Abstract
Patients with epithelial ovarian cancer (EOC) are at high risk of tumor recurrence. Human epididymis protein 4 (HE4) has been shown to be overexpressed in EOC. The primary aim of our study was to evaluate the role of HE4 in predicting recurrence in EOC patients. Furthermore, we assessed the role of HE4 in predicting recurrence after second-line chemotherapy. We retrospectively analyzed data of 92 out of 275 primary EOC patients of the multicenter project “Ovarian Cancer: Diagnosis of a silent killer” (OVCAD). The concentrations of HE4 and CA125 were determined preoperatively and 6 months after the end of platinum-based first-line chemotherapy (FU) using ELISA and Luminex technique, respectively. The role of HE4 and CA125 for prediction of recurrence was determined using receiver operating characteristics (ROC) curves. Out of 92 patients included, 70 (76 %) were responders and 22 (23 %) non-responders in terms of response to platinum-based first-line chemotherapy. Median HE4 concentrations at follow-up (FU) differed between responders and non-responders (60.5 vs. 237.25 pM, p = 0.0001), respectively. The combined use of HE4 and CA125 at FU with cut-off values of 49.5 pM and 25 U/ml for HE4 and CA125, respectively, for predicting recurrence within 12 months after first-line chemotherapy performed better than HE4 or CA125 alone (area under the curve (AUC) 0.928, 95 % confidence intervals (CI) 0.838–1, p < 0.001). HE4 at FU could predict recurrence within 6 months after second-line chemotherapy (AUC 0.719, 95 % CI 0.553–0.885, p = 0.024). The combination of both elevated biomarkers revealed significantly worse estimated median progression-free survival (PFS; hazard ratio (HR) 8.14, 95 % CI 3.75–17.68, p < 0.001) and slightly worse PFS in those in whom only one biomarker was elevated (HR 1.46, 95 % CI 0.72–2.96, p = 0.292) compared to those patients in whom no biomarker was elevated. For the estimated median overall survival (OS), our analysis revealed similar results. HE4 in combination with CA125 performed better than CA125 and HE4 alone in predicting recurrence within 12 months after first-line chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epithelial ovarian cancer (EOC) still accounts for the majority of deaths among all gynecologic malignant tumors in the industrialized world [1]. There is still a remarkable discrepancy in the prognosis between early (International Federation of Gynecology and Obstetrics (FIGO I–II)) and advanced (FIGO III–IV) stages of disease [2]. The majority (≥80 %) of EOC cases is diagnosed in advanced stages (FIGO III–IV) [3]. The standard upfront treatment for advanced EOC consists in primary cytoreductive surgery, i.e., debulking, followed by six courses of platinum-based chemotherapy [4]. The lack of reliable predictive biomarkers, the incomplete comprehension of its tumor biology, and the resistance to chemotherapy contribute to the poor prognosis and to high rates of EOC recurrence [5–9]. Most (80 %) of the advanced EOC patients relapse and develop chemotherapy resistance and finally die from the disease [10, 11]. FIGO stage has been shown to be one of the most important prognostic factors for the overall survival (OS) with 5-year survival rates for FIGO stages III–IV being 20–40 %, compared to 90 % in FIGO stage I [9].
Still, imaging and serum CA125 levels are the most often used methods to assess the response on primary EOC treatment [11–14]. A randomized trial (EORTC 55955) has questioned the value of monitoring patients for disease recurrence with CA125 and found that there is no survival benefit for early treatment based on increased CA125 levels alone [15]. However, this trial may be criticized because of the very low rate of secondary debulking at the time of relapse.
Human epididymis protein 4 (HE4) was first identified in the epithelium of the epididymis and initially predicted to be a protease inhibitor involved in sperm maturation but was also found to be overexpressed in EOC but not in normal ovarian tissue. Additionally, HE4 could predict disease recurrence prior to CA125 [2, 16, 17]. Despite the growing evidence that HE4 might be a biomarker of value for outcome prediction in ovarian malignant tumors [18–20], research of its usefulness in the prediction of treatment response claims further confirmation and is subject to currently ongoing research.
To date, there are no validated biomarkers to predict recurrence of EOC during or after primary chemotherapy [21]. The “Ovarian Cancer: Diagnosis of a silent killer” (OVCAD) study was a FP6 funded European project with the main aim of detecting predictive biomarkers for platinum response and minimal residual disease after primary debulking in EOC patients.
The primary aim of the current study was to assess the role of HE4 in predicting recurrence of disease in a subset of OVCAD patients, consisting of responders and non-responders for whom plasma values measured preoperatively and in the follow-up (FU) were available. Our secondary aim was to assess the role of HE4 in the follow-up in predicting response to second-line chemotherapy.
Patients and methods
Study design
We retrospectively analyzed data and performed biomarker measurements in stored plasma samples in a subset of patients of the OVCAD study. In this multicenter study, patient recruitment was performed by five comprehensive centers for gynecologic oncology (Department of Gynecology, Charité-Medical University, Berlin; Department of Gynecology and Gynecologic Oncology, Katholieke Universiteit Leuven; Department of Gynecology, University Center Hamburg; Department of Obstetrics and Gynecology, Medical University Vienna; and Department of Obstetrics and Gynecology, Medical University Innsbruck) [21].
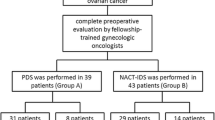
A total of 602 patients with suspected pelvic tumors were screened between February 2005 and December 2008. Out of these, a total of 399 patients had EOC. Two hundred seventy-five patients fulfilled all inclusion criteria: primary FIGO II to IV EOC, radical cytoreductive surgery (consisting of hysterectomy, bilateral salpingo-oophorectomy, peritoneal washings, omentectomy, appendectomy, lymphadenectomy, and subtotal peritonectomy) followed by platinum-based chemotherapy (first-line chemotherapy). FIGO I cases were excluded due to their excellent prognosis [21].
The study protocol was approved by the local ethics committees of the participating OVCAD partners (EK207/2003, ML2524, HEK190504, EK366, and EK260). All patients gave their written informed consent prior to inclusion into the study.
Response to platinum-based chemotherapy
Response to treatment and diagnosis of recurrence was determined according to the “Response Evaluation Criteria In Solid Tumours” (RECIST) criteria or according to CA125 variations (GCIG-criteria) [22, 23]. Patients with recurrence during primary therapy or within 6 months after primary therapy were defined as non-responders [24]. Progression-free survival (PFS) was calculated as time from initial diagnosis to recurrence of disease and overall survival (OS) as time from initial diagnosis to death or loss to follow-up.
Sample collection
For the present study, we retrospectively identified 92 out of the 275 OVCAD patients in whom preoperative and follow-up (FU) plasma samples for analyzing HE4 and CA125 were available. In the present study, FU was defined as follows: for responders, it was the day of plasma collection 6 months after the end of last platinum-based first-line chemotherapy cycle, while for non-responders, it was the day of plasma collection on the day of first recurrence.
Sample processing
After centrifugation and aliquotation into cryovials, all plasma samples were frozen at −80 °C until further use. HE4 plasma concentration was measured using the HE4 EIA assay (Fujirebio Diagnostics AB, Gothenburg, Sweden). Each sample was analyzed in duplicate. CA125 plasma concentration was measured in plasma from patients using the Luminex technique. Samples were analyzed following the instruction of the MILLIPLEX MAP Kit (Cancer Biomarker Panel, Cat: 48–020).
Statistical analysis
All clinical and pathological data were collected and entered in an SPSS database. All statistical analyses were performed with IBM SPSS Statistics, Version 21.0 (SPSS, Inc., Chicago, IL). Continuous variables were summarized by the median and range, and all other variables were presented as frequency with percentage. Non-normal distributed continuous data were compared using the Mann-Whitney U test and the Wilcoxon signed-rank test.
The predictive values of HE4 and CA125 for recurrence within the subsequent 6 months since plasma collection were determined using receiver operating characteristics (ROC) curves. To adjust for patient’s age and biomarker values at FU, a logistic regression model was performed for prediction of recurrence or death in responders. To maximize prediction accuracy, a stepwise multiple regression model was applied. Estimates of OAS and PFS rates and 95 % confidence intervals (95 % CI) were calculated using the Kaplan-Meier method. Log-rank tests were used for univariate statistical comparisons. Adjusted hazard ratios and 95 % CI were estimated with the Cox proportional hazards model. A two-tailed p value of <0.05 was considered statistically significant.
Results
Patient’s characteristics
Out of 92 patients included in the current study, 70 (76 %) were responders and 22 (23 %) were non-responders. The median age at time of initial diagnosis was 56 years (range 18–80 years) in responders and 59.5 years (range 27–81 years) in non-responders, respectively. The majority of responders and non-responders presented with serous histological type (82.9 and 100 %, respectively), FIGO stage III (82.9 and 68.2 %, respectively), and grade 3 tumors (70 and 72.7 %, respectively). Most of the patients received optimal cytoreductive surgery in terms of no macroscopical tumor residuals (Table 1) followed by platinum-based first-line chemotherapy.
HE4 and CA125 concentrations
For the 92 patients included in the study, 79 preoperative HE4 plasma samples were available (missing values, 10 for responders and 3 for non-responders, respectively). At FU, HE4 plasma samples were available for all patients. For CA125, three preoperative values were missing (two for responders and one for non-responders), while for CA125 at FU, ten values were missing (eight for responders and two for non-responders, respectively). Median HE4 and CA125 in responders and non-responders are shown in Table 1.
Median HE4 values preoperatively and at FU differed significantly (p = 0.0001) between responders and non-responders.
Median CA125 values preoperatively and at FU differed also significantly (p = 0.0001) between responders and non-responders.
Prediction of recurrence or death in all patients based on preoperative values
The prediction of recurrence or death in the first year after the last cycle of platinum-based first-line chemotherapy based on preoperative HE4 and CA125 values was performed for all patients (responders and non-responders).
Our analyses revealed that 36 out of the 79 patients in whom preoperative HE4 values were available experienced either recurrence or death in the first year after the last cycle of platinum-based first-line chemotherapy. The area under the curve (AUC) for predicting recurrence based on preoperative HE4 values was 0.658 (95 % CI 0.535–0.781, p = 0.016). With a cut-off-value of 165 pM, a sensitivity of 86.1 % and a specificity of 34.9 % could be reached.
Our analyses revealed that 41 out of the 89 patients in whom preoperative CA125 values were available experienced either recurrence or death in the first year after the last cycle of platinum-based first-line chemotherapy. The AUC for CA125 was 0.623 (95 % CI 0.506–0.74, p = 0.046). At a cut-off-value of 400 U/ml, a sensitivity of 80.7 % and a specificity of 50 % could be reached.
Prediction of recurrence or death in responders based on values at FU
The prediction of recurrence or death in the first year after the last cycle of platinum-based first-line chemotherapy based on HE4 and CA125 values was performed for responders.
Receiver operator characteristic (ROC) analysis for HE4 at FU showed that at a cut-off value of 49.5 pM, a sensitivity of 100 % and a specificity of 49.0 % could be reached for predicting recurrence within 12 months after the end of platinum-based first-line chemotherapy (AUC 0.810, p < 0.001, 95 % CI 0.704–0.917).
CA125 values at FU were available for 62 patients. Recurrence was subsequently detected in 19 patients within 12 months after the end of platinum-based first-line chemotherapy. With a cut-off value of 20 U/ml, a sensitivity of 78.9 % and a specificity of 90.7 % could be reached (AUC 0.884, p < 0.001, 95 % CI 0.770–0.999).
The combined use of HE4 and CA125 at FU for predicting recurrence within 12 months after the end of platinum-based first-line chemotherapy performed better than either using CA125 or HE4 alone: with cut-off values of 49.5 pM for HE4 and 25 U/ml for CA125, a sensitivity of 73 % and a specificity of 100 % could be reached (AUC 0.93, 95 % CI 0.86–1, p < 0.001; Fig. 1). After adjustment for patient’s age, HE4 at FU and CA125 at FU, respectively, the performance of the biomarker combination for prediction of recurrence at FU remained better than the single biomarker use (AUC 0.928, 95 % CI 0.838–1, p < 0.001).
Ratio-based prediction of recurrence or death in responders
For the prediction of recurrence or death in responders in the first year after the last cycle of platinum-based first-line chemotherapy, ratios between biomarker values at FU and preoperatively were calculated.
Based on the ratio “HE4 at FU/preoperative HE4,” 17 out of 59 responders that experienced recurrence or death in the first year after last cycle of platinum-based first-line chemotherapy could be detected. At a cut-off value of 0.247, a sensitivity of 82.4 % and a specificity of 59.5 % could be reached (AUC 0.754, 95 % CI 0.610–0.897, p = 0.002).
Based on the ratio “CA125 at FU/preoperative CA1254,” 19 out of 42 responders that experienced recurrence or death in the first year after last cycle of platinum-based first-line chemotherapy could be detected. At a cut-off-value of 0.015, a sensitivity of 89.5 % and a specificity of 45.2 % could be reached (AUC 0.733, 95 % CI 0.597–0.869, p = 0.04).
Prediction of recurrence or death in non-responders
The predictive role of HE4 at FU for prediction of recurrence in the first 6 months after second-line chemotherapy was performed for 22 non-responders. Our analysis revealed an AUC of 0.871 (95 % CI 0.703–1, p = 0.01). For an HE4 cut-off value of 220 pM, a sensitivity of 90 % and a specificity of 71.4 % could be reached. For CA125, the AUC was the same as for HE4 (AUC 0.871, 95 % CI 0.699–1, p = 0.01). A CA125 cut-off value of 60 U/ml was needed to reach a sensitivity of 100 % and a specificity of 57.1 %.
In a stepwise regression for the risk of recurrence within the first 6 months after second-line chemotherapy, we found that with increasing values of CA125, the risk of experiencing a recurrence was rising significantly (hazard ratio (HR) 3.16, 95 % CI 1.06–9.41, p = 0.038), while there was no additional predictive value for HE4 and patient’s age. Furthermore, we found a strong correlation between CA125 and HE4 (Spearman’s rho coefficient 0.76).
Prediction of response to platinum-based second-line chemotherapy based on values at FU
Our analyses revealed that out of 38 responders, 15 experienced their second recurrence or died within 6 months after the last cycle of platinum-based second-line chemotherapy.
In patients with a second recurrence within 6 months after platinum-based second-line chemotherapy, the HE4 cut-off value of 50 pM reached a sensitivity of 93.3 % and a specificity of 43.5 % (AUC 0.719, 95 % CI 0.553–0.885, p = 0.024; Fig. 2). In contrast, with a cut-off value of 80 pM, a sensitivity of 80 % but a specificity of 69.6 % could be reached.
In patients with a second recurrence within 6 months after platinum-based second-line chemotherapy, the CA125 cut-off value of 11.5 U/ml reached a sensitivity of 71.4 % and specificity of 47.6 %., while a cut-off value of 19.99 U/ml rendered a sensitivity of 57.1 % and a specificity of 61.9 % (AUC 0.53, 95 % CI 0.325–0.73, p = 0.788).
Survival analysis for responders
In the univariate analysis, the estimated median PFS times differed significantly (p < 0.001) between the three groups. The combination of both elevated biomarkers revealed significantly worse estimated median PFS (HR 8.14, 95 % CI 3.75–17.68, p < 0.001) and slightly worse PFS in those in whom only one biomarker was elevated (HR 1.46, 95 % CI 0.72–2.96, p = 0.292) compared to those patients in whom no biomarker was elevated (Fig. 3).
The estimated median OS was worse for patients in whom both biomarkers were elevated (HR 17.96, 95 % CI 4–80.85, p < 0.001) and slightly worse in those in whom only one biomarker was elevated (HR 3.55, 95 % CI 0.75–16.76, p = 0.11) compared to patients in whom no biomarker was elevated (Fig. 4).
Regarding PFS and OS, the combination of both biomarkers being elevated remained significant (p = 0.001) in the multivariate analysis after adjusting for age, FIGO stage, histological type, amount of ascites, and postoperative tumor burden.
Survival analysis for non-responders
Our univariate analysis revealed that with increasing CA125 and HE4 concentrations, the estimated median survival times for PFS decreased significantly (p = 0.001). In a stepwise Cox regression model, a cut-off value of CA125 >400 U/ml remained a significant predictive factor for PFS while age and HE4 did not have any additional value.
For the OS, the estimated median times did not show any significant differences with increasing concentrations of HE4 and CA125 (p = 0.17 and p = 0.87, respectively). In a stepwise Cox regression model, no significant predictors were found.
Due to the small number of events, we did not perform a multivariate analysis for OS and PFS.
Discussion
A clinically relevant question in the debate about the appropriate surveillance after upfront treatment of primary EOC is whether early detection of recurrent disease improves survival. The major findings of our study were that the highest prediction for first recurrence within 12 months after the end of platinum-based first-line chemotherapy was achieved by the combined use of both biomarkers at FU. We therefore suggest that the combined use of both HE4 and CA125 may constitute a valuable tool for the prediction of EOC recurrence in responders. Furthermore, our results indicated that HE4 performed better than CA125 in predicting second recurrence after platinum-based second-line chemotherapy.
The role of CA125 as a marker for disease recurrence in patients undergoing curative intent resection of primary EOC has been investigated in extenso [15]. New and innovative approaches are needed to detect earlier recurrence and develop treatment strategies. The measurement of plasma CA125 levels in women with advanced EOC has become a standard component in current clinical practice. However, the question remains if there is any advantage in routine monitoring of CA125 in women with advanced EOC in complete remission. In a randomized controlled trial, Rustin et al. showed that women treated for recurrent EOC detected by elevated CA125 levels did not have a better outcome than those who waited to be treated after the onset of clinical symptoms several months later [15]. New monitoring biomarkers that may not only be increased in widespread disease are therefore needed in future. In the study of Rustin et al., most of the patients received systemic therapy as treatment of relapsed EOC [15]. Although data from prospective, randomized studies are missing, there might be a benefit in detecting patients with minimal tumor residuals who could benefit from a secondary cytoreduction. Currently, the DESKTOP III study (Identifier: NCT01166737), a prospective randomized study, analyzing the role of systemic treatment versus cytoreductive surgery in preselected first relapsed ovarian cancer patients is still ongoing. Several previous studies have shown that HE4 has great potential to serve as an efficient tool for anticipation of disease recurrence [1, 2, 4, 11, 25, 26]. In a study by Plotti et al., the best HE4 cut-off value to detect recurrence of ovarian cancer was 67.1 pM [2]. Furthermore, they revealed that the combination of CA125 with HE4 at a cut-off value of 70 pM renders a sensitivity of 76.47 % and a specificity of 100 % to assess the recurrence of EOC [2]. Although Plotti et al. used patients with benign adnexal pathology as a control group in their study, our results are in line with theirs regarding the fact that CA125 in combination with HE4 achieves high specificity in predicting disease recurrence. Havrilesky et al. monitored 27 patients who experienced recurrent ovarian cancer and found that the sensitivity in predicting disease recurrence was 100 % considering a biomarker panel, consisting of HE4, MMP7, and glycodelin, and 96 % for CA125 alone [3]. It needs to be emphasized that the studies of Plotti et al. and Havrilesky et al. (in accordance with our study) used biomarker values based on pretreatment analyses and on the follow-up situation to predict disease recurrence. In addition, Havrilesky et al. used a combination of several biomarkers, while we focussed on CA125 and HE4 values only. The use of HE4 as an early predictor of disease recurrence was, however, also supported by Anastasi et al. [11]. One of their aims was to investigate the role of HE4 as indicator of disease recurrence in patients followed up for 20 months after EOC diagnosis [11]. They noticed an increase of HE4 5–8 months before the increase of CA125 in five of eight patients [11]. Although being a clinically important finding, it has to be interpreted with caution since the number of patients was very low (n = 8) during the follow-up [11].
In the study by Angioli et al., CA125 and HE4 were measured at different time points: before first cycle of chemotherapy, and at third and sixth cycle; after the sixth cycle, the samples were collected every 3 months until the sixth months of follow-up [4]. Angioli et al. found that the HE4 profile was significantly associated with platinum-based chemotherapy response, while CA125 values during chemotherapy turned out to not be statistically significant in regard to prediction of platinum response [4]. They found HE4 levels >70 pM in 36 of 36 cases and in 6 of 40 cases in platinum-sensitive/intermediate patients (sensitivity = 100 %, specificity = 85 %) at third cycle in platinum-resistant patients, concluding that the time needed for HE4 normalization during initial chemotherapy may allow the identification of non-responders after the third cycle [4]. In a study by Manganaro et al., each patient gave three serum samples taken at 3-month intervals: time interval I (1–3 months from surgery), time interval II (4–6 months from surgery), and time interval III (7–10 months from surgery) [25]. In patients with EOC recurrence, an increment in HE4 was seen in 22, 78, and 89 % of patients within the time intervals I, II, and III, respectively [25]. Positive values for CA125 were seen later in the course (at time interval III) and only in 44 % of patients [25]. The authors therefore concluded that, in case of disease recurrence, increased levels of HE4 may precede an elevation in CA125 by approximately 3 months [25]. Angioli et al. [4] and Manganaro et al. [25] used biomarker measurements after surgery with different time points, elucidating the dynamics of changes in biomarker concentrations over time. In our study, we also observed tumor marker expression changes in the same patients both before and after chemotherapy and in the follow-up period. Each patient served as her own control, thus limiting the selection bias when comparing samples collected before and after chemotherapy.
To the best of our knowledge, there is only a scant amount of literature elucidating the role of HE4 in the context of prediction of recurrence as well as its role for prediction of response to second-line chemotherapy. The elevation of markers in the follow-up may have hazardous effects on patients’ well-being since the burden of anxiety and uncertainty it may have [26]. Furthermore, the question remains which advantages each patient might have in case of an earlier detection of disease recurrence, particularly in terms of OS, PFS, and quality of life [26]. Basically, this question depends once more on the efforts to find a reliable surrogate marker that helps to avoid unnecessary interventions but leads us to those cases where intervening will benefit the patient. Regarding the possible benefit of cytoreductive surgery in patients with suspicion of first recurrence of disease, the ongoing DESKTOP III trial (Identifier: NCT01166737) will hopefully bring valuable contributions regarding this issue.
Although the combined use of HE4 and CA125 for the follow-up setting has been approved by the FDA [26, 27], there is still lack of evidence regarding its role in recurrent cases, and a broad uncertainty regarding the use of HE4 as a diagnostic and follow-up biomarker among European countries and around the globe [26]. We therefore consider the current study as a contribution to encounter the existing uncertainty and diversity regarding the use of HE4 as a biomarker in the follow-up setting as well as to encourage further research in this field.
There are several limitations of our study, such as the fact that we only focused on two points of time for biomarker measurement and that a separate control group was lacking to validate our results. Our results basically apply for the group of responders. The number of events in the group of non-responders was too small to allow for a multivariate analysis. Hence, the results of our univariate survival analysis in this group have to be interpreted with caution. Despite those limitations, our results indicate that even after adjustment for possible confounders, the combined use of HE4 and CA125 remained stronger than the single use of either biomarker alone in predicting disease recurrence in the group of responders. Furthermore, our retrospective analyses are based on a homogenous cohort of patients that were included in the prospective, multicenter OVCAD study. The OVCAD study defined strict inclusion and exclusion criteria and precise standard operating procedures (SOP) for tissue processing for all five included gynecologic oncology centers, thus leading to a high internal validity of the results.
Conclusion
Our study showed that the combination of HE4 and CA125 may help to identify responders at risk for disease recurrence. Furthermore, HE4 appears to be a valuable biomarker to predict recurrence after the end of second-line chemotherapy. To validate our results, further prospective multicenter studies are needed.
References
Granato T, Midulla C, Longo F, Colaprisca B, Frati L, Anastasi E. Role of HE4, CA72.4, and CA125 in monitoring ovarian cancer. Tumour Biol. 2012;33(5):1335–9.
Plotti F, Capriglione S, Terranova C, Montera R, Aloisi A, Damiania P, et al. Does HE4 have a role as biomarker in the recurrence of ovarian cancer? Tumour Biol. 2012;33(6):2117–23.
Havrilesky LJ, Whitehead CM, Rubatt JM, Cheek RL, Groelke J, He Q, et al. Evaluation of biomarker panels for early stage ovarian cancer detection and monitoring for disease recurrence. Gynecol Oncol. 2008;110(3):374–82.
Angioli R, Capriglione S, Aloisi A, Guzzo F, Luvero D, Miranda A, et al. Can HE4 predict platinum response during first-line chemotherapy in ovarian cancer? Tumour Biol. 2014;35(7):7009–15.
Harter P, Muallem ZM, Buhrmann C, Lorenz D, Kaub C, Hils R, et al. Impact of a structured quality management program on surgical outcome in primary advanced ovarian cancer. Gynecol Oncol. 2011;121(3):615–9.
Chang SJ, Bristow RE. Evolution of surgical treatment paradigms for advanced-stage ovarian cancer: redefining ‘optimal’ residual disease. Gynecol Oncol. 2012;125(2):483–92.
Chi DS, Bristow RE, Armstrong DK, Karlan BY. Is the easier way ever the better way? J Clin Oncol. 2011;29(31):4073–5.
Bristow RE. Surgical standards in the management of ovarian cancer. Curr Opin Oncol. 2000;12(5):474–80.
Braicu EI, Fotopoulou C, Van Gorp T, Richter R, Chekerov R, Hall C, et al. Preoperative HE4 expression in plasma predicts surgical outcome in primary ovarian cancer patients: results from the OVCAD study. J Gynecol Oncol. 2013;128(2):245–51.
Haries M, Gore M. Part I: chemotherapy for epithelial ovarian cancer-treatment at first diagnosis. Lancet Oncol. 2002;3:529–36.
Anastasi E, Marchei GG, Viggiani V, Gennarini G, Frati L, Reale MG. HE4: a new potential early biomarker for the recurrence of ovarian cancer. Tumour Biol. 31(2):113–9.
Drapkin R, von Horsten HH, Lin Y, Mok SC, Crum CP, Welch WR, et al. Human epididymis protein 4 (HE4) is a secreted glycoprotein that is overexpressed by serous and endometrioid ovarian carcinomas. Cancer Res. 2005;65:2162–9.
McIntosh MW, Drescher C, Karlan B, Scholler N, Urban N, Hellstrom KE, et al. Combining CA 125 and SMR serum markers for diagnosis and early detection of ovarian carcinoma. Gynecol Oncol. 2004;95:9–15.
Galgano MT, Hampton GM, Frierson Jr HF. Comprehensive analysis of HE4 expression in normal and malignant human tissues. Mod Pathol. 2006;19:847–53.
Rustin GJ, van der Burg ME, Griffin CL, Guthrie D, Lamont A, Jayson GC, et al. Early versus delayed treatment of relapsed ovarian cancer (MRC OV05/EORTC 55955): a randomised trial. Lancet. 2010;376(9747):1155–63.
Grover S, Quinn MA, Weidemann P, Koh H. Factors influencing serum CA 125 levels in normal women. Obstet Gynecol. 1992;79(4):511–4.
Kirchhoff C. Molecular characterization of epididymal proteins. Rev Reprod. 1998;3(2):86–95. Review.
Lu R, Sun X, Xiao R, Zhou L, Gao X, Guo L. Human epididymis protein 4 (HE4) plays a key role in ovarian cancer cell adhesion and motility. Biochem Biophys Res Commun. 2012;419(2):274–80.
Park Y, Lee JH, Hong DJ, Lee EY, Kim HS. Diagnostic performances of HE4 and CA125 for the detection of ovarian cancer from patients with various gynecologic and non-gynecologic diseases. Clin Biochem. 2011;44(10–11):884–8.
Speeckaert MM, Speeckaert R, Delanghe JR. Human epididymis protein 4 in cancer diagnostics: a promising and reliable tumor marker. Adv Clin Chem. 2013;59:1–21.
Chekerov R, Braicu I, Castillo-Tong DC, Richter R, Cadron I, Mahner S, et al. Outcome and clinical management of 275 patients with advanced ovarian cancer International Federation of Obstetrics and Gynecology II to IV inside the European Ovarian Cancer Translational Research Consortium-OVCAD. Int J Gynecol Cancer. 2013;23(2):268–75.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92(3):205–16.
Rustin GJ, Vergote I, Eisenhauer E, Pujade-Lauraine E, Quinn M, Thigpen T, et al. Definitions for response and progression in ovarian cancer clinical trials incorporating RECIST 1.1 and CA 125 agreed by the Gynecological Cancer Intergroup (GCIG). Int J Gynecol Cancer. 2011;21(2):419–23.
Friedlander M, Butow P, Stockler M, Gainford C, Martyn J, Donovan OA, et al. Symptom control in patients with recurrent ovarian cancer: measuring the benefit of palliative chemotherapy in women with platinum refractory/resistant ovarian cancer. Int J Gynecol Cancer. 2009;19(Supp 2):S44–8.
Manganaro L, Michienzi S, Vinci V, Falzarano R, Saldari M, Granato T, et al. Serum HE4 levels combined with CE CT imaging improve the management of monitoring women affected by epithelial ovarian cancer. Oncol Rep. 2013;30(5):2481–7.
Piovano E, Attamante L, Macchi C, Cavallero C, Romagnolo C, Maggino T, et al. The role of HE4 in ovarian cancer follow-up: a review. Int J Gynecol Cancer. 2014;24(8):1359–65.
Ledermann JA, Raja FA, Fotopoulou C, Gonzalez-Martin A, Colombo N, Sessa C, et al. Newly diagnosed and relapsed epithelial ovarian carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24 Suppl 6:vi24–32.
Acknowledgments
This work is part of a Master’s thesis of the Master’s Program in Clinical Research, Center for Clinical Research and Management Education, Division of Health Care Sciences, Dresden International University, Dresden, Germany. Dr. Elena Ioana Braicu is a participant of the Charité Clinical Scientist Program funded by the Charité Universitätsmedizin Berlin and the Berlin Institute of Health.
Conflicts of interest
This study was performed within the OVCAD FP6 European Project. The sample analysis was performed by Fujirebio Diagnostics AB, Sweden. Christina Hall is an employee of Fujirebio Diagnostics AB in Sweden. Dr. Elena Ioana Braicu is a participant of the Charité Clinical Scientist Program funded by the Charité Universitätsmedizin Berlin and the Berlin Institute of Health. The other authors declare no conflicts of interest in regard to the present study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nassir, M., Guan, J., Luketina, H. et al. The role of HE4 for prediction of recurrence in epithelial ovarian cancer patients—results from the OVCAD study. Tumor Biol. 37, 3009–3016 (2016). https://doi.org/10.1007/s13277-015-4031-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4031-9