Abstract
Axillary lymph nodes status is the most important prognosis factor in early breast cancer. This status is known by a selective sentinel lymph node biopsy (SLNB) and/or lymphadenectomy. Immunohistochemical studies of breast cancer tumour tissue have reported a relation between the increased expression of vascular endothelial growth factor-C (VEGF-C) and the risk of lymph node metastasis. We researched whether serum levels of VEGF-C could be a predictor factor of sentinel lymph node status in these patients. A prospective analysis was performed on serum from 174 patients with early breast cancer who underwent SLNB. The level of VEGF-C was determined by enzyme-linked immunosorbent assay. Clinical-pathologic variables were collected. Univariate analysis and multivariate logistic regression were conducted, taking SLNB positivity as the segmentation variable. The predictive value of VEGF-C was assessed using ROC curves. Of the sample group of 167 patients, 64 (38.3 %) had affected lymph node. Eighteen patients (28.1 %) presented micrometastasis; there were isolated tumour cells in 11 cases (17.2 %) and macrometastasis in 35 (54.6 %). The median value of VEGF-C was 6561.5 pg/ml. These values did not correlate with any clinical variables, and there was no association between the level of VEGF-C and SLNB status (p = 0.626). In the multivariate analysis, tumour size (p = 0.009) and the presence of vascular invasion (p < 0.001) were independently associated with sentinel lymph node affected. Serum levels of VEGF-C do not appear to predict sentinel lymph node status in patients with early breast cancer who undergo SLNB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Axillary lymph node status in patients with early breast cancer is the main prognostic factor in this group of patients [1]. To determine this status, a histological analysis of the lymph nodes must be performed, by selective sentinel lymph node biopsy (SLNB) and/or axillary lymphadenectomy (LA). Traditionally, the latter approach has been taken, but with de idea to reduce the morbidity related, it is increasingly being replaced by SLNB [2]. However, this technique is not devoid of morbidity either (due to the radiation received, allergic reactions to the test, etc.) and it is subject to a false negative rate of 8 % [3].
Furthermore, less than a third of patients with T1-2 tumours, no palpable lymph nodes, and fewer than three sentinel lymph nodes positive are found to have additional non-sentinel nodes compromised when LA is practiced [4, 5]. This additional procedure to SLNB does not seem to influence patients’ survival but does significantly increase the likelihood of complications [6, 7]. Even outside this subgroup, among a large proportion of patients (52 %), LA subsequent to a positive SLNB does not reveal any alteration in the remaining lymph nodes, and so these patients will have been subjected to an unnecessary procedure [8].
In view of these data, studies have been undertaken to identify predictors of axillary status. To date, the factors most generally accepted in this respect are tumour size, lymphovascular invasion, histological grade and the patient’s age. However, no combination of these factors or any diagnostic imaging technique has yet replaced surgical resection and subsequent anatomic-pathological examination of the lymph nodes [9].
The invasion of the lymph vessels and the consequent generation of metastases in the lymph nodes by solid tumours require the growth of new lymphatic vessels (lymphangiogenesis). The mechanisms by which tumours promote lymphangiogenesis remain unclear, but in recent years, the development of molecular biology has led to an important finding, namely the discovery of growth factors that promote lymphangiogenesis and the dissemination of solid tumours by lymphatic pathways. Specifically, vascular endothelial growth factors C and D (VEGF-C and VEGF-D) and the membrane receptor VEGFR-3 are strongly associated with the above phenomena and have been studied extensively [10]. Thus, the expression of VEGF-C (and to a lesser extent that of VEGF-D) has been shown to be strongly correlated with the risk of lymph node metastases, in over 30 studies of different malignancies, including cancers of the lung, breast or colon [11–13].
In breast cancer, the increased expression of VEGF-C (measured by immunohistochemistry in tumour biopsies) is related to the density of peritumoural lymph capillaries and the risk of metastasis in the lymph nodes. These data suggest that an analysis of VEGF-C may help in assessing the risk of axillary nodal spread in early breast cancer [14, 15].
If serum levels of VEGF-C were correlated with the risk of axillary nodal spread, this would offer a simple, risk-free mean of predicted lymph node status, enabling to optimise the resource use, including operating theatres time, and reduce the delay between the histological diagnosis and the first surgical treatment for breast cancer.
However, to date, no study of breast cancer has related serum VEGF-C with the probability and amount of axillary lymph node spreads. It has not been done any research to assess the possible predictive power of this association and the ability to use it as an indicator before performing invasive strategies such as SLNB or LA.
Study goals
The main goal of this study is to determine whether there is a correlation between serum levels of VEGF-C and status of axillary lymph nodes determined by SLNB in patients with early breast cancer. We also examine whether there is any relationship between VEGF-C levels and lymph node alteration after SLNB and its relationship with various prognostic variables, in order to define a multifactorial score with which to predict axillary status in women with early breast cancer.
Material and methods
Study design and sample
Prospective cohort study included 174 patients with early breast carcinoma diagnosed between September 2009 and November 2012. All patients were evaluated by a multidisciplinary committee and treated at the Hospital Costa del Sol (Marbella, Spain).
Eligible patients were women aged over 18 years, diagnosed with invasive breast carcinoma, early stage according to the 7th edition of the AJCC Cancer Staging Manual [16]. Tumour size was assessed by ultrasound and mammography and had to be less than 3 cm for the patient to be included in the study. If ultrasound examination produced conflicting results, the larger diameter was taken. No multicentre tumours were included. A further condition for inclusion was a negative clinical and ultrasound axillary assessment. If there were doubts about axillary status, cytology fine needle aspiration under radiologic guidance was conducted. The study with chest radiography and blood test was negative in every case.
Exclusion criteria included previous contralateral or metachronous breast cancer, the presence of any allergy contraindicative to selective SLNB and a history of any prior neoplasia other than non-melanoma skin cancer.
Sample collection and surgical procedure
Before surgical treatment, we obtained the informed consent of all patients who agreed to participate in the study. After this, we take two samples from each patient containing 10 ml each of peripheral blood, which was processed within 2 hours of the sample. From each sample, we obtained serum and plasma. All included patients underwent surgery of the primary tumour together with SLNB and/or LA (see Fig. 1).
In all cases, we used isotope tracing to locate the sentinel node. When the technique was not effective, lymph node status was assessed after axillary lymphadenectomy, and these patients were retained in the study. Until September 2011, all patients who presented alteration in any sentinel lymph node underwent a standard LA. However, after the publication of the Z0011 study results [8], patients with only microscopic SLNB alterations were not subjected to LA; this was the case of 15 patients with micrometastases in the SLNB. As the main goal of the present study is to determine whether there is a correlation between serum VEGF-C and the axillary lymph nodes status obtained by SLNB, this change did not provide any reason to interrupt the recruitment of patients.
The remaining clinical-pathological variables required were obtained after the histological study of the surgical specimens (radiological and histological tumour size, histological type, histological grade, vascular and lymphatic invasion, hormone receptor status, amplification of HER2 expression, Ki67, SLNB status, number and type of lymph node status: isolated cells, microscopic or macroscopic lymph node metastasis, alteration to periganglionar fat and alteration to the remaining lymph nodes, in the case of LA).
Histologic SLNB studies
The SLNB were identified by injection of a radioactive (99Tc-labelled) tracer the day of surgery and were removed surgically with the aid of a hand-held gamma-ray detecting probe (Ethicon Endo-Surgery, Cincinnati, OH), as previously reported [17]. The majority of patients received SLNB during conservative or radical breast surgery. The sentinel lymph node study was performed intraoperatively according to the previously described procedure [2]. Briefly, the SLNB sections were bisected along the major axis, and both moieties were embedded in paraffin for later histological analysis. Lymph nodes of 5 mm were embedded and uncut. Thirty pairs of adjacent sections, 4 μm thick, were cut at 50-μm intervals. If residual tissue sections remained, additional pairs of sections were cut at 100-μm intervals until the lymph node was entirely sectioned. One section of each pair was stained with haematoxylin and eosin (H&E). The lymph node was then homogenised for the study using a molecular technique. The study was conducted by a molecular analysis involving the one-step nucleic acid amplification of cytokeratin-19 mRNA (Sysmex®). Pairs of paraffin-embedded sections were cut at 50 and 100-μm intervals and stained as above. Metastatic deposits were measured according to the three axes, and the largest size was recorded [18]. The size of the metastatic nests in the plane of the tissue sections was measured histologically with an ocular micrometer, and the thickness was calculated according to the number of involved contiguous sections and to the sectioning interval between them. To avoid underestimation of the thickness of the metastases, the cutting intervals immediately preceding the first and following the last involved sections also were included. The recorded largest size corresponded to the maximum diameter in the plane of the section or to the thickness of the metastatic foci, whichever was larger. If multiple but distinct (i.e. separated by uninvolved tissue sections) metastases were identified in the same SLN, the size of the largest was recorded.
Measuring serum VEGF-C
Serum VEGF-C levels were measured using serum obtained by centrifugation of the two peripheral blood samples for 15 min at 1000 g. The serum was then separated into several aliquots and frozen to −80 °C.
The Quantikine (R&D) VEGF-C assay is a sandwich-type immunoassay that uses a monoclonal antibody specific for VEGF-C, coated on the surface of a microplate so that the VEGF-C molecules in the serum bind to the immobilised antibody. After repeated washing to remove unbound substances, an enzyme-labelled polyclonal antibody specific for VEGF-C is added to the wells. After another washing, the concentration of VEGF-C is determined by incubation with the substrate. Finally, the stop solution is added, ending the reaction and producing a coloured end product. The amount of bound conjugate is measured in units of absorbance at 540 or 570 nm (Zenit SP+ Menarini). The concentration of VEGF-C can be calculated by interpolation from the calibration curve of the standards. Absorbance is measured using a ZENIT SP+ analyser (Menarini), which is an open system for processing immunoenzymatic tests using the ELISA 8 × 12 microplate system. This procedure meets the requirements of Medical Device Directive 98/79/EC for in vitro diagnostics. The results are calculated as the average of the duplicate readings for each standard, control and sample and then subtracting the average zero standard optical density. The optical density is mapped against the concentration of the standards and the best curve drawn. To determine the concentration of VEGF-C in each sample, the optical density data are interpolated in the standard curve. If the samples have been diluted, the concentration read from the standard curve must be multiplied by the dilution factor. Some studies have related serum levels of VEGF and the platelet count, as the platelets appear to store and release these factors into the bloodstream [19]. Therefore, we took into account the platelet count obtained in the plasma sample.
We used a control group of healthy women. Dr. Rueda did a study in lymphoma patients [20] where 22 serums of healthy women were used. Here, the median age of this group was similar to our work and the results of VEGF-C were similar to our study.
Measuring other variables
Ki67
-
Immunohistochemical staining is conducted, and the proportion of the malignant cells staining positive for the nuclear antigen Ki-67 is evaluated in a quantitative and visual way using light microscopes.
-
Ki-67 values are acquired as the percentage of positively marking malignant cells using the antihuman Ki-67 monoclonal antibody MIB1 which is one of the most commonly used antibodies and considered as the ‘gold standard’.
-
The Ki-67 percentage score is defined as the percentage of positively stained tumour cells among the total number of malignant cells assessed. Withal, only the positivity is of interest independent of the intensity of coloration. To ensure quality assurance of the staining, positive control tissues are completed.
-
A Ki-67 cut-off point of 14 % was defined according to the experience of different pathologists as well as national and international recommendations at present.
-
The complete specimen is investigated and checked for immunostaining tumour cell nuclei. Scoring is conducted considering the whole tumour section and not only limiting to the hot spots of the carcinoma or to the most evident positive parts within the invasive segment or the front of necrosis. In summary, the Ki-67-labelling index is the percentage of cells with Ki-67-positive nuclear immunostaining.
Lymphovascular invasion
-
The distinction between lymph channels and blood vessels is unnecessary according to international guidelines [21]. Because the routine staining (haematoxylin-eosin) cannot distinguish between lymphatic and blood vessels, it is preferable to speak of lymphovascular invasion or vascular invasion. In the detection of lymphovascular invasion, the diagnostic criteria of Rosen are followed [22].
Statistical analysis
The sample size required for the diagnostic test (serum VEGF-C) was predetermined for an expected prevalence of axillary lymph nodes positive of 25 %, with an absolute accuracy of 3 %, a confidence level of 95 % and an expected specificity of 95 %. It was thus determined that a sample of 199 patients with operable breast cancer would be needed, and accordingly, a minimum sample size of 200 patients was assumed.
A descriptive analysis was carried out, with measures of central trend and dispersion for the quantitative variables and of frequency distribution for the qualitative ones. The Kolmogorov-Smirnov test was used to determine the normality of the sample for the quantitative variable VEGF-C. Univariate analyses were conducted, taking as outcome variables the value of serum VEGF-C and the presence of sentinel lymph node alteration. The relationship between two quantitative variables was assessed using Pearson’s correlation, and that between a quantitative and a qualitative variable using Student’s T test with a dichotomous qualitative variable, and one-factor ANOVA for qualitative variables with three or more categories. The association between qualitative variables was assessed by the chi-square test. Finally, taking as the outcome variable the presence of altered sentinel lymph nodes, multiple logistic regression was performed, including in the model the variables found to be significant in the bivariate analysis, together with the patient’s age and the VEGF-C results, using the stepwise forward method and ascertaining the odds ratio with the respective 95 % confidence interval. In all analyses, the significance level was set at p < 0.05.
Results
A total of 174 patients were finally included during the study period. Seven patients (4 %) did not undergo SLNB due to problems associated with the technique (non-migration of the tracer or failure to achieve intraoperative localization) and received LA concurrently with the primary surgery. The study patients had a median age of 56 (24–79 years). Over half were postmenopausal at diagnosis, and the most common histological type was ductal carcinoma. Most of the patients had tumours with a good prognosis: over half had tumours smaller than 2 cm and no vascular invasion, grade I-II and the presence of positive hormone receptors. Ki-67 exceeding 14 % was observed in 62.1 % of the participating patients (see Table 1).
Of those who underwent SLNB, 63 patients (38.4 %) presented an altered status in one or more of the lymph nodes removed (55 % macrometastasis, 28 % micrometastasis and 17 % isolated tumour cells). On median, two sentinel lymph nodes were removed (interquartile range = 1). Of the 46 patients who underwent LA, 39 had a SLNB positive. The median number of nodes removed during LA was 16.5 (interquartile range = 11) with a median of 3.39 lymph nodes affected. The LA was positive in 13 (34.2 %) of the patients who had a positive prior SLNB. 12.5 % of the patients had extracapsular lymph node damage.
The serum levels of VEGF-C fitted a normal distribution, with a median value of 6561.5 pg/ml (interquartile range = 2121.3 pg/ml). There was no significant difference between the serum levels of VEGF-C of healthy women and women with breast cancer (median = 6125; RI = 1907; p = 0.288).
In the univariate analysis, SLNB status was significantly associated with tumour size determined by ultrasound (p = 0.017), with final size after pathological study (p = 0.001), histological grade (p = 0.04), vascular invasion (p < 0.001) and Ki-67 (p < 0.01). No relationship was observed with the other variables: age, menstrual status, hormone receptor status, HER2 overexpression or histologic subtype. However, there was a relationship between sentinel lymph node positive and the total number of platelets (p = 0.025); the SLNB patients presented a higher number of platelets.
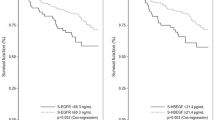
There was no found to be a significant correlation between the serum level of VEGF-C and SLNB compromised (p = 0.626). Furthermore, the median level in the patients with sentinel lymph node positive was slightly lower (Fig. 2). There was no association between the serum level of VEGF-C and the total number of lymph nodes affected (p = 0.146) or between VEGF-C and axillary lymph node compromised in the LA after a positive SLNB (p = 0.95).
VEGF-C levels were not correlated with any of the remaining clinical or pathological variables analysed. However, there was a correlation between the value of VEGF-C and the total number of platelets (r = 0.158) (p = 0.037) (see Table 2).
In the multivariate analysis, only tumour size (p = 0.009) and vascular invasion (p < 0.001) remained statistically significant regarding lymph node status in the SLNB.
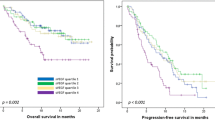
In a final analysis during follow-up, there were nine relapses. There was no relationship between level of VEGF-C and type of relapse, disease-free interval or overall survival.
Discussion
To the best of our knowledge, this study is the first to examine whether serum levels of lymphangiogenesis factor VEGF-C are predictors of the axillary lymph node status revealed by SLNB in women with early breast cancer.
Knowledge of axillary status in early breast cancer has high prognostic value and influences the adjunctive treatment administered to these patients [23], although only a third of those who undergo SLNB have axillary nodes compromised. In the remaining two thirds, the decision to administer adjuvant treatment is based on other known prognostic factors (age, histologic grade, hormone receptors, overexpression of the HER-2/neu gene). Due to the cost, comorbidity and surgical time and complexity associated with the SLNB technique, studies have been undertaken to identify a predictor factor of lymph node damage [1].
A total of 174 patients were included in this study that were homogeneously treated by the same surgical and medical team. The characteristics of this cohort and the results obtained are similar to those reported elsewhere: 32 % of the patients had sentinel lymph node alteration and of those subjected to LA; 58 % had no metastases to any of the lymph nodes removed in this procedure [24].
In recent years, nomograms have been developed with the aim of predicting axillary status, taking into account various clinical and anatomo-pathological variables. However, the results of these initiatives have been disappointed. In our study, a sub-analysis of the first 174 patients was performed. Given the results presented above, we decided not to continue the recruitment because an increasing sample would not change the results. Among the variables analysed, tumour size and lymphovascular invasion were found to be independent predictors of axillary alteration after SLNB. These data are consistent with those previously reported in the literature [9, 25]. As a previously unreported finding, an association was found between the number of platelets and altered sentinel lymph node status [18]. However, the joint consideration of the platelets and the other factors was not sufficient to enable us to create a score that could be used before breast cancer surgery to predict axillary status after SLNB.
Previous studies have shown the importance of VEGF-C and VEGF-D and of the receptor VEGFR3 in lymphangiogenesis. The role of VEGF-C in the lymphatic spread of breast cancer has been established in experiments with mouse models in which the administration of RNAi anti-VEGF-C significantly decreased the risk of lymph node metastases [26]. This suppression of lymphatic spread, following the administration of RNAi anti-VEGF-C, has also been observed in mouse models of colon cancer [27].
In view of these findings and the absence of any prior study evaluating serum levels of VEGF-C as predictors of axillary status in breast cancer, we examined this factor using the ELISA technique. After quantification of the samples, the analysis revealed no significant relationship between the level of this protein and altered axillary status after SLNB or LA. Neither there was any relation when the platelet count was taken into consideration, as a possible distorting factor of serum levels of VEGF-C (data not shown).
The expression of VEGF-C into serum in breast cancer patients was first described in a study of cases and controls by Al-Mowallad et al. [28]. In this study, the serum levels of the protein were analysed by ELISA in 122 patients with cancer and 64 controls. No significant differences were found in serum levels of VEGF-C between patients and healthy controls; VEGF-C levels were higher in inflammatory breast tumours, but not significantly so. Subsequently, Gisterek et al. [19] analysed the serum of 377 patients with breast cancer and healthy controls to determine the levels of VEGF-A, VEGF-D and VEGF-C. In this study, no differences were found between patients and healthy controls in the levels of these three factors.
In contrast, two studies of breast cancer have attempted to demonstrate a relationship between the expression of the factors involved in lymphangiogenesis and the risk of lymph node metastasis [14, 15]. By immunohistochemical analysis of surgical specimens of the primary tumour, these studies found that the increased expression of VEGF-C is related to the density of peritumoural lymphatic capillaries and to the risk of metastasis in the lymph nodes. Studies of other solid tumours have demonstrated a statistically significant relationship between the risk of lymph node spread and the presence of high levels of serum VEGF-C in patients with tumours such as non-small cell lung cancer, colon cancer, gastric cancer and oesophageal cancer [29–31]. In a study conducted in 116 patients diagnosed with operable non-small cell lung cancer, serum levels of VEGF-C below 1850 pg/ml predicted the negativity of the mediastinal lymph nodes in the histological study of hilar-mediastinal lymphadenectomy, with a specificity of 77 %. This specificity increased to 80 % when the level of VEGF-C was combined with the results of axial computerised tomography [32].
Recently, other works have determined serum VEGF-C and they have seen that there was a relationship between the levels of VEGF-C and lymph node involvement. The study of Morgillo F et al. [33] states that the serum levels of VEGF-C are higher among patients with breast cancer and nodal involvement than patients without lymph node involvement in a group of patient with breast cancer and hormone receptor positive. This study used ELISA technique, but the kit and the level of VEGF-C were different from our study. In addition, our objective was to determine whether the levels of VEGF-C were able to be a predictor factor of sentinel lymph node status.
Analysis of the remaining variables showed that none of the prognostic variables considered was significantly related to the serum level of VEGF-C. However, there was found to be an association between axillary alteration and the number of platelets and a significant relationship between the level of VEGF-C and the number of platelets. Such a relationship has also been described in other studies with respect to the expression of VEGF-A and D, since the platelets appear to be responsible for storing these factors and subsequently releasing them into the bloodstream [19, 34].
The present study examines a cohort of patients with early breast cancer, who received very similar treatment and were prospectively assessed and included for analysis. These characteristics enabled us to obtain good quality in the collection and storage of samples for the determination of VEGF-C, in performing selective sentinel lymph node biopsy and in obtaining a homogeneous evaluation of the surgical specimens.
We conclude that, in view of the results obtained, the serum levels of VEGF-C cannot be considered a predictive biomarker of the axillary lymph node alteration after SLNB in patients with early breast cancer. Data interpretation and overall conclusions should take into account the complexity of the process, heterogeneity of breast cancer and significant limitations of correlative studies that typically performed with patient samples because of complex process of lymphangiogenesis.
References
Burstein HJ, Harris JR, Morrow M. Malignant tumors of the breast. In: De Vita VT, Lawrence TH, Rosenberg SA, editors. Cancer Principles & Practice of Oncology. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 1606–54.
Veronessi U, Paganelli G, Viale G, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Eng J Med. 2003;349:546–53.
Purushotham AD, Upponi S, et al. Morbidity after sentinel lymph node biopsy in primary breast cancer: results from a randomized controlled trial. J Clin Oncol. 2005;23:4312–21.
Fein DA, Fowble BL, Hanlon AL, et al. Identification of women with T1-T2 breast cancer at low risk of positive axillary nodes. J Surg Oncol. 1997;65:34–9.
Silverstein MJ, Skinner KA, Lomis TL. Predicting axillary nodal positivity in 2282 patients with breast carcinoma. World J Surg. 2001;25:767–72.
Montgomery LL, Thorne AC, et al. Isosulfan blue dye reactions during sentinel lymph node mapping for breast cancer. Anesth Analg. 2002;95:385–8.
Fisher B, Jeong JH, Anderson S, et al. Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med. 2002;347:567–75.
Giuliano A, Hunt K, Ballman K, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis. JAMA. 2011;305:569–75.
Dauphine CE, Haukoos JS, Vargas MP, Isaac NM, Khalkhali I, Vargas HI. Evaluation of three scoring systems predicting non sentinel node metastasis in breast cancer patients with a positive sentinel node biopsy. Ann Surg Oncol. 2007;14:1014–9.
Sunder SS, Ganesan TS. Role of lymphangiogenesis in cancer. J Clin Oncol. 2007;25:4298–307.
Pepper MS, Tille JC, Nisato R, et al. Lymphangiogenesis and tumor metastasis. Cell Tissue Res. 2003;314:167–77.
Krishnan J, Kirkin V, Steffen A, et al. Differential in vivo and in vitro expression of vascular endothelial growth factor (VEGF)-C and VEGF-D in tumors and its relationship to lymphatic metastasis in immunocompetent rats. Cancer Res. 2003;63:713–22.
Lin J, Lalani AS, Harding TC, et al. Inhibition of lymphogenous metastasis using adeno-associated virus-mediated gene transfer of a soluble VEGFR-3 decoy receptor. Cancer Sci. 2004;65:6901–9.
Mohammed RA, Green A, El-Shikh S, et al. Prognostic significance of vascular endothelial cell growth factors -A, -C and -D in breast cancer and their relationship with angio- and lymphangiogenesis. Br J Cancer. 2007;96:1092–100.
Zhang XH, Huang DP, Guo GL, et al. Coexpression of VEGF-C and COX-2 and its association with lymphangiogenesis in human breast cancer. BMC Cancer. 2008;8:4. doi:10.1186/1471-2407-8-4.
Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC Cancer Staging Manual. 7th ed. 2010.
Veronesi U, Paganelli G, Viale G, et al. Sentinel lymph node biopsy and axillary dissection in breast cancer: results in a large series. J Natl Cancer Inst. 1999;91:368–73.
Viale G, Bosari S, Mazzarol GM, et al. Intraoperative examination of axillary sentinel lymph nodes in breast carcinoma patients. Cancer. 1999;85:2433–8.
Gisterek I, Matkowski R, Lacko A, et al. Serum vascular endothelial growth factors a, C and d in human breast tumors. Pathol Oncol Res. 2010;16:337–44.
Rueda A, Rifa J, Quero C, et al. High serum levels of vascular endothelial growth factor C have a positive impact on outcome of patients with advanced diffuse large B cells lymphoma. Leuk Lymphoma. 2014;55(6):1413–6. doi:10.3109/10428194.2013.836601.
Schoppmann S et al. Prognostic value of lymphangiogenesis and lymphovascular invasion in invasive breast cancer. Ann Surg. 2004;240(2):306–12.
Rosen PP. Tumor emboli in intramammary lymphatics in breast carcinoma: pathologic criteria for diagnosis and clinical significance. Pathol Annu. 1983;18(Pt 2):215–32.
Lyman GH, Giuliano AE, Somerfield MR, et al. American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol. 2005;23:7703–20.
McCready DR, Yong WS, et al. Influence of the new AJCC breast cancer staging system on sentinel lymph node positivity and false-negative rates. J Natl Cancer Inst. 2004;96:873–5.
Viale G, Zurrida S, Maiorano E, et al. Predicting the status of auxillary sentinel lymph nodes in 4351 patients with invasive breast carcinoma treated in a single institution. Cancer. 2005;103:492–500.
Shibata MA, Morimoto J, Shibata J, Otsuki Y. Combination therapy with short interfering RNA vectors against VEGF-C and VEGF-A suppresses lymph node and lung metastasis in a mouse immunocompetent mammary cancer model. Cancer Gene Ther. 2008;15:776–86.
Xiao-wen HE, Xiao YU, Ting L, Shi-yi YU, Dao-jin C. Vector-based RNA interference against vascular endothelial growth factor-C inhibits tumor lymphangiogenesis and growth of colorectal cancer in vivo in mice. Chin Med J. 2008;121:439–44.
Al-Mowallad A, Kirwan C, Byrne G, et al. Vascular endothelial growth factor-C in patients with breast cancer. In Vivo. 2007;21:549–51.
Tamura M, Ohta Y. Serum vascular endothelial growth factor-C level in patients with primary nonsmall cell lung carcinoma. A possible diagnostic tool for lymph node metastasis. Cancer. 2003;98:1217–22.
Tsirlis TD, Papastratis G, Masselou K, et al. Circulating lymphangiogenic growth factors in gastrointestinal solid tumors, could they be of any clinical significance? World J Gastroenterol. 2008;14:2691–701.
Wang TB, Deng MH, Qiu WS, Dong WG. Association of serum vascular endothelial growth factor-C and lymphatic vessel density with lymph node metastasis and prognosis of patients with gastric cancer. World J Gastroenterol. 2007;13:1794–8.
Tamura M, Oda M, Tsunezuka Y, et al. Chest CT and serum vascular endothelial growth factor-C level to diagnose lymph node metastasis in patients with primary non-small cell lung cancer. Chest. 2004;126:342–6.
Morgillo F, De Vita F, Antoniol G, et al. Serum insulin-like growth factor 1 correlates with the risk of nodal metastasis in endocrine-positive breast cancer. Curr Oncol. 2013;20:e283–8.
George ML, Eccles SA, Tutton MG, Abulafi AM, Swift RI. Correlation of plasma and serum vascular endothelial growth factor levels with platelet count in colorectal cancer: clinical evidence of platelet scavenging? Clin Cancer Res. 2000;6:3147–52.
Acknowledgments
We thank all the patients and family for their help to do this work.
Ethical standards
This study was approved by the hospital ethics committee and was conducted in accordance with the principles of the Declaration of Helsinki (Seoul, 2008). All patients gave their written informed consent to participate in the study. Project data were collected anonymously, following Spanish data protection legislation (Act 15/1999 of 15 December).
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Drs Rueda, Zarcos and Pérez-Ruiz and Rivas-Ruiz and Redondo belong to REDISSEC.
Rights and permissions
About this article
Cite this article
Pérez, D., Rohde, A., Callejón, G. et al. Correlation between serum levels of vascular endothelial growth factor-C and sentinel lymph node status in early breast cancer. Tumor Biol. 36, 9285–9293 (2015). https://doi.org/10.1007/s13277-015-3663-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3663-0