Abstract
It has been previously shown that the simultaneous exposure of colon cancer cells MIP to irinotecan and secreted protein acidic and rich in cysteine (SPARC) enhances anticancer activity. However, whether there is same effect of SPARC in pancreatic cancer remains largely unknown. Therefore in this study, we aimed to investigate the role of SPARC played in the sensitivity of pancreatic cancer to gemcitabine. We first treated MIAPaCa2 and MIAPaCa2/SPARC69 cells with different concentrations of gemcitabine (2, 5, 10, and 20 μM) for 24, 48, and 72 h and selected the appropriated concentration for further study. Then we analyzed cell viability, cell cycle, and apoptosis and the levels of apoptosis-related proteins by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide, fluorescence-activated cell sorting and Western blot were used, respectively. In this study, we found that gemcitabine inhibited the proliferation of pancreatic cancer cells in a time- and dose-dependent manner. Overexpression of SPARC increased the inhibiting effect of gemcitabine on pancreatic cancer cells. The colony size of MIAPaCa2/SPARC69 was much smaller than that of MIAPaCa2/V. There was a G0/G1 arrest with significant increase of apoptosis after gemcitabine treatment in MIAPaCa2/SPARC69 cells. Furthermore, our results demonstrated that overexpression of SPARC markedly increased the levels of pro-apoptotic proteins in gemcitabine-treated pancreatic cancer cells. The SPARC can enhance the chemosensitivity of pancreatic cancer cells to gemcitabine via regulating the expression of apoptosis-related proteins. These results have shown that the SPARC/ gemcitabine combination treatment may be a potentially useful therapeutic option for individuals diagnosed with pancreatic cancer
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Pancreatic cancer is the eighth leading cause of cancer death in the world and the fourth leading cause of cancer death in USA [1]. Pancreatic cancer is classified into adenocarcinoma and neuroendocrine tumors based on the cell type it arises from. Adenocarcinoma is the most common type and accounts for 95 % of pancreatic cancers. The 5-year overall survival rate is under 5 % for all pancreatic cancer patients with combined stages, much lower than that for all other cancers [2].
Pancreatic cancer has the characteristics of occult symptom, strong invasive potential, and hard to be diagnosed at early stage. The vast majority of patients with pancreatic cancer are diagnosed at advanced stage. Only 10 to 15 % of pancreatic cancer patients are diagnosed early enough for surgical resection of cancer tissue [2]. Chemotherapy with gemcitabine becomes the standard treatment for retractable pancreatic cancers [3]. Unfortunately, most pancreatic cancers are not sensitive to chemotherapy and quickly become drug resistant after several rounds of chemotherapy, causing the survival rate having not been significantly improved. Therefore, increasing drug sensitivity of pancreatic cancer would be a viable strategy for treating advanced stage pancreatic cancers.
Secreted protein acidic and rich in cysteine (SPARC) expressed by pancreatic cancer stromal fibroblasts but not that by cancer cells is associated with poor prognosis [4]. Compared with pancreatic cancer cells, normal pancreatic stellate cells (PSCs) expressed high levels of SPARC, and knockdown SPARC in pancreatic ductal adenocarcinoma cells resulted in increased cell proliferation, transwell migration, and xenograft growth [5]. The lack of or depressed expression of SPARC in pancreatic cancer may be due to abnormal DNA methylation in the promoter region of SPARC gene [6, 7]. Pancreatic cancer cells could stimulate SPARC expression in fibroblasts from noncancerous pancreatic tissue in vitro [7]. Pancreatic tumors grew much faster in SPARC-null mice than in wild-type mice with decreased extracellular matrix deposition [8]. SPARC was found overexpressed in ovarian cancers with high stage, low differentiation, and lymph node metastasis. Knockdown SPARC expression in SKOV3-S1 and HO8910PM with shRNA significantly suppressed their proliferation, induced apoptosis, and inhibited invasion [9]. These data indicate that SPARC serves as a tumor suppressor in pancreatic cancers and some other types of cancer.
SPARC has been shown to express in nearly 68 % of pancreatic cancer patients [10]. It is involved in cancer onset, progression, reduction of tumor cell adhesion, degradation of the extracellular matrix (extracellular matrix, ECM), and tumor angiogenesis. SPARC can arrest cells at G1 phase [11] and induce apoptosis of tumor cells. Overexpression of SPARC increases the sensitivity of colon cancer to chemotherapy [12]. By using techniques including Western blot, colony formation assay, and flow cytometry, we demonstrated that SPARC could improve the therapeutic effects of gemcitabine on pancreatic cancer.
Material and methods
Cell culture
The cells used in this experiment were obtained from the American Type Culture Collection (Manassas, VA, USA) and cultured in Dulbecco’s modified Eagle’s medium (Invitrogen, Carlsbad, CA, USA) or RPMI1640 (Invitrogen), supplemented with 10 % fetal bovine serum (FBS; PAA Laboratories, Pasching, Austria), 10 U/ml penicillin, and 10 U/ml streptomycin, at 37 °C in a humidified atmosphere containing 5 % CO2.
Forced expression of SPARC in MIAPaCa2 cells
A modified lentivirus-based FG12 vector with a CMV promoter to introduce SPARC gene (NM003118.3) was expressed in MIA PaCa2 cells. After infection, the cells were sorted by fluorescence-activated cell sorting (FACS) to collect GFP-positive cells. The cells transfected with empty vector were used as control (MIA PaCa2/V). Cells were counted and seeded at the same initial density into 96-well plates. Gemcitabine were added into wells at the concentration of 2, 5, 10, and 20 μM. Each treatment was performed in triplicate.
MTT experiment
After cells were treated with gemcitabine (Lilly France) at specified concentration (10 μM) for 24, 48, and 72 h, 10 μg/ml of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) was added and incubated for 4 h protected from light. The MTT-treated cells were solved with 150 μl of DMSO (Invitrogen, Shanghai, China) and measured at 570 nm/630 nm. The rate of growth inhibition was calculated by 1 − ODtreatment/ODcontrol. The experiment was independently performed three times with four replicates each time.
Adhesion-dependent colony formation test
The MIAPaCa2, MIAPaCa2/V, and MIAPaCa2/SPARC69 cells were plated onto six-well plates for 24 h prior to drug treatment. Then, cells were incubated with 10 μM of gemcitabine for 24 h while same volume of vehicle was added into parallel wells as control. After 48 h, colonies were stained with Coomassie blue and the ones greater than 50 cells were counted. All experiments were repeated three times.
Cell cycle analysis
Cells were collected and washed twice with PBS, centrifuged at 500×g for 5 min, fixed with 70 % ethanol at 4 °C for 30 min followed by 1× washing with PBS. After digested with 50 μg/ml of RNase at 37 °C for 1 h, cells were stained with 100 μg/ml of propidium iodide (PI, Sigma, St Louis, MO) in dark for 60 min. Cell cycle distribution was analyzed on a BD LSRFortessa with ModFit program (BD Science, Shanghai, China).
Cell apoptosis analysis
Apoptosis was analyzed with an apoptosis detection kit from Sigma (St. Louis, MO) according to manufacturer’s instruction. Briefly, cells were washed twice with ice-cold PBS and resuspended in binding buffer to a cell density of 1 × 106/ml. Staining solution containing Annexin V/FITC was added to the cell suspension and incubated in the dark for 15 min and continued incubation for another 5 min more after the addition of PI. Cells were analyzed on a BD LSRFortessa with ModFit program (BD Science, Shanghai, China).
Western blot
The MIA PaCa2, MIA PaCa2/V, and MIAPaCa2/SPARC69 cells were inoculated in six-well plate and incubated with gemcitabine (10 μM) for 24 h. The cells were washed and lyzed in 100 μl of RIPA buffer (1 % NP-40, 0.1 % SDS, 50 mM Tris–HCl pH 7.4, 150 mM NaCl, 0.5 % sodium deoxycholate, 1 mM EDTA). Total protein was extracted by collecting the supernatant after centrifugation at 10,000×g for 30 min at 4 °C. The proteins were resolved on 10 % polyacrylamide gels and transferred onto nitrocellulose membranes. Membranes were blocked at room temperature in 5 % fat-free milk in TBST (50 mM Tris pH 7.6, 50 mM NaCl, 0.05 % Tween-20) for 1 h before incubated with antibodies against Bcl-2, caspase 2, caspase 8, or cleaved PARP (BD Bioscience, Shanghai, China) overnight at 4 °C. The membranes were washed three times with TBST and incubated with appropriate HRP-conjugated secondary antibody at room temperature for 1 h. The immunoreactive protein bands were visualized using an ECL kit (Pierce, Rockford, IL, USA).
Statistical analysis
The data were expressed as mean ± standard deviation. SPSS 16.0 statistical software was used for data analysis of variance (ANOVA) or independent sample t test; P < 0.05 was considered statistically significant.
Results
Overexpression of SPARC enhanced the inhibition of pancreatic cancer cell proliferation by gemcitabine
To evaluate the cytotoxicity of gemcitabine on MIAPaCa2 and overexpression of SPARC carcinoma cells (MIA PaCa2/SPARC69), we initially treated MIAPaCa2 with various doses of gemcitabine at different time points and evaluated cellular proliferation using the MTT assay. Gemcitabine inhibited MIAPaCa2 pancreatic cancer cells proliferation in a time- and dose-dependent manner. Its IC50 values at 24, 48, and 72 h were 40.1 ± 2.5, 15.0 ± 0.5, and 6.57 ± 0.1 μM, respectively (Fig. 1). Figure 2a demonstrates that SPARC enhances the inhibition effect of gemcitabine on cell MIA PaCa2 proliferation in a time-dependent manner. For MIAPaCa2/SPARC69 cells, the IC50 at 24, 48, and 72 h were 24.3 ± 1.5, 7.70 ± 0.3, and 4.8 ± 0.2 μM, respectively (Fig. 2a).
Dose- and time-dependent inhibition effect of gemcitabine on pancreatic cancer MIAPaCa2 cells. MIAPaCa2 cells were treated with 0 to 20 μM of gemcitabine for 24, 48, and 72 h. Cell proliferation inhibition was determined by MTT assay. Results were normalized against vehicle control and initial plating density. Experiments were done in triplicate wells per condition, and values (means ± S.E.M.) were representative of three independent experiments
SPARC enhances inhibition effect of gemcitabine on MIAPaCa2 cell proliferation in a time-dependent manner. MIAPaCa2/SPARC69 (a) cells were treated with 0 to 20 μM of gemcitabine for 24, 48, and 72 h followed by MTT analysis. b MIAPaCa2, MIAPaCa2/V, and MIAPaCa2/SPARC69 cells were treated with 10 μM gemcitabine for 24, 48, and 72 h and analyzed with MTT assay. The respective untreated cells were used as controls. Experiments were repeated at least three times. Results were presented as mean ± standard deviation. *P < 0.05 compared with the control cells
Since gemcitabine at a concentration of 20 μM showed significant toxicity, we therefore used 10 μM of gemcitabine in the experiments where we used in combination with SPARC (MIAPaCa2/SPARC69). After treating MIA PaCa2, MIA PaCa2/V, and MIA PaCa2/SPARC69 cells for 24, 48, and 72 h, MTT showed that the inhibition rate of MIAPaCa2/ SPARC69 cells by gemcitabine was significantly higher compared to that of MIAPaCa2 and MIAPaCa2/V cells at each time point (Fig. 2b).
The inhibition of SPARC and gemcitabine on pancreatic cancer was also test with adhesion-dependent colony formation assay. The treatment with gemcitabine resulted in significantly less colonies of MIAPaCa2/SPARC69 cells than those of MIAPaCa2 and MIAPaCa2/V cells (Fig. 3). Compared with the untreated groups, the number of colony of MIAPaCa2, MIAPaCa2/V, and MIAPaCa2/SPARC69 cells decreased 25, 30, and 50 %, respectively (Fig. 3).
SPARC increased the inhibition of gemcitabine on the colony formation of MIAPaCa2 cells. a Representative photographs of colonies of MIAPaCa2, MIAPaCa2/V, and MIAPaCa2/SPARC69 cells after treated with 10 μM gemcitabine. b Quantitative analysis of colony-formation assay. Experiments were repeated at least three times.*P < 0.05 compared with the control cells
SPARC overexpression increased G0/G1 arrest of pancreatic cancer cells by gemcitabine
To study the effects of SPARC and gemcitabine on cell cycle distribution, MIAPaCa2, MIAPaCa2/V, and MIAPaCa2/SPARC69 cells were treated with gemcitabine (10 μM) for 48 h. Cellular DNA was stained with propidium iodide and cell cycle distribution was studied by FACS analysis. As shown in Fig. 4, the populations of MIAPaCa2, MIAPaCa2/V, and MIAPaCa2/SPARC69 cells in the G0/G1 phase were 56, 55, and 68 % (P < 0.01 vs. MIAPaCa2 or MIAPaCa2/V, Fig. 4b), whereas cells in S phase were 33, 31, and 20 %, respectively. The portions of cells in G2/M phase were similar among three cell lines. A histogram representing this G0/G1 arrest is shown in Fig. 4a. These results indicate that SPARC enhances the effect of gemcitabine on cell cycle distribution of pancreatic carcinoma cells.
SPARC increased the portion of cells at G0/G1 stage after gemcitabine treatment. Cells were treated with 10 μM gemcitabine for 24 h. The cells were stained with propidium iodide and subjected to flow cytometry for the analysis of the percentage of cells in each group cell cycle phase. a Histograms showed number of cells per channel. b The values indicated the percentage of cells in the indicated phases of the cell cycle. Representative of at least three independent experiments done in triplicate wells per condition. *P < 0.05 compared with the control cells
SPARC overexpression increased cellular apoptosis induced by gemcitabine
To investigate if the observed sub-G1 peak was due to apoptosis, the cells were stained with propidium iodide (which binds late apoptotic cells) and Annexin V conjugated-FITC (which only binds early apoptotic cells). In cells, MIAPaCa2/SPARC69 for 48 h results in higher levels of apoptosis compared with MIAPaCa2 or MIA PaCa2/V. As can be seen in Fig. 5, the percentage of apoptotic cells induced by 10 μm of gemcitabine was 22.40 and 19.85 % in control and MIA PaCa2/V, respectively. Compared with control, the percentage of apoptotic cells induced by gemcitabine in MIAPaCa2/SPARC69 was significantly higher, up to 37.72 % (P < 0.01 vs. control or), which indicates that SPARC enhances the gemcitabine-induced apoptosis in MIA PaCa2 cells (Fig. 5).
SPARC enhanced gemcitabine-induced apoptosis in pancreatic cancer cells. Cells were treated with 10 μM gemcitabine and stained with Annexin V-FITC/propidium iodide before flow cytometric analysis for the analysis of the proportion of apoptotic cells. a The apoptosis rate of each group cells. b Graphic presentation of data obtained from Annexin V and propidium iodide staining assay. The values represented means and SE. Representative of at least three independent experiments done in triplicate wells per condition. *P < 0.05 compared with the control cells
SPARC increases apoptotic signals
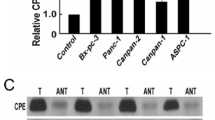
In order to understand the mechanism involved in combined activity of SPARC and gemcitabine on cell cycle distribution and apoptosis, we investigated the combination effect of SPARC and gemcitabine on the expression of proteins associated with apoptosis and cell cycle. As previously shown, there the expression of cyclinD1 remarkably decreased while the expression of P53 and P27kip dramatically increased in MIAPaCa2/SPARC69 (data not shown). After gemcitabine treatment, the levels of caspase 2, caspase 9, and cleaved caspase 8 proteins were significantly higher in MIAPaCa2/SPARC69 cells than that in MIAPaCa2 and MIAPaCa2/V cells (Fig. 6a). At the same time, there was no obvious change in the expression of Bcl-2 protein (Fig. 6b).
SPARC elevated the levels of pro-apoptotic proteins in gemcitabine-treated pancreatic cancer cells. a The levels of caspase 2, caspase 9, caspase 8 and cleaved PARP were significantly higher in MIAPaCa2/SPARC69 cells than those in MIAPaCa2 or MIAPaCa2/V cells after treatment with gemcitabine. b The level of Bcl-2 protein was no obvious change among MIAPaCa2/SPARC69, MIAPaCa2, and MIAPaCa2/V cells
Discussion
In SPARC-overexpressing MIAPaCa2/SPARC69 cells, gemcitabine showed much stronger inhibition of cell growth and triggered stronger apoptotic response partly due to G0/G1 arrest. MIAPaCa2/SPARC69 cells also had significantly less and smaller colonies after gemcitabine treatment compared to control MIAPaCa2 and MIAPaCa2/V cells. SPARC also markedly increased gemcitabine-induced expression of pro-apoptotic proteins in MIAPaCa2 cells, indicating that SPARC enhanced the sensitivity of MIAPaCa2 cells to gemcitabine.
Pancreatic cancer is an occult, invasive, and hard to diagnose malignancy with a 5-year survival rate of about 5 %. In recent years, the incidence of pancreatic cancer showed an upward trend, in which 85 % of the patients were diagnosed at late stages and lost the opportunity for radical surgery. Among all available chemotherapeutics, gemcitabine has become one of the first-line drugs in pancreatic cancer chemotherapy [13] due to its safety and excellent response rate. Unfortunately, pancreatic cancers in general are insensitive to chemotherapy reagents and easy to obtain resistance. Overall survival rate of pancreatic cancer patients has not been significantly improved over the years. Therefore, it is imperative to find ways to increase the chemosensitivity of pancreatic cancer.
Previous studies showed that SPARC could activate apoptotic pathway to accelerate tumor regression [14, 15]. Cellular apoptosis could be activated by both endogenous signaling pathway and exogenous signaling pathway [14, 15]. Most chemotherapy drugs induced cellular apoptosis through activation of endogenous signaling pathway [14]; however, more evidences suggested that exogenous apoptotic signaling pathway was also involved in chemotherapy-induced cell death. Evidence was found that SPARC could activate caspase 8-dependent signaling pathway to effectively increase apoptosis [16]. In Chan et al. experiments [17], their result showed that combined treatment with irinotecan, SPARC could enhance the chemosensitizing effects in CRCs through cell senescence, whether SPARC was endogenous or exogenous. These results implied that the expression level of SPARC in the malignant tumor might be an index of chemosensitivity to chemotherapy in some type of tumor.
In order to illuminate how SPARC increased gemcitabine-induced cell cycle arrest and apoptosis in MIAPaCa2 cells, we examined the levels of proteins critical for apoptosis signal pathways, such as caspase family proteins and substrate. The results showed that gemcitabine caused significant increase of caspase 2, caspase 8, caspase 9, and caspase 3 substrate cleaved PARP level in cells overexpressing SPARC. There was no obvious change in the expression of Bcl-2 protein. Chan et al. [17] demonstrated that the effect of SPARC promoted the cell senescence was p53 and p16INK4A dependent, which coincided with our previous works [18]. This result implies that there may be the same mechanism involved in the SPARC enhancing the chemosensitivity of pancreatic cancer cells to gemcitabine. These results clearly demonstrated that expression of SPARC in MIAPaCa2 cells enhances gemcitabine-induced cell cycle arrest and apoptosis.
In conclusion, SPARC sensitized pancreatic cancer cell line MIAPaCa2 to the treatment of gemcitabine. When treated with gemcitabine, SPARC-overexpressing MIAPaCa2 cells had higher inhibition and apoptotic rates in accompanying with G0/G1 arrest and elevated levels of caspases and cleaved PARP.
References
Hariharan D, Saied A, Kocher HM. Analysis of mortality rates for pancreatic cancer across the world. HPB (Oxford). 2008;10(1):58–62.
Chang MC, Wong JM, Chang YT. Screening and early detection of pancreatic cancer in high risk population. World J Gastroenterol. 2014;20(9):2358–64.
Antoniou G, Kountourakis P, Papadimitriou K, Vassiliou V, Papamichael D. Adjuvant therapy for resectable pancreatic adenocarcinoma: review of the current treatment approaches and future directions. Cancer Treat Rev. 2014;40(1):78–85.
Infante JR, Matsubayashi H, Sato N, Tonascia J, Klein AP, Riall TA, et al. Peritumoral fibroblast SPARC expression and patient outcome with resectable pancreatic adenocarcinoma. J Clin Oncol. 2007;25(3):319–25.
Chen G, Tian X, Liu Z, Zhou S, Schmidt B, Henne-Bruns D, et al. Inhibition of endogenous SPARC enhances pancreatic cancer cell growth: modulation by FGFR1-III isoform expression. Br J Cancer. 2010;102(1):188–95.
Zhang FX, Yang L, Li ZS, Zhang L, Gao J, Gong YF. SPARC gene expression in pancreatic cancer cell lines of its promoter methylation Ningxia. Med J. 2008;30(12):1087–8.
Sato N, Fukushima N, Maehara N, Matsubayashi H, Koopmann J, Su GH, et al. SPARC/osteonectin is a frequent target for aberrant methylation in pancreatic adenocarcinoma and a mediator of tumor-stromal interactions. Oncogene. 2003;22(32):5021–30.
Puolakkainen PA, Brekken RA, Muneer S, Sage EH. Enhanced growth of pancreatic tumors in SPARC-null mice is associated with decreased deposition of extracellular matrix and reduced tumor cell apoptosis. Mol Cancer Res. 2004;2(4):215–24.
Chen J, Wang M, Xi B, Xue J, He D, Zhang J, et al. SPARC is a key regulator of proliferation, apoptosis and invasion in human ovarian cancer. PLoS ONE. 2012;7(8):e42413.
Mason IJ, Taylor A, Williams JG, Sage H, Hogan BL. Evidence from molecular cloning that SPARC, a major product of mouse embryo parietal endoderm, is related to an endothelial cell ‘culture shock’ glycoprotein of Mr 43,000. EMBO J. 1986;5(7):1465–72.
Brekken RA, Sage EH. SPARC, a matricellular protein: at the crossroads of cell-matrix communication. Matrix Biol. 2001;19(8):816–27.
Tai IT, Dai M, Owen DA, Chen LB. Genome-wide expression analysis of therapy-resistant tumors reveals SPARC as a novel target for cancer therapy. J Clin Invest. 2005;115(6):1492–502.
Saif MW. Pancreatic cancer: is this bleak landscape finally changing? Highlights from the ‘43rd ASCO Annual Meeting’. Chicago, IL, USA. June 1–5, 2007. JOP. 2007;8(4):365–73.
Fulda S, Debatin KM. Apoptosis signaling in tumor therapy. Ann N Y Acad Sci. 2004;1028:150–6.
Yang BF, Lu YJ, Wang ZG. MicroRNAs and apoptosis: implications in the molecular therapy of human disease. Clin Exp Pharmacol Physiol. 2009;36(10):951–60.
Bast A, Krause K, Schmidt IH, Pudla M, Brakopp S, Hopf V, et al. Caspase-1-dependent and -independent cell death pathways in Burkholderia pseudomallei infection of macrophages. PLoS Pathog. 2014;10(3):e1003986.
Chan JM, Ho SH, Tai IT. Secreted protein acidic and rich in cysteine-induced cellular senescence in colorectal cancers in response to irinotecan is mediated by P53. Carcinogenesi. 2010;31(5):812–9.
Mao Z, Ma X, Fa X, Cui L, Zhu T, Qu J, et al. Secreted protein acidic and rich in cysteine inhibits the growth of human pancreatic cancer cells with G1 arrest induction. Tumor Biol. 2014;35(10):10185–93.
Acknowledgments
The authors would like to thank Dr. Shi Lei (Chi Biotechnology) for critical reading. This work was sponsored by The natural science foundation of Jiangsu Province (Youth Fund), grant number BK20130475; Zhenjiang Science and Technology Pillar Program, grant numbers SH2012030, SH2012031, and SH2014035; The Foundation for Young Scientists of affiliated Hospital of Jiangsu University (grant number JDFYRC2013009); post-doctoral research funding schemes of Jiangsu Province (grant number 1302096B); and Research innovation project of Jiangsu Province General University Graduate (CXLX13-688).
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Xin Fan and Zhengfa Mao contributed equally to this work.
Rights and permissions
About this article
Cite this article
Fan, X., Mao, Z., Ma, X. et al. Secreted protein acidic and rich in cysteine enhances the chemosensitivity of pancreatic cancer cells to gemcitabine. Tumor Biol. 37, 2267–2273 (2016). https://doi.org/10.1007/s13277-015-4044-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4044-4