Abstract
Colorectal adenomatous polyp (CRAP) is a major risk factor for the development of sporadic colorectal cancer (CRC). Histone modifications are one of the epigenetic mechanisms that may have key roles in the carcinogenesis of CRC. The objective of the present study is to investigate the alternations in the defined histone modification gene expression profiles in patients with CRAP and CRC. Histone modification enzyme key gene expressions of the CRC, CRAP, and control groups were evaluated and compared using the reverse transcription PCR (RT-PCR) array method. Gene expression analysis was performed in the CRAP group after dividing the patients into subgroups according to the polyp diameter, pathological results, and morphological parameters which are risk factors for developing CRC in patients with CRAP. PAK1, NEK6, AURKA, AURKB, HDAC1, and HDAC7 were significantly more overexpressed in CRC subjects compared to the controls (p < 0.05). PAK1, NEK6, AURKA, AURKB, and HDAC1 were significantly more overexpressed in the CRAP group compared to the controls (p < 0.005). There were no significant differences between the CRAP and CRC groups with regards to PAK1, NEK6, AURKA, or AURKB gene overexpression. PAK1, NEK6, AURKA, and AURKB were significantly in correlation with the polyp diameter as they were more overexpressed in polyps with larger diameters. In conclusion, overexpressions of NEK6, AURKA, AURKB, and PAK1 genes can be used as predictive markers to decide the colonoscopic surveillance intervals after the polypectomy procedure especially in polyps with larger diameters.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is one of the leading causes of morbidity and mortality since it accounts for 10 % of all cancers in adults and the fourth leading cause of cancer-related deaths [1]. Most CRCs progress from colorectal adenomatous polyps (CRAPs) [2]. CRAPs are benign tumors of columnar cells or the glandular tissue, and sporadic adenomatous polyps tend to progress to cancer with increasing degrees of dysplasia associated with progressive accrual of several genetic and epigenetic changes [2, 3]. High malignancy risk criteria in CRAPs include advanced age, number of polyps, polyp diameter, villous component, nuclear atypia frequency, sessility, family history, and dysplasia severity. Of the adenomas larger than 1 cm, involving villous components and with severe dysplasia, 3, 17, and 37 %, respectively, transform to cancer annually [2, 4].
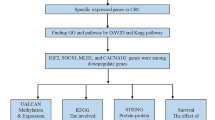
Different pathways such as chromosomal instability and microsatellite instability pathway, β-catenin/Wnt, TGFβ/SMAD, and RAF/RAS/MAPK intermediary pathways have been described in CRC carcinogenesis. K-RAS mutation, B-RAF mutation, 18q deletion, APC mutation, p53 mutation as well as genetic and epigenetic alternations like DNA CpG islet hypermethylation, non-coding RNA (miRNA) expressions and specific histone modifications are observed in these pathways [5–7]. Epigenetic changes that result in subsequent aberrant gene expression are known to have key roles as ultimate predictors in inflammation-induced CRC carcinogenesis. Recent studies indicate that histone modification genes including NEK6, AURKA, PAK1, HDAC1, HDAC2, HDAC3, HDAC5, and HDAC7 have key roles in the carcinogenesis of CRC [8–16].
There is a clear need for more effective and selective markers to determine in CRAP patients who are at a higher risk of developing CRC. It is reasonable to commend that epigenetic alternations including histone modification have significant roles in cancer formation from CRAP tissues, and further studies are needed to elucidate this pathogenesis. There are no studies about the relationship comparing epigenetic chromatin histone modification patterns of CRAP and CRC in the literature. Therefore, we aimed in this study to investigate the value of chromatin histone modification in patient with regards to risk of CRC progression from CRAP.
Materials and methods
Study location
The study was performed at the Gastroenterology and Medical Biology departments of Manisa Celal Bayar University Medical High School between November 2012 and November 2013. Patients presenting to the Gastroenterology Department of Manisa Celal Bayar University were included in the study.
Ethics committee
This study was performed in accordance with the Declaration of Helsinki, good clinical practice, and applicable regulatory requirements. The study was carried out with the approval of the Institutional Ethical Review Board of the Celal Bayar University Medical Center with the approval number 269 dated 26 November 2012. Informed written consent form was obtained from each patient.
Study design and samples
Fresh matched tissue samples were collected from a total of 75 patients presenting to the Gastroenterology Department of Celal Bayar University between November 2012 and November 2013 [group 1 (25 patients) was categorized as histopathologically confirmed CRC group; group 2 (25 patients) was categorized as the histopathologically confirmed CRAP group; group 3 (25 patients) was the control group and included patients with normal colon mucosa]. In addition, 25 patients in each group, 2 colon cancer samples, 3 polyp, and 1 control samples were lost due to RNA degradation. Patients were excluded from the study if they received colectomy for any reason, diagnosed with any types of malignancy, and had received chemotherapy or radiotherapy. Age, sex, and history/family history were questioned and documented for all patients. All patients were checked for complete blood count and biochemical tests.
For patients with CRAP, polyp diameter, macroscopic polyp appearance (sessile/pedinculated), colonic location of the polyp, presence/number of any additional polyps at other foci as determined by colonoscopy, routine evaluations and examinations were documented for data purposes. Therapeutic polypectomy with endoscopic snare was performed for all polyps. All results of pathological assessments of the resected polyps such as histological type, morphological type (tubular, tubulovillous, villous), and presence of dysplasia were evaluated and documented.
For all patients diagnosed with CRC, CT or PET/CT was performed for malignancy staging and tumor type was identified in biopsy samples and colon resection material if the patient was operated, and the results were documented.
Colonoscopy
Colonoscopic examinations of all patients were performed at the Gastroenterology Department of Celal Bayar University by the three gastroenterologists (EK, HY, EG) who performed the study. Olympus Luxera CFQ260AL was used for colonoscopy. Complete colonoscopic examinations including the terminal ileum were performed for all controls and diagnosed with CRAP. For patients with CRC, complete colonoscopic examination including the terminal ileum was performed if access to the proximal of the tumor could be achieved. If total ileocolonoscopy was not successful, proximal of the tumor was assessed with abdominal CT. For pathologic assessments, mucosal biopsy samples were collected from the tumor tissue in the CRC group, from the polyp tissue in the CRAP group, and from rectal, cecal, and terminal ileal mucosa in the control group using Olympus biopsy forceps. Pathologic assessments of all biopsy samples were performed in the Pathology Department of Celal Bayar University, and the resulting data were documented.
Additional mucosal biopsy samples from the tumor tissue of the CRC patients, from the polyp tissue of the CRAP patients, and from normal appearing mucosa of the control group were collected for histone modification gene expression analyses using Olympus biopsy forceps.
The tissue samples were immediately frozen using dry ice (a block of dry ice has a surface temperature of −78.5 °C) and stored at −80 °C until RNA extraction.
RNA isolation from tissue
Total RNA was isolated using RNeasy Mini Kit (Qiagen, Germany) described in the manufacturer’s protocol with small modifications. The fresh tissue samples (20–30 mg) from patients were with 600 μl Buffer RLT and a metal ball with a 7 mm diameter homogenized in TissueLyser II homogenizer (Qiagen, Germany) at 25,000 Hz for 5 min. The lysate was centrifuged at maximum speed, and supernatant was treated after this point following the RNeasy Mini Kit protocol.
Quantity and purity of total RNA
RNA was quantified measuring the absorbance at 260 nm (A260), and RNA purity was determined by the ratio A260/A280 using spectrophotometer. RNA quality was considered to be acceptable with A260/A280 ratio slightly higher than 2.0 and A260/A230 ratio slightly higher than 1.8. All steps were taken according to the manufacturer’s protocol.
cDNA synthesis
We performed the complementary DNA (cDNA) synthesis with RT First Strand Kit (C-03) (SA Bioscience, Frederick, MD, USA). Eight microliters of RNA sample was incubated with 2 μl of GE (5× gDNA Elimination Buffer) at 42 °C for 5 min in a 0.2 ml PCR tube. In another tube, a PCR cocktail (4 μl RT Buffer 3 (5× BC3), 1 μl P2 (Primer and External Control mix), 2 μl RT Enzyme Mix 3 (RE3), and 3 μl H2O were prepared and added onto the RNA sample following by a 15-min incubation at 42 °C and 5-min incubation at 95 °C. The cDNA samples were later diluted as needed. All steps were taken according to the manufacturer’s protocol.
Human Epigenetic Chromatin Modification Enzyme RT2 Profiler™ PCR Array
The Human Epigenetic Chromatin Modification Enzyme RT2 Profiler™ PCR Array (PAHS-085A) (SA Biosciences, Frederick, MD, USA) was used to detect the expression levels of 84 key genes listed in Table 1.
A total of 2300 μl reverse transcription PCR (RT-PCR) array mix (102 μl diluted cDNA, 1150 μl 2× RT2 SYBR Green ROX FAST Master mix, and 1048 μl H2O) was prepared and loaded on 96-well Human Epigenetic Chromatin Modification Enzymes RT2 Profiler™ PCR arrays 20 μl per well. Arrays were placed in Rotor-Gene RG-3000 (Corbett Research, Qiagen, Germany) and were initially activated at 95 °C for 10 min followed by 40 cycles of 95 °C for 15 s and 60 °C for 30-s incubation. Array data was analyzed, and eight genes were determined to be the most overexpressed or underexpressed to cross-validate by RT qPCR.
RT2 qPCR primer assay
The cDNA samples of the eight genes chosen to be overexpressed or underexpressed (AURKB, AURKA, SETD8, PAK1, NEK6, KDM4C, HDAC1, HDAC7) and one housekeeping gene (HPRT1) were further tested by RT qPCR. The Primer Assays and SYBR Green Master Mix (SA Biosciences, Frederick, MD, USA) specific for the eight genes were purchased, and each PCR reaction mix was prepared by adding 12.5 μl of SYBR Green Master Mix and 1 μl of Primer (10 pmol) per 2.2 μl cDNA sample. Total volume was adjusted to 25 μl with dH2O, and PCR mixes were loaded on the plate of Rotor-Gene RG-3000 (Corbett Research, Qiagen, Germany) for amplification. Amplification was performed with an initial denaturation step at 95 °C for 5 min followed by 40 cycles of 94 °C for 1 min, 61 °C for 40 s, and 72 °C for 1 min with a final elongation step at 72 °C for 2 min. Cycle threshold (Ct) values obtained from the RT qPCR reactions were normalized to the reference gene (HPRT1) and evaluated using Relative Expression Software Tool (REST) 2009 (V.2.0.13) in standard mode. All steps were taken according to the manufacturer’s protocol.
Data analysis and statistics
Data were analyzed using RT2 profiler PCR array and RT2 qPCR primer assay data analysis software (http://www.sabiosciences.com/pcrarraydataanalysis.php). The website allowed online analysis. PCR array was quantified based on the Ct number. A gene was considered to be not detectable when Ct is above 32. Ct was defined as 35 for the ΔCt calculation when the signal was under detectable limits. Fold change and fold regulation values over 2 were indicative of upregulated genes; fold change values under 0.5 and fold regulation values under −2 were indicative of downregulated genes. Results were expressed as the mean values ± standard deviation, and the p values were calculated based on a Student’s t test of the replicate 2−ΔCt values for each gene in the control group, CRC group, and CRAP group. The characteristics data among the three groups were obtained using Statistical Package for the Social Sciences (SPSS Inc, Chicago, IL 60606–6412) version 15.0 for Windows 7. The chi-squared test and Fisher’s exact test were used to determine among the three groups. Age was compared using the two-tailed t test. A p value under 0.05 was regarded as statistically significant.
Results
A total of 75 patients included in the study were divided into three groups: 25 patients in the CRC group, 25 patients in the CRAP group, and 25 subjects in the control group. The mean age of the patients in the study group was 59.49 ± 11.34 years. The mean age was 60.96 ± 12.18 years in the CRC group, 60.48 ± 10.31 years in the CRAP group, and 57.04 ± 10.60 in the control group. The three groups did not differ significantly with regards to age (p > 0.05). The proportion of male gender in the 75 subjects was 57.3 % (n = 43). In the CRC, CRAP, and control groups, 40 % (n = 10), 68 % (n = 17), and 64 % (n = 16) were males, respectively. (CRC M/F 10/15, CRAP M/F 17/8, control M/F 16/9). The characteristics of the three groups were summarized in Table 2. No significant difference was observed among the biochemical data of AURKB, AURKA, SETD8, PAK1, NEK6, KDM4C, HDAC1, and HDAC7 genes in all three groups, p > 0.05.
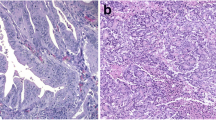
Colorectal cancers and gene expression analysis
In CRC patients (n = 25), AURKA, AURKB, HDAC1, HDAC7, NEK6, and PAK1 genes were overexpressed (fold change > 2) (Figs. 1 and 2), and the overexpression of the AURKA, AURKB, HDAC1, HDAC7, NEK6, and PAK1 genes was statistically significantly higher levels than the control group (p < 0.05) (Table 3) (Fig. 2). Sites of involvement of CRCs were assessed, and the majority of the tumors were located in the distal colon. The proportion of CRC patients by site of involvement were as follows: rectum 40 % (n = 10), sigmoid colon 28 % (n = 7), descending colon 4 % (n = 1), transverse colon 12 % (n = 3), ascending colon 8 % (n = 2), and cecum 8 % (n = 2). Pathological assessment demonstrated adenocarcinoma for all CRC patients. Of the patients, 28 % (n = 7) had poorly differentiated, 64 % (n = 16) had moderately differentiated tumors, and only 8 % (n = 2) had well-differentiated tumors. AURKA, AURKB, NEK6, PAK1, HDAC1, and HDAC7 genes were statistically significantly more overexpressed in poorly differentiated tumors than well and moderatelly differentiated tumors in the CRC (Table 4). The pathological classification and staging of CRC was in accordance with the American Joint Committee on Cancer (AJCC) tumor-node-metastasis (TNM) staging system (seventh edition, 2010). Of the patients, 68 % (n = 17) were in stage III and IV and 32 % (n = 17) were in stage I and II. AURKA, AURKB, NEK6, PAK1, HDAC1, and HDAC7 genes were statistically significantly more overexpressed in stage TNM III–IV than stage I–II in the CRC (Table 5). Of the patients, 40 % (n = 10) had higher than 5 ng/ml carcinoembryonic antigen (CEA) and 60 % (n = 15) lower than 5 ng/ml. There was no significant difference between higher than 5 ng/ml CEA and lower than 5 ng/ml CEA in the CRC group (Table 6).
The clustergram creates a heat map with dendrograms to indicate genes that are co-regulated. The color saturation reflects the magnitude of the change in gene expression. Green squares represent lower gene expression in the experimental samples (ratios <1); black squares represent genes equally expressed (ratios near 1); red squares represent higher than control levels of gene expression (ratios >1); gray squares indicate insufficient or missing data. The x-axis indicates the groups (CRC colorectal cancer, CRAP colorectal adenomatous polyp, CTR control group), and the y-axis indicates the genes
Colorectal adenomatous polyps and gene expression analysis
The patients with polyps (n = 25) AURKA, AURKB, NEK6, PAK1, and HDAC1 genes were statistically significantly more overexpressed compared to the control group (fold change > 2, p < 0.05). (Figs. 2 and 3 and Table 7). The comparison of the CRC and CRAP groups demonstrated that the HDAC1 and HDAC7 genes were statistically significantly more expressed in the former group (p < 0.05) (Table 8).
Most of the colorectal adenomatous polyps were located in the distal and left colon as a CRC. The proportions of patients with CRAP by the location of polyp were as follows: rectum 16 % (n = 4), sigmoid colon 36 % (n = 9), descending colon 24 % (n = 6), transverse colon 4 % (n = 1), and ascending colon 20 % (n = 5).
Gene expression analysis by pathological assessment
The patients with polyps (n = 25) were divided into three subgroups by pathological assessments as villous (32 %, n = 8), tubulovillous (40 %, n = 10), and tubular (28 %, n = 7) subgroups. Early onset adenocarcinoma foci or carcinoma and high-grade dysplasia were not observed in situ in any of the polyps.
The subgroups were compared both among themselves and to the control group for gene expressions. In the villous adenoma subgroup, AURKA, AURKB, PAK1, NEK6, HDAC1, and HDAC7 genes were overexpressed (fold change > 2). In the tubulovillous adenoma subgroup, AURKA, NEK6, and PAK1 genes were overexpressed (fold change > 2). However, inter-comparison of the subgroups did not yield a statistically significant difference (Tables 9 and 10).
Gene expression analysis by polyp diameter
The largest polyp diameter was 40 mm, and the smallest was 7 mm, and the mean polyp diameter was 16.72 ± 9.56 mm. The patients were divided into two subgroups by polyp diameter as ≥10 mm polyps (64 %, n = 16) and <10 mm polyps (36 %, n = 9). The extent of overexpression of AURKA, AURKB, PAK1, and NEK-6 and HDAC1 genes was statistically significantly greater in patients with polyp diameters ≥10 mm compared to those with polyp diameters <10 mm (Table 11).
Gene expression analysis by polyp morphological appearance
The patients were divided into two subgroups by macroscopic polyp classification with colonoscopy as sessile polyps (28 %, n = 7) and pedunculated polyps (72 %, n = 18). Patients with sessile polyps and pedunculated polyps did not differ statistically significantly (Table 12).
Discussion
Understanding of the epigenetic changes in cancer cells leads to important information on the stages of carcinogenesis [17]. Monitoring of precancerous and cancerous cells improves as our limited body of knowledge on cancer molecular biology expands [18, 19]. The fact that epigenetic alterations, in contrast to genetic ones, are reversible support, the concept of those epigenetic treatments may be used in the future [20].
PAK1 (p-21 activated kinase) coordinates RAS/RAF/MAPK and Wnt/β-catenin signaling in CRC by acting small GTPases [21–23]. There are no studies in the literature demonstrating PAK1 gene overexpression in the polyp tissue, which is a precancerous tissue for CRC.
The aurora kinase family (AURKA, AURKB, AURKC) is serine/threonine kinases involved as key regulators in mitosis and regulate the G2/M phase of the cell cycle. AURKA mRNA amplification has been established in many cancers including CRC [24–26]. A study described that high AURKA expression was associated with increased recurrence/relapse frequency [12]. NEK6 is a serine/threonine kinase from the never in mitosis gene a (NIMA) [27]. Studies have observed termination of mitotic division, chromatin spindle defects, abnormal chromosome differentiation, and apoptosis induction with NEK6 dysfunction [28–30]. There are no studies in the literature demonstrating NEK6, AURKA, and AURKB overexpression in the polyp tissue, which is a precancerous tissue for CRC. NEK6 and AURKA are overexpressed in esophagitis [31], and AURKA is overexpressed in Barrett’s esophagus [32]. A study by Katsha et al. found higher levels of AURKA in premalignant and malignant lesions compared to healthy gastric tissue [33]. There are studies which suggested that AURKA inhibitors could be developed as therapeutic agents for gastric cancer [33]. Nassirpour et al. have shown that the kinase activity of NEK6 was found to be increased in several cancer cells including colorectal cancer and that suppression of NEK6 resulted in tumor regression in a mice xenograft model [16].
HDACs are a critical family of proteins involved in the transcriptional regulation of a large number of genes and in the functional regulation of multiple proteins. Several studies have also examined HDAC expression in colon tumors. Most of these studies have reported increased expression of the HDAC1 and HDAC7 [11, 34]. Our findings are consistent with previous data in the villous adenoma subgroup and CRC patients that HDAC1 and HDAC7 were overexpressed (fold change > 2) (Figs. 1 and 2). But, HDAC1 and HDAC7 were not significantly different in other pathologic subgroups. Therefore, they may not be appropriate genetic markers for the early diagnosis of patients.
Current research suggests that PAK1, AURKA, NEK6, HDAC1, HDAC2, HDAC3, HDAC5, and HDAC7 genes play a key role in colorectal cancer carcinogenesis, and these genes is also an important prognostic and diagnostic marker in colorectal cancer and [8, 9, 12, 15, 16]. AURKA, AURKB, NEK6, PAK1, HDAC1, and HDAC7 was overexpressed in our study with poorly differentiated and advanced TNM. In light of the results, we speculate that these genes could be used as a prognostic marker in advanced CRC.
This is the first study which shows that PAK1, NEK6, AURKA, and AURKB genes are significantly overexpressed in polyp tissue. Our study was able to arrive at this conclusion despite the presence of major dysplasia only in two of the subjects with polyps. In light of the results reported from the studies mentioned above and those obtained in our study, we believe that these four genes have significant involvements in the stages of CRC progressing from polyps, and we further believe that these four histone modification enzyme genes can be used in anticancer treatments as therapeutic targets.
In adenomatous polyps, the risk of developing CRC is known to increase with increasing age, number of polyps, polyp diameter, villous component ratio, nuclear atypia frequency, increased dysplasia severity and sessile polyp presence, and familial history of CRC [2, 4]. The better understanding of these risk factors [2, 4] and their integration to clinical practice results in significant reductions in morbidity and mortality [35]. Our study demonstrated a significant relationship between PAK1, NEK6, AURKA, and AURKB gene overexpressions and increased polyp diameter, which is a risk factor for CRC cancer development in polyp tissue. Based on this result, we may speculate that colonoscopic screening recommended by several guidelines following polypectomy for polyps larger than 10 mm may be performed at shorter intervals if these markers are tested positive. The extent of overexpression of the PAK1, NEK6, AURKA, and AURKB genes increase with the presence and progression of villous component in the polyp, which is another risk factor, although a statistically significant relationship could not be shown in the subgroups. Significant reductions will be achieved in morbidity and mortality if genetic and epigenetic markers, which may be used in CRC screening of patients with CRAP, are integrated to clinical practice.
In conclusion, we demonstrated the overexpression of PAK1, NEK6, AURKA, and AURKB genes in patients with CRAP and CRC in the Turkish population. Elucidation of the molecular pathophysiology of CRC and CRAP will contribute to the treatment and prognosis of the diseases. Further studies are needed to understand the roles of these four genes in the CRC carcinogenesis. In addition, PAK1, NEK6, AURKA, and AURKB genes may be studied as promising genetic markers in new studies in different populations.
References
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917.
Shussman N, Wexner SD. Colorectal polyps and polyposis syndromes. Gastroenterol Rep (Oxf). 2014;2:1–15.
Leslie A, Carey FA, Pratt NR, Steele RJ. The colorectal adenoma-carcinoma sequence. Br J Surg. 2002;89:845–60.
Imperiale TF, Juluri R, Sherer EA, Glowinski EA, Johnson CS, Morelli MS. A risk index for advanced neoplasia on the second surveillance colonoscopy in patients with previous adenomatous polyps. Gastrointest Endosc 2014.
Jawad N, Direkze N, Leedham SJ. Inflammatory bowel disease and colon cancer. Recent Results Cancer Res. 2011;185:99–115.
Kulaylat MN, Dayton MT. Ulcerative colitis and cancer. J Surg Oncol. 2010;101:706–12.
Migheli F, Migliore L. Epigenetics of colorectal cancer. Clin Genet. 2012;81:312–8.
Stypula-Cyrus Y, Damania D, Kunte DP, Cruz MD, Subramanian H, Roy HK, et al. HDAC up-regulation in early colon field carcinogenesis is involved in cell tumorigenicity through regulation of chromatin structure. PLoS ONE. 2013;8, e64600.
Higashijima J, Kurita N, Miyatani T, Yoshikawa K, Morimoto S, Nishioka M, et al. Expression of histone deacetylase 1 and metastasis-associated protein 1 as prognostic factors in colon cancer. Oncol Rep. 2011;26:343–8.
Wilson AJ, Byun DS, Popova N, Murray LB, L’Italien K, Sowa Y, et al. Histone deacetylase 3 (HDAC3) and other class I HDACs regulate colon cell maturation and p21 expression and are deregulated in human colon cancer. J Biol Chem. 2006;281:13548–58.
Witt O, Deubzer HE, Milde T, Oehme I. HDAC family: what are the cancer relevant targets? Cancer Lett. 2009;277:8–21.
Belt EJ, Brosens RP, Delis-van Diemen PM, Bril H, Tijssen M, van Essen DF, et al. Cell cycle proteins predict recurrence in stage II and III colon cancer. Ann Surg Oncol. 2012;19 Suppl 3:S682–692.
Glauben R, Sonnenberg E, Zeitz M, Siegmund B. HDAC inhibitors in models of inflammation-related tumorigenesis. Cancer Lett. 2009;280:154–9.
Khare V, Lyakhovich A, Dammann K, Lang M, Borgmann M, Tichy B, et al. Mesalamine modulates intercellular adhesion through inhibition of p-21 activated kinase-1. Biochem Pharmacol. 2013;85:234–44.
He H, Huynh N, Liu KH, Malcontenti-Wilson C, Zhu J, Christophi C, et al. P-21 activated kinase 1 knockdown inhibits beta-catenin signalling and blocks colorectal cancer growth. Cancer Lett. 2012;317:65–71.
Nassirpour R, Shao L, Flanagan P, Abrams T, Jallal B, Smeal T, et al. Nek6 mediates human cancer cell transformation and is a potential cancer therapeutic target. Mol Cancer Res. 2010;8:717–28.
Feinberg AP, Ohlsson R, Henikoff S. The epigenetic progenitor origin of human cancer. Nat Rev Genet. 2006;7:21–33.
Lao VV, Grady WM. Epigenetics and colorectal cancer. Nat Rev Gastroenterol Hepatol. 2011;8:686–700.
Yi JM, Dhir M, Guzzetta AA, Iacobuzio-Donahue CA, Heo K, Yang KM, et al. DNA methylation biomarker candidates for early detection of colon cancer. Tumour Biol. 2012;33:363–72.
Yoo CB, Jones PA. Epigenetic therapy of cancer: past, present and future. Nat Rev Drug Discov. 2006;5:37–50.
He TC, Sparks AB, Rago C, Hermeking H, Zawel L, da Costa LT, et al. Identification of c-MYC as a target of the APC pathway. Science. 1998;281:1509–12.
Polakis P. The many ways of Wnt in cancer. Curr Opin Genet Dev. 2007;17:45–51.
Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M, et al. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988;319:525–32.
Marumoto T, Zhang D, Saya H. Aurora-A—a guardian of poles. Nat Rev Cancer. 2005;5:42–50.
Bischoff JR, Anderson L, Zhu Y, Mossie K, Ng L, Souza B, et al. A homologue of Drosophila aurora kinase is oncogenic and amplified in human colorectal cancers. EMBO J. 1998;17:3052–65.
Carvalho B, Postma C, Mongera S, Hopmans E, Diskin S, van de Wiel MA, et al. Multiple putative oncogenes at the chromosome 20q amplicon contribute to colorectal adenoma to carcinoma progression. Gut. 2009;58:79–89.
Jee HJ, Kim AJ, Song N, Kim HJ, Kim M, Koh H, et al. Nek6 overexpression antagonizes p53-induced senescence in human cancer cells. Cell Cycle. 2010;9:4703–10.
Belham C, Roig J, Caldwell JA, Aoyama Y, Kemp BE, Comb M, et al. A mitotic cascade of NIMA family kinases. Nercc1/Nek9 activates the Nek6 and Nek7 kinases. J Biol Chem. 2003;278:34897–909.
O’Regan L, Fry AM. The Nek6 and Nek7 protein kinases are required for robust mitotic spindle formation and cytokinesis. Mol Cell Biol. 2009;29:3975–90.
Cao X, Xia Y, Yang J, Jiang J, Chen L, Ni R, et al. Clinical and biological significance of never in mitosis gene A-related kinase 6 (NEK6) expression in hepatic cell cancer. Pathol Oncol Res. 2012;18:201–7.
Kasap E, Boyacioglu SO, Korkmaz M, Yuksel ES, Unsal B, Kahraman E, et al. Aurora kinase A (AURKA) and never in mitosis gene A-related kinase 6 (NEK6) genes are upregulated in erosive esophagitis and esophageal adenocarcinoma. Exp Ther Med. 2012;4:33–42.
Rugge M, Fassan M, Zaninotto G, Pizzi M, Giacomelli L, Battaglia G, et al. Aurora kinase A in Barrett’s carcinogenesis. Hum Pathol. 2010;41:1380–6.
Katsha A, Soutto M, Sehdev V, Peng D, Washington MK, Piazuelo MB, et al. Aurora kinase A promotes inflammation and tumorigenesis in mice and human gastric neoplasia. Gastroenterology. 2013;145:1312–22. e1311-1318.
Mariadason JM. HDACs and HDAC inhibitors in colon cancer. Epigenetics. 2008;3:28–37.
Winawer SJ, Zauber AG, Gerdes H, O’Brien MJ, Gottlieb LS, Sternberg SS, et al. Risk of colorectal cancer in the families of patients with adenomatous polyps. National Polyp Study Workgroup. N Engl J Med. 1996;334:82–7.
Acknowledgments
This study was supported by the Celal Bayar University Coordinator of the Scientific Research Projects (2013-10) Manisa, Turkey.
Compliance with ethical standards
ᅟ
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kasap, E., Gerceker, E., Boyacıoglu, S.Ö. et al. The potential role of the NEK6, AURKA, AURKB, and PAK1 genes in adenomatous colorectal polyps and colorectal adenocarcinoma. Tumor Biol. 37, 3071–3080 (2016). https://doi.org/10.1007/s13277-015-4131-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4131-6