Abstract
The aim of this study was to investigate the role of ultrasonographic microvascular imaging in the evaluation of prognosis of patients with invasive breast cancer treated by adjuvant therapies. A total of 121 patients with invasive breast cancer underwent ultrasonographic contrast-enhanced imaging, vascular endothelial growth factor (VEGF) staining, and microvessel density (MVD) counts. The parameters of microvascular imaging and the expression of VEGF and MVD in primary breast cancer were calculated. The correlation between these factors and the overall and progression-free survival rate were analyzed using the Kaplan-Meier method. Among 121 cases, the positive VEGF cases were 75 and negative ones were 46. The cut point of 52.3 was calculated by the regressive curve for MVD counts. The data showed the mean intensity (MI) was positively associated with both the MVD counts (r = .51, p < .001) and VEGF expression (r = .35, p < .001). For the prognosis of patients, high VEGF expression and MVD counts were associated with reduced progressive and survival times (PFS, p = .032 and p = .034; OS, p = .041 and p = .038, respectively). The correlation between parameters of microvascular imaging, VEGF expressive status, and the MVD counts were established. The cut point of mean intensity (MI = 40) was used to investigate as an independent predictor for PFS (p = .021) and OS (p = .025), respectively, due to a strong correlation between MVD counts and VEGF expression in patients with invasive breast cancer. The microvascular imaging could be a visual and helpful tool to predict the prognosis of patients with invasive breast cancer treated by adjuvant therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most frequently diagnosed cancer and has become the sixth leading cause of cancer-related death in Chinese women [1]. The locoregional spread and recurrence of the breast cancer is the leading cause of breast cancer-related death. Invasive breast cancer occurs from inside the breast ducts or lobules and invades into nearby breast tissue. So far, a variety of models was performed to predict the survival and recurrent rate of invasive breast cancer, including angiogenetic makers or other tumor factors, for optimizing the consensus treatments [2–5].
Angiogenesis is an essential factor to stimulate the tumor growth and development of metastases [6]. Vascular endothelial growth factor (VEGF), also know as vascular permeability factor, has the ability to increase vascular permeability, cell migration, and proliferation [7]. Microvascular density (MVD) is shown at the vascular “hot spot” with the probability of metastasis in different stages of invasive breast cancer [8]. Large-scale studies of the value of VEGF and MVD on the prediction of prognosis of breast tumors were reported [9, 10].
To investigate whether the presence of vascular spots and microvessel density in the breast cancer are correlated with a worse prognosis, we performed the combination methods including the angiogenetic markers and microvascular imaging to evaluate the prognosis of patients with invasive breast cancer after treating adjuvant therapies.
In our study, we intend to perform microvascular imaging to assess the angiogenesis of invasive breast cancer to predict prognosis after treating with chemotherapy and endocrine therapy. Microvascular imaging by ultrasound contrast agents could be used in the evaluation of angiogenesis of breast tumors. Ultrasonographic contrast agents within the microvessels of tumors, as the second generation bubbles, could be detected by ultrasonic backscatter imaging [5, 11, 12]. After systematic adjuvant treatments, such as chemotherapy or endocrine treatment, the vascularization of the primary tumor would be altered. The status of vascular makers or imaging could be considered the indicators for the prediction of relapse or survival in patients with breast cancer. The tumor relapse and recurrence of breast carcinoma are predominant factors in the assessment of the survival rate of patients with invasive breast cancer after delivering adjuvant treatments. The outcome of patients with breast cancer should be studied as the indicators of making the therapeutic determination.
In this report, we show that parameters of microvascular imaging, expression of VEGF, and microvessel counts are predictors for overall and progression-free survival rate in patients with invasive breast cancer after adjuvant treatments. The results of microvascular imaging reveal that it could be a visual tool to evaluate the angiogenesis of carcinomas and to provide the evidence for making decision in the treatment of multiple cancers.
Patients and methods
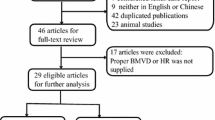
The clinical characteristics and therapeutic strategies were collected from 121 patients with invasive breast carcinomas, diagnosed and treated between 2009 and 2010 in Tianjin Medical University Cancer Institute and Hospital. The median age in our study is 52 years. The tumor classification and staging were conducted based on the International Union Against Cancer tumor-node-metastasis (UICC-TNM) [13]. The new adjuvant systemic treatment was administered to all patients to receive chemotherapy with 6 cycles of taxol epirubicin or taxol epirubicin cyclophosphamide) (TA or TAC). Patients were performed with ultrasonic contrast imaging with contrast agent SonoVue@ before adjuvant chemotherapy. In all cases, data regarding tumor size, histologic type, estrogen receptor (ER), progesterone receptor (PR) status, axillary lymph node metastases, VEGF protein expression, microvacular density counts, and parameters of ultrasonic contrast imaging were collected. The median follow-up time for survivors was 41 months. This protocol was approved by the Institutional Ethical Board of Tianjin Cancer Hospital.
VEGF and microvessel density analysis
Samples from the surgical resection were collected and analyzed by immunohistochemical (IHC) examination to measure the CD34 MVD counts (a mouse antihuman CD34 monoclonal antibody, ZM-0046; ZSGB-BIO Corporation, Beijing, China) and VEGF (a mouse monoclonal antibody, VEGF, VG-1, Abcam company, MA, USA) expression level. For each breast tumors, the IHC results were analyzed by a pathologist with 10 years of experience in pathologic diagnosis. The technique details in this study have been described in previous publications [5, 12]. Microvessels labeled with the CD34 antibody were also counted by a pathologist with 10 years of experience in the pathologic diagnosis. Each slide was examined at a low magnification (×40) to identify four separate areas containing the greatest number of microvessels (“hot spots”). Individual vessels from these hot spots were subsequently counted on a ×400 field.
As previous methods have shown [5, 12], VEGF expression were graded according to the percentage of positively stained tumor cells (0, 0 %immunopositive cells; 1, <25 % positive cells; 2, 26–50 % positive cells; and 3, >50 % positive cells) and the staining intensity (0, negative; 1, weak; 2, moderate; and 3, high). Combined scores of 0 to 2 for the above parameters were graded as negative; scores of 3 and 4 were graded as positive; and scores of 5 and 6 were graded as strongly positive. A sample score of greater than 3 and less than 3 was regarded as the high and low VEGF expression, respectively.
Microvascular imaging by ultrasonographic contrast agent
A total of 121 patients were performed ultrasonographic microvascular imaging examination by the 9M transducer (IU22, Phillip Medical Systems, USA) before treatment performance, including surgery and adjuvant therapy. A dose of 2.4-ml contrast agent SonoVue (sulfur hexafluoride microbubbles, Braco Company, Italy) was injected intravenously via a 20-gauge intravenous cannula in 1–2 s, followed by 5 ml saline solution. The real-time CEUS imaging process lasted for 180 s. The mechanical index (MI) of 0.06 and the frame rate was 15 Hz. The whole CEUS process was stored on the hard disk of the scanner for picture archiving and communication systems) (PACS) review. When making the final diagnosis, the same radiologists (W.X. and Z.Y.) studied PACS review of CEUS blinded for diagnosis, respectively. Discordant findings were resolved by consensus review by a third radiologist. Breast lesions were then analyzed as time-intensity curves by QLAB software. For each patient, three ROIs in the tumor were selected, and the mean CEUS parameter value was considered as the final value. The region of interest was drawn as the same size of 5 mm2 in the remarkable perfusion area of a lesion. The time-intensity curve was analyzed for the following parameters: arrival time (AT) (seconds), defined as the first point of the curve clearly above the baseline intensity followed by a further rise; time to peak (in seconds), defined as the time from the start of injection to the maximum intensity of the curve; peak intensity (PI) (dB), defined as the intensity at the peak time; mean intensity (MI) (dB), defined as the average intensity during the whole time.
Statistical methods
Association between VEGF expression and parameters of microvascular imaging was tested by the Pearson chi-square test. Survival was predicted using the Kaplan-Meier method, and comparison between study groups was performed with the log-rank test. The optimal cutoff point for mean intensity of microvascular imaging, based on the lowest p value and the highest relative risk, was found at 52.3/×200 and 40.1 dB for OS. This cut point was also used in the univariate and multivariate analysis. The continuous variable in a univariate Cox regression test was performed to evaluate the different factors on survival. For each variable, the patients were classified in two prognostic categories. In all tests, the significance level was set to .05, and all tests were two sided.
Results
The basic characteristics of postmenopausal patients with invasive breast cancer (113 ductal invasive and 8 lobular invasive breast cancer) were shown as 95 of 121 patients underwent chemotherapy with six cycles of TA or TAC and 26 received a 40 mg of adjuvant tamoxifen daily for 5 years after the treatment of chemotherapy. The average of tumor size was 2.6 cm, stage with T1–2 N0–3 M0, and steroid receptor status (ER/PR) was positive for 85/76 cases of 121 patients. There were 86 (76.8 %) and 16 (14.2 %) cases with lymph node involvement in the adjuvant chemotherapy and endocrine treatment groups, respectively. Histological grades were evaluated in all cases, and majority of cases were grade II and III (47/121 and 57/121), respectively (Table 1).
The follow-up time for patients with the date of first recurrence or death has been documented. The metastatic sites including breast local recurrence, brain, bone, and soft tissue metastases were all recorded. Twenty-two recurrences and 19 deaths were involved in our series. The microvascular markers, VEGF, and MVD were stained for the breast cancer samples after the performance of operation. The results showed VEGF expression was positive in 75 and negative in 46 cases. There were 63 positive and 32 negative results for patients who received the adjuvant chemotherapy as well as 12 positive and 14 negative for those who received endocrine treatment (Table 2). Microvessel density (MVD) was performed in all cases for evaluation of microvascular distribution in breast carcinomas. The average numbers of microvessels per ×200 fields was 55.2 ± 21.1 (/×200), and the cut point of 52.3 was calculated by the regressive curve.
The ultrasonographic microvascular imaging was performed to detect the microvascular imaging within tumors before patients undergo further adjuvant treatments (Table 2). The correlation between parameters of microvascular imaging, VEGF expressive status, and the MVD counts were established in Table 3. The data showed the mean intensity (MI) was positively associated with both the MVD counts (r = .51, p < .001) and VEGF expression (r = .35, p < .001) in patients with breast carcinoma. Other parameters, besides the peak intensity (PI) showing correlated with MVD counts (r = .46, p = .001), did not demonstrate an association with microvascular markers in tumor samples. The progression-free survival rate was described to predict the first relapse of patients after performing the adjuvant chemotherapy or endocrine therapy. When VEGF status and the cut point of MVD count (value = 52) content were used to predict PFS and OS, the results demonstrated patients with higher VEGF expression and MVD counts had reduced progression-free and overall survival times compared to those with lower VEGF and MVD contents (PFS, p = .032 and p = .034; OS, p = .041 and p = .038, respectively) (Fig. 1). Because of the strong correlation between mean intensity and these two hispathologic markers, the cut point of mean intensity (MI = 40) was used to investigate the predicted value of PFS and OS in patients with invasive breast cancer. The data showed the mean intensity of microvascular imaging as an independent predictor for PFS (p = .021) and OS (p = .025), respectively (Fig. 1).
a–c Patients with invasive breast carcinoma was stained by VEGF marker. Positive VEGFs were shown (a), and the progression-free survival (PFS, b) and overall survival rate (OS, c) were analyzed using Kaplan-Meier plot based on VEGF expression. d–f Patients with invasive breast carcinoma was stained by microvessel density marker. The staining microvessels were shown (d), and the progression-free survival (PFS, e) and overall survival rate (OS, f) were analyzed using Kaplan-Meier plot based on the cutoff counts of MVD (MVD = 52). g–i Patients with invasive breast carcinoma was performed by ultrasonographic microvascular imaging. The images of microvascular in primary breast cancer were shown (g, arrows shown), and the progression-free survival (PFS, h) and overall survival rate (OS, i) were analyzed using Kaplan-Meier plot based on the mean intensity (cutoff point is 40 dB)
Discussion
A variety of studies showed that the angiogenesis plays a critical role in different stages of the occurrence, development, and prognosis of neoplasm [14, 15]. Microvascular density (MVD) and VEGF status could be standard methods to evaluate the angiogenesis of neoplasm. The high vascular volume of carcinoma is supposed to be associated with high MVD and would promote cancer cells immigration to other organs to form the metastatic foci. The VEGF contributes to the angiogenesis of tumor by acting on the vascular endothelial cell to enhance the permeability of vessels within tumor and then promote the invasion and metastasis of carcinoma [15]. In our study, the results of vascular endothelial growth factor (VEGF) and microvessel density demonstrated higher VEGF expression, and MVD counts had a statistical association with lower overall and progression survival rate (OS and PFS) among patients with invasive breast cancer treated by subsequent adjuvant therapy. Therefore, the angiogenic makers, such as VEGF factor and microvessel density within tumors, could be considered as indicators for recurrent rate or even survival rate of patients with invasive breast cancer.
As some independent studies shown, increasing microvessels density and the content of VEGF demonstrated a worse prognosis for patients with primary tumor [16, 17]. Linderholm B et al. [17] showed an observation that the quantitative measurement of VEGF content could predict the responsiveness to the adjuvant endocrine therapy of breast cancer. Patients with a high VEGF expression in the primary tumor had a worse PFS and OS after treatment with chemotherapy and endocrine therapy. The preferred parameter for quantification of angiogenesis was found in previous studies, such as endothelial cell proliferation fraction. Vascular endothelial growth factor and microvessel density were also used to find out the association between the clinicopathological data and angiogenesis. Arapandoni et al. [18] demonstrated a correlation between microvascular hotspots and the primary tumor. The microvessel density could predict the survival rate in our series, but limited number of patients enrolled restricts the value of MVD as a maker in other cohort studies. Furthermore, some authors do not detect the same associations because of different study population and difficult results from the comparable methodologies of angiogenesis quantification [19, 20]. Thus, the quantity of angiogenesis calculated by the parameters of microvascular imaging combined with VEGF and MVD would be of note in our clinical practice. In our cohort study, the microvascular imaging provides a visualized method to evaluate the angiogenic growth in breast cancer.
We performed ultrasonographic contrast-enhanced imaging in patients with breast cancer before surgery and adjuvant treatments. The analyses of parameters of microvascular imaging showed that one of parameters (mean intensity, MI) was strongly associated with both VEGF and MVD counts in our patients. Thus, the cut point of MI was used to evaluate the PFS and OS in our cohort. The results revealed the mean intensity of microvascular imaging as an independent predictor for PFS and OS. In the conventional ultrasonic methods, Color Doppler has been used to evaluate the status of small vessels within different carcinomas [21]. However, the level of small arteries or veins, rather not microvessels within lesions, could be demonstrated by Color Doppler. Thus, contrast ultrasound could be considered as a promising tool to display the microvascular status within the parenchyma of tumor by overcoming the pitfall of Color Doppler [21]. According to other parameters, including peak time, peak and mean intensity, they would be influenced by a variety of factors, such as the dose of contrast agent, the injection speed, and cardiac status of subjects. Based on our data, the low MI of microvascular imaging was expected to have a good correlation with poor prognosis of breast cancer patients.
Although we found good results of microvascular imaging for the evaluation of prognosis of patients with breast cancer, some limitations in this study should be illuminated. Firstly, the different chemotherapy or endocrine therapy protocols in the treatment of patients with invasive breast cancer would have an influence on the prognosis and recurrent rate. Secondly, the microvascular status would be changed in primary breast cancers after treatment with sequential therapies. Furthermore, lymph nodes involvement should be stained by IHC markers or performed by microvascular imaging for further investigation.
In summary, we speculate that the microvascular imaging could evaluate the angiogenic status in primary breast cancer. The parameters of microvascular imaging would be a promising quantitative measurable tool for predicting disease progression in multiple carcinomas after adjuvant treatments.
References
Fan L, Strasser-Weippl K, Li JJ, St Louis J, Finkelstein DM, Yu KD, et al. Breast cancer in China. Lancet Oncol. 2014;15(7):e279–89.
Fox S, Leek R, Smith K, Hollyer J, Greenall M, Harris A. Tumor angiogenesis in node-negative breast carcinomas-relationship with epidermal growth factor receptor, estrogen receptor, and survival. Breast Cancer Res Treat. 1994;29:109–16.
Weidner N, Semple J, Welch W, Folkman J. Tumor angiogenesis and metastasis—correlation in invasive breast carcinoma. N Engl J Med. 1991;324:1–8.
Hansen S, Grabau D, Sorensen F, Bak M, Vach W, Rose C. The prognostic value of angiogenesis by Chalkley counting in a confirmatory study design on 836 breast cancer patients. Clin Cancer Res. 2000;6:139–46.
Wei X, Li Y, Zhang S, Ming G. Evaluation of thyroid cancer in Chinese females with breast cancer by vascular endothelial growth factor (VEGF), microvessel density, and contrast-enhanced ultrasound (CEUS). Tumour Biol. 2014;35(7):6521–9.
Folkman J. How is blood vessel growth regulated in normal and neoplastic tissue? G.H.A. Clowes Memorial Award Lecture. Cancer Res. 1986;46:467–73.
Leung DW, Cachianes G, Kuang WJ, Goeddel DV, Ferrara N. Vascular endothelial growth factor is a secreted angiogenic mitogen. Science. 1989;246:1306–9.
Bosari S, Lee AKC, De Lellis RA, Wiley BD, Heatley GJ, Silverman ML. Microvessel quantification and prognosis in invasive breast carcinoma. Hum Pathol. 1992;23:755–61.
Schneider BP, Gray RJ, Radovich M, Shen F, Vance G, Li L, et al. Prognostic and predictive value of tumor vascular endothelial growth factor gene amplification in metastatic breast cancer treated with paclitaxel with and without bevacizumab; results from ECOG 2100 trial. Clin Cancer Res. 2013;19(5):1281–9.
Linardou H, Kalogeras KT, Kronenwett R, Kouvatseas G, Wirtz RM, Zagouri F, et al. The prognostic and predictive value of mRNA expression of vascular endothelial growth factor family members in breast cancer: a study in primary tumors of high-risk early breast cancer patients participating in a randomized Hellenic Cooperative Oncology Group trial. Breast Cancer Res. 2012;14(6):R145.
Wei X, Li Y, Zhang S, Xin XJ, Zhu L, Gao M. The role of contrast-enhanced ultrasound (CEUS) in the early assessment of microvascularization in patients with aggressive B-cell lymphoma treated by rituximab-CHOP: a preliminary study. Clin Hemorheol Microcirc. 2014;58(2):363–76.
Xu Y, Zhang S, Wei X, Pan Y, Hao J. Contrast enhanced ultrasonography prediction of cystic renal mass in comparison to histopathology. Clin Hemorheol Microcirc. 2014;58(3):429–38.
Uehiro N, Horii R, Iwase T, Tanabe M, Sakai T, Morizono H, et al. Validation study of the UICC TNM classification of malignant tumors, seventh edition, in breast cancer. Breast Cancer. 2014;21(6):748–53.
Koutras A, Kotoula V, Fountzilas G. Prognostic and predictive role of vascular endothelial growth factor polymorphisms in breast cancer. Pharmacogenomics. 2015;16(1):79–94.
Gasparini G. Prognostic value of vascular endothelial growth factor in breast cancer. Oncologist. 2000;5:37–44.
Toi M, Kashitani J, Tominaga T. Tumor angiogenesis is an independent prognostic indicator in primary breast carcinoma. Int J Cancer. 1993;55:371–4.
Linderholm B, Grankvist K, Wilking N, Johansson M, Tavelin B, Henriksson R. Correlation of vascular endothelial growth factor content with recurrences, survival, and first relapse site in primary node-positive breast carcinoma after adjuvant treatment. J Clin Oncol. 2000;18(7):1423–31.
Arapandoni-Dadioti P, Giatromanolaki A, Trihia H, Harris AL, Koukourakis M. Angiogenesis in ductal breast carcinoma. Comparison of microvessel density between primary tumour and lymph node metastasis. Cancer Lett. 1999;137:145–50.
Schindl M, Schoppmann S, Samonigg H, Hausmaninger H, Kwasny W, Gnant M, et al. Overexpression of hypoxia-inducible factor 1alpha is associated with an unfavorable prognosis in lymph node-positive breast cancer. Clin Cancer Res. 2002;8:1831–7.
Blackwell K, Dewhirst M, Liotcheva V, Snyder S, Broadwater G, Bentley R, et al. HER-2 gene amplification correlates with higher levels of angiogenesis and lower levels of hypoxia in primary breast tumors. Clin Cancer Res. 2004;10:4083–8.
Wei X, Li Y, Zhang S, Li X, Wang H, Yong X, et al. Evaluation of microvascularization in focal salivary gland lesions by contrast-enhanced ultrasonography (CEUS) and Color Doppler sonography. Clin Hemorheol Microcirc. 2013;54(3):259–71.
Acknowledgments
This work is supported by a grant from the National Natural Science Foundation of China (No. 81401412).
Author information
Authors and Affiliations
Corresponding author
Additional information
Ying Li and Xi Wei contributed equally to this work.
Rights and permissions
About this article
Cite this article
Li, Y., Wei, X., zhang, S. et al. Prognosis of invasive breast cancer after adjuvant therapy evaluated with VEGF microvessel density and microvascular imaging. Tumor Biol. 36, 8755–8760 (2015). https://doi.org/10.1007/s13277-015-3610-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3610-0