR-22 mimics interfered with cell proliferation, migration, and invasion of U87 and U251 cells. Mechanically, the 3′-untranslated regions (3′-UTRs) of SIRT1 were a direct target of miR-22, leading to the decreased expression of SIRT1 protein in U87 and U251 cells. Meanwhile, miR-22 mimics also inhibited the expression of epidermal growth factor receptor (EGFR) and matrix metallopeptidase 9 (MMP9). In conclusion, miR-22 inhibited cell proliferation, migration, and invasion via targeting the 3′-UTR of SIRT1 in the progression of glioblastoma and miR-22-SIRT1 pathway can be recommended as a potential target for treatment of glioblastoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma multiforme (GBM) is the most frequent primary tumor in the central nervous system, and patients with malignant glioma have a very poor prognosis. Unfortunately, there are no well-established methods to inhibit cell growth in glioma cells [1, 2]. Currently, GBM is still being treated by means of radical surgery followed by radiotherapy and chemotherapy. It appears that the conventional drugs, such as temozolomide, have therapeutic benefits in prolonging the survival of GBM patients. Targeted therapies against a genetic anomaly using specific small molecule inhibitors are now in clinical trials. Although some of them are showing promising results [3–6], multiple genetic changes in GBM suggest that a single drug is unlikely to offer effective and complete solution to the problem.
MicroRNAs (miRNAs) are a recently discovered category of small (19 ~ 24 nucleotides), non-protein-coding, and single-stranded endogenous RNA molecules [7]. miRNAs function as regulators of approximately 60 % of protein-coding gene expression mainly at the post-transcriptional level by binding to the sequences in the 3′-untranslated region (3′-UTR) of their targeted messenger RNAs (mRNAs), resulting in translational repression or gene silencing [8]. As they are involved in the regulation of a wide array of biological processes including cell proliferation, differentiation, apoptosis, metastasis, angiogenesis, and immune response, miRNAs have been considered to be new approaches of tumor biomarkers for early cancer diagnosis and prognosis [9–12]. According to our literature retrieval, miR-22 has been demonstrated to play important roles in different types of cancer, such as hepatocellular carcinoma, breast cancer, colon cancer, lung cancer, and prostate cancer, and plays an essential role in a couple of oncogenesis, including survival, growth, apoptosis, migration, and metastasis [13, 14]. However, its roles in tumorigenesis of glioblastoma are still unknown.
In the present study, we investigated the expression level of miR-22/SIRT1 on the proliferation, migration, and invasion in glioblastoma cells in vitro and characterized its anticancer effects. We also evaluated whether there is objective evidence that miR-22/SIRT1 would be potential targets for glioblastoma therapy.
Materials and methods
Patients and tissues
Fifteen cases of GBM specimens were obtained from patients during surgery at the Suzhou Kowloon Hospital, Shanghai Jiao Tong University School of Medicine. A portion of the tumor tissues were saved and made into paraffin sections for histopathologic diagnosis in strict accordance with the World Health Organization (WHO) criteria by two established neuropathologists, with differences resolved by careful discussion, and the remaining tissue was snap frozen in liquid nitrogen and then stored at −80 °C for RNA extraction and other biological molecular experiments. Before the RNA extraction from frozen tissues, the adjacent tumor tissues were subjected to frozen sections and reviewed by a pathologist to ensure that a minimum of 80 % tumor cells were included in the sample. For GBM patients, none of them had received chemotherapy or radiotherapy prior to surgery and all patients were well followed up. Patients, who died of diseases not directly related to their gliomas or due to unexpected events, were excluded from this study. The present study was approved by the Ethics Committee of Shanghai Jiao Tong University School of Medicine.
Cell culture
As cell culture, primary normal human astrocytes (NHAs) were purchased from the Sciencell Research Laboratories (Carlsbad, CA, USA) and cultured under the conditions as instructed by the manufacturer. Cell lines U87 and U251 were obtained from the KeyGen Company (China) and cultured in Dulbecco’s modified Eagle’s medium (DMEM), with 10 % fetal bovine serum (Gibco, Grand Island, NY, USA) and 1 % penicillin-streptomycin (Gibco, Grand Island, NY, USA) at 37 °C in a humidified atmosphere under 5 % CO2. The medium was replaced every 3 days.
Transient transfection of miR-22 oligonucleotides
Cells were transiently transfected with 50 nmol of the miR-22 mimic with Lipofectamine 2000 (Invitrogen) according to the manufacturer’s recommendation. The antisense oligonucleotides used in these studies were the miR-22 stem loop primer for complementary DNA (cDNA) (5′-CTCAACTGGTGTCGTGGAGTCGG-3′ and 5′-CAATTCAGTTGAGACAGTTCT-3′) and the miRNA mimic-negative control (NC mimic) (5′-UUCUCCGAACGUGUCACGUTT-3′ and 5′-ACGUGACACGUUCGGAGAATT-3′). All miRNA oligonucleotides were purchased from GenePharma (Shanghai, China).
Reverse transcription PCR analysis
Reverse transcription PCR and immunoblotting
Total RNAs were isolated from the cells using TRIzol reagent (TaKaRa, Japan). The sequences of primers used in this study were the following:
SIRT1
Forward: 5′-ATCTGACTTTGCTCCCCTTAACC-3′
Reverse: 5′-GGGCCCTGGTTGCAAGA-3′
NAPDH
Forward: 5′-CAATGACCCCTTCATTGACC-3′
Reverse: 5′-GACAAGCTTCCCGTTCTCAG-3′
Total RNA (1 μg) was reversely transcribed into cDNA using a QuantScript RT Kit (Tiangen, China). PCR was performed using a PCR Master Mix Kit (BioTeke, China) in a GeneAmp PCR System 9600 (ABI International). cDNA was amplified under the thermocycling conditions as follows: 3-min initial denaturation at 94 °C (1 cycle), 30-s denaturation at 94 °C (35 cycles), annealing at 57 °C for 30 s, and extension at 72 °C for 45 s. The last amplification was followed by final 7-min incubation at 72 °C. PCR products were separated by electrophoresis through 1 % agarose gel, stained with ethidium bromide, and visualized by UV transillumination in a Tocan Gel Imaging System (Tocan Co., Shanghai, China). NAPDH was used as an internal control. The mRNA level was calculated by determining the integrated intensity of the bands of each treated group as a ratio of the control. Each sample was measured in triplicate. Reverse transcription PCR (RT-PCR) for miR-22 was performed using real-time PCR Universal Reagent (GenePharma). U6 was used as an internal control.
Western blot analysis
For the protein analysis, the cells were harvested at 12~24 h following different treatments, as described above, and washed with cold PBS and then incubated in ice-cold RIPA buffer. Cell lysates were sonicated for 30 s on ice and lysed at 4 °C for 60 min. Then, the cell lysates were centrifuged at 12,000g for 30 min at 4 °C. Protein concentrations in the supernatants were determined using the BCA reagent. Total protein was separated by denaturing 8–12 % SDS-polyacrylamide gel electrophoresis, which was resolved over and electrotransferred by semidry blotting (Bio-Rad Laboratories, Shanghai) onto a nitrocellulose membrane. The membrane was incubated with antibodies SIRT1 (Abcam, Cambridge, UK; 1:1000 dilution) or β-actin (Santa Cruz Biotech, Santa Cruz, CA, USA; 1:1000 dilution) overnight at 4 °C and then with peroxidase-conjugated secondary antibody (Santa Cruz Biotech, Santa Cruz, CA, USA; 1:1000 dilution) and was visualized by chemiluminescence (GE, Fairfield, CT, USA).
Cell proliferation assay
Cells were seeded at 2000 per well in 96-well plates and cultured after transfection. Cell proliferation was detected at the indicated time points using Cell Counting Kit-8 (CCK-8) (Dojindo Laboratories) following the manufacturer’s instructions. All assays were performed in octuplicate and repeated at least three times.
Wound healing assay
Cells were seeded in 12-well plates and grown to 90 % confluence. Cells were transfected with or without NC miRNAs or miR-22 mimics. After 36 h of transfection, the cells were serum starved overnight and a linear wound was created using a pipette tip. Wound closure was monitored by live cell imaging microscopy at an interval of 30 min for 24–48 h. Wound size was then measured randomly at three sites perpendicular to the wound.
Transwell invasion assays
As for transwell assay, we seeded cells on the upper chamber of each insert and then 500 μl of DMEM (10 % FBS) was added to a 24-well plate for 12-h incubation at 37 °C; the cells on the lower layer were collected and fixed with a 0.1 % crystal violet. As for invasion assay, transwell chambers were uniformly plated with 60 μl Matrigel diluted with DMEM and then incubated for 4 h at 37 °C and then the same procedures with migration assay were conducted.
Luciferase reporter assay
A dual-luciferase reporter vector was used to generate the luciferase constructs. The target genes of miR-22 were selected based on target scan algorithms [microRNA.org (http://www.microrna.org/microrna/home.do), Microcosm (http://www.ebi.ac.uk/enright-srv/microcosm/htdocs/targets/), and TargetScan (http://www.targetscan.org/)]. For 3′-UTR luciferase assay, the putative binding sites of miR-22 and its homologous mutation sites in the 3′-UTR region of SIRT1 mRNA were amplified and cloned into pGL3 control luciferase reporter plasmid (Invitrogen, Carlsbad, CA, USA). The pRL vector constitutively expressing Renilla luciferase was used to normalize for transfection efficiency. Luciferase activity was measured using the Dual-Luciferase Reporter Assay System (Promega, Madison, USA) after transfection at 48 h. Data are presented as the mean value ± standard deviations (SDs) for triplicate experiments.
Statistical analysis
Significance was determined using the one-way ANOVA test on the mean values of three different experiments. Significance was determined using the mean ± SD and analyzed using two-tailed Student’s t tests using the Statistical Program for Social Sciences 13.0 software (SPSS Corp., Shanghai, China). p < 0.05 was used as the cutoff for statistically significant differences. In the western blotting analysis, the corresponding strips used to estimate the value of the relative protein content were captured photographically through a Bio-Rad image analysis system with Image-Pro software analysis.
Results
The expression profile of miR-22 and SIRT1 in glioblastoma tissues
In the present study, we tested the expression of miR-22 and SIRT1 in 15 paired tumor and adjacent non-tumor tissue samples and we observed that the expression of miR-22 in tumor tissues was significantly higher than that in matched non-tumor tissues (p < 0.001) (Fig. 1a). On the other hand, the expression of SIRT1 mRNA was obviously increased in tumor tissues than that in matched non-tumor tissues (p < 0.001) (Fig. 1b). Accordingly, the expression of SIRT1 protein was also significantly upregulated in tumors than that in non-tumor tissues (p < 0.001) (Fig. 1c). Generally, the mean optical intensity of SIRT1 mRNA and protein bands in all 15 tissues is 0.89 ± 0.11 and 1.12 ± 0.23, respectively, compared with that in non-tumors (0.31 ± 0.06 and 0.34 ± 0.07, respectively).
The expression profile of miR-22 and SIRT1 in glioblastoma tissues. a, b The RT-PCR analysis of miR-22 and SIRT1 mRNA expression was conducted in tumor tissues and matched non-tumor tissues. Quantification analysis was defined as the relative density of miR-22 and SIRT1 mRNA to U6 and NAPDH, respectively. U6 or NAPDH was used as an internal control. Results shown are the mean ± SD of repeated independent experiments. *p < 0.001, compared with normal tissues, one-way ANOVA. c The expression of SIRT1 protein was examined in tumor tissues and matched non-tumor tissues using western blot. The average SIRT1 protein expression was normalized to β-actin. Results shown are the mean ± SD of repeated independent experiments. *p < 0.001, compared with normal tissues, one-way ANOVA
The expression profile of miR-22 and SIRT1 in glioblastoma cell lines
To further understand the function of miR-22 in the development of glioblastoma cells, we detected the expression of miR-22 and SIRT1 in glioblastoma U87 and U251 cell lines. In this work, total RNA was extracted from differentially treated cells and then the miR-22 and SIRT1 expression levels were subjected to RT-PCR assay. Our findings showed that the expression level of miR-22 was seriously downregulated in U87 and U251 cells whereas its expression was obviously upregulated in sham NHA cells (p < 0.001) (Fig. 2a). Likewise, the expression of SIRT1 mRNA was obviously increased in U87 and U251 cells rather than in NHA cells (p < 0.001) (Fig. 2b). Furthermore, the expression of SIRT1 protein was also upregulated in U87 and U251 cells, when compared with NHA cells (p < 0.001) (Fig. 2c).
The expression profile of miR-22 and SIRT1 in glioblastoma cell lines. a, b RT-PCR analysis of miR-22 and SIRT1 expression in glioblastoma U87 and U251 cell lines. Quantification analysis was defined as the relative density of miR-22 and SIRT1 mRNA to U6 and NAPDH, respectively. U6 or NAPDH was used as an internal control. Results shown are the mean ± SD of repeated independent experiments. *p < 0.001, compared with NHA cells, one-way ANOVA. c The expression of SIRT1 protein was examined in glioblastoma cell lines U87 and U251 using western blot. The SIRT1 expression was normalized to β-actin expression. Results shown are the mean ± SD of repeated independent experiments. *p < 0.001, compared with NHA cells, one-way ANOVA
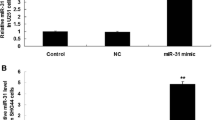
Effects of miR-22 expression on cell proliferation in glioblastoma
To figure out the effect of miR-22 on glioblastoma cell proliferation, U87 and U251 cells were transfected with miR-22 mimic or NC miRNA and then subjected to the CCK-8 assay. Our findings showed that miR-22 mimics obviously decreased the number of viable cells in U87 and U251 cells compared with the NC control (p < 0.001) (Fig. 3a), indicating that cell proliferation was significantly repressed due to the overexpression of miR-22. Using western blot, we evaluated cell proliferation-related protein epidermal growth factor receptor (EGFR). Consistently, we observed that the expression of EGFR protein was decreased in U87 and U251 cells transfected with miR-22, compared with NC mRNA transfection (p < 0.001) (Fig. 3b). These findings suggested that miR-22 inhibited cell proliferation in glioblastoma.
miR-22 inhibits glioblastoma cell proliferation. a Cell proliferation was measured using a CCK-8 assay. U87 and U251 cells were transfected with miR-22 mimics or scramble control miRNAs. b Relative EGFR expression in U87 and U251 cells was measured after the cells were transfected with miR-22 mimics or NC miRNA using western blot. Results shown are the mean ± SD of repeated independent experiments. *p < 0.001, compared with NC miRNAs, one-way ANOVA
Effects of miR-22 expression on cell migration and invasion in glioblastoma
To elucidate the impact of miR-22 on cell migration and invasion, our team conducted the wound healing and transwell assays on U87 and U251 cells transfected with miR-22 mimics or with NC miRNAs. The wound healing assay revealed that miR-22 was able to affect cell migration in U87 and U251 cells, compared with NC miRNAs (p < 0.001) (Fig. 4a). In the transwell assay, increased miR-22 expression could reduce cell invasion in U87 and U251 cell lines, compared with NC miRNAs (p < 0.001) (Fig. 4b). Mechanically, we used western blot to assess the molecular mechanisms of cell invasion and found that the expression of matrix metallopeptidase 9 (MMP9) protein in U87 and U251 cells transfected with miR-22 was decreased whereas its expression was increased in the NC miRNA-treated cells (p < 0.001) (Fig. 4c). These findings suggested that miR-22 exerts the inhibitory effects on cell migration and invasion in glioblastoma.
miR-22 reduces glioblastoma cell invasion. a Wound healing assay performed with U87 and U251 cells over 48 h. Cells and wounds were pretreated as described in the text. Wound healing within the scrape line was recorded every day. Representative scrape lines are shown at day 3; dashed line indicates the margin of the scratch at day 1. b Representative fields (×10 magnification) showing invasive cells after 24-h culture in Matrigel invasion chambers. The panels show U87 and U251 cell invasion after transfection with miR-22 mimics or NC miRNAs. Quantitative analysis of cell invasion experiments demonstrates that miR-22 decreases U87 and U251 glioma cell invasion compared to NC miRNA (*p < 0.001, vs. NC miRNA control). c Relative MMP9 expressions in U87 and U251 cells were measured after the cells were transfected with miR-22 mimics or NC miRNA using western blot. Results shown are the mean ± SD of repeated independent experiments. *p < 0.001, compared with NC miRNAs, one-way ANOVA
The 3′-UTR of SIRT1 is a direct target of miR-22
In the present study, miR-22 directly targets and inhibits SIRT1 using three miRNA databases. Furthermore, we identified a putative miR-22 binding site located in the 3′-UTR of SIRT1 mRNA. In order to validate the relationship between miR-22 and SIRT1, we analyzed the TCGA dataset and found that the inverse correlation between miR-22 and SIRT1 was obviously significant (p < 0.0001). To confirm whether miR-22 directly binds to the 3′-UTR of SIRT1 mRNA, we cloned a full-length 3′-UTR (wild type/mutant (wt/mut)) of SIRT1 mRNA and inserted it into a luciferase reporter vector with downstream from the firefly luciferase gene. SIRT1 protein level was also measured in the cell lines using the western blot. We found that the overexpression of miR-22 reduced the luciferase activity of SIRT1-3′-UTR-wt in a consistent and dose-dependent manner (Fig. 5a). However, transfection of the miR-22 did not decrease the luciferase activity of SIRT1-3′-UTR-mut (Fig. 5b). Our analyses showed that the expression of SIRT1 protein was declined in the miR-22-transfected 3′-UTR-wt cell lines compared to the negative controls; however, the expression of SIRT1 protein in the miR-22-transfected 3′-UTR-mut cell lines showed the same expression model with its negative control. These findings indicated that the 3′-UTR of SIRT1 is a direct miR-22 target, by which miR-22 affected the expression of SIRT1, leading to loss of cell function.
SIRT1 is a candidate target of miR-22. Western blot analysis was performed to detect SIRT1 protein expression in U87 and U251 cells transfected with miR-22 mimics or NC miRNAs. a The miR-22 mimic inhibited the luciferase activity controlled by wild-type SIRT1-3′-UTR (a) but did not affect the luciferase activity controlled by mutant SIRT1-3′-UTR (b) in U87 and U251 cells. The mean SIRT1 protein expression was normalized to β-actin. Results shown are the mean ± SD of repeated independent experiments. *p < 0.001, compared with control, one-way ANOVA
Discussion
SIRT1 affects a variety of biological functions, including DNA repair, energy metabolism, tumor suppression, and mitochondrial homeostasis. These effects have been linked to cell behaviors, involving cell growth, differentiation, migration, and survival. To date, the expression and role of SIRT1 have been under investigation and its expression has been identified in various tumors, including breast cancer and liver cancer [15–17]. As reported, the downregulation of miRNAs can trigger oncogenesis via regulating oncogenes or silencing tumor suppressor genes. miR-22 is downregulated in human pancreatic adenocarcinoma and ampullary adenocarcinoma [18]. In the context of glioblastoma, the aberrant expression of specific miRNAs are closely associated with tumor cell proliferation, migration, and invasion by targeting proteins involved in these cellular functions. However, the expression and the role of miR-22 in glioblastoma have not been clearly demonstrated.
Our sample analysis identified that the expression of miR-22 was lower in tumors than in matched non-tumor tissues. By contrast, the mRNA and protein of SIRT1 showed much higher expression in tumor tissues than those matched non-tumor tissues. These findings were in agreement with previous findings, which demonstrated that miR-22 is downregulated in human breast cancer [18]. In vitro assays suggested that miR-22 plays an obviously suppressive role in tumor cell proliferation, migration, and invasion. Our bioinformatic analysis and cell culture experiments further indicate that the tumor-suppressing effects of miR-22 were mediated through its downregulation of SIRT1 translation. To our knowledge, this is the first study to demonstrate the post-transcriptional regulation of SIRT1 by miR-22 in glioblastoma.
Recent data suggest that increased expression of epidermal growth factor (EGF) and its receptor EGFR in the gastric mucosa may induce changes in gastric epithelial cells, leading to tumorigenesis [19, 20]. EGF, through interaction with its receptor, stimulates the cell proliferation and migration and triggers epithelial cell signaling [21]. Besides, matrix metalloproteinases are secreted during the growth, invasion, metastases, and angiogenesis of tumors and can affect the surrounding microenvironment, causing dynamic changes of biological behaviors of the tumor [22–25]. However, the precise molecular mechanisms between EGFR and MMP9 in the cellular malignant and invasive phenotypes are not fully understood. In the present study, we found that cells transfected with miR-22 decreased the expression of EGFR protein while the NC miRNAs unaffected the expression of EGFR protein, which indeed suggested that miR-22 decreased cell proliferation of glioblastoma. At the same time, we also found that cells transfected with miR-22 decreased the expression of MMP9 protein whereas the NC miRNAs promoted the expression of MMP9 protein. These results indicated that miR-22 expression exerts the inhibitory effects on cell migration and invasion in glioblastoma.
In conclusion, this study suggested that the expression of miR-22 and SIRT1 may be predictive of worse clinical outcome in patients with glioblastoma. Our findings also highlight the therapeutic potential of miR-22/SIRT1 pathway in glioblastoma patients and support the development of effective therapeutic strategies that target miR-22 or SIRT1 using a pharmacological approach.
References
Jemal A, Siegel R, Xu J. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300.
Liao A, Shi R, Jiang Y, Tian S, Li P, Song F, et al. SDF-1/CXCR4 axis regulates cell cycle progression and epithelial-mesenchymal transition via up-regulation of survivin in glioblastoma. Mol Neurobiol. 2014 Nov 25.
Lv Q, Zhang J, Yi Y, Huang Y, Wang Y, Wang Y, et al. Proliferating cell nuclear antigen has an association with prognosis and risks factors of cancer patients: a systematic review. Mol Neurobiol. 2015.
Lv B, Yang X, Lv S, Wang L, Fan K, Shi R, et al. CXCR4 signaling induced epithelial-mesenchymal transition by PI3K/AKT and ERK pathways in glioblastoma. Mol Neurobiol. 2015;52(3):1263–8.
Altieri R, Fontanella M, Agnoletti A, Panciani PP, Spena G, Crobeddu E, et al. Role of nitric oxide in glioblastoma therapy: another step to resolve the terrible puzzle? Transl Med UniSa. 2014;12:54–9.
De Paepe A, Vandeneede N, Strens D, Specenier P. The economics of the treatment and follow-up of patients with glioblastoma. Value Health. 2015;18(7):A448.
Kagiya T. MicroRNAs and osteolytic bone metastasis: the roles of microRNAs in tumor-induced osteoclast differentiation. J Clin Med. 2015;4(9):1741–52.
Sanei M, Chen X. Mechanisms of microRNA turnover. Curr Opin Plant Biol. 2015;27:199–206.
Luna-Aguirre CM, de la Luz M-FM, Mar-Aguilar F, Garza-Veloz I, Treviño-Alvarado V, Rojas-Martinez A, et al. Circulating microRNA expression profile in B-cell acute lymphoblastic leukemia. Cancer Biomark. 2015;15(3):299–310.
Sampson VB, Yoo S, Kumar A, Vetter NS, Kolb EA. MicroRNAs and potential targets in osteosarcoma: review. Front Pediatr. 2015;3:69.
Kanda M, Kodera Y. Recent advances in the molecular diagnostics of gastric cancer. World J Gastroenterol. 2015;21(34):9838–52.
Lim LP, Lau NC, Garrett-Engele P, Grimson A, Schelter JM, Castle J, et al. Microarray analysis shows that some microRNAs downregulate large numbers of target mRNAs. Nature. 2005;433(7027):769–73.
Lu W, You R, Yuan X, Yang T, Samuel EL, Marcano DC, et al. The microRNA miR-22 inhibits the histone deacetylase HDAC4 to promote TH17 cell-dependent emphysema. Nat Immunol. 2015;16(11):1185–94.
Yang Q, Jiang W, Zhuang C, Geng Z, Hou C, Huang D, et al. MicroRNA-22 downregulation of galectin-9 influences lymphocyte apoptosis and tumor cell proliferation in liver cancer. Oncol Rep. 2015;34(4):1771–8.
Zhou Y, Zhou Z, Zhang W, Hu X, Wei H, Peng J, et al. SIRT1 inhibits adipogenesis and promotes myogenic differentiation in C3H10T1/2 pluripotent cells by regulating Wnt signaling. Cell Biosci. 2015;5:61.
Maiese K. MicroRNAs and SIRT1: a strategy for stem cell renewal and clinical development? J Transl Sci. 2015;1(3):55–7.
Shuang T, Wang M, Zhou Y, Shi C. Over-expression of Sirt1 contributes to chemoresistance and indicates poor prognosis in serous epithelial ovarian cancer (EOC). Med Oncol. 2015;32(12):260.
Xiong J, Yu D, Wei N, Fu H, Cai T, Huang Y, et al. An estrogen receptor alpha suppressor, microRNA-22, is downregulated in estrogen receptor alpha-positive human breast cancer cell lines and clinical samples. FEBS J. 2010;277:1684–94.
García I, Vizoso F, Andicoechea A, Fernandez P, Suarez C, García-Muñz JL, et al. C-erbB-2 oncoprotein content in gastric cancer and in adjacent mucosa. Int J Biol Markers. 2000;15(3):231–4.
Dan L, Jian D, Na L, Xiaozhong W. Crosstalk between EGFR and integrin affects invasion and proliferation of gastric cancer cell line, SGC7901. Onco Targets Ther. 2012;5:271–7.
Chen W, Zhong X, Wei Y, Liu Y, Yi Q, Zhang G, et al. TGF-β regulates survivin to affect cell cycle and the expression of EGFR and MMP9 in glioblastoma. Mol Neurobiol. 2015.
Kessenbrock K, Plaks V, Werb Z. Matrix metalloproteinases: regulators of the tumor microenvironment. Cell. 2010;141(1):52–67.
Yang X, Lv S, Liu Y, Li D, Shi R, Tang Z, et al. The clinical utility of matrix metalloproteinase 9 in evaluating pathological grade and prognosis of glioma patients: a meta-analysis. Mol Neurobiol. 2015;52(1):38–44.
Kumar B, Koul S, Petersen J, Khandrika L, Hwa JS, Meacham RB, et al. p38 mitogen-activated protein kinase-driven MAPKAPK2 regulates invasion of bladder cancer by modulation of MMP-2 and MMP-9 activity. Cancer Res. 2010;70(2):832–41.
Yao C, Li P, Song H, Song F, Qu Y, Ma X, et al. CXCL12/CXCR4 axis upregulates twist to induce EMT in human glioblastoma. Mol Neurobiol. 2015.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Project No. 81502163 and 31370810). We greatly thank Bo Hong in Department of Neurosurgery, Changhai Hospital, Second Military Medical University (Shanghai, 200433, P.R. China) for valuable suggestions and his fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Hanchun Chen and Qiong Lu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Chen, H., Lu, Q., Fei, X. et al. miR-22 inhibits the proliferation, motility, and invasion of human glioblastoma cells by directly targeting SIRT1. Tumor Biol. 37, 6761–6768 (2016). https://doi.org/10.1007/s13277-015-4575-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4575-8