Abstract
Hypoxia can induce HIF-1α expression and promote the epithelial-mesenchymal transition (EMT) and invasion of cancer cells. However, their mechanisms remain unclear. The objective of this study was to evaluate the role of Gli-1, an effector of the Hedgehog pathway, in the hypoxia-induced EMT and invasion of breast cancer cells. Human breast cancer MDA-MB-231 cells were transfected with HIF-1α or Gli-1-specific small interfering RNA (siRNA) and cultured under a normoxic or hypoxic condition. The relative levels of HIF-1α, Gli-1, E-cadherin, and vimentin in the cells were characterized by quantitative RT-PCR and Western blot assays, and the invasion of MDA-MB-231 cells was determined. Data was analyzed by Student T test, one-way ANOVA, and post hoc LSD test or Mann-Whitney U when applicable. We observed that hypoxia significantly upregulated the relative levels of vimentin expression, but downregulated E-cadherin expression and promoted the invasion of MDA-MB-231 cells, associated with upregulated HIF-1α translation and Gil-1 expression. Knockdown of HIF-1α mitigated hypoxia-modulated Gil-1, vimentin and E-cadherin expression, and invasion of MDA-MB-231 cells. Knockdown of Gil-1 did not significantly change hypoxia-upregulated HIF-1α translation but completely eliminated hypoxia-modulated vimentin and E-cadherin expression and invasion of MDA-MB-231 cells. These data indicate that Gil-1 is crucial for hypoxia-induced EMT and invasion of breast cancer cells and may be a therapeutic target for intervention of breast cancer metastasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the leading cause of cancer-related mortality in women in the USA. About 1.3 million women are diagnosed with breast cancer each year in the world [1]. Currently, therapeutic strategies, including surgical removal of tumor, chemotherapy, radiotherapy, and endocrine therapy, have improved the survival rate of patients with breast cancer. However, the recurrence, metastasis, and refractory to therapy of breast cancer affect many patients, particularly for the local and distant metastasis, which remains serious threats to patients [2]. Therefore, understanding the molecular mechanisms underlying the metastasis of breast cancer will be of great significance.
Previous studies have indicated that the tumor microenvironment and inflammatory mediators can promote the epithelial-mesenchymal transition (EMT) of cancer and cancer stem cells, which is crucial for the metastasis of cancer [3–5]. During the EMT process, epithelial cells lose their cell polarity and cell-cell junctions and gain mesenchymal properties of migration and invasion as well as morphology. Furthermore, cancer cells undergoing the EMT usually decrease their E-cadherin expression, but increase their vimentin and fibronectin expression, invading through the basement membrane and distant organs, which the invaded cancer cells undergo the MET and colonize into the solid metastatic tumors [3, 6]. Hence, the EMT process is necessary for the invasion-metastasis cascade of cancer.
Solid tumors usually experience a hypoxic environment, which mainly resulted from imbalance of abnormal vascularization and aggressive growth of tumors. Previous studies have shown that hypoxia play an important role in tumor invasiveness, metabolism, and stemness induction [7–9]. Hypoxia can induce the expression of hypoxia inducible factors (HIFs) which are overexpressed in many carcinomas, including breast cancer [10]. HIF-1α can, through its signaling, directly regulate the proliferation, invasion, and EMT of cancer cells by triggering the expression of vascular endothelial growth factor (VEGF) and endothelin-1 [11–13]. Furthermore, HIF-1α can also indirectly crosstalk with other signal pathways, such as the NF-κB, Hedgehog (Hh), and Wet/β-catenin pathways to promote the invasion and EMT of cancer cells [14–16]. Aberrant activation of the Hedgehog (Hh) pathway is implicated in the development of several tumors, including brain, pancreas, and breast cancer. Previous studies have shown that activation of the Hedgehog pathway can promote myofibroblast differentiation, stromal hyperplasia, and extracellular matrix (ECM) production, which facilitate the EMT process, invasion, and metastasis of breast cancer [17, 18]. Gli-1 is a transcriptional factor of the Hedgehog pathway. High levels of Gli-1 expression have been detected in some breast cancers and are associated with the invasiveness of breast cancer [19]. High levels of Gli-1 expression are also associated with the poor prognosis and represent progressive stages of disease [20]. We have recently showed that hypoxia can induce EMT and enhance the invasiveness of pancreatic cancer cells by upregulating Gli-1 expression [21]. However, the roles of Gli-1 in the hypoxia-induced EMT and invasion of breast cancer cells as well as its relationship with HIF-1α have not been clarified.
In this study, we investigated the effects of HIF-1α or Gli-1 silencing on the hypoxia-induced EMT and invasion as well as the expression of HIF-1α and Gil-1 in breast cancer cells.
Materials and methods
Cell culture
Human breast cancer MDA-MB-231 cells were purchased from the Cell Bank of the Chinese Academy of Sciences (Shanghai, China) and were cultured in L-15 medium (Sigma, Saint Louis, MO, USA) supplemented with 10 % heat-inactivated fetal bovine serum (FBS) (HyClone), 100 units/ml ampicillin, and 100 μg/ml streptomycin at 37 °C in a humidified atmosphere of 5 % CO2 as a normoxic condition. To evaluate the effects of hypoxia, MDA-MB-231 cells were cultured under the normoxic condition up to 65–70 % confluence and subsequently cultured in a consistent 3 % O2 hypoxic condition for 48 h, as described previously [22, 23].
RNA interference
The specific small interfering RNA (siRNA) for HIF-1α (5′-CCACCACUGAUGAAUUAAATT-3′, 5′-UUUAAUUCAUCAGUGGUGGTT-3′), for Gli-1 (5′-GGCUCAGCUUGUGUGUAAUTT-3′, 5′-AUUACACACAAGCUGAGCCTT-3′), and a negative control siRNA (5′-UUCUCCGA ACGUGUCACGUTT-3′, 5′-ACGUGACACGUUCGGAGAATT-3′) were obtained from GenePharm (Shanghai, China). MDA-MB-231 cells (2 × 105 per well) were cultured in a six-well plate and transfected with 100 nM siRNA using Lipofectamine 2000 (Invitrogen, CA, USA), according to the manufacturers’ instruction. Forty-eight hour after transfection, the cells were harvested for further experiments.
Cell invasion assay
The impact of hypoxia on the invasion of cancer cells was determined by invasion assays using a Millicell invasion chamber (Millipore, Billerica, MA, USA). Briefly, the membrane in the upper chamber was coated with Matrigel (Becton Dickinson Labware, Bedford, MA, USA). MDA-MB-231 cells (5 × 104) were cultured in the upper chamber in serum-free media for 24 h. After the non-invading, cells were removed from the upper surface of membrane using a cotton swab and the invaded cells on the bottom surface of the membrane were stained with crystal violet. The invaded cells at eight random fields of each membrane were photographed at magnification ×100 and counted.
Quantitative real-time PCR assay
MDA-MB-231 cells were cultured in the experimental conditions. Their total RNA was extracted using the TRIzol Reagent (Invitrogen, CA, USA) and reversely transcribed into cDNA using a PrimeScript RT reagent Kit (TaKaRa, Dalian, China), according to the manufacturer’s instruction. The relative levels of target gene messenger RNA (mRNA) transcript were determined by quantitative real-time PCR assay (qRT-PCR) using the SYBR Green Master Mix and specific primers in the iQ5 Multicolor Real-Time PCR Detection System (Bio-Rad, Hercules, CA, USA). The cycling conditions were as follows: denaturation at 95 °C for 30 s and followed by 40 cycles of denaturation at 95 °C for 5 s, annealing at 60 °C for 30 s, and extension at 72 °C for 30 s. A melting curve analysis was used to evaluate the specificity of the amplified PCR products. The sequences of primers were forward 5′-CGCAAGTCCTCAAAGCACAGTTAC-3′ and reverse 5′-GCAGTGGTAGTGGTGGCATTAGC-3′ for HIF-1α (81 bp); forward 5′-GGGATGATCCCACATCCTCAGTC-3′ and reverse 5′-CTGGAGCAGCCCCCCCAGT-3′ for Gli-1 (344 bp); forward 5′-ATTCTGATTCTGCTGCTCTTG-3′ and reverse 5′-AGTCCTGGTCCTCTTCTCC-3′ for E-cadherin (136 bp); forward 5′-AATGACCGCTTCGCCAAC-3′ and reverse 5′-CCGCATCTCCTCCTCGTAG-3′ for vimentin (135 bp); and forward 5′-GAAGGTGAAGGTCGGAGT-3′ and reverse 5′-CATGGGTGGAATCATATTGGAA-3′ for GAPDH (155 bp). The relative levels of target gene mRNA transcripts to GAPDH were determined by 2−ΔΔCt [24].
Western blot analysis
MDA-MB-231 cells were cultured in the experimental conditions and lysed on ice for 20 min by using a lysis buffer (40 mM Tris pH 7.4, 10 mM NaF, 5 mM ethyleneglycol-bis- tetraacetic acid, 2 mM ethylenediaminetetraacetic acid, 0.3 % Triton X-100, 0.35 mM vanadate, 10 % glycerol, β-glycerophosphate, and protease inhibitors; Roche, Penzberg, Germany). After centrifugation, the cell lysate (100 μg) was separated in a 10 % sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) gels and transferred onto polyvinylidene fluoride (PVDF) membranes (Roche). The membranes were blocked using 5 % non-fat dry milk in TBST (150 mM NaCl, 0.05 % Tween 20, 10 mM Tris–HCl, pH 8.0) and were subsequently incubated with primary anti-E-cadherin (Santa Cruz Biotechnology), anti-HIF-1α (Bioworld, St. Louis Park, MN, USA), anti-vimentin, anti-Gli-1, or anti-β-actin (Cell Signaling Technology, Beverly, MA, USA) overnight at 4 °C. After being washed, the bound antibodies were detected with horseradish peroxidase (HRP)-conjugated secondary antibodies at room temperature for 2 h and visualized using an enhanced chemiluminescence detection system. The relative levels of target protein to the control β-actin were analyzed by densitometric scanning using Image-Pro Plus 5.0 software (Media Cybernetics, Inc. Rockville, MD, USA).
Statistical analysis
Data are present as means ± standard deviation (SD). The difference was analyzed by student T test, one-way ANOVA, and post hoc LSD test or Mann-Whitney U test when applicable using the SPSS13.0 software (version 13.0; SPSS, Chicago, IL, USA). A p value of <0.05 was considered statistically significant.
Results
Hypoxia facilitates the EMT process and invasion of breast cancer cells
Hypoxia can promote the invasion of cancer cells, which is associated with enhancing the EMT process [11]. To investigate the role of hypoxia in the EMT and invasion of breast cancer cells, MDA-MB-231 cells were cultured under a normoxic (21 % O2) or hypoxic condition (3 % O2) for 48 h. The relative levels of E-cadherin and vimentin expression in the cells and their invasion were characterized by qRT-PCR, Western blot, and invasion assays. As shown in Fig. 1a, b, the relative levels of E-cadherin expression in the cells under a hypoxic condition were significantly lower than that in the normoxic condition (p < 0.05, tested by student T test). In contrast, the relative levels of vimentin expression in the cells under a hypoxic condition were significantly higher than that in the normoxic condition (p < 0.05, tested by student T test). Furthermore, the numbers of invaded cells from cultured in the hypoxic condition were significantly greater than that in the normoxic condition (p < 0.05, Fig. 1c). Hence, hypoxia promoted the EMT process and invasion of breast cancer cells in vitro.
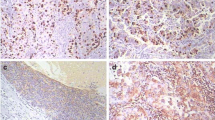
Hypoxia induces the EMT and invasion of breast cancer cells. MDA-MB-231 cells were cultured in a normoxic or hypoxic condition for 48 h. a Western blot analysis of the E-cadherin and vimentin expression in MDA-MB-231 cells. b qRT-PCR analysis of the relative levels of gene mRNA transcripts. c The invasion of breast cancer cells (×100 magnification). Data are representative images and expressed as the means ± SD of individual groups of cells from three separate experiments. *p < 0.05. vs. the normoxic controls
Hypoxia enhances HIF-1α translation and upregulates Gli-1 expression in breast cancer cells
Hypoxia induces HIF-1α, which can activate the NF-κB pathway and crosstalk with other signaling events to regulate the proliferation, apoptosis, and metastasis of cancer cells [10]. Our previous study has shown that hypoxia can upregulate the expression of HIF-1α and Gli-1 in pancreatic cancer cells [21]. To understand the role of hypoxia in regulating the metastasis of breast cancer cells, MDA-MB-231 cells were cultured in the normoxic or hypoxic condition for 48 h and the relative levels of HIF-1α and Gli-1 expression and their invasion were determined. The relative levels of HIF-1α and Gli-1 protein expression in the cells cultured in a hypoxic condition were obviously higher than that in the normoxic condition (Fig. 2a). However, the relative levels of Gil-1, but not HIF-1α, mRNA transcripts in the cells cultured in the hypoxic condition were significantly higher than that in the normoxic condition (p < 0.05, tested by student T test, Fig. 2b). Thus, hypoxia enhanced HIF-1α translation and Gil-1 expression in breast cancer cells in vitro.
Effects of hypoxia on the relative levels of HIF-1α and Gli-1 expression in breast cancer cells. MDA-MB-231 cells were cultured in a normoxic or hypoxic condition for 48 h. The relative levels of HIF-1α and Gli-1 expression were determined by Western blot (a) and qRT-PCR assay (b). Data are representative images and expressed as the means ± SD of individual groups of cells from three separate experiments. *p < 0.05 vs. the normoxic controls
Knockdown of HIF-1α expression abolishes hypoxia-induced Gli-1 expression and EMT process in breast cancer cells
To evaluate the role of HIF-1α further, MDA-MB-231 cells were transfected with the HIF-1α-specific or control siRNA and cultured in the normoxic or hypoxic condition for 48 h, followed by analysis of their Gil-1, E-cadherin and vimentin expression, and invasion. Transfection with the HIF-1α-specific siRNA, but not with control siRNA, dramatically downregulated HIF-1α expression in MDA-MB-231 cells, demonstrating effective HIF-1α knockdown (p < 0.05, tested by Mann-Whitney U test, Fig. 3a, b). Western blot analyses indicated while significant difference in the levels of Gli-1, E-cadherin, and vimentin expression among different groups of cells (p < 0.05, tested by one-way ANOVA and post hoc LSD test), the relative levels of Gil-1, E-cadherin, and vimentin expression in the HIF-1α-silencing cells cultured in the hypoxic condition were similar to that in the normoxic condition, demonstrating that knockdown of HIF-1α eliminated hypoxia-induced Gil-1 expression and EMT process in MDA-MB-231 cells (Fig. 3c). More interestingly, while there was a significant difference in the numbers of invaded cells cultured in normoxic condition, related to that in a hypoxic condition (p < 0.05, determined by Mann-Whitney U test) knockdown of HIF-1α also mitigated hypoxia-induced invasion of MDA-MB-231 cells (Fig. 3d), suggesting that higher levels of Gil-1 expression may be crucial for the invasion of MDA-MB-231 cells.
Knockdown of HIF-1α reverses the hypoxia-induced Gli-1 upregulation, EMT process, and invasion of breast cancer cells. MDA-MB-231 cells were transfected with the HIF-1α-specific or control siRNA and cultured in a normoxic or hypoxic condition for 48 h. a Western blot analysis of HIF-1α expression. b qRT-PCR analysis of HIF-1α mRNA transcripts. c Western blot analysis of the relative levels of Gli-1, E-cadherin, and vimentin expression. d The numbers of invaded cells. Data are representative images and expressed as the means ± SD of individual groups of cells from three separate experiments.*p < 0.05 vs. the normoxic controls
Knockdown of Gli-1 expression mitigates hypoxia-enhanced EMT process and invasion of breast cancer cells
To test the importance of Gil-1 in regulating hypoxia-induced EMT process and invasion, MDA-MB-231 cells were transfected with the Gil-1-specific siRNA or control RNA and cultured under a hypoxic or normoxic condition, followed by analysis of their Gil-1, HIF-1α, E-cadherin, and vimentin expression and invasion. First, the relative levels of Gil-1 in the cells transfected with the Gil-1-specific siRNA were dramatically reduced, as compared with that in the control siRNA-transfected cells, demonstrating effective knockdown of Gil-1 expression (p < 0.05, determined by student T test, Fig. 4a, b). Second, while significantly greater numbers of invaded cells were detected in the control siRNA-transfected cells cultured in the normoxic condition (p < 0.05, determined by student T test), the numbers of invaded cells in the Gil-1-specific siRNA-transfected cells cultured in the hypoxic condition were similar to that in the normoxic condition, indicating that knockdown of Gil-1 mitigated hypoxia-induced invasion of breast cancer cells in our experimental conditions (Fig. 4c, d). Western blot analyses revealed that the relative levels of HIF-1α expression in the cells cultured in the hypoxic condition were significantly higher than that in the normoxic condition (p < 0.05, determined by student T test), regardless of Gil-1 silencing, demonstrating that knockdown of Gil-1 did not significantly modulate hypoxia-enhanced HIF-1α expression in MDA-MB-231 cells (Fig. 4e). Furthermore, there was a significant difference in the relative levels of Gil-1, E-cadherin, and vimentin expression in the control siRNA-transfected cancer cells between cultured in the normoxic and hypoxic conditions (p < 0.05, determined by student T test), but the difference was not detected in the Gil-1-silencing MDA-MB-231 cells. Therefore, knockdown of Gil-1 expression mitigated hypoxia-induced EMT and invasion of MDA-MB-231 cells.
Knockdown of Gli-1 mitigates the hypoxia-enhanced EMT and invasion, but not HIF-1α expression in MDA-MB-231 cells. MDA-MB-231 cells were transfected with the Gli-1-specific or control siRNA and cultured in a normoxic or hypoxic condition for 48 h. a Western blot analysis of Gli-1 expression. b qRT-PCR analysis of Gli-1 mRNA transcripts. c Western blot analysis of Gli-1, E-cadherin, and vimentin expression. d The numbers of invaded cells. Data are representative images and expressed as the means ± SD of individual groups of cells from three separate experiments.*p < 0.05 vs. the normoxic controls
Discussion
The EMT plays pivotal roles in the invasion and metastasis of cancers [25]. Previous studies have shown that hypoxia can enhance the EMT process by upregulating the expression of HIF-1α and other EMT-related transcription factors, such as Snail [12, 26]. Our previous study has shown that hypoxia induces HIF-1α, which crosstalks with the Hedgehog pathway to upregulate Gil-1 expression and promote the invasion of pancreatic cancer cells [21]. In this study, we investigated the roles of Gil-1 in the hypoxia-induced EMT and invasion of breast cancer cells and the relationship between the HIF-1α and Gil-1 expression in breast cancer cells cultured in a hypoxic condition. We found that hypoxia enhanced HIF-1α and Gil-1 expression and promoted the EMT and invasion of breast cancer cells. Knockdown of HIF-1α eliminated the hypoxia-enhanced Gli-1 expression, EMT, and invasion of breast cancer cells, while knockdown of Gil-1 did not affect the hypoxia-enhanced HIF-1α expression, but dramatically mitigated the hypoxia-enhanced EMT and invasion of breast cancer. These novel data suggest that Gil-1 may be crucial for the hypoxia-enhanced EMT and invasion of breast cancer and HIF-1α may crosstalk with the Hedgehog pathway to enhance hypoxia-induced Gil-1 expression and promote the EMT and invasion of breast cancer. Our findings suggest that Gil-1 may be a new target for intervention of breast cancer metastasis.
HIF-1 consists of HIF-1α and HIF-1β subunits [27, 28]. HIF-1α has two O2-dependent posttranslational modifications, and its expression is sensitive to hypoxia. Interestingly, we found that hypoxia failed to upregulate the relative levels of HIF-1α mRNA transcripts, but increased the relative levels of HIF-1α protein in breast cancer cells. This suggests that hypoxia may enhance the stability of HIF-1α mRNA and prevent its degradation, leading to enhanced HIF-1α translation in breast cancer cells [29–31]. Krishnamachary et al. [32] have demonstrated that HIF-1α is an important upstream regulator of the EMT process. It is possible that hypoxia induces HIF-1α expression, which induces Snail expression, leading to the suppression of E-cadherin and induction of vimentin in breast cancer cells. As a result, hypoxia enhances the EMT and invasion of breast cancer cells. Therefore, HIF-1α is a target for design of therapies for the prevention and intervention of breast cancer metastasis.
Previous studies have shown that HIF-1α can crosstalk with the Notch and NF-κB signaling to enhance the EMT process of cancer cells [11, 33]. Furthermore, hypoxia can stimulate the canonical Hodgehog signaling via upregulating HIF-1α expression in vitro and in vivo [34, 35]. Our previous study has shown that HIF-1α can crosstalk with the non-canonical Hedgehog pathway to promote hypoxia-enhanced EMT and invasion of pancreatic cancer [21]. We showed that hypoxia enhanced HIF-1α translation and upregulated Gli-1 expression to promote the EMT and invasion of breast cancer cells. A previous study has shown that the Hedgehog signaling events, such as SHH, SMO, PTCH, and Gli-1, are highly expressed in some breast cancers, associated with poor prognosis of breast cancer [36]. The Gli-1 is an effector of the Hedgehog pathway [37–39]. Particularly, induction of Gil-1 expression can occur independent of SMO regulation in some carcinomas, including medulloblastoma, glioma, breast and prostate cancers, and basal cell carcinoma [40]. We found that knockdown of Gli-1 dramatically mitigated the hypoxia-enhanced EMT and invasion of breast cancer cells in vitro. These data suggest that Gli-1 positively regulates the hypoxia-induced EMT and invasion of breast cancer cells, independent of enhancing vascularization. Given that many transcription factors and chemokines regulate the expression of E-cadherin and vimentin expression, it is possible that Gli-1 may regulate their expression indirectly promoting the EMT and invasion in breast cancer cells. We are interested in further investigating how HIF-1α signaling crosstalks with the Hedgehog pathway to promote Gli-1 expression and how Gli-1 regulates the EMT and invasion of breast cancer cells.
In summary, our data indicated that hypoxia induced HIF-1α translation and Gli-1 expression in breast cancer cells in vitro. Knockdown of HIF-1α eliminated the hypoxia-enhanced Gli-1 expression, EMT, and invasion of breast cancer cells. Knockdown of Gli-1 did not affect the relative levels of HIF-1α expression but significantly mitigated the hypoxia-enhanced EMT and invasion of breast cancer cells. Hence, our findings indicate that GLi-1 positively regulates the hypoxia-induced EMT and invasion of breast cancer and may be a target for intervention of breast cancer metastasis.
References
Benson JR, Jatoi I. The global breast cancer burden. Future Oncol. 2012;6(8):697–702.
Youlden DR, Cramb SM, Dunn NA, et al. The descriptive epidemiology of female breast cancer: an international comparison of screening, incidence, survival and mortality. Cancer Epidemiol. 2012;3(36):237–48.
Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. J Clin Invest. 2009;6(119):1420–8.
Thiery JP, Acloque H, Huang RY, et al. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;5(139):871–90.
Wang Y, Zhou BP. Epithelial-mesenchymal transition—a hallmark of breast cancer metastasis. Cancer Hallm. 2013;1(1):38–49.
Kalluri R, Neilson EG. Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest. 2003;12(112):1776–84.
Michieli P. Hypoxia, angiogenesis and cancer therapy: to breathe or not to breathe. Cell Cycle. 2009;20(8):3291–6.
Pennacchietti S, Michieli P, Galluzzo M, et al. Hypoxia promotes invasive growth by transcriptional activation of the met protooncogene. Cancer Cell. 2003;4(3):347–61.
Esteban MA, Tran MG, Harten SK, et al. Regulation of E-cadherin expression by VHL and hypoxia-inducible factor. Cancer Res. 2006;7(66):3567–75.
Semenza GL. Targeting HIF-1 for cancer therapy. Nat Rev Cancer. 2003;10(3):721–32.
Cheng ZX, Sun B, Wang SJ, et al. Nuclear factor-kappaB-dependent epithelial to mesenchymal transition induced by HIF-1alpha activation in pancreatic cancer cells under hypoxic conditions. PLoS ONE. 2011;8(6):e23752.
Imai T, Horiuchi A, Wang C, et al. Hypoxia attenuates the expression of E-cadherin via up-regulation of SNAIL in ovarian carcinoma cells. Am J Pathol. 2003;4(163):1437–47.
Sharp FR, Bernaudin M. HIF1 and oxygen sensing in the brain. Nat Rev Neurosci. 2004;6(5):437–48.
Semenza GL. HIF-1 and tumor progression: pathophysiology and therapeutics. Trends Mol Med. 2002;4(8):S62-7.
Harris AL. Hypoxia—a key regulatory factor in tumour growth. Nat Rev Cancer. 2002;1(2):38–47.
Gupta GP, Massague J. Cancer metastasis: building a framework. Cell. 2006;4(127):679–95.
Harmon EB, Ko AH, Kim SK. Hedgehog signaling in gastrointestinal development and disease. Curr Mol Med. 2002;1(2):67–82.
Bale AE, Yu KP. The hedgehog pathway and basal cell carcinomas. Hum Mol Genet. 2001;7(10):757–62.
Jeng KS, Sheen IS, Jeng WJ, et al. High expression of Sonic Hedgehog signaling pathway genes indicates a risk of recurrence of breast carcinoma. Onco Targets Ther. 2013;7:79–86.
Ten HA, Bektas N, Von SS, et al. Expression of the glioma-associated oncogene homolog (GLI) 1 in human breast cancer is associated with unfavourable overall survival. BMC Cancer. 2009;9:298.
Lei J, Ma J, Ma Q, et al. Hedgehog signaling regulates hypoxia induced epithelial to mesenchymal transition and invasion in pancreatic cancer cells via a ligand-independent manner. Mol Cancer. 2013;12:66.
Aleffi S, Petrai I, Bertolani C, et al. Upregulation of proinflammatory and proangiogenic cytokines by leptin in human hepatic stellate cells. Hepatology. 2005;6(42):1339–48.
Novo E, Cannito S, Zamara E, et al. Proangiogenic cytokines as hypoxia-dependent factors stimulating migration of human hepatic stellate cells. Am J Pathol. 2007;6(170):1942–53.
Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc. 2008;6(3):1101–8.
Huber MA, Kraut N, Beug H. Molecular requirements for epithelial-mesenchymal transition during tumor progression. Curr Opin Cell Biol. 2005;5(17):548–58.
Polyak K, Weinberg RA. Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer. 2009;4(9):265–73.
Wang GL, Semenza GL. Purification and characterization of hypoxia-inducible factor 1. J Biol Chem. 1995;3(270):1230–7.
Wang GL, Jiang BH, Rue EA, et al. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc Natl Acad Sci U S A. 1995;12(92):5510–4.
Ivan M, Kondo K, Yang H, et al. HIFalpha targeted for VHL-mediated destruction by proline hydroxylation: implications for O2 sensing. Science. 2001;5516(292):464–8.
Jaakkola P, Mole DR, Tian YM, et al. Targeting of HIF-alpha to the von Hippel-Lindau ubiquitylation complex by O2-regulated prolyl hydroxylation. Science. 2001;5516(292):468–72.
Yu F, White SB, Zhao Q, et al. HIF-1alpha binding to VHL is regulated by stimulus-sensitive proline hydroxylation. Proc Natl Acad Sci U S A. 2001;17(98):9630–5.
Krishnamachary B, Zagzag D, Nagasawa H, et al. Hypoxia-inducible factor-1-dependent repression of E-cadherin in von Hippel-Lindau tumor suppressor-null renal cell carcinoma mediated by TCF3, ZFHX1A, and ZFHX1B. Cancer Res. 2006;5(66):2725–31.
Chen J, Imanaka N, Chen J, et al. Hypoxia potentiates Notch signaling in breast cancer leading to decreased E-cadherin expression and increased cell migration and invasion. Br J Cancer. 2010;2(102):351–60.
Wang G, Zhang Z, Xu Z, et al. Activation of the sonic hedgehog signaling controls human pulmonary arterial smooth muscle cell proliferation in response to hypoxia. Biochim Biophys Acta. 2010;12(1803):1359–67.
Bijlsma MF, Groot AP, Oduro JP, et al. Hypoxia induces a hedgehog response mediated by HIF-1alpha. J Cell Mol Med. 2009;8B(13):2053–60.
Sims-Mourtada J, Yang D, Tworowska I, et al. Detection of canonical hedgehog signaling in breast cancer by 131-iodine-labeled derivatives of the sonic hedgehog protein. J Biomed Biotechnol. 2012; 2012: 639562.
Porter JA, Young KE, Beachy PA. Cholesterol modification of hedgehog signaling proteins in animal development. Science. 1996;5285(274):255–9.
Chen Y, Struhl G. Dual roles for patched in sequestering and transducing Hedgehog. Cell. 1996;3(87):553–63.
Stone DM, Hynes M, Armanini M, et al. The tumour-suppressor gene patched encodes a candidate receptor for Sonic hedgehog. Nature. 1996;6605(384):129–34.
Li X, Ma Q, Duan W, et al. Paracrine sonic hedgehog signaling derived from tumor epithelial cells: a key regulator in the pancreatic tumor microenvironment. Crit Rev Eukaryot Gene Expr. 2012;2(22):97–108.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jianjun Lei and Lin Fan made equal contributions to the study and should be considered co-first authors.
Rights and permissions
About this article
Cite this article
Lei, J., Fan, L., Wei, G. et al. Gli-1 is crucial for hypoxia-induced epithelial-mesenchymal transition and invasion of breast cancer. Tumor Biol. 36, 3119–3126 (2015). https://doi.org/10.1007/s13277-014-2948-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-2948-z