Abstract
This study aims to assess the association of the preoperative neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) with tumor stage in colorectal cancer (CRC) patients. A retrospective study was performed in 336 CRC patients. Preoperative whole blood counts, serum levels of carcinoembryonic antigen (CEA), and clinicopathologic data were collected. The correlations between laboratory parameters and the tumor, node, and metastasis (TNM) stages were analyzed. The clinicopathologic TNM stages among CRC patients were 12.8 % at stage I, 32.4 % at stage II, 44.6 % at stage III, and 10.1 % at stage IV. NLR, PLR, and CEA levels were higher in CRC patients compared to healthy controls (all P < 0.0001). Both NLR and PLR showed an early elevation as compared to CEA, with a higher area under curve (AUC) value (0.71 vs. 0.62) in predicting the presence of the tumor with stage I/II. Accordingly, significant elevations of NLR (P = 0.0018) and PLR (P < 0.0001) were firstly detected in stage I and stage II, respectively. In addition, NLR exhibited a second phase elevation in stage IV, with a significant higher level in M1 subgroup compared to M0 subgroup (P = 0.022). While PLR showed a T stage-dependent increase (P = 0.0003) and was identified as an independent factor for the T grade development (P < 0.0001). Our data indicated that both neutrophil- and platelet-mediated inflammatory reactions are predominantly involved in the different stages of CRC development. Determination of pretreatment levels of NLR and PLR might provide useful information for the early diagnosis or the therapeutic choices in CRC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is one of the most common types of cancer worldwide. Due to the changes in lifestyle, the incidence of CRC in previously low-risk countries, such as China and some countries in eastern Europe, is rapidly increased in recent years [1, 2]. Despite the advancement of new therapeutic strategies in surgery, neoadjuvant radiotherapy and adjuvant chemotherapy, the overall prognosis of advanced CRC is still poor, with a 5-year survival rate less than 12 % [1, 3].
Effective treatment of CRC is largely relied on the early diagnosis and the precise therapeutic plan. The most efficient method for the diagnosis of CRC is endoscopy. However, its general application as a routine screening tool was limited due to the uncomfortable experience and the high cost. Alternatively, many tumor markers have been developed, such as fecal occult blood (FOB) test, serum levels of carcinoembryonic antigen (CEA), and carbohydrate antigen (CA-199). Unfortunately, those markers in CRC diagnosis were circumscribed due to the insufficient sensitivity and organic specificity [4]. For clinical management, tumor, node, and metastasis (TNM) stage system is a gold standard that provides useful information for the choices of clinical treatments and predicts the patient’s prognosis in CRC. However, the current system has a drawback that has not able to predict the response and outcome individually, particular for stage II and III CRC patients [1]. Hence, any informative biomarker that could help the early diagnosis or guide the therapeutic choice would be very helpful for an appropriate therapeutic plan.
Cancer was described as a wound that refuses to heal [5], and today, many cancers including CRC have been tightly correlated with local or systemic inflammatory responses [6–8]. Among the various indices developed for the determination of systemic inflammation, the neutrophil to lymphocyte ratio (NLR) and the platelet to lymphocyte ratio (PLR) get increased attention [9, 10]. In CRC, as well as other cancers, an increase in the pretreatment NLR and/or PLR has been linked to poorer disease progression and/or survival [11–16] or response to treatment [17, 18]. Those results highlighted the critical roles of neutrophil- and platelet-dependent inflammatory response in cancer biology and the usefulness of both indices to the current clinical management of CRC patients. However, the precise contribution of both inflammatory reactions to the development of CRC and the regulating mechanism are poorly understood.
Given the importance of chronic inflammatory reactions in tumor development and therapy [6], particularly, the involvement of inflammatory reactions in the early steps of colorectal cancer [19], we hypothesized that the systemic inflammatory reactions in CRC might exhibit unique behaviors related to the tumor stage development, which could be reflected by the levels of NLR and PLR. For this purpose, the current study was designed to analyze the relationships between preoperative levels of NLR and PLR and tumor TNM stages in a group of CRC patients.
Methods
Patients and controls
We reviewed altogether the records of 336 patients at the Fujian Provincial Cancer Hospital during the period from January 2012 to May 2014 after the study protocol was approved by the institutional ethics committee. Patients were admitted to the hospital for curative resection of primary colorectal adenocarcinomas; no patients received any cancer-specific pretreatment. Primary diagnosis included 160 individuals with colon cancer and 176 individuals with rectal cancer. Patients who had evidence of infection, hematological diseases, renal dysfunction, and hyperpyrexia were excluded from the study. The median age for the study cohort was 59 years (range from 20 to 91 years.). The male to female ratio was 1.58:1. As a control group, we reviewed the records of 336 age- and gender-matched healthy individuals who performed their annual health check at the hospital.
Data collection
For each patient, we recorded the preoperative circulating blood counts (CBC), preoperative CEA levels, and the postoperative pathologic TNM stages (according to the 7th edition of UICC/AJCC TNM Classification System for Colorectal Cancer). Data of CBC and CEA levels were also collected from healthy controls.
NLR and PLR calculation
For the calculation of the NLR and PLR, we used the CBC counts obtained on the day of admission to our hospital. NLR and PLR ratios were calculated by dividing the total number of neutrophils or platelet counts per microliter whole blood by the absolute number of lymphocytes per microliter whole blood.
Statistical analysis
Data were expressed at either median and interquartile range (IQR) or mean and 95 % confidence interval (CI), as appropriated. Statistical analyses were carried out by the GraphPad Prism 5 and SPSS version 17 softwares. Differences of NLR, PLR, and CEA between patients and healthy subjects were evaluated by t test for variables with normal distribution or by Mann–Whitney U test for abnormally distributed variables. Values of the area under curve (AUC) obtained from receiver-operating characteristic curve (ROC) analysis were used to compare the predictive efficacy of NLR, PLR, and CEA. The association of NLR, PLR, and CEA with TNM stages was evaluated by Kruskal–Wallis test followed by a post-hoc test and a multivariate regression model. A two-tailed P value of <0.05 was considered statistically significant.
Results
Patient characteristics
Detailed demographic information of patients is shown in Table 1. Evaluation of TNM stages revealed the following distribution: 12.8 % (43 patients) of stage I, 32.7 % (110 patients) of stage II, 44.4 % (149 patients) of stage III, and 10.1 % (34 patients) of stage IV. Classification according to the T, N, and M stage revealed that 67.2 % of patients had deep tumor infiltration (T stage = 4), and 53.6 % had lymph node invasion (N stage >0), while 10.1 % of the included patients had distant metastasis (M stage = 1).
Comparison of NLR, PLR, and CEA in CRC patients and healthy controls
As shown in Table 1, CRC patients had higher CEA levels, absolute white blood cell (WBC), and neutrophil counts, higher platelet counts but lower absolute lymphocyte and red blood cell (RBC) counts compared to that of controls. Changes in the distribution of the WBC subsets were reflected in higher median values of NLR and PLR in the patient group. In CRC patients, median NLR was 2.0 (1.5 to 2.7) compared to 1.5 (1.2 to 1.9) in healthy controls. Similarly, PLR was higher in patients with a median of 130 (99 to 170) compared to 106 (85 to 124) in healthy controls (Fig. 1).
ROC analysis indicated that there are no differences between AUC values for NLR (0.71), PLR (0.70), and CEA (0.71), suggesting that all three markers had the comparable predictive powers for the presence of CRC in the general patient group.
Association of laboratory data with TNM stages in CRC patients
The associations between laboratory parameters with TNM stage were shown in Table 2. Kruskal–Wallis test indicated that there were significant interactions between tumor stages (I to IV) with NLR (P = 0.01), PLR (P = 0.0008), and CEA (P = 0.0001), with the lowest values in stage I. Post-hoc test indicated a different pattern of changes for three markers as compared to stage I, in that PLR showed a sharp increase in stage II followed by nearly constant levels till stage IV, while a significant increase of NLR was observed in stage IV. For CEA, an increasing trend following the tumor stages was observed with a significantly detectable higher level since stage III. There was no detectable interaction between the tumor stages and the blood counts, although a trend of elevation was observed for the neutrophil count (P = 0.17) and platelet count (P = 0.06).
In comparison with the control group, the earliest elevations in stage I were only detected at the levels of NLR and neutrophil count (both P = 0.0018) while PLR and platelet count were significantly raised since stage II (all P < 0.0001). The first detectable elevation of CEA was also found since stage II (P < 0.0001). There was no significant difference between stage II and stage III for all three markers.
Evaluation of the early diagnosis efficacy for NLR, PLR, and CEA
Levels of NLR, PLR, and CEA are all higher in the subgroup of early tumor stage (I/II) as compared to controls. Moreover, the increases in neutrophil and platelet count and a decrease in lymphocyte count were also detected (P < 0.0001). ROC analysis revealed a higher AUC value for NLR and PLR at 0.71 compared to CEA at 0.62, in differentiating early-stage (I and II) CRC patients from healthy controls.
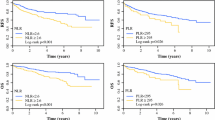
Association of NLR and PLR with independent T, N, and M stages in CRC patients
To focus our interest on the relationship between NLR and PLR with tumor stages, we further analyzed the correlation of both markers with independent T, N, and M stages. Levels of NLR and PLR, classified separately by T, N, and M stages, are shown in Fig. 2. Kruskal–Wallis analysis revealed that PLR (P = 0.0003), but not NLR (P = 0.09), showed a stage-dependent increase following the development of T stages. Neither NLR (P = 0.33) nor PLR (P = 0.63) showed any significant association with the development of N stages. In M stage comparison, only NLR showed significant higher levels in M1 subgroup (P = 0.022) as compared to M0 subgroup.
Categorized comparison of NLR and PLR by T, N, and M stages in CRC patients (data were expressed by mean and 95 % CI). a The increase of PLR was associated with T stage development (P = 0.0003), with a significant difference between T4 subgroup and T1/T2 subgroup (P < 0.001). PLR showed no difference among N stages and between M stages. b No significant association of NLR with T stages or N stages was detected. NLR was higher in M1 compared to M0 stages (P = 0.022)
Using the multivariate regression analysis model, the PLR was identified as an independent factor associated with T stage development (P < 0.0001).
Validation test of PLR role in association with T stage development
Validation of the relationship between PLR and T stages was further performed in a subgroup of 153 patients with TNM stage I and II, whose pathologic classifications only differ in T stages. As shown in Fig. 3, there is a significant interaction between PLR and T stages, with the median levels of PLR from T1 to T4 at 112, 109, 126, and 146, respectively, while no significant interaction for NLR was detected.
NLR and PLR levels in patients with the exclusive difference of T stages. a A significant correlation between the levels of PLR and T stages was detected (P = 0.001). The post-hoc test reveals a significant higher level of PLR in T4 subgroup as compared to T2 subgroup (P < 0.01). b There is no significant correlation between the levels of NLR and T stages
Discussion
CRC is a type of cancer which is tightly correlated with chronic inflammation, particularly in colitis-associated cancer [20]. Previous studies have paid much attention exploring the usefulness of inflammation indices, including NLR and PLR, in CRC patient’s prognosis or treatment response. In the present study, we retrospectively analyzed NLR and PLR in a cohort of CRC patients, with a particular interest on the relationships between both parameters and the tumor TNM stages. We observed that the levels of both markers were significantly higher in CRC patients than in healthy controls. The increase in NLR and PLR was all correlated with the development of TNM stages. More importantly, we found that NLR showed a two-phase elevation separately by stage I and stage IV while PLR was significantly elevated from stage II with no further changes in the later stages and was an independent predictor for T stage development. Those results implicated that both neutrophil- and platelet-dependent inflammation responses were actively engaged in the different stages of cancer progression.
The observed higher levels of NLR and PLR in the CRC patient group are consistent with the recent publication by Kilincalp et al. [21]. The increased levels of both markers would reflect the active interaction of host immune system with tumor burden in vivo. In addition to the conclusion drawn from the Kilincalp’s study that NLR and PLR exhibited a potential value for the diagnosis of CRC by analyzing the data from healthy and whole CRC cohort, the present study puts a little bit forward, evaluating the tumor stage-dependent changes of both markers. We found that both NLR and PLR were elevated in the early tumor stage, highlighting the value of both markers in the early detection of CRC. Compared with well-known tumor marker CEA, both markers showed a better predictive power for the detection of early stage (I/II) CRC.
Of note, both NLR and PLR showed an early response in the process of tumor progression, which supports the novel hypothesis that the inflammatory reactions play an important role in the early steps of colorectal cancer development [19]. It has been known that neutrophil and platelet are actively engaged in the process of tumor progression and metastasis [19, 20, 22]. Increased NLR and PLR were reflected by a synchronous elevation of neutrophil and platelet count and a relative decrease in lymphocyte count, suggesting the heightened neutrophil- and platelet-dependent inflammatory reactions and a decreased lymphocyte-mediated antitumor immune response. With respect to our observation on the different response phases of NLR and PLR in the early stage of CRC, it might reflect that the consequence of inflammation cascade involved in the cancer development. As immune cells, the neutrophils were rapidly activated and migrated to the inflamed site upon encountering inflammatory signals. The persistent stimulus on neutrophils due to chronic inflammation could result in an aggravating oxidative stress leading to epithelium damage and promutagenic DNA lesions [19]. Once tumor establishes from the above processes, the tumor could secrete bio-substances (e.g., interleukin-6 and tissue factor) that further promoted platelet production and activated platelets in circulation [23–25]. In turn, with this alteration, the activated platelet favors tumor growth by releasing the granule components such as vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), and transforming growth factor β (TGF-β) [22]. Besides both markers showed a different change in the early stage of CRC, both markers have the similarity that did not show significant changes in the level between stage II and III. The underlying mechanism is currently unclear. However, NLR, but not PLR, showed a second-phase increase in stage IV, implicating the important role of neutrophil-dependent inflammatory response in the development of CRC metastasis. Our observation is in line with the view that myeloid cells facilitate the later stages of tumor development by producing the inflammatory microenvironment that is required for EMT, intravasation, and metastasis [6]. In the very latest publication by Nature, a critical role of neutrophil-mediated immune response in spontaneous breast cancer metastasis was identified in mouse models [26]. The difference in tumor stage responses between both indices should reflect the different pathophysiologic roles of neutrophils and platelets in cancer development. Such notion might be explainable for a previous report that NLR was a better prognostic and predictive factor in patients with metastatic colorectal cancer, as compared to PLR [27].
Also to the findings mentioned above, the present study indicated that PLR is an independent predictive factor for the extent of tumor invasion (T stage) in CRC. The basis of these observations would relate to the unique role of the platelet in the loop of platelet-cancer interaction by releasing platelet granule contents that favor to cancer growth [22]. Activated platelets in the tumor environment of ovarian cancer cells have been found to increase tumor cell invasion in a dose-dependent fashion [28]. In a recent study, a mechanism of platelet-stimulated colon cancer invasion has been proposed. The platelet-derived thrombospondin 1 and clusterin were found to upregulate the gene expression of MMP-9 via a P38MAPK pathway, with the subsequent cell invasion-promoting effects [29].
Our study provided the first insight into the correlations of the changes of preoperative NLR and PLR levels with CRC tumor stages. The clinical importance of our study would be (1) to better understand the roles of both neutrophil- and platelet-dependent inflammatory response in different tumor stages (This advantage might be helpful for the therapeutic plan either in the selection of drugs or monitoring the treatment response. For instance, PLR was significantly elevated in stage II CRC patients. Thus, the use of drugs against platelet-derived factors might be a choice of therapy in those patients. Furthermore, monitoring PLR level in stage II and III CRC patients might help to clarify the patients who might or might not benefit from a class of drugs of antiplatelet-derived factors.); (2) to help explain some cancer behaviors; and (3) to provide potential early detection markers for CRC and a potential marker for T stage evaluation. The latter would be a valuable aid for preoperative evaluation in rectal cancer since exact local T staging at the time of diagnosis is essential and is the basis for the requirement of neoadjuvant treatment.
The present study had the limitation that it was a retrospective, single-center study with a limited number of patients, particularly, only a few stage I and stage IV patients were included. This drawback might lead to an underestimation of the statistical power. Therefore, larger prospective studies will need to be performed to confirm these preliminary results.
In summary, our study demonstrated that the levels of preoperative NLR and PLR are independently correlated with the tumor TNM stages in CRC patients, suggesting the important roles of neutrophils and platelets in bridging the cancer–host interaction during the different steps of cancer development. Both of them have shown the potential values as the markers either in the early diagnosis or tumor T stage evaluation in CRC patients. The utility of them in individual therapy would be an interesting topic in the future study.
References
Brenner H, Kloor M, Pox CP. Colorectal cancer. Lancet. 2014;383:1490–502.
Dai Z, Zheng RS, Zou XN, Zhang SW, Zeng HM, Li N, et al. Analysis and prediction of colorectal cancer incidence trend in China. Zhonghua Yu Fang Yi Xue Za Zhi. 2012;46:598–603.
Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220–41.
Swiderska M, Choromańska B, Dąbrowska E, Konarzewska-Duchnowska E, Choromańska K, Szczurko G, et al. The diagnostics of colorectal cancer. Contemp Oncol (Pozn). 2014;18:1–6.
Dvorak HF. Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med. 1986;315:1650–9.
Elinav E, Nowarski R, Thaiss CA, Hu B, Jin C, Flavell RA. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nat Rev Cancer. 2013;13:759–71.
Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009;30:1073–81.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646–74.
Templeton AJ, McNamara MG, Šeruga B, Vera-Badillo FE, Aneja P, Ocaña A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106:dju124.
Templeton AJ, Ace O, McNamara MG, Al-Mubarak M, Vera-Badillo FE, Hermanns T, et al. Prognostic role of platelet to lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2014;23:1204–12.
Li MX, Liu XM, Zhang XF, Zhang JF, Wang WL, Zhu Y, et al. Prognostic role of neutrophil-to-lymphocyte ratio in colorectal cancer: a systematic review and meta-analysis. Int J Cancer. 2014;134:2403–13.
Malietzis G, Giacometti M, Askari A, Nachiappan S, Kennedy RH, Faiz OD, et al. A preoperative neutrophil to lymphocyte ratio of 3 predicts disease-free survival after curative elective colorectal cancer surgery. Ann Surg. 2014;260:287–92.
Liu H, Du X, Sun P, Xiao C, Xu Y, Li R. Preoperative platelet-lymphocyte ratio is an independent prognostic factor for resectable colorectal cancer. Nan Fang Yi Ke Da Xue Xue Bao. 2013;33:70–3.
Lee S, Oh SY, Kim SH, Lee JH, Kim MC, Kim KH, et al. Prognostic significance of neutrophil lymphocyte ratio and platelet lymphocyte ratio in advanced gastric cancer patients treated with FOLFOX chemotherapy. BMC Cancer. 2013;13:350.
Smith RA, Bosonnet L, Raraty M, Sutton R, Neoptolemos JP, Campbell F, et al. Preoperative platelet-lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg. 2009;197:466–72.
Zhou X, Du Y, Huang Z, Xu J, Qiu T, Wang J, et al. Prognostic value of PLR in various cancers: a meta-analysis. PLoS One. 2014;9, e101119.
Chua W, Charles KA, Baracos VE, Clarke SJ. Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in patients with advanced colorectal cancer. Br J Cancer. 2011;104:1288–95.
Cannon NA, Meyer J, Iyengar P, Ahn C, Westover KD, Choy H, et al. Neutrophil-lymphocyte and platelet-lymphocyte ratios as prognostic factors following stereotactic radiation therapy for early-stage non-small cell lung cancer. J Thorac Oncol. 2015;10:280–5.
Mariani F, Sena P, Roncucci L. Inflammatory pathways in the early steps of colorectal cancer development. World J Gastroenterol. 2014;20:9716–31.
Grivennikov SI. Inflammation and colorectal cancer: colitis-associated neoplasia. Semin Immunopathol. 2013;35:229–44.
Kilincalp S, Coban S, Akinci H, Hamamc M, Karaahmet F, Coşkun Y, et al. Neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, and mean platelet volume as potential biomarkers for early detection and monitoring of colorectal adenocarcinoma. Eur J Cancer Prev. 2014.
Goubran HA, Burnouf T, Radosevic M, El-Ekiaby M. The platelet-cancer loop. Eur J Intern Med. 2013;24:393–400.
Kaser A, Brandacher G, Steurer W, Kaser S, Offner FA, Zoller H, et al. Interleukin-6 stimulates thrombopoiesis through thrombopoietin: role in inflammatory thrombocytosis. Blood. 2001;98:2720–5.
van Rossum AP, Vlasveld LT, Vlasveld IN, Jansen PM, Dik WA, Hooijkaas H, et al. Granulocytosis and thrombocytosis in renal cell carcinoma: a pro-inflammatory cytokine response originating in the tumour. Neth J Med. 2009;67:191–4.
Goubran HA, Stakiw J, Radosevic M, Burnouf T. Platelet-cancer interactions. Semin Thromb Hemost. 2014;40:296–305.
Coffelt SB, Kersten K, Doornebal CW, Weiden J, Vrijland K, Hau CS, et al. IL-17-producing γδ T cells and neutrophils conspire to promote breast cancer metastasis. Nature. 2015.
He W, Yin C, Guo G, Jiang C, Wang F, Qiu H, et al. Initial neutrophil lymphocyte ratio is superior to platelet lymphocyte ratio as an adverse prognostic and predictive factor in metastatic colorectal cancer. Med Oncol. 2013;30:439.
Holmes CE, Levis JE, Ornstein DL. Activated platelets enhance ovarian cancer cell invasion in a cellular model of metastasis. Clin Exp Metastasis. 2009;26:653–61.
Radziwon-Balicka A, Santos-Martinez MJ, Corbalan JJ, O'Sullivan S, Treumann A, Gilmer JF, et al. Mechanisms of platelet-stimulated colon cancer invasion: role of clusterin and thrombospondin 1 in regulation of the P38MAPK-MMP-9 pathway. Carcinogenesis. 2014;35:324–32.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jia, J., Zheng, X., Chen, Y. et al. Stage-dependent changes of preoperative neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in colorectal cancer. Tumor Biol. 36, 9319–9325 (2015). https://doi.org/10.1007/s13277-015-3667-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3667-9