Abstract
The aim was to analyze quantitative (mitochondrial DNA (mtDNA) content) and qualitative (G10398A polymorphism) mtDNA alterations as well as human papillomavirus (HPV) infection in cervical cancer prognosis. One hundred and twenty-two cases of formalin-fixed paraffin-embedded cervical carcinoma specimens were collected from the Yichang Tumor Hospital and Zhongnan Hospital of Wuhan University in the recent 10 years together with medical records. A quantitative real-time PCR (RT-PCR) was used to determine the copy number of the mitochondrial DNA and HPV expression levels. G10398A polymorphism was determined by PCR-RFLP assay. The overall survival of patients with higher mtDNA content was significantly reduced compared with lower mtDNA content patients (P = 0.029). But there was no difference of prognosis between the mtDNA 10398 A allele and G allele. However, the Kaplan–Meier survival curve illustrated a significantly reduced overall survival in the patients with 10398A plus high mtDNA copy number compared with the other groups (P < 0.05). Although no association between HPV expression level and cervical cancer prognosis was observed, 10398A got increased mtDNA content compared with 10398G (P < 0.05) and 10398G displayed an increased HPV-positive rate compared with 10398A. Furthermore, HPV-18 and mtDNA content were positively related in the younger subgroup (≤45 years) (correlation coefficient = 0.456, P = 0.022). This study indicated that mtDNA content and HPV infection status are associated with cervical cancer prognosis. High mitochondrial DNA content plus 10398 A may be a marker of poor prognosis in cervical cancer. And mtDNA variation may potentially influence the predisposition to HPV infection and cervical carcinogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mitochondria play a central role in cells’ response to environmental stressors not only through energetics and ATP production but also through metabolites generated in the tricarboxylic acid cycle, as well as mitochondria–nuclear signaling related to mitochondria morphology, biogenesis, fission/fusion, mitophagy, apoptosis, and epigenetic regulation [1]. Human mitochondrial DNA (mtDNA) is a 16,569-base pair (bp) double-stranded circular DNA, which encodes 13 core polypeptide subunits of the respiratory chain complexes, two ribosomal RNAs, and a set of 22 transfer RNAs. Unlike nuclear DNA, mtDNA is not protected by histones and has less efficient repair mechanisms, therefore making it particularly susceptible to reactive oxygen species (ROS) and other genotoxic damage [2]. Previous studies indicate that mtDNA alterations (increased or decreased) and mutations are involved in the tumorigenesis of various cancers [3–7].
mtDNA content fluctuates from 102 to 104 copies per cell, and these levels vary across different cell types and tissues [8]. mtDNA content may get significant changes under different internal or external microenvironments, such as altered oxidative stress, aging, immune response activation, and environmental exposures [9]. Furthermore, genomic regions are also reported to possibly harbor genes influencing variations in mtDNA content [10]. In addition, other factors, such as p53, Ras, and p66 (shc), may also modulate mtDNA content [11].
The mechanism of action of mtDNA 10398 loci in tumor formation is not completely clear. Mariola et al. reported that the mtDNA G10398A variant in African–American women with breast cancer provides resistance to apoptosis and promotes metastasis in mice [12]. There was an additional study on cell injury which proposes the following process: complex I damage, ROS induction, and increased ROS damage to various cell components leading to cell death [13]. The precise mechanism of the adverse effect of the 10398A or 10398G allele is not clear, and previous reports have elaborated the association between A10389G polymorphism and cancer risk, but the results are not consistent [12, 14].
Studies on human papillomavirus (HPV) showed that HPV played an important role in cervical cancer [15–18]. The Amerindian haplogroup B2 increases the risk for cervical cancer and enhances the risk conferred by HPV alone by 36 % [19]. Wallace DC’s research showed that the C150T mtDNA polymorphism is significantly associated with HPV infection [20]. A recent report demonstrated that mtDNA copy number increased during cervical cancer development (L-SIL, H-SIL, and cervical cancer) compared with healthy tissues. Increased mtDNA levels harboring a 4997-bp deletion are associated with cell susceptibility to persistent HPV infection and cervical cancer development [21].
Based on this background, in this study, we detected mtDNA mutations (mtDNA copy number and G10398A polymorphism) and HPV infection status in cervical cancer patients to explore the correlations between mtDNA G10398A polymorphism, HPV infection status, clinicopathological parameters, and prognosis. We aimed to find out the relationship between mtDNA and HPV and how they affect cervical cancer prognosis in order to get a marker for the assessment of cervical cancer prognosis.
Materials and methods
Tissues and patients
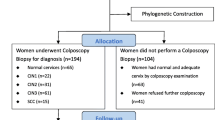
Formalin-fixed paraffin-embedded surgical tissue samples were collected from the Department of Pathology at Zhongnan Hospital of Wuhan University and Yichang Tumor Hospital between December 2002 and December 2014. Clinical stage was assessed according to the FIGO clinical staging criteria. None of the patients received radiotherapy or chemotherapy prior to surgery. Pathological diagnosis was performed cervical according to the World Health Organization 2004 scheme. The study protocol was reviewed and approved by the Institutional Review Board of Zhongnan Hospital of Wuhan University. All participants provided written informed consent to participate in this study. Clinical information, including age, tumor stage (FIGO), pathological type, and clinical follow-up data, was recorded prospectively (Table 1). In addition to a scheduled follow-up examination, patients were assessed at 3-month intervals for up to 2 years and every 6 months for 5 years and then annually thereafter. In total, 122 Han Chinese cases were detected. These patients ranged from 22 to 77 years old, and the mean age was 45 ± 9 years old.
Extraction of total DNA
Total DNA was isolated from paraffin wax specimens according to the manufacturer’s protocol (E.Z.N.A.FFPE DNA Kit). The purity and concentration of DNA were analyzed spectrometrically (UV spectrophotometer) and then stored at −20 °C.
Determination of mtDNA copy number by quantitative real-time PCR
mtDNA content was assessed by quantification of a unique fragment in the NC_012920 human mitochondrial genome region relative to a single-copy region of the nuclear gene β2M using a real-time PCR (RT-PCR) assay (primers in Table 2). RT-PCR was performed using an IQ™ 5 Multicolor RT-PCR Detection System (Bio-Rad). The 25 μl total volume reaction mixture contained 100 ng DNA template (2 μl), 12.5 μl QuantiTect SYBR-Green PCR Master mix (Takara), 0.5 μl of each primer, 0.5 μl ROX Reference Dye II, and 9 μl ddH2O. The following protocol was used: initial “Hot Start” activation step for 5 min at 94 °C followed by 40 cycles of 30 s at 94 °C, 30 s at 60 °C, and 30 s at 72 °C. All of the sample reactions were performed at least in triplicate. To get the mtDNA and nuclear DNA (nDNA) quantities in samples, we obtained the average threshold cycle number (Ct) values of the nDNA and mtDNA from each case. Then, the level of mtDNA was calculated by using the delta Ct (ΔCt) of average mtDNA and nDNA Ct values (ΔCt = CtmtDNA − CtnDNA) in the same well expressed as an exponent of 2 (2ΔCt).
Detection of the 10398 loci
DNA samples were amplified by PCR using primers (Table 2) located between 10,284∼10,306 and 10,484∼10,459 nt followed by digestion with DdeI at 37 °C [22]. Upon resolution of the DdeI-digested products in a 2 % agarose gel, the 10398A allele produces 128- and 73-bp bands, whereas the 10398G allele produces 90-, 73-, and 38-bp bands.
HPV detection
HPV DNA was detected by PCR with consensus primers. To identify the specific HPV type (16 or 18) in the HPV-positive specimens, additional PCR was performed using HPV-16- and HPV-18-specific primers [23]. The HPV-16 and HPV-18 primer pairs were designed from the L1 and E1 regions of the HPV genome, respectively (Table 2). The reaction was performed as follows: enzyme reactivation for 10 min; 35 cycles of 95 °C for 30 s, 62 °C for 30 s, and 68 °C for 30 s; and 72 °C for 5 min.
Quantitative amplification and quantification of the E2 and E6 genes were performed simultaneously in a 96-well PCR plate separately. And in order to provide quality assurance of the quantification system in each reaction, there was one sibling control sample to quantify previously. The numbers of the threshold cycle (Ct) obtained from E2 and E6 PCR reactions were regressed to the standard curve to obtain the HPV copy number. The mean value and standard deviation (SD) were calculated to evaluate triplicate data. Data between the ranges of mean T 1.96 SD were considered acceptable. Multiple negative water blanks were included in every analysis. The reaction was performed in a 25-μl mixture containing 12.5 μl of 2× SYBR Premix Ex Taq, 0.5 μl of each primer (4 pmol, Table 2), 1 μl of template DNA, 0.5 μl of ROX Reference Dye II (50× conc), and 10 μl of ddH2O. The reaction was performed as follows: enzyme reactivation for 10 min followed by 40 cycles of 95 °C for 10 s and 62 °C for 1 min. All of the reactions were performed at least in triplicate.
Statistical analysis
Patients were followed from the date of cervical cancer diagnosis to emigration, death, or end of the study (December 2014), whichever occurred first. Non-parametric statistics (median, range, χ 2 test, t test, and Mann–Whitney or Kruskal–Wallis tests) were used to describe the demographics and clinical and pathological characteristics of the patient population. The Kaplan–Meier product limit method was used to estimate survival outcomes. Univariate and multivariate Cox regression analyses were conducted to adjust for patient and tumor characteristics. The hazard ratios are presented with 95 % confidence intervals (95 % CI). All statistical tests were two sided. The differences were considered significant when P < 0.05. All statistical analyses were performed using the SPSS version 19.0 software.
Results
Higher mtDNA content is associated with poorer prognosis of cervical cancer patients
We analyzed the association between mtDNA content in cervical cancer tissues and traditional clinical parameters (Table 3). However, a significantly different mtDNA content was observed based on patient age (median 1045.59 vs 2470.78, P = 0.019; Table 3 and Fig. 1a), while mtDNA content was not related with either the 10398 allele or HPV status (P = 0.152 and P = 0.118, respectively; Fig. 1b, c). Due to a small number in the subtype, we observed no relationship with tumor type (squamous, adenocarcinoma, adenosquamous) and tumor stage (I, II, III) (Fig. 1d, e). Then, patients were subdivided into two subgroups (high and low mtDNA copy number) according to whether their mtDNA content was above or below the average mtDNA copy number in all 122 patients. The Kaplan–Meier survival curve illustrated that the overall survival (OS) of patients with higher mtDNA content is significantly reduced compared with lower mtDNA content patients (5-year OS 78.18 vs 60.53 %, P = 0.029; 8-year OS 68.18 vs 40 %, P = 0.003; Fig. 2). The above results indicated that patients with low mtDNA content displayed a better prognosis than patients with high mtDNA content.
The distribution of mtDNA content. a Significantly different mtDNA content was observed based on patient age (median 1045.59 vs 2470.78, P = 0.019), b, c while mtDNA content was not related with either the 10398 allele or HPV status (P = 0.152 and P = 0.118, respectively). e, f Due to a small number in the subtype, we observed no relationship with tumor type (squamous, adenocarcinoma, adenosquamous) and tumor stage (I, II, III)
Overall survival. Patients who had a higher mtDNA copy number had poorer 8-year survival than patients with a lower mtDNA copy number when assessed by Kaplan–Meier curves, and the difference was significant (overall survival, 68.23 vs 40.00 %, P = 0.003). 1 = low mtDNA copy number group; 2 = high mtDNA copy number group; their survival rates are 68.18 and 40.00 %. Censored symbols represent patients that were lost to follow-up in this research
G10398A polymorphism was not related with prognosis of cervical cancer patients
Based on electrophoresis results of the 10398 locus mutation, 49 cases displayed an A and 73 cases harbored a G at the site. In this study, we analyzed the associations between the 10398 allele in cervical cancer tissues and traditional clinical parameters (Table 4). We discovered that the 10398 allele was not associated with age (>45, ≤45), but we found significantly different allele distributions according to tumor type (squamous i, adenocarcinoma ii, adenosquamous iii), tumor stage (I, II, III), and follow-up (alive or dead). The mutations in squamous patients were significantly different from those in adenocarcinoma and adenosquamous patients (P < 0.05, Table 4), and the mutations in stage I patients were significantly different from those in stage II and III patients (P < 0.05, Table 4). The mutations in alive patients were significantly different from those in dead patients (P < 0.05, Table 4), whereas no significant differences were observed between different groups by age (>45, ≤45). We subdivided the patients into two subgroups (A and G) based on the 10398 allele. The Kaplan–Meier survival curve illustrated no statistically significant differences between the two groups (5-year OS 74.29 vs 68.57 %, P = 0.683; 8-year OS 60 vs 56.82 %, P = 0.922). So, there was no statistically significant difference of prognosis between the two groups.
Patients with high content of mtDNA and 10398 A had the worst prognosis
The patients were divided into four subgroups based on 10398 site mutations (A or G) and mtDNA content (low or high). The Kaplan–Meier survival curve illustrated a significantly reduced OS in the patients with 10398A plus high mtDNA copy number compared with the other groups (P < 0.05, Fig. 3). These data suggested that high mtDNA content plus an A allele at the 10398 site is associated with the poorest prognosis. Stepwise Cox univariate and multivariate regression analyses indicated significant differences in OS between patients with high or low mtDNA copy number, among patients with different tumor stages and HPV infection status (P < 0.05, Tables 5 and 6). So, there were three parameters which affected prognosis of cervical cancer, and they were mtDNA content, tumor stage, and HPV infection status.
Overall survival. Patients who had a higher mtDNA copy number plus 10398A had the poorest 8-year survival than the other groups when assessed by Kaplan–Meier curves, and the difference was significant (overall survival, overall comparisons P = 0.011). 1 = low mtDNA copy number plus 10398A group; 2 = low mtDNA copy number plus 10398 G group, 3 = high mtDNA copy number plus 10398 A group, 4 = high mtDNA copy number plus 10398 G group; their survival rates are 76.47, 62.96, 25.00, and 47.06 %, respectively. Patients that were lost to follow-up were censored
10398A got increased mtDNA content compared with 10398G
In this study, we divided the patients into two subgroups based on HPV infection status (negative or positive). The Kaplan–Meier survival test indicates no statistically significant differences between the two groups (5-year OS 73.53 vs 69.49 %, P = 0.581; 8-year OS 65.38 vs 53.49 %, P = 0.281). Analyzing the relationship among mtDNA 10398 site mutations, mtDNA content, and HPV infection status, we found that 10398A got increased mtDNA content compared with 10398G (P > 0.05, Table 7), and 10398G displayed an increased HPV-positive rate compared with 10398A (P < 0.05, Table 7). No statistically significant differences in mtDNA content were observed between HPV-positive and HPV-negative individuals (P > 0.05, Table 7). We performed correlation analysis between HPV and mtDNA content and observed that HPV-18 and mtDNA content were positively related in the younger subgroup (≤45 years) (correlation coefficient = 0.456, P = 0.022).
Discussion
For a long time, studies on the mechanisms of tumorigenesis are more concentrated on nuclear gene alterations. Recently, mtDNA mutations (both mtDNA content and mtDNA locus mutation) have been reported in a variety of human tumors [24]. Among those studies, Kabekkodu et al. reported that mitochondrial DNA variation was common in cervical cancer. Seven hundred and thirty-nine variations in malignant cervical cancer tissues were identified distributing in the D-loop, the coding region for tRNA and rRNA genes. Moreover, mtDNA alterations were significantly higher in malignant samples by two-tailed Fisher’s exact test (P ≤ 0.05) [25].
mtDNA content is increased in tissues from patients with head and neck, ovarian, and esophageal cancers, and mtDNA content is decreased in hepatocellular carcinoma (HCC), renal cell carcinoma (RCC), advanced gastric cancer, and breast cancer [26, 27]. Based on this background, it is rational to believe that the role of mtDNA in human cancers is cancer site specific. Mambo et al. [28, 29] reported that alterations in mtDNA content in breast cancer did not correlate with tumor grade and metastasis. Similarly, our study indicates that mtDNA content in cervical cancer is not associated with tumor stage (I, II, III). All of these studies suggest that mtDNA content mutation may occur in the early stages of tumorigenesis. Through stepwise Cox univariate and multivariate regression analyses, we observed that individuals with low mtDNA copy number display higher OS rates. So, we speculate that cervical cancer patients with increased mtDNA content may display a poorer prognosis.
The extent to which mtDNA content is influenced by genetic factors has not been clearly clarified. Although a lot of proteins encoded by the nuclear genes have been shown involved in the replication, transcription, and maintenance of mtDNA, the genetic loci and biologic mechanisms remain to be elucidated. Mitochondria and mtDNA production may increase through a pathway that bypasses cell cycle control in the cells under mild oxidative stress. Also, the mtDNA content increase in aging cells has been suggested as a result of defective mitochondria bearing impaired respiratory chain or mutated mtDNA. Two previous studies reported that higher mtDNA content was significantly associated with an increased risk of NHL and lung cancer, respectively [30]. Elevated mtDNA content was associated with altered oxidative stress, immune response activation, aging, and response to environmental exposures. Furthermore, genomic regions were also possible to harbor genes influencing mtDNA content variations. In addition, other factors such as p53, Ras, and p66 may also modulate mtDNA content. Taken together, the modulation of mtDNA content with cancer risk is multifactorial and multifaceted. Additional basic studies are needed to further elucidate the molecular mechanisms.
Studies on mtDNA in cervical cancer demonstrate that qualitative (mutations) and quantitative (copy number) mutations in mtDNA often exist simultaneously [31]. Therefore, we chose 10398 locus polymorphism, which has been frequently studied in other cancers. A previous study reported that 10398A was relevant to sporadic breast cancer risk; however, the mutation was not associated with age, tumor differentiation, stage, lymph node metastasis, ER, PR, and pre- or post-menstruation, suggesting that germ line mtDNA mutations might be important in the etiology of certain cancers. Another study demonstrated that the 10398 A allele was associated with increased risk for invasive breast cancer in both pre- and post-menopausal African–American women compared with those harboring the 10398G allele [32]. Studies on the 10398 alleles in breast cancer mechanistically implicate an inhibition of apoptotic resistance and altered transfer of calcium signals in the cytoplasm. Thus, these observations suggest that alleles at a few SNP sites could also act as risk factors for various diseases. In contrast with the previous studies, we demonstrate that the mutations in stage I were different from those in stages II and III. Also, mutations in squamous patients were significantly different from those in adenocarcinoma and adenosquamous patients; however, individual overall survival rate displayed no significant differences between the 10398A and 10398G alleles.
Zhai K et al. reported that the mtDNA control region variant C150 (REF. 35) was associated with an increased risk of HPV infection and cervical cancer in Chinese women [31]. In that case, HPV may have interactions with mitochondria in the cervical cancer pathogenesis. Therefore, we observed that individuals with the 10398G allele displayed an increased HPV-positive rate, and the HPV-18 and mtDNA contents were positively related in the younger subgroup (≤45 years) (correlation coefficient = 0.468, P = 0.016). Therefore, we conclude that qualitative (by mutations) and quantitative (by mtDNA copy number) mtDNA alterations are associated with susceptibility to persistent HPV infection. This was similar to previous studies. We observed that patients with increased mtDNA content with the 10398 A allele displayed the worst prognosis in cervical cancer.
Our population was enrolled from the Yichang Tumor Hospital and Zhongnan Hospital of Wuhan University. This region has an elevated cervical cancer incidence rate. However, our small sample size limits our statistical capacity to detect minimum to modest interactions between mtDNA content and other major risk factors. Additionally, our study was restricted to Han Chinese, and the generalizability of these results to other ethnic groups needs further evaluation. Also, our study does not bypass the reverse causation problem. We detected both mtDNA alterations and HPV infections and reported a relationship between these factors.
In conclusion, our data are the first to demonstrate that increased mtDNA content is associated with poor cervical cancer prognosis and high mtDNA content plus 10398A allele displays the worst prognosis. mtDNA alterations and HPV infections are related, and they both potentially affect prognosis. So, we speculate that the mtDNA alterations and HPV infections may have prognostic value; further studies are required to validate our result.
Abbreviations
- mtDNA:
-
Mitochondrial DNA
References
Shaughnessy DT, McAllister K, Worth L, et al. Mitochondria, energetics, epigenetics, and cellular responses to stress. Environ Health Perspect. 2014;122(12):1271–8. doi:10.1289/ehp.1408418.
Copeland WC, Longley MJ. Mitochondrial genome maintenance in health and disease. DNA Repair (Amst). 2014;19:190–8. doi:10.1016/j.dnarep.2014.03.010.
Jiang H et al. Peripheral blood mitochondrial DNA content, G10398A polymorphism, and risk of breast cancer in a Han Chinese population. Cancer Sci. 2014;105(6):639–45. doi:10.1111/cas.12412.
Xu H et al. Prognostic value of mitochondrial DNA content and G10398A polymorphism in non-small cell lung cancer. Oncol Rep. 2013;30(6):3006–12. doi:10.3892/or.2013.2783.
Wang Y, Liu VW, Xue WC, Tsang PC, Cheung AN, Ngan HY. The increase of mitochondrial DNA content in endometrial adenocarcinoma cells: a quantitative study using laser-captured microdissected tissues. Gynecol Oncol. 2005;98(1):104–10. doi:10.1016/j.ygyno.2005.04.015.
Lee HC et al. Somatic mutations in the D-loop and decrease in the copy number of mitochondrial DNA in human hepatocellular carcinoma. Mutat Res. 2004;547(1–2):71–8. doi:10.1016/j.mrfmmm.2003.12.011.
Lin CS et al. The role of mitochondrial DNA alterations in esophageal squamous cell carcinomas. J Thorac Cardiovasc Surg. 2010;139(1):189–97. doi:10.1016/j.jtcvs.2009.04.007.
Lauria A, Pompilioa G, Capogrossib MC. The mitochondrial genome in aging and senescence. Ageing Res Rev. 2014;18:1–15. doi:10.1016/j.arr.2014.07.001.
Santos RX, Correia SC, Zhu X, et al. Mitochondrial DNA oxidative damage and repair in aging and Alzheimer’s disease. Antioxid Redox Signal. 2013;18(18):2444–57. doi:10.1089/ars.2012.5039.
Liu CS et al. Oxidative stress-related alteration of the copy number of mitochondrial DNA in human leukocytes. Free Radic Res. 2003;37(12):1307–17. doi:10.1080/10715760310001621342.
Trinei M, Berniakovich I, Pelicci PG, Giorgio M. Mitochondrial DNA copy number is regulated by cellular proliferation: a role for Ras and p66(Shc). Biochim Biophys Acta. 2006;1757(5–6):624–30. doi:10.1016/j.bbabio.2006.05.029.
Canter JA, Kallianpur AR, Parl FF, Millikan RC. Mitochondrial DNA G10398A polymorphism and invasive breast cancer in African-American women. Cancer Res. 2005;65(17):8028–33. doi:10.1158/0008-5472.CAN-05-1428.
Ryan L, Parr RL. Somatic mitochondrial DNA mutations in prostate cancer and normal appearing adjacent glands in comparison to age-matched prostate samples without malignant histology. J Mol Diagn. 2006;8(3):312–9. doi:10.2353/jmoldx.2006.050112.
Hung WY, Wu CW, Yin PH, et al. Somatic mutations in mitochondrial genome and their potential roles in the progression of human gastric cancer. Biochim Biophys Acta. 2010;1800(3):264–70. doi:10.1016/j.bbagen.2009.06.006.
Faridi R et al. Oncogenic potential of human papillomavirus (HPV) and its relation with cervical cancer. Virol J. 2011;8:269. doi:10.1186/1743-422X-8-269.
Saraiya M, Berkoviwitz Z, Yabroff KR, Wideroff L, Kobrin S, Benard V. Cervical cancer screening with both human papillomavirus and Papanicolaou testing vs Papanicolaou testing alone: what screening intervals are physicians recommending? Arch Intern Med. 2010;170(11):977–85. doi:10.1001/archinternmed.2010.134.
Schiffman M, Wetzensen N, Wacholder S, Kinney W, Gage JC, Castle PE. Human papillomavirus testing in the prevention of cervical cancer. J Natl Cancer Inst. 2011;103(5):368–83. doi:10.1093/jnci/djq562.
Wu R et al. Human papillomavirus messenger RNA assay for cervical cancer screening: the Shenzhen Cervical Cancer Screening Trial I. Int J Gynecol Cancer. 2010;20(8):1411–4. doi:10.1111/IGC.0b013e3181f29547.
Wallace DC, Fan W, Procaccio V. Mitochondrial energetics and therapeutics. Annu Rev Pathol. 2010;5:297–348. doi:10.1146/annurev.pathol.4.110807.092314.
Wallace DC. Mitochondria and cancer. Nat Rev Cancer. 2012;12(10):685–98. doi:10.1038/nrc3365.
Warowicka A, Kwasniewska A, Gozdzicka-Jozefiak A. Alterations in mtDNA: a qualitative and quantitative study associated with cervical cancer development. Gynecol Oncol. 2013;129(1):193–8. doi:10.1016/j.ygyno.2013.01.001.
Egan K et al. Mitochondrial DNA in residual leukemia cells in cerebrospinal fluid in children with acute lymphoblastic leukemia. J Clin Med Res. 2010;2(5):225–9. doi:10.4021/jocmr443w.
Chen T et al. The mitochondrial DNA 4,977-bp deletion and its implication in copy number alteration in colorectal cancer. BMC Med Genet. 2011;12:8. doi:10.1186/1471-2350-12-8.
Milanea L, Trivedib M, Singha A, Talekara M, Amijia M. Mitochondrial biology, targets, and drug delivery. J Control Release. 2015;207:40–58. doi:10.1016/j.jconrel.2015.03.036.
Kabekkodu SP, Bhat S, Mascarenhas R, et al. Mitochondrial DNA variation analysis in cervical cancer. Mitochondrion. 2014;16:73–82. doi:10.1016/j.mito.2013.07.001.
Xing J et al. Mitochondrial DNA content: its genetic heritability and association with renal cell carcinoma. J Natl Cancer Inst. 2008;100(15):1104–12. doi:10.1093/jnci/djn213.
Yu M. Generation, function and diagnostic value of mitochondrial DNA copy number alterations in human cancers. Life Sci. 2011;89(3–4):65–71. doi:10.1016/j.lfs.2011.05.010.
Vivekanandan P et al. Mitochondrial mutations in hepatocellular carcinomas and fibrolamellar carcinomas. Mod Pathol. 2010;23(6):790–8. doi:10.1038/modpathol.2010.51.
Guardado-Estrada M, Medina-Martinez I, Juárez-Torres E, et al. The Amerindian mtDNA haplogroup B2 enhances the risk of HPV for cervical cancer: de-regulation of mitochondrial genes may be involved. J Hum Genet. 2012;57(4):269–76. doi:10.1038/jhg.2012.17.
Kabekkodu SP et al. Mitochondrial DNA variation analysis in cervical cancer. Mitochondrion. 2014;16:73–82. doi:10.1016/j.mito.2013.07.001.
Zhai K et al. Mitochondrial C150T polymorphism increases the risk of cervical cancer and HPV infection. Mitochondrion. 2011;11(4):559–63. doi:10.1016/j.mito.2011.02.005.
Kulawiec M, Owens KM, Singh KK. mtDNA G10398A variant in African-American women with breast cancer provides resistance to apoptosis and promotes metastasis in mice. J Hum Genet. 2009;54(11):647–54. doi:10.1038/jhg.2009.89.
Acknowledgments
The authors would like to thank the patients and their families for contributing to this study. This research was supported by the grant of National Natural Science Funds (No. 81172129 and No. 81472798).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflicts of interest
None
Additional information
Dali Feng and Hui Xu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Feng, D., Xu, H., Li, X. et al. An association analysis between mitochondrial DNA content, G10398A polymorphism, HPV infection, and the prognosis of cervical cancer in the Chinese Han population. Tumor Biol. 37, 5599–5607 (2016). https://doi.org/10.1007/s13277-015-4429-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4429-4






