Abstract
Medicinal plant extracts have been widely used for cancer treatment. Nitidine chloride (NC) is a natural bioactive alkaloid that has recently been reported to have diverse anticancer properties. We aimed to investigate the cytotoxic effects of NC and the effectiveness of combinatorial treatment including NC and doxorubicin in breast cancer cells. Using MTT and flowcytometry assays, we found that NC induced cell growth inhibition and G2/M cell cycle arrest in a time- and dose-dependent manner both in MCF-7 and MDA-MB-231 breast cancer cell lines. Cancer cell growth inhibition was associated with increased levels of the p53 and p21 proteins. Apoptosis induction by NC treatment was confirmed by JC-1 mitochondrial membrane potential, annexin V-positive cell, and TUNEL staining. Using western blot analysis, we found that NC upregulated the pro-apoptotic proteins Bax, cleaved caspase-9 and -3 and cleaved PARP and that it downregulated the anti-apoptotic proteins Bcl-2 and PARP. By using the PI3K/Akt inhibitor LY294002, we further demonstrated that NC-induced apoptosis might be Akt-specific or dependent. In addition, NC exhibited a synergistic effect with doxorubicin on the growth inhibition of the human breast cancer cell lines MCF-7 and MDA-MB-231. Our study demonstrated the anticancer effect of NC on breast cancer and highlighted the potential clinical application of NC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As one of the most common cancers among females around the world, in recent years, breast cancer has been the major cause of cancer-related deaths [1, 2]. In the western world, the 10-year relative survival rate for early breast cancer has improved to 83 %, and its 5-year relative survival rate has increased to 98 % [3]. Despite significant progress in early diagnosis and treatment, the therapeutic options for advanced-stage breast cancer are still fairly limited [4]. The current clinical treatments for breast cancer include surgical operation, chemotherapy, and radiotherapy [5]. However, at present, the drawback to chemotherapy for breast cancer is drug resistance or developing resistance after exposure to chemotherapeutic drugs [6]. Indeed, chemotherapeutic drugs often complicate cancer treatment because the therapeutic dosages must be limited to ensure the patients’ quality of life. Therefore, there is a great need for novel agents and new combination regimens for breast cancer patients to improve their quality of life and prognosis.
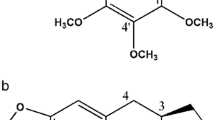
Nitidine was first derived from the root of Zanthoxylum nitidum, which is a natural phytochemical alkaloid. Nitidine chloride (NC) is a chloride of nitidine. It has been found that NC exhibits several types of biological activities, including anti-inflammatory [6], antimalarial [7], antifungal [8], anti-angiogenesis [9], and anticancer activity [10]. It has been reported that NC can inhibit the proliferation of hepatocellular carcinoma and renal cancer [11, 12] and the metastasis of breast cancer through suppressing the c-Src/focal adhesion kinase (FAK)-associated signaling pathway [13]. Studies have reported that NC has anticancer characters; however, it still remains unknown whether NC has any effect on breast cancer apoptosis. Although NC monotherapy appears to be successful for cancer, the efficacy of combined chemotherapy with other therapeutic drugs is still unknown. The present study aimed to investigate the anticancer effects of NC and to evaluate the chemopreventive potential of NC concurrent with doxorubicin on the human breast cancer cell lines MCF-7 and MDA-MB-231.
Materials and methods
Cell lines and reagents
The human MCF-7 and MBA-MD-231 cell lines were obtained from American Type Culture Collection (ATCC) and were routinely cultured in DMEM medium (Gibco-BRL, Rockville, IN, USA) containing 10 % FBS, 100 U/ml penicillin, and 100 μg/ml streptomycin in 5 % CO2 at 37 °C. An annexin V-FITC/PI assay kit was purchased from Sigma (St. Louis, MO, USA). A TUNEL kit, JC-1 assay kit, and caspase peptide inhibitor (Z-VAD-FMK) were purchased from Beyotime Institute of Biotechnology (Shanghai, China). Monoclonal antibodies against β-actin (#3700), Bax (#2772), caspase-3 (#9668) and caspase-9 (#7237), PARP (#9532), p53 (#9919), p21 (#2946), phospho-Akt (#4060, ser473), and Akt (#2920) were purchased from Cell Signaling Technology (Beverly, MA, USA). Anti-Bcl-2 (M0887) was purchased from Dako Corp (Carpinteria, CA, USA). AnticyclinB1 (YT1169) was obtained from Immuno-way (Newark, DE, USA). The secondary horseradish peroxidase (HRP)-linked antibodies were obtained from Tiangen Biotech CO., LTD (Beijing, China).
Nitidine chloride was purchased from Tauto Biotech (Shanghai, China) and dissolved in dimethyl sulfoxide (DMSO). DMSO was also applied to the controls.
MTT assay of cell viability
MCF-7 (3 × 103 cells/well) and MDA-MB-231 (2 × 103cells/well) cells were seeded into 96-well culture plates and incubated in 5 % CO2 at 37 °C. After incubation overnight, the cells were exposed to different concentrations of nitidine chloride and incubated for 24, 48, or 72 h. After treatment, 20 μL of 5 mg/ml MTT was added and incubated in the dark for 4 h at 37 °C. After removal of MTT, 100 μL of DMSO was added to each well, and the plate was gently shaken for 10 min at room temperature. The absorbance was measured at 490 nm by the Microplate Reader (Bio-Rad, Hercules, CA, USA). All experiments were repeated at least three times.
Colony formation assay
MCF-7 and MDA-MB-231 cells in single-cell suspension (500 cells per well) were seeded in six-well plates and incubated for 24 h. The cells were treated with different concentrations of NC for 24 h. Then, the medium was replaced with 4 ml of fresh medium, and the cells were cultured for another 14 days. The media were refreshed every 5 days. The cells were fixed with paraformaldehyde for 15 min and stained with 2 % crystal violet for 20 min. The colonies consisting of more than 50 cells were counted directly on the plate. Photos were taken using an Olympus digital camera (Olympus, Tokyo, Japan). The relative staining intensities were quantified using ImageJ software.
Identification of apoptosis by PI-annexin V staining
MCF-7 and MDA-MB-231 cells were cultured in a six-well plate for 24 h prior to treatment. The cells were treated with different concentrations of NC, ranging from 0 to 10 μM, for 24 h. Then, the cells were stained with 5 μL annexin V-FITC and 10 μl propidium iodide (PI) (20 μg/ml) and incubated for 15 min in the dark at room temperature. After incubation, 400 μl of binding buffer was added to each reaction tube. The apoptotic cell percentages were determined using a FACScan flow cytometer, and the data were analyzed using WinMDIV2.9 software (The Scripps Research Institute, San Diego, CA, USA).
Cell cycle analysis by flow cytometry
The cell cycle distribution of the cells was analyzed using a flow cytometer. A density of 2.5 × 105 cells/well was seeded into a 6-cm Petri dish and incubated for 24 h. The cells were then treated with NC for 24 h. After incubation, the total cells were collected by centrifugation at 800 g for 5 min and washed with phosphate-buffered saline (PBS). The cells were fixed in 4 ml of cold 70 % ethanol at 4 °C overnight. Then, the cells were stained with RNase A (1 mg/ml) and propidium iodine (PI, 100 μl/ml) and analyzed using the flow cytometer (Becton Dickinson, Franklin Lakes, NJ, USA). The data were analyzed by ModFitLT V2.0 software (Becton Dickinson).
Terminal deoxynucleotidyl transferased UTP nick end labeling assays
The terminal deoxynucleotidyl transferased UTP nick end-labeling (TUNEL) method was performed to label the 3′-OH ends of the fragmented DNA of apoptotic cells using a TUNEL Apoptosis Detection kit. Briefly, cells were incubated with NC (0, 5, and 10 μM) for 24 h. After incubation, the cells were fixed with 4 % paraformaldehyde and steeped with 0.1 % Triton X-100 for 10 min at 4 °C. The cells were further stained by the TUNEL mixture for 1 h and then stained with 4,6-diamidino-2-phenylindole (DAPI) for 10 min. The TUNEL-positive cells were evaluated qualitatively by fluorescence microscopy (Olympus, Tokyo, Japan). TUNEL-positive (red staining) cells were characterized as apoptotic cells and were assessed by the random selection of five fields of view per cells.
Measurement of the mitochondrial membrane potential (ΔΨm)
Mitochondrial stability was assessed using a mitochondrial membrane potential assay kit with JC-1(5,5′,6′,6-tetrachloro-1,1′,3,3′-tetraethylbenzimidazolcarbocyanine iodide). MCF-7 and MDA-MB-231 cells were cultured in 12-well plates and treated with 5 and 10 μM NC. After 24-h treatment, the cells were incubated with 1 ml JC-1 fluorescent dye for 30 min in the dark at 37 °C. Then, the cells were washed slowly twice with JC-1 dyeing buffer. The mitochondrial membrane potential was imaged using fluorescence microscopy (Olympus, Tokyo, Japan) at 550 nm excitation and 570 nm emission.
Western blot analysis
The cells were washed twice with phosphate-buffered saline (PBS) and lysed with lysis buffer on ice. The protein concentrations of the cell lysates were determined using a BCA protein concentration kit. Fifty micrograms of proteins were resolved on SDS-PAGE gels and then transferred to a PVDF membrane (Millipore, Bedford, MA, USA). After blocking with 5 % nonfat milk at room temperature, the membrane was incubated overnight at 4 °C with the primary antibody. After washing with TBST, the membrane was labeled with secondary antibody for 2 h, and the proteins were detected by a chemiluminescence system (ECL kit).
The synergy of doxorubicin and NC with CDI evaluation
To investigate whether NC has a synergistic effect with doxorubicin on the growth inhibition of the human breast cancer cell lines MCF-7 and MDA-MB-231, the inhibitory effects of the drugs were measured by a cytotoxicity test. The coefficient of drug interaction (CDI) was used to analyze the synergistic inhibitory effect of drug combination [14]. The CDI was calculated using the formula CDI=AB/(A×B), where AB is the ratio of the drug combination group to the control group at an absorbance of 490 nm, and A and B are the ratios of the single treatment groups to the control group at an absorbance of 490 nm. CDI values of <1 indicate that the drugs are synergistic, CDI = 1 or >1 indicate additive or antagonistic effects, respectively. CDI <0.7 indicates that the drugs are significantly synergistic.
Statistical analysis
The data are expressed as the mean±SD. The SPSS version 18.0 software was used for statistical analysis, and Student’s t test was used to analyze all other data. The IC50 was calculated using probit regression analysis. All error bars represent the S.E. of three experiments. P < 0.05was considered statistically significance.
Results
NC inhibited breast cancer cell proliferation
The antiproliferative effect of NC on both breast cancer cell lines was investigated using MTT and colony formation assays. As shown in Fig. 1a, b, NC inhibited the proliferation of both breast cancer cells in a time- and dose-dependent manner. In addition, the IC50 of NC against MCF-7 and MDA-MB-231 cells were approximately 7.47 and 6.79 μM at 24 h; thus, in the following experiments, the concentration of NC ranged from 5 to 10 μM. The colony formation ability of the MCF-7 and MDA-MB-231 cells was analyzed using colony formation assays. As shown in Fig. 1c, d, a significant inhibitory effect was observed with ascending concentrations of NC. The MDA-MB-231 cells were shown to be more sensitive to NC-inhibited colony formation than MCF-7 cells. These results were consistent with those from the MTT assay.
The effect of the indicated concentrations of NC on breast cancer cell viability and colony-forming capacity were measured using MTT-based and clonogenic survival assays. MCF-7 (a) and MDA-MB-231 cells (b) were cultured in 96-well plates and treated with NC for 24, 48, and 72 h. c Representative images of MCF-7 and MDA-MB-231 cell colonies after treatment with NC for 24 h. d The colony formation rate of breast cancer cells after treatment with NC for 24 h. *P < 0.05 or # P < 0.01 compared with the control. The data are presented as the mean±SD of three separate experiments
NC-induced breast cancer cell apoptosis tested by PI-annexin V and TUNEL assays
To determine whether this reduced cell viability was due to apoptosis, PI-annexin V double staining was used. As shown in Fig. 2a, MCF-7 cells treated with various concentrations of NC showed increased percentages of apoptotic cells of 9.41, 20.65, and 25.5 %, respectively, at 24 h (Fig. 2b). Similar results could be observed in MDA-MB-231 cells, where the apoptotic ratio increases were 9.42, 13.32, and 22.3 % at 24 h, respectively (Fig. 2b). TUNEL is used to evaluate the fragmented DNA of the apoptotic cells. After NC treatment for 24 h, the cells were stained with DAPI and TUNEL and analyzed by fluorescence microscopy. Blue staining represented the nucleus, and red staining represented apoptotic cells (Fig. 3a, b). These data showed that NC could induce apoptosis in both cell lines in a dose-dependent manner, especially during early apoptosis.
The MCF-7 and MDA-MB-231 cell lines were treated with NC at 5 and 10 μM for 24 h and then double-stained with PI and annexin V. a The cells were analyzed using a flow cytometer. b The distributions of early and late apoptosis cells are shown on the lower right (LR) and upper right (UR) quadrants, respectively, of the histograms. Z-VAD-FMK was added to the culture medium 1 h before treatment with 10 μM NC for 24 h. The data represent the results of three independent experiments;*P < 0.05 or **P < 0.01. c Induction of G2/M phase arrest in MCF-7 and MDA-MB-231 cell lines by NC. The DNA content of cells treated as above for 24 h was detected and analyzed by flow cytometry (d). The data are presented as the mean±SD of three separate experiments
Breast cancer cells were treated with 0, 5, or 10 μM NC for 24 h and then stained with DAPI and TUNEL.Z-VAD-FMK was then added to the culture medium 1 h before treatment with 10 μM NC for 24 h, and the labeled 3′-OH ends of the fragmented DNA of the apoptotic cells were viewed under a fluorescence microscope (arrows apoptotic cells, 200×). *P < 0.05 or **P < 0.01. The data are presented the mean±SD of three separate experiments
NC-induced G2/M cell cycle arrest
The effects of NC on cell cycle progression in MCF-7 and MDA-MB-231 cells were investigated by flow cytometry. Cells incubated with different concentrations (0, 5, and 10 μM) of NC for 24 h were examined with a flow cytometer. Compared with the control, NC treatment resulted in a significant accumulation of cells in G2/M phase, accompanied by a decrease in S-phase cells (Fig. 2c). In MCF-7 cells, the percentage of cells in G2/M phase increased from 4.65 to 66.76 % upon NC treatment (Fig. 2d). Furthermore, MDA-MB-231 cells treated with NC had an increasing percentage of cells in G2/M phase (from 7.11 to 76.36 %) and a decreased percentage of cells in S phase (from 38.18 to 23.64 %; Fig. 2d). These results suggest that NC arrests cell growth at the G2/M phase.
NC-induced mitochondrial membrane depolarization, as shown by a JC-1 assay
The mitochondrion is a central organelle used for the production of cellular energy and has important roles in programmed cell death. JC-1 localizes to the mitochondrial membrane as a monomer or dimer depending on the mitochondrial membrane potential [15]. Therefore, we determined whether NC caused disruption or loss of the mitochondrial membrane potential. Cells were treated with NC, harvested 24 h post-treatment, and stained with JC-1 dye. As shown in Fig. 4, fluorescence from red to green was observed in response to NC treatment in a dose-dependent manner, which suggests that NC-caused depolarization of the mitochondrial membrane potential may be a major mechanism for the induction of apoptosis of MCF-7 and MDA-MB-231 cells.
Breast cancer cells were treated with 0, 5, and 10 μM NC for 24 h and then subjected to JC-1 staining to evaluate changes in the mitochondrial membrane potential. The cells were then viewed under a fluorescence microscope (400×). In JC-1 stained cells, red fluorescence was visible in cellular areas with high mitochondrial membrane potential, while green fluorescence of the JC-1 monomer is present in cellular areas with low mitochondrial potential
NC-induced cell cycle arrest through activation of p53 and altering the levels of cell cycle proteins
To elucidate the mechanism underlying the NC-mediated cell cycle arrest in breast cancer cells, various cell cycle regulatory proteins were examined by western blot analysis. The activation of p53 leads to potent tumor suppression and plays an important role in apoptosis signaling [16, 17]. Previous studies have shown that the accumulation of p53 is crucial for tumor development prevention as well as for anticancer therapy [17]. p21 is a target of p53 and acts as a cell cycle inhibitory protein of G2/M phase-related cyclin-dependent kinases [18]. Hence, p53, p21, and cell cycle proteins that regulate cell cycle progression at the G2/M boundary, such as cyclin B1, were detected by western blotting. Our study indicated that the expression of p53 was significantly increased after NC treatment for 24 h (Fig. 5d). To confirm the trans-activation of p53 upon NC treatment, p21expression was examined. As shown in Fig. 5d, p21 was also activated in response to NC, consistent with the p53 activation. The expression levels of cyclin B1 significantly decreased after 24 h of NC treatment (Fig. 5d). In contrast, the β-actin level, an internal control, was not changed.
The effects of NC on the expression of Bax, Bcl-2, cleaved caspase, and PARP. a MCF-7 and b MDA-MB-231 cells were incubated with 5 μM NC for 12, 24, and 48 h. c and d Both cell types were treated with 0, 5, or 10 μM NC for 24 h and then analyzed by Western blotting. e The cyclinB1, p21, and p53proteins were examined after NC treatment for 24 h. The results are representative of three independent experiments
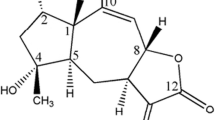
NC-induced apoptosis through alterations in the levels of Bcl-2 family proteins and activation of caspase
To further investigate the mechanism involved in NC-mediated apoptosis, we measured the expression of Bcl-2 family members. The Bcl-2 family proteins consist of both the pro-apoptotic Bax and anti-apoptotic Bcl-2 proteins that regulate the mitochondrial membrane potential and caspase activation [19]. Activation of caspase-3 leads to cleavage of several substrates, including PARP [20, 21]. As shown in Fig. 5a, b, NC treatment significantly increased the expression of the pro-apoptotic protein Bax and downregulated the expression of the anti-apoptotic protein Bcl-2 in both cell lines. On the other hand, the expression of cleaved caspase-9 and caspase-3 was upregulated (Fig. 5a–c). In accordance with the caspase-3 results, increasing PARP cleavage was detected in both cell lines. These results suggest that NC increases the expression of Bax, cleaved caspase-3, and cleaved PARP and decreases Bcl-2 expression in breast cancer cells in time- and dose-dependent manners, respectively.
To confirm caspase activation during NC-induced apoptosis, we also investigated the effect of a pan-caspase inhibitor, Z-VAD-FMK, on the induction of apoptosis. As shown in Figs. 2b and 3a, b, treatment with 40 μM Z-VAD-FMK for 24 h markedly inhibited NC-induced apoptosis in MCF-7 and MDA-MB-231 cells, suggesting that caspase activity is required for NC-induced apoptosis in both breast cancer cell lines.
NC-inhibited Akt phosphorylation
Akt is an important pathway associated with tumor development. The inhibition of either the MAPK pathway or Akt activation has been shown to induce apoptosis in tumor cells [22]. To further elucidate the potential mechanisms of NC on apoptosis, we investigated the effect of NC on Akt activation. Akt phosphorylation decreased after NC treatment for 24 h in a dose-dependent manner, indicating that Akt may be involved in the apoptosis pathway (Fig. 6a). To confirm whether NC is PI3K/Akt-dependent, we inhibited Akt phosphorylation using the PI3K inhibitor LY294002 [23]. As shown in Fig. 6c, d, the PI3K inhibitor could decrease the viability of cells compared with the control. To further investigate the activation of the apoptotic pathway, we examined the expression of apoptosis-related proteins in both cell lines. As shown in Fig. 6b, inhibition of AKT activity with LY294002 could upregulate Bax, cleaved caspase-3, and cleaved PARP expression and downregulate Bcl-2 expression induced by NC. This demonstrated that NC-induced apoptosis might be Akt-specific or Akt-dependent.
The anti-apoptotic effect of NC is Akt-dependent. a Treatment of both cell lines with NC (0, 5, or 10 μM) for 24 h resulted in a significant decrease in phosphorylated Akt in a dose-dependent manner. MCF-7 and MDA-MB-231 cells were pretreated with the Akt inhibitor LY294002 (50 μM) for 30 min followed by incubation with or without NC for24 h. MCF-7 (b) and MDA-MB-231 (c) cell proliferation was analyzed using the MTT assay. d The expression of p-Akt, Akt, Bax, Bcl-2, cleaved caspase, and PARP was analyzed by western blot. The results are representative of three independent experiments
NC demonstrated a synergistic effect with doxorubicin in breast cancer cells
Recently, synergistic cell killing to overcome drug resistance is a frequent goal of clinically used drug combinations [24]. New anticancer drugs are commonly combined with traditional chemotherapeutic agents to achieve better clinical effects. To clearly define the synergistic inhibitory effect of combined treatment with doxorubicin and NC in breast cancer MCF-7 and MDA-MB-231 cells, cells were treated with increasing concentrations of doxorubicin and NC (1 μM) for 48 and 72 h, respectively, and then submitted to MTT assays. The graph clearly demonstrates that doxorubicin alone or in combination with NC (1 μM) suppressed the survival of both breast cancer cell lines in dose- and time-dependent manners. Specifically, in MCF-7 cells, after treatment with an increasing dose of only doxorubicin for 48 h, the survival rate decreased from 79.2 % (0.2 μM) to 22.1 % (2 μM) (Fig. 7a). For MDA-MB-231 cells, the survival rate decreased from 96.7 % (0.2 μM) to 44.4 % (4 μM) at 48 h (Fig. 7d). Notably, the combined treatment resulted in a decrease in the survival rate of MCF-7 cells from 32.3 % (0.2 μM) to 22.1 % (2 μM) at 72 h (Fig. 7b) and in MDA-MB-231 cells from 62.5 % (0.2 μM) to 22.3 % (4 μM) at 72 h (Fig. 7e). These results suggested that the combined treatment of NC and doxorubicin had inhibitory effects on the proliferation of the human breast cancer cell lines. NC enhanced cytotoxicity in MCF-7 and MDA-MB-231 cells with statistical significance when using the coefficient of drug interaction (CDI). As shown in Fig. 7c, f, the most prominent synergistic effect was a CDI of 0.58 after exposure of MCF-7 cells to 0.2 μM doxorubicin combined with NC for 72 h, while the most prominent synergistic effect appeared after exposure of MDA-MB-231 cells to higher concentrations of doxorubicin (2 μM). This study demonstrates that the combination of NC and doxorubicin has a synergistic inhibitory effect on the proliferation and enhances the anticancer effects of human breast cancer cell lines.
The synergistic effect of NC and doxorubicin on the cytotoxicity of breast cancer cells. The cell survival rate of doxorubicin alone (0.2–0.4 μM) or in combination with NC (1 μM) after exposure for 48 h or72 h. MCF-7 (a and b) and MDA-MB-231 (d and e) cell proliferation was analyzed using the MTT assay. CDI (coefficient of drug interaction) values for the combination treatment of doxorubicin with NC (1 μM) on the MCF-7 and MDA-MB-231 cell lines (c and f), where CDI <1 or <0.7 indicate synergistic or significantly synergistic effects, respectively. The data are presented as the mean±SD of three separate experiments
Discussion
Phytochemicals, including terpenoids, flavonoids, isothiocyanates, and alkaloids, are extracted from traditional herbs. Recently, increasing attention has been focused on the therapeutic activities of natural products in cancer therapy [25–28]. NC is a type of natural, bioactive phytochemical alkaloid that has been reported to possess a wide range of pharmacological properties [6–13]. In previous study, Fang et al. proved that NC could induce cell apoptosis of renal cancer cells via the ERK-associated signaling pathway, accompanied by upregulation of Bax and downregulation of Bcl-2 [11]. NC has also been found to modulate cell migration and invasion in breast cancer cells through the c-scr-fak signaling pathway [13]. Therefore, it is one of the most promising chemopreventive agents for several types of cancer. However, it is unknown whether NC has any effect on breast cancer cell apoptosis. We show for the first time that NC can induce cell apoptosis and inhibit cell proliferation in a dose- and time-dependent manner in breast cancer cells. In addition, it caused cell G2/M phase arrest through the suppression of the expression of cyclin B1- and p53-dependent pathway. Furthermore, NC inhibited the expression of anti-apoptotic proteins (Bcl-2) and activated pro-apoptotic proteins (Bax). It further activated caspase-9 which subsequently induced caspase-3 activation, resulting in PARP cleavage. Crucially, NC blocked Akt phosphorylation in both MCF-7 and MDA-MB-231 cells. It was also identified that the inhibition of caspase by the pan-caspase inhibitor, z-VAD-fmk, blocked NC-induced apoptosis in both cells. What is more, synergism was observed when NC was combined with doxorubicin. However, for the normal mammary epithelial cells MCF-10A, there was no obvious cytotoxicity observed after NC incubation (data not shown).
To explore the underlying mechanism of apoptosis in breast cancer cells, the proteins of the Bcl-2 family were examined [29]. The relative balance of various pro-apoptotic (Bax, Bad) and anti-apoptotic (Bcl-2, Bcl-xL, Bcl-w, and Mcl-1) Bcl-2 family members is a critical determinant of cellular homeostasis [30, 31]. The anti-apoptotic Bcl-2 proteins interfere with engagement of the mitochondrial apoptotic machinery by inhibiting the oligomerization of Bax and Bak [32]. Bax is translocated into mitochondria upon the induction of apoptosis. After translocation, Bax forms large oligomers, which insert into mitochondrial membranes, leading to cytochrome c release and cytotoxic activities [33, 34]. The collapse of the MMP can initiate the release of molecules from the space between the outer and inner mitochondrial membranes into the cytosol, which triggers the caspase cascade and other apoptotic processes [35]. Our results showed that NC treatment increased the Bax/Bcl-2 ratio and collapsed the MMP in MCF-7 and MDA-MB-231 cells. The results also showed the activation of caspase-9 and caspase-3 followed by PARP cleavage. Furthermore, Z-VAD-FMK blocked NC-induced apoptotic cells, as demonstrated by the PI-annexin V and TUNEL staining assays. These results indicated that NC treatment might induce apoptosis via activating the intrinsic, mitochondria-mediated caspase pathway. Recent studies have demonstrated that the p53 protein can promote cytochrome C release and stimulate Bax oligomerization [36].
Cell cycle regulation is also a main mechanism of cell growth, and many drugs can trigger apoptosis in cancer cells when accompanied by cell cycle arrest [37, 38]. p21 is known as a cell cycle inhibitor involved in G1 or G2/M phase progression, and its upregulation has been linked to cell cycle arrest. Recent studies have demonstrated that p53 acts upstream of p21 and proteins of the Bcl-2 family and is a very important tumor suppressor gene [39]. CyclinB1 is also important for cell cycle arrest at the G2/M phase through the formation of a cyclin-CDK complex to promote cell cycle progression [40]. Our western blot results showed that NC treatment could activate p53, upregulate the expression of p21, and downregulate the expression of cyclinB1in both breast cancer cell lines.
The Akt signaling pathway is one of the key signal transduction pathways involved in the apoptosis of cancer cells. Akt activation serves as a prosurvival signal, which inhibits cell apoptosis and promotes cell survival [41]. A recent report indicated that PI3K/Akt could suppress the proapoptotic activity of Bax by retaining Bax in the cytosol. Previous studies have shown that Akt activation can promote cell survival and inhibit cell apoptosis via the mitochondrial pathway [42]. To confirm the effect of NC on Akt, we blocked AKT phosphorylation in both cell lines using the PI3K/Akt inhibitor LY294002, which enhanced NC-induced apoptosis, as indicated by MTT assays and western blot analysis. The results from this study demonstrate the effect of NC in inhibiting the phosphorylation of Akt, implying the suppression of cell survival signals in both MCF-7 and MDA-MB-231 cells.
Combination therapy has been a regular treatment [43] because it is a valid approach to decrease the resistance of cancer cells to treatment. As the most commonly used anthracycline antibiotic for the treatment of cancers, doxorubicin exerts its effects by intercalating between the base pairs of DNA, thereby inhibiting DNA synthesis and eventually leading to cell death. However, the problems of side effects, such as nausea, vomiting, neutropenia, and cardiotoxicity, still exist. Thereby, it is rational to develop combination regimens to minimize chemotherapy-related morbidity. In our study, a synergistic effect was observed when NC combined with doxorubicin was applied to breast cancer cells. It is worth noting that the synergistic effect was more obvious at low concentrations of doxorubicin in MCF-7 cells. This result suggests that the combination of NC and doxorubicin at certain concentrations may reduce painful side effects. However, the potential mechanisms by which NC improves chemotherapeutic efficacy remain unclear. It is therefore worthwhile to further verify the mechanisms of this synergism to evaluate the reasonable applications of NC in human breast cancer treatment.
Conclusion
We demonstrated that NC exerts anticancer effects in both estrogen receptor (ER)-positive and ER-negative breast cancer cells. This effect is mediated through the induction of G2/M phase cycle arrest and triggering apoptosis. NC-induced apoptosis through the upregulation of pro-apoptotic proteins and downregulation of anti-apoptic proteins. In addition, NC-induced apoptosis is likely to act through the intrinsic, mitochondrial-dependent caspase pathway. Furthermore, NC exhibited a synergistic effect with doxorubicin on the growth inhibition of the human breast cancer cell lines MCF-7 and MDA-MB-231. Our study suggests that NC is a promising drug for breast cancer treatment, but further study is necessary to explore its roles for clinical application.
References
Yedjou C, Izevbigie E, Tchounwou P. Preclinical assessment of Vernonia amygdalina leaf extracts as DNA damaging anti-cancer agent in the management of breast cancer. Int J Environ Res Publ Health. 2008;5:337–41.
Ligresti G, Libra M, Militello L, Clementi S, Donia M, Imbesi R, et al. Breast cancer: molecular basis and therapeutic strategies (review). Mol Med Rep. 2008;1:451–8.
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA: Cancer J Clin. 2010;60:277–300.
Allinen M, Beroukhim R, Cai L, Brennan C, Lahti-Domenici J, Huang H, et al. Molecular characterization of the tumor microenvironment in breast cancer. Cancer Cell. 2004;6:17–32.
Pu CY, Lan VM, Lan CF, Lang HC. The determinants of traditional Chinese medicine and acupuncture utilization for cancer patients with simultaneous conventional treatment. Eur J Cancer Care. 2008;17:340–9.
Wang Z, Jiang W, Zhang Z, Qian M, Du B. Nitidine chloride inhibits LPS-induced inflammatory cytokines production via MAPK and NF-kappab pathway in raw 264.7 cells. J Ethnopharmacol. 2012;144:145–50.
Bouquet J, Rivaud M, Chevalley S, Deharo E, Jullian V, Valentin A. Biological activities of nitidine, a potential anti-malarial lead compound. Malar J. 2012;11:67.
Del Poeta M, Chen SF, Von Hoff D, Dykstra CC, Wani MC, Manikumar G, et al. Comparison of in vitro activities of camptothecin and nitidine derivatives against fungal and cancer cells. Antimicrob Agents Chemother. 1999;43:2862–8.
Chen J, Wang J, Lin L, He L, Wu Y, Zhang L, et al. Inhibition of stat3 signaling pathway by nitidine chloride suppressed the angiogenesis and growth of human gastric cancer. Mol Cancer Ther. 2012;11:277–87.
Fang Z, Tang Y, Jiao W, Xing Z, Guo Z, Wang W, et al. Nitidine chloride inhibits renal cancer cell metastasis via suppressing akt signaling pathway. Food Chem Toxicol: int J Publ Br Ind Biol Res Assoc. 2013;60:246–51.
Fang Z, Tang Y, Jiao W, Xing Z, Guo Z, Wang W, et al. Nitidine chloride induces apoptosis and inhibits tumor cell proliferation via suppressing erk signaling pathway in renal cancer. Food Chem Toxicol: Int J Publ Br Ind Biol Res Assoc. 2014;66:210–6.
Liao J, Xu T, Zheng JX, Lin JM, Cai QY, Yu DB, et al. Nitidine chloride inhibits hepatocellular carcinoma cell growth in vivo through the suppression of the jak1/stat3 signaling pathway. Int J Mol Med. 2013;32:79–84.
Pan X, Han H, Wang L, Yang L, Li R, Li Z, et al. Nitidine chloride inhibits breast cancer cells migration and invasion by suppressing c-src/fak associated signaling pathway. Cancer Lett. 2011;313:181–91.
Hao JQ, Li Q, Xu SP, Shen YX, Sun GY. Effect of lumiracoxib on proliferation and apoptosis of human nonsmall cell lung cancer cells in vitro. Chin Med J. 2008;121:602–7.
Cossarizza A, Baccarani-Contri M, Kalashnikova G, Franceschi C. A new method for the cytofluorimetric analysis of mitochondrial membrane potential using the j-aggregate forming lipophilic cation 5,5′,6,6′-tetrachloro-1,1′,3,3′-tetraethylbenzimidazolcarbocyanine iodide (JC-1). Biochem Biophys Res Commun. 1993;197:40–5.
Levine AJ, Hu W, Feng Z. The p53 pathway: what questions remain to be explored? Cell Death Differ. 2006;13:1027–36.
Dulic V, Kaufmann WK, Wilson SJ, Tlsty TD, Lees E, Harper JW, et al. P53-dependent inhibition of cyclin-dependent kinase activities in human fibroblasts during radiation-induced g1 arrest. Cell. 1994;76:1013–23.
Anttila MA, Kosma VM, Hongxiu J, Puolakka J, Juhola M, Saarikoski S, et al. P21/waf1 expression as related to p53, cell proliferation and prognosis in epithelial ovarian cancer. Br J Cancer. 1999;79:1870–8.
Hennet T, Bertoni G, Richter C, Peterhans E. Expression of bcl-2 protein enhances the survival of mouse fibrosarcoid cells in tumor necrosis factor-mediated cytotoxicity. Cancer Res. 1993;53:1456–60.
Calandria C, Irurzun A, Barco A, Carrasco L. Individual expression of poliovirus 2apro and 3cpro induces activation of caspase-3 and parp cleavage in hela cells. Virus Res. 2004;104:39–49.
Yap E, Tan WL, Ng I, Ng YK. Combinatorial-approached neuroprotection using pan-caspase inhibitor and poly (adp-ribose) polymerase (parp) inhibitor following experimental stroke in rats; is there additional benefit? Brain Res. 2008;1195:130–8.
Sebolt-Leopold JS, English JM. Mechanisms of drug inhibition of signalling molecules. Nature. 2006;441:457–62.
Noshita N, Lewen A, Sugawara T, Chan PH. Evidence of phosphorylation of akt and neuronal survival after transient focal cerebral ischemia in mice. J Cereb Blood Flow Metab: Off J Int Soc Cereb Blood Flow Metab. 2001;21:1442–50.
Stein R, Smith MR, Chen S, Zalath M, Goldenberg DM. Combining milatuzumab with bortezomib, doxorubicin, or dexamethasone improves responses in multiple myeloma cell lines. Clin Cancer Res: Off J Am Assoc Cancer Res. 2009;15:2808–17.
Dorai T, Aggarwal BB. Role of chemopreventive agents in cancer therapy. Cancer Lett. 2004;215:129–40.
Surh YJ. Cancer chemoprevention with dietary phytochemicals. Nat Rev Cancer. 2003;3:768–80.
Tan AC, Konczak I, Sze DM, Ramzan I. Molecular pathways for cancer chemoprevention by dietary phytochemicals. Nutr Cancer. 2011;63:495–505.
Thomasset SC, Berry DP, Garcea G, Marczylo T, Steward WP, Gescher AJ. Dietary polyphenolic phytochemicals—promising cancer chemopreventive agents in humans? A review of their clinical properties. Int J Cancer J Int Cancer. 2007;120:451–8.
Adams JM, Cory S. The bcl-2 protein family: Arbiters of cell survival. Science. 1998;281:1322–6.
Kim R. Unknotting the roles of bcl-2 and bcl-xl in cell death. Biochem Biophys Res Commun. 2005;333:336–43.
Mayorga M, Bahi N, Ballester M, Comella JX, Sanchis D. Bcl-2 is a key factor for cardiac fibroblast resistance to programmed cell death. J Biol Chem. 2004;279:34882–9.
Precht TA, Phelps RA, Linseman DA, Butts BD, Le SS, Laessig TA, et al. The permeability transition pore triggers bax translocation to mitochondria during neuronal apoptosis. Cell Death Differ. 2005;12:255–65.
Eldering E, Mackus WJ, Derks IA, Evers LM, Beuling E, Teeling P, et al. Apoptosis via the b cell antigen receptor requires bax translocation and involves mitochondrial depolarization, cytochrome c release, and caspase-9 activation. Eur J Immunol. 2004;34:1950–60.
Crompton M. Bax, bid and the permeabilization of the mitochondrial outer membrane in apoptosis. Curr Opin Cell Biol. 2000;12:414–9.
Valentijn AJ, Upton JP, Bates N, Gilmore AP. Bax targeting to mitochondria occurs via both tail anchor-dependent and -independent mechanisms. Cell Death Differ. 2008;15:1243–54.
Chipuk JE, Kuwana T, Bouchier-Hayes L, Droin NM, Newmeyer DD, Schuler M, et al. Direct activation of bax by p53 mediates mitochondrial membrane permeabilization and apoptosis. Science. 2004;303:1010–4.
Murray AW. Recycling the cell cycle: cyclins revisited. Cell. 2004;116:221–34.
Abu Bakar MF, Mohamad M, Rahmat A, Burr SA, Fry JR. Cytotoxicity, cell cycle arrest, and apoptosis in breast cancer cell lines exposed to an extract of the seed kernel of Mangifera pajang (bambangan). Food Chem Toxicol: Int J Publ Br Ind Biol Res Assoc. 2010;48:1688–97.
Hall M, Peters G. Genetic alterations of cyclins, cyclin-dependent kinases, and cdk inhibitors in human cancer. Adv Cancer Res. 1996;68:67–108.
O'Connell MJ, Walworth NC, Carr AM. The g2-phase DNA-damage checkpoint. Trends Cell Biol. 2000;10:296–303.
Gardai SJ, Hildeman DA, Frankel SK, Whitlock BB, Frasch SC, Borregaard N, et al. Phosphorylation of bax ser184 by akt regulates its activity and apoptosis in neutrophils. J Biol Chem. 2004;279:21085–95.
Schulze-Bergkamen H, Brenner D, Krueger A, Suess D, Fas SC, Frey CR, et al. Hepatocyte growth factor induces mcl-1 in primary human hepatocytes and inhibits cd95-mediated apoptosis via akt. Hepatology. 2004;39:645–54.
Khan KH, Blanco-Codesido M, Molife LR. Cancer therapeutics: targeting the apoptotic pathway. Crit Rev Oncol Hematol. 2013;90(3):200–19.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (no. 30772133, no. 81072150, no. 81172529, and no. 81272903) and the Shandong Science and Technology Development Plan (no. 2012GZC22115). Disclosure Statement: None. We thank Cunzhong Yuan and Shi Yan for technical supports with experiments. We also thank Xiangnan Kong and Xiaoyan Li for critical discussing and substantial helps.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sun, M., Zhang, N., Wang, X. et al. Nitidine chloride induces apoptosis, cell cycle arrest, and synergistic cytotoxicity with doxorubicin in breast cancer cells. Tumor Biol. 35, 10201–10212 (2014). https://doi.org/10.1007/s13277-014-2327-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-2327-9