Abstract
The Akt/mTOR and MAPK pathways play important roles in modulating cellular function in response to extracellular signals, and they are known to be activated in certain kinds of sarcomas. Few investigations have examined these pathways in dedifferentiated liposarcoma (DDLS), in relation to clinicopathological features. Clinicopathological and immunohistochemical analyses were conducted using 99 DDLS specimens. An in vitro study was also conducted to examine the antitumor effects of an mTOR inhibitor and a MEK inhibitor on two DDLS cell lines. The clinicopathological analyses revealed that the AJCC staging was a significant prognostic factor for overall survival and that the tumor size, depth, and location were significant prognostic factors for event-free survival. Phosphorylated Akt (pAkt), pmTOR, pS6RP, p4E-BP1, pMEK, and pERK expressions were positive in 57.4, 52.4, 71.4, 57.1, 84.1, and 50.8 % of the dedifferentiated component of the 63 primary DDLSs. Positive staining for pmTOR was significantly more frequent in the dedifferentiated component than the well-differentiated component. A univariate prognostic analysis revealed that pmTOR expression was associated with poor prognosis in the tumors in the retroperitoneum/ventral body cavity. The mTOR and MEK inhibitors dose-dependently inhibited the cell proliferation of both DDLS cell lines and decreased the expression of downstream pS6RP and pERK, respectively. The combined use of the two inhibitors enhanced antiproliferative activity. In conclusion, the Akt/mTOR and MAPK pathways were activated in DDLS specimens, and the inhibition of these pathways decreased cell proliferation in DDLS cell lines. Our findings suggest that these pathways could be a therapeutic target for patients with DDLS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dedifferentiated liposarcoma (DDLS) consists of an atypical lipomatous tumor/well-differentiated liposarcoma (ALT/WDLS)-like component and a nonlipogenic dedifferentiated component [1]. DDLS and ALT/WDLS share the same genetic abnormality characterized by supernumerary ring and giant chromosomes that contain amplified sequences originating from the 12q14-15 region [2, 3]. DDLS shows a worse prognosis than ALT/WDLS, with an estimated 5-year disease-specific survival of 44 % versus 93 % [4]. Conventional cytotoxic chemotherapy has reportedly provided a limited response rate [5, 6]. Thus, surgery is the main method of management of primary DDLS. A margin-free resection is a feasible treatment for DDLS located in the limbs but is more challenging for a retroperitoneal tumor. Retroperitoneal tumors are thus associated with a higher rate of recurrence [7, 8]. The introduction of new drugs and new therapeutic strategies for DDLS is still awaited.
The Akt/mammalian target of rapamycin (mTOR) and mitogen-activated protein kinase (MAPK) pathways are known to play important roles in modulating cellular functions in response to extracellular signals such as growth factors and cytokines [9, 10]. Akt is a serine/threonine kinase that is activated by phosphoinositide 3-kinase. Akt activates many downstream molecules involved in the regulation of cellular functions, including mTOR. mTOR is a key factor in the Akt/mTOR pathway; it activates p70S6 kinase and S6 ribosomal protein (S6RP) and inhibits the 4E binding protein 1 (4E-BP1). mTOR activation induces cellular proliferation, survival, motility, invasion, and differentiation and consequently leads to tumor initiation and progression [11]. The Ras/Raf/mitogen-activated protein kinase (MEK)/extracellular signal-regulated kinase (ERK) pathway, also known as the MAPK pathway, also regulates a variety of cell functions such as proliferation, growth, and survival [12]. There are a cross talk and a compensatory relationship between the Akt/mTOR and MAPK pathways [13, 14]. Ras can activate both the Akt/mTOR and the MAPK pathways. In addition, ERK can activate mTOR.
It was reported that the Akt/mTOR and MAPK pathways are activated in several soft tissue tumors [15–18]. The activation of the Akt/mTOR pathway is associated with poor prognosis in certain sarcomas [19–22]. In DDLS, the activation of the Akt pathway was demonstrated in 35 DDLS cases [23]. However, the prognostic relevance of these pathways in DDLS is still uncertain. In addition, a relationship between the Akt/mTOR and MAPK pathways in DDLS was not well studied.
Here we conducted a clinicopathologic and prognostic analysis of the Akt/mTOR and MAPK pathways in a large series of 99 DDLS clinical specimens. We then tested the antitumor activity of an mTOR inhibitor and a MEK inhibitor on DDLS cell lines in vitro.
Materials and methods
Patients
Ninety-nine paraffin-embedded specimens composed of 63 primary cases and 36 recurrent cases from 79 DDLS patients were retrieved from the registry of the Department of Anatomic Pathology, Kyushu University (Fukuoka, Japan) between 1976 and 2012. The diagnoses of DDLS had been made according to the latest edition of the World Health Organization classification [1]. The histological grade was evaluated according to the grading system of the French Federation of Cancer Centers (FNCLCC) [24]. Clinical details and follow-up information were obtained by reviewing medical charts. The tumor stage was also evaluated in accord with the staging system described in the seventh edition of the cancer staging manual issued by the American Joint Committee on Cancer (AJCC) [25].
This study was conducted in accord with the principles embodied in the Declaration of Helsinki. The study was also approved by the Ethics Committee of Kyushu University (No. 26-258) and conducted according to the Ethical Guidelines for Epidemiological Research enacted by the Japanese Government.
Immunohistochemistry
Immunohistochemical staining was performed for the 63 primary tumor and 36 recurrent tumor specimens. Formalin-fixed paraffin-embedded tissue was cut at 3 μm. Antigen retrieval was performed by boiling the slides with 10 mM sodium citrate (pH 6.0) or target retrieval solution (Dako, Carpinteria, CA, USA). The following rabbit antibodies were used as primary antibodies: phosphorylated (p) Akt (pAkt) (Ser473, 1:50), phosphorylated mTOR (pmTOR) (Ser2448, 1:50), pS6RP (Ser235/236, 1:50), p4E-BP1 (Thr37/46, 1:400), pMEK1/2 (Ser221, 1:50), and pErk1/2 (Thr202/Tyr204, 1:100) (Cell Signaling Technology, Danvers, MA).
The immune complex was detected with the DAKO EnVision Detection System (Dako). Immunohistochemical results were judged by two investigators (T.I. and K.K.), who were blinded to the clinical status of the patients. A consensus judgment was adopted as the proper immunohistochemical result. Positive staining for individual markers was evaluated on the basis of its staining intensity. When the tumor cells showed cytoplasmic and/or nuclear staining with equal to stronger intensity compared to that of the endothelial cells, the expression was considered positive by reference to the previously published reports [21].
Cells and culture conditions
The DDLS cell lines FU-DDLS-1 and NDDLS-1 were established by Dr. Nishio [26] and Dr. Ariizumi [27] and maintained in DMEM/F12 and RPMI-1640 media, respectively. Both media preparations were supplemented with 10 % fetal bovine serum (FBS) plus penicillin and streptomycin.
Cell proliferation assay
FU-DDLS-1 and NDDLS-1 cells were plated on 96-well plates at a concentration of 2000 cells per well in serum-containing growth medium. Cells were treated with carrier alone (0.01 % DMSO), an mTOR inhibitor (everolimus, RAD001, Selleck Chemicals, Houston, TX), or a MEK inhibitor (PD0325901, Selleck Chemicals) with the indicated concentrations or with a combined use of the mTOR (100 nM) and MEK (100 nM) inhibitors for 72 h. Viability was assessed by WST-8 assay using the Cell Counting Kit 8 (Dojindo Molecular Technologies, Kumamoto, Japan) according to the manufacturer’s instructions. The absorbance at 450 nm was measured using a microplate reader (Model 680 Microplate Reader, Bio-Rad Laboratories, Hercules, CA). All experiments were done in triplicate and repeated three times.
Western blot analysis
A western blot analysis was conducted using the DDLS cell lines and monoclonal antibodies of mTOR (1:400), pmTOR (Ser2448, 1:200), S6RP (1:400), pS6RP (Ser235/236, 1:500), p4E-BP1 (Thr37/46, 1:200), Erk1/2 (1:600), pErk1/2 (Thr202/Tyr204, 1:400), and beta-actin (1:5000). Proteins were extracted using lysis buffer (PRO-PREP Protein Extraction Solution, iNtRON Biotechnology, Seongnam, South Korea) after treatment with carrier alone, everolimus (RAD001), or PD0325901 with the indicated concentrations for 48 h. The lysates (20 μg) were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) using 4–15 % (mTOR and pmTOR) or Any kD™ (S6RP, pS6RP, p4E-BP1, Erk1/2, pErk1/2, and beta-actin) Mini-protean TGX precast gels (Bio-Rad, Hercules, CA) and transferred to polyvinylidene difluoride membranes. The membranes were blocked with 5 % bovine serum albumin (BSA) and incubated with the primary antibodies using the SNAP i.d. Protein Detection System (Millipore, Bedford, MA) in accord with the manufacturer’s instructions. As an internal control, antiactin (1:5000) (MP Biomedicals, Irvine, CA) mouse monoclonal antibody was used. The membranes were then incubated with antirabbit immunoglobulin (IgG) (Cell Signaling Technology) or antimouse IgG1 (Santa Cruz Biotechnology, Santa Cruz, CA). All membranes were observed using ECL Plus (GE Healthcare, Buckinghamshire, UK).
Statistical analysis
The survival analyses were conducted using the log-rank test. The chi-square test or McNemar’s test was applied to evaluate the association between two variables. Continuous variables are presented as means ± standard error. The Steel-Dwass multiple comparison test was used to compare the data of the four groups. Statistical significance was defined as P < 0.05. The data analyses were conducted with JMP statistical software (ver. 9.0.2, SAS Institute, Cary, NC).
Results
Clinical and pathologic features
The clinicopathological features of the 63 primary tumors are summarized in Table 1. The tumor samples were taken from 44 males and 19 females whose ages ranged from 39 to 89 years (median 67 years). The tumor sizes ranged from 4 to 40 cm in maximum dia (median 14 cm). Most of the tumors (57 cases) were located in deep sites (subfascial or even deeper). In 45 cases, the tumors were in the retroperitoneum/ventral body cavity (RT/VC) (retroperitoneum, 37; abdominal cavity, 4; mediastinum, 2; scrotum, 2). In 18 cases, the tumors were in the extremity/trunk (E/T) (extremities, 12; thoracoabdominal wall, 2; head and neck, 2; back, 1; buttock, 1). Forty-one cases had microscopically positive margins defined as tumor present at or within 1 mm from the margin [28]. Necrosis was observed in 38 cases (<50 %, 33; ≥50 %, 5). Mitotic activities were counted per 10 high power fields (HPF) (0–9/10 HPF, 53; 10–19/HPF, 9; ≥20/HPF, 1). Fifty-one cases and 12 cases were categorized as FNCLCC grade 2 and grade 3, respectively. Similarly, 4 cases, 42 cases, 12 cases, and 2 cases were categorized in AJCC stages IIA, IIB, III, and IV, respectively.
The statistical analysis of the clinicopathological features revealed that the AJCC staging (IIA + IIB vs. III + IV, P = 0.0411) was a significant prognostic factor for overall survival and that the tumor size (P = 0.0040), tumor depth (P = 0.0432), tumor location (P = 0.0015), and resected margin (P = 0.0250) were significant prognostic factors for event-free survival, based on the results of a univariate analysis with the log-rank test. Mitotic activity, FNCLCC grade, and AJCC stage were shown to be significant prognostic factors for overall survival and event-free survival for tumors in E/T locations. A multivariate analysis was performed, but statistical significance was not obtained for any parameters (data not shown).
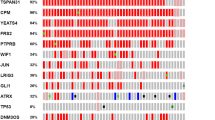
Activation status of the Akt/mTOR and MAPK pathways in DDLS
Our comparison of the activation status of the Akt/mTOR and MAPK pathways between the dedifferentiated and well-differentiated components and the primary and recurrent dedifferentiated lesions is summarized in Table 2. We compared the dedifferentiated component and well-differentiated component in the same lesion (both the primary and recurrent lesions). We also compared the dedifferentiated lesions of the primary and recurrent lesions. In the 36 recurrent cases, five lesions do not contain dedifferentiated component but composed of only well-differentiated component; thus, these five cases were excluded from the comparison. Most of the differences were not significant, except that positive staining for pmTOR and pMEK was observed significantly more frequently in the dedifferentiated component compared to the well-differentiated component (P = 0.0006 and P = 0.0201, respectively).
The results of the immunostaining for each antibody are illustrated in Fig. 1. pAkt, pmTOR, pS6RP, p4E-BP1, pMEK, and pERK expressions were positive in 36 (57.4 %), 33 (52.4 %), 45 (71.4 %), 36 (57.1 %), 53 (84.1 %), and 32 (50.8 %) of the dedifferentiated component of the 63 primary tumors, respectively. The results of immunostaining and the correlation between them and with prognosis are summarized in Table 3. The positive results for pmTOR and for downstream pS6RP and p4E-BP1 and pERK were correlated with each other. Among the factors of the Akt/mTOR and MAPK pathways investigated, positivity for pmTOR (P = 0.0301) showed a significant association with event-free survival in the univariate prognostic analysis of the tumors that developed in RT/VC.
Antitumor effects of the mTOR and MEK inhibitors on the DDLS cell lines
On the basis of the activation status of the Akt/mTOR and MAPK pathways, we chose an mTOR inhibitor (RAD001) and a MEK inhibitor (PD0325901) for the in vitro experiment. These inhibitors dose-dependently inhibited the cell proliferation of both the FU-DDLS-1 and NDDLS-1 cell lines (Fig. 2a, b). RAD001 and PD0325901 treatment decreased cell proliferation in both cell lines with a dose of over 100 and 300 nM, respectively. There is a slight enhancement of proliferation rate, in part, by the low-dose use of each inhibitor. In addition, the combined use of RAD001 and PD0325901 enhanced antiproliferative activity in both cell lines and significant enhancements were observed in FU-DDLS-1 (Fig. 2c).
a, b The effects of RAD001 and PD0325901 with the indicated concentrations on the two DDLS cell lines evaluated by cell proliferation assay. RAD001 and PD0325901 dose-dependently inhibited cell proliferation in both DDLS cell lines. c The effects of the combined use of RAD001 (100 nM) and PD0325901 (100 nM) in the DDLS cell lines evaluated by cell proliferation assay. MEKi: MEK inhibitor, PD0325901; mTORi: mTOR inhibitor, RAD001. *P < 0.05 by Steel-Dwass multiple comparison test
The western blotting analysis revealed that RAD001 and PD0325901 treatment dose-dependently decreased the phosphorylation of its downstream S6RP and ERK, respectively (Fig. 3a, b). RAD001 treatment decreased the expression of pmTOR and pS6RP, especially with a dose of over 100 nM. RAD001 treatment decreased the expression of p4E-BP1 in FU-DDLS-1, whereas increased expression was observed in NDDLS-1. The expression of p4E-BP1 was decreased in FU-DDLS-1, but increased in NDDLS-1. In the same line, PD0325901 treatment decreased the expression of pERK, especially with a dose of over 10 nM. Western blotting also confirmed that RAD001 treatment dose-dependently increased the pERK expression as a compensatory relationship between the Akt/mTOR and MAPK pathways in the NDDLS-1 cells, whereas PD0325901 treatment showed no clear effect on pmTOR expression.
Discussion
The objectives of this study were to investigate the activation status and prognostic impact of the Akt/mTOR and MAPK pathways in DDLS and clarify the potency of molecular therapy targeting these pathways. The results suggest that the inhibition of these pathways could provide clinical benefit in patients with DDLS and could be an option for systemic treatment.
Our findings revealed that RT/VC and deep location and large tumor size are associated with decreased event-free survival in DDLS. It was reported that retroperitoneal DDLS tumors have significantly higher rates of local recurrence rate compared to limb tumors [7, 8]. DDLS is usually asymptomatic, and retroperitoneal tumors are found by chance as a large mass [1]. Our present findings are thus consistent with previous reports. Recent studies demonstrated that high histological grade is associated with a worse prognosis in DDLS [28, 29], but the present investigation did not reveal any such significant relation, with no association between high AJCC stage and decreased overall survival. However, our analysis of the 18 E/T tumors showed that FNCLCC grade and AJCC stage were significantly associated with the patients’ overall survival and event-free survival. These associations were not observed in the RT/VC tumors. Complete resection is difficult in RT/VC tumors, and residual tumors that are not recognized at surgery could exist. Therefore, the histological grade might not have a major impact on the prognosis of patients with RT/VC tumors. In addition, our series had a relatively small number of grade 3 tumors compared to the previous studies, and this difference might have affected the result. Although at this point we cannot make any conclusion about the prognostic impact of histological grade in RT/VC DDLS, RT/VC DDLSs are still preferred candidates for systemic treatment. In summary, RT/VC tumors and histologically high-grade tumors are preferred candidates for systemic treatment.
Immunopositivity for pmTOR was identified as an adverse prognostic factor in RT/VC DDLS. The positive results for pmTOR and downstream p4E-BP1 and pS6RP were correlated with each other, suggesting that these molecules are activated in a pathway manner. However, we did not detect a significant correlation between the positive results for pAkt and pmTOR. The correlations between pAkt and downstream p4E-BP1 and pS6RP were significant and marginally significant, respectively. A large-scale series might therefore detect a significant correlation between pAkt and pmTOR. In addition, it is well known that the Akt/mTOR and MAPK pathways engage in cross talk [13], and in our study, the immunopositivities for pmTOR and pERK were correlated with each other. We thus speculate that mTOR may be activated via ERK activation in DDLS.
We also found that most of the molecules analyzed in this study are frequently activated in dedifferentiated and recurrent lesions compared to well-differentiated and primary lesions, respectively. Though a significant difference was detected only in the positive result for pmTOR in our comparison of the dedifferentiated and well-differentiated components, these findings suggest that the Akt/mTOR and MAPK pathways are highly activated in aggressive tumors, and they support the idea that these pathways are eligible for molecular target therapy.
RAD001 (an mTOR inhibitor) and PD0325901 (a MEK inhibitor) dose-dependently inhibited the cell proliferation in the two DDLS cell lines and the expression of its downstream pS6RP and pERK, respectively. We also showed that RAD001 was likely to have a higher antitumor effect than PD0325901, and thus, the mTOR inhibitor might be the preferred agent to use in combination with other molecular target therapies and conventional chemotherapy. The effect of RAD001 is consistent with a previous report of targeted PI3K signaling inhibition for liposarcoma [30]. However, a phase III trial of ridaforolimus (an mTOR inhibitor) targeting metastatic sarcomas did not achieve a satisfactory outcome [31]. Ridaforolimus only delayed tumor progression to a small degree, and the activation of an intracellular compensatory signaling pathway was cited as a possible cause of the resistance to this mTOR inhibitor. Combination therapy with other signaling inhibitors may thus lead to more substantial clinical benefit.
Regarding potential targets for combination therapy, the MAPK pathway has gained attention. The Akt/mTOR and MAPK pathways have cross talk and compensatory actions [13, 14], and the coinhibition of both pathways has been successful in reducing tumor growth in xenograft cancer models [32, 33]. In the present study, the pERK expression in the NDDLS-1 cell line was increased by mTOR inhibitor treatment. This result indicates that the single use of an mTOR inhibitor could increase the signal toward the MAPK pathway and thus potentially develops resistance to the mTOR inhibitor in DDLS. However, we also observed that the antiproliferative activity was enhanced by targeted Akt/mTOR and MAPK pathway inhibition in both of the DDLS cell lines. The combination of mTOR and MEK inhibitors may provide a therapeutic benefit through the abrogation of feedback and could be a candidate DDLS treatment strategy.
Interestingly, our data showed a slight enhancement of proliferation rate by the low-dose use of each inhibitor. Though apparent compensatory actions between the Akt/mTOR and MAPK pathways were not observed in the western blotting analysis, the activation of intracellular compensatory signaling pathway could be a possible cause. When in a clinical setting, physicians should be cautious about blood concentration and tumor response and consider combination use with other agent.
At this stage, we cannot identify the markers that would be useful in deciding whether targeting these pathways would be optimal for each DDLS patient. In a phase II study of ridaforolimus, eight signal proteins including pAkt, pS6, and 4E-BP1 that lie upstream or downstream of mTOR were examined; none of them were found to be a good predictor of a clinically beneficial response [34]. On the other hand, in patients with metastatic renal cell carcinoma, the expression levels of pmTOR and pS6RP were reported to be a potential predictive biomarker for the efficacy of RAD001 [35]. Here we observed that pmTOR positivity in the RT/VC tumors was correlated with prognosis. This result supports the further investigation of mTOR inhibitors as either monotherapy or in combination with another cytotoxic treatment in RT/VC DDLS.
In conclusion, the results of the present study demonstrated that the Akt/mTOR and MAPK pathways were activated in DDLS and that the coinhibition of both pathways enhanced antiproliferative activity. These findings support the validity of molecular therapy targeting these pathways in patients with DDLS, especially those with RT/VC tumors.
References
Dei Tos J. Dedifferentiated liposarcoma. In: Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F, editors. WHO classification of tumours of soft tissue and bone. Lyon: International Agency for Research on Cancer (IRAC); 2013. p. 37–8.
Pedeutour F, Forus A, Coindre JM, Berner JM, Nicolo G, Michiels JF, et al. Structure of the supernumerary ring and giant rod chromosomes in adipose tissue tumors. Genes Chromosom Cancer. 1999;24:30–41.
Mertens F, Fletcher CD, Dal Cin P, De Wever I, Mandahl N, Mitelman F, et al. Cytogenetic analysis of 46 pleomorphic soft tissue sarcomas and correlation with morphologic and clinical features: a report of the CHAMP Study Group. Chromosomes and MorPhology. Genes Chromosom Cancer. 1998;22:16–25.
Dalal KM, Kattan MW, Antonescu CR, Brennan MF, Singer S. Subtype specific prognostic nomogram for patients with primary liposarcoma of the retroperitoneum, extremity, or trunk. Ann Surg. 2006;244:381–91.
Italiano A, Toulmonde M, Cioffi A, Penel N, Isambert N, Bompas E, et al. Advanced well-differentiated/dedifferentiated liposarcomas: role of chemotherapy and survival. Ann Oncol. 2012;23:1601–7.
Jones RL, Fisher C, Al-Muderis O, Judson IR. Differential sensitivity of liposarcoma subtypes to chemotherapy. Eur J Cancer. 2005;41:2853–60.
Coindre JM, Pedeutour F, Aurias A. Well-differentiated and dedifferentiated liposarcomas. Virchows Arch. 2010;456:167–79.
Linehan DC, Lewis JJ, Leung D, Brennan MF. Influence of biologic factors and anatomic site in completely resected liposarcoma. J Clin Oncol. 2000;18:1637–43.
Altomare DA, Testa JR. Perturbations of the AKT signaling pathway in human cancer. Oncogene. 2005;24:7455–64.
Vakiani E, Solit DB. KRAS and BRAF: drug targets and predictive biomarkers. J Pathol. 2011;223:220–30.
Hsieh AC, Liu Y, Edlind MP, Ingolia NT, Janes MR, Sher A, et al. The translational landscape of mTOR signalling steers cancer initiation and metastasis. Nature. 2013;485:55–61.
Dasari A, Messersmith WA. New strategies in colorectal cancer: biomarkers of response to epidermal growth factor receptor monoclonal antibodies and potential therapeutic targets in phosphoinositide 3-kinase and mitogen-activated protein kinase pathways. Clin Cancer Res. 2010;16:3811–8.
Mendoza MC, Er EE, Blenis J. The Ras-ERK and PI3K-mTOR pathways: cross-talk and compensation. Trends Biochem Sci. 2011;36:320–8.
Wang C, Cigliano A, Delogu S, Armbruster J, Dombrowski F, Evert M, et al. Functional crosstalk between AKT/mTOR and Ras/MAPK pathways in hepatocarcinogenesis: implications for the treatment of human liver cancer. Cell Cycle. 2013;12:1999–2010.
Dobashi Y, Suzuki S, Sato E, Hamada Y, Yanagawa T, Ooi A. EGFR-dependent and independent activation of Akt/mTOR cascade in bone and soft tissue tumors. Mod Pathol. 2009;22:1328–40.
Dobashi Y, Suzuki S, Sugawara H, Ooi A. Involvement of epidermal growth factor receptor and downstream molecules in bone and soft tissue tumors. Hum Pathol. 2007;38:914–25.
Yamada Y, Kohashi K, Fushimi F, Takahashi Y, Setsu N, Endo M, et al. Activation of the Akt-mTOR pathway and receptor tyrosine kinase in patients with solitary fibrous tumors. Cancer. 2014;120:864–76.
Takahashi Y, Kohashi K, Yamada Y, Endo M, Setsu N, Ishii T, et al. Activation of the Akt/mammalian target of rapamycin pathway in myxofibrosarcomas. Hum Pathol. 2014;45:984–93.
Tomita Y, Morooka T, Hoshida Y, Zhang B, Qiu Y, Nakamichi I, et al. Prognostic significance of activated AKT expression in soft-tissue sarcoma. Clin Cancer Res. 2006;12:3070–7.
Setsu N, Kohashi K, Fushimi F, Endo M, Yamamoto H, Takahashi Y, et al. Prognostic impact of the activation status of the Akt/mTOR pathway in synovial sarcoma. Cancer. 2013;119:3504–13.
Endo M, Yamamoto H, Setsu N, Kohashi K, Takahashi Y, Ishii T, et al. Prognostic significance of AKT/mTOR and MAPK pathways and antitumor effect of mTOR inhibitor in NF1-related and sporadic malignant peripheral nerve sheath tumors. Clin Cancer Res. 2013;19:450–61.
Setsu N, Yamamoto H, Kohashi K, Endo M, Matsuda S, Yokoyama R, et al. The Akt/mammalian target of rapamycin pathway is activated and associated with adverse prognosis in soft tissue leiomyosarcomas. Cancer. 2012;118:1637–48.
Gutierrez A, Snyder EL, Marino-Enriquez A, Zhang YX, Sioletic S, Kozakewich E, et al. Aberrant AKT activation drives well-differentiated liposarcoma. Proc Natl Acad Sci U S A. 2011;108(39):16386–91.
Trojani M, Contesso G, Coindre JM, Rouesse J, Bui NB, de Mascarel A, et al. Soft-tissue sarcomas of adults; study of pathological prognostic variables and definition of a histopathological grading system. Int J Cancer. 1984;33:37–42.
Pollock RE, Baker LH, Brennan MF, Coombes K, Kattan M, Kneisl JS, et al. Soft tissue sarcoma. In: Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual 7th edn. American Joint Committee on Cancer, Springer: Chicago; 2010. pp 291–298.
Nishio J, Iwasaki H, Ishiguro M, Ohjimi Y, Fujita C, Ikegami H, et al. Establishment of a novel human dedifferentiated liposarcoma cell line, FU-DDLS-1: conventional and molecular cytogenetic characterization. Int J Oncol. 2003;22:535–42.
Ariizumi T, Ogose A, Kawashima H, Hotta T, Li G, Xu Y, et al. Establishment and characterization of a novel dedifferentiated liposarcoma cell line, NDDLS-1. Pathol Int. 2011;61:461–8.
Jour G, Gullet A, Liu M, Hoch BL. Prognostic relevance of Fédération Nationale des Centres de Lutte Contre le Cancer grade and MDM2 amplification levels in dedifferentiated liposarcoma: a study of 50 cases. Mod Pathol. 2015;28:37–47.
Gronchi A, Collini P, Miceli R, Valeri B, Renne SL, Dagrada G, et al. Myogenic differentiation and histological grading are major prognostic determinants in retroperitoneal liposarcoma. Am J Surg Pathol. 2015;39:383–93.
Guo S, Lopez-Marquez H, Fan KC, Choy E, Cote G, Harmon D, et al. Synergistic effects of targeted PI3K signaling inhibition and chemotherapy in liposarcoma. PLoS One. 2014;9:e93996.
Demetri GD, Chwla SP, Ray-Coquard I, Le Cesne A, Staddon AP, Milhem MM, et al. Results of an international randomized phase III trial of the mammalian target of rapamycin inhibitor ridaforolimus versus placebo to control metastatic sarcomas in patients after benefit from prior chemotherapy. J Clin Oncol. 2013;31:2485–92.
Kinkade CW, Castillo-Martin M, Puzio-Kuter A, Yan J, Foster TH, Gao H, et al. Targeting AKT/mTOR and ERK MAPK signaling inhibits hormone-refractory prostate cancer in a preclinical mouse model. J Clin Invest. 2008;118:3051–64.
Engelman JA, Chen L, Tan X, Crosby K, Guimaraes AR, Upadhyay R, et al. Effective use of PI3K and MEK inhibitors to treat mutant Kras G12D and PIK3CA H1047R murine lung cancers. Nat Med. 2008;14:1351–6.
Chawla SP, Staddon AP, Baker LH, Schuetze SM, Tolcher AW, D’Amato GZ, et al. Phase II study of the mammalian target of rapamycin inhibitor ridaforolimus in patients with advanced bone and soft tissue sarcomas. J Clin Oncol. 2012;30:78–84.
Li S, Kong Y, Si L, Chi Z, Cui C, Sheng X, et al. Phosphorylation of mTOR and S6RP predicts the efficacy of everolimus in patients with metastatic renal cell carcinoma. BMC Cancer. 2014;14:376.
Acknowledgments
This work was supported by JSPS KAKEN Grant Number 25293088. The English used in this article was revised by KN International (http://www.kninter.com). We would like to express our sincere appreciation to Prof. Masao Tanaka, Department of Surgery and Oncology, Prof. Yoshihiko Maehara, Department of Surgery and Science and Prof. Seiji Naito, Department of urology, Graduate School of Medical Sciences, Kyushu University for kind support for our research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Ishii, T., Kohashi, K., Iura, K. et al. Activation of the Akt-mTOR and MAPK pathways in dedifferentiated liposarcomas. Tumor Biol. 37, 4767–4776 (2016). https://doi.org/10.1007/s13277-015-4232-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4232-2