Abstract
The Arg194Trp polymorphism in the X-ray cross-complementing group 1 (XRCC1) had been implicated in cancer susceptibility. The previous published data on the association between XRCC1 Arg194Trp polymorphism and cancer risk remained controversial. Hence, we performed a meta-analysis to investigate the association between cancer susceptibility and XRCC1 Arg194Trp (59,227 cases and 81,587 controls from 201 studies) polymorphism in different inheritance models. We used odds ratios with 95 % confidence intervals to assess the strength of the association. Overall, significantly increased cancer risk was found (recessive model: (odds ration [OR] = 1.18, 95 % confidence interval [CI] = 1.09–1.27; homozygous model: OR = 1.21, 95 % CI = 1.10–1.33; additive model: OR = 1.05, 95 % CI = 1.01–1.09) when all eligible studies were pooled into the meta-analysis. In further stratified and sensitivity analyses, significantly increased glioma risk was found among Asians, significantly decreased lung cancer risk was found among Caucasians, and significant increased breast cancer risk was found among hospital-based studies. In summary, this meta-analysis suggests that Arg194Trp polymorphism may be associated with increased breast cancer risk, Arg194Trp polymorphism is associated with increased glioma risk among Asians, and Arg194Trp polymorphism is associated with decreased lung cancer risk among Caucasians. In addition, our work also points out the importance of new studies for Arg194Trp association in some cancer types, such as gastric, pancreatic, prostate, and nasopharyngeal cancers, where at least some of the covariates responsible for heterogeneity could be controlled, to obtain a more conclusive understanding about the function of the XRCC1 Arg194Trp polymorphism in cancer development (I 2 > 75 %).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
DNA repair systems play critical roles in protecting against mutations and are essential for maintaining the integrity of the genome. Certain common genetic polymorphisms within the genes involved in DNA damage responses may contribute to the development of cancer and be associated with an increased risk of the disease. Because reduced DNA repair capacity may lead to genetic instability and carcinogenesis, genes involved in DNA repair have been proposed as candidate cancer susceptibility genes [1]. Until now, more than a hundred proteins implicated in DNA repair have been found in human cells. These proteins are implicated in four major DNA repair pathways, including nucleotide excision repair (NER), base excision repair (BER), double-strand break repair (DSBR), and mismatch repair (MMR) [1,2].
The X-ray cross-complementing (XRCC) genes were initially discovered through their role in DNA damage response caused by ionizing radiation. They are important components of various DNA repair pathways contributing to DNA-damage processing and genetic stability [3]. The DNA repair enzymes XRCC1 play a central role in the BER pathway [4,5]. XRCC1 is located on chromosome no. 19q13.2–13.3, and its gene product is implicated in single-strand break repair and base excision repair mechanisms [6]. Although there are more than 300 validated single nucleotide polymorphisms (SNPs) in the XRCC1 gene reported in the dbSNP database (http://www.ncbi.nlm.nih.gov/SNP/), three of which are common [7] and lead to amino acid substitutions in XRCC1 at codon 194 (exon 6, base C to T, amino acid Arg to Trp, dbSNP no. rs1799782), codon 280 (exon 9, base G to A, amino acid Arg to His, dbSNP no. rs25489), and codon 399 (exon 10, base G to A, amino acid Arg to Gln, dbSNP no.rs25487), these non-conservative amino acid changes may alter XRCC1 function. This change in protein biochemistry leads to the supposition that variant alleles may diminish repair kinetics, thereby influencing susceptibility to adverse health effects, including cancer.
In the past decade, a number of molecular epidemiological studies have been done to evaluate the association between XRCC1 Arg194Trp polymorphism and different types of cancer risk in diverse populations [8–202]. The tumor types included breast cancer [8–34,170], lung cancer [35–51,53,54,163,178,189,190], head and neck cancer [68–77,79–83,117,119,122,123,125,128,137,146,157,165,172–174,191–194], esophageal cancer [101–106,141], and prostate cancer [96–100,126,166,175], and so on. However, the results were inconsistent or even contradictory. Partially because of the possible small effect of the polymorphism on cancer risk and the relatively small sample size in each of published studies. In addition, some recent meta-analyses analyzed such an association only for single cancer such as lung cancer, glioma, and leukemia, and so on [203–205]. Therefore, we performed a comprehensive meta-analysis by including the most recent and relevant articles to identify statistical evidence of the association between XRCC1 Arg194Trp polymorphism and risk of all cancers that have been investigated.
Materials and methods
Identification and eligibility of relevant studies
A comprehensive literature search was performed using the PubMed and ISI database for relevant articles published (the last search update was February 24, 2014) with the following key words “XRCC1,” “polymorphism,” “Variant,” or “Mutation,” and “Cancer” or “Carcinoma.” MESH terms: XRCC1 [All Fields] and ((“polymorphism, genetic” [MeSH Terms] OR (“polymorphism” [All Fields] AND “genetic” [All Fields]) or “genetic polymorphism” [All Fields] or “polymorphism” [All Fields]) or variant [All Fields] or (“mutation” [MeSH Terms] OR “mutation” [All Fields])) and ((“neoplasms” [MeSH Terms] or “neoplasms” [All Fields] or “cancer” [All Fields]) or (“carcinoma” [MeSH Terms] or “carcinoma” [All Fields])). The search was not limited to language. Additional studies were identified by hand searching references in original articles and review articles. Authors were contacted directly regarding crucial data not reported in original articles. In addition, studies were identified by a manual search of the reference lists of reviews and retrieved studies. We included all the case–control studies and cohort studies that investigated the association between XRCC1 Arg194Trp polymorphism and cancer risk with genotyping data. All eligible studies were retrieved, and their bibliographies were checked for other relevant publications. When the same sample was used in several publications, only the most complete information was included following careful examination.
Inclusion criteria
The included studies needed to have met the following criteria: (1) only the case–control studies or cohort studies were considered, (2) evaluated the XRCC1 Arg194Trp polymorphism and the risk of cancer, and (3) the genotype distribution of the polymorphisms in cases and controls were described in details and the results were expressed as odds ratio (OR) and corresponding 95 % confidence interval (95 % CI). Major reasons for exclusion of studies were as follows: (1) not for cancer research, (2) only case population, and (3) duplicate of previous publication (When the same sample was used in several publications, only the most complete information was included following careful examination).
Data extraction
Information was carefully extracted from all eligible studies independently by two investigators according to the inclusion criteria listed above. The following data were collected from each study: first author’s name, year of publication, country of origin, ethnicity, source of controls, sample size, and numbers of cases and controls in the XRCC1 Arg194Trp genotypes whenever possible. Ethnicity was categorized as “Caucasian,” “African,” (including African Americans) and “Asian.” We considered the samples of studies from India and Pakistan as of “Indian’” ethnicity, and samples from Middle Eastern countries as “Middle Eastern” ethnicity. When one study did not state which ethnic groups was included or if it was impossible to separate participants according to phenotype, the sample was termed as “mixed population.” Meanwhile, studies investigating more than one kind of cancer were counted as individual data set only in subgroup analyses by cancer type. We did not define any minimum number of patients to include in this meta-analysis. For articles that reported different ethnic groups and different countries or locations, we considered them different study samples for each category cited above.
Statistical analysis
Crude ORs together with their corresponding 95 % CIs were used to assess the strength of association between the XRCC1 Arg194Trp polymorphism and the risk of cancer. The pooled ORs were performed for co-dominant model (Trp/Trp versus Arg/Arg and Arg/Trp versus Arg/Arg), dominant model (Arg/Trp + Trp/Trp versus Arg/Arg), recessive model (Trp/Trp versus Arg/Arg + Arg/Trp), and additive model (Trp versus Arg), respectively. Between-study heterogeneity was assessed by calculating Q statistic (Heterogeneity was considered statistically significant if P < 0.10) [206] and quantified using the I 2 value, a value that describes the percentage of variation across studies that are due to heterogeneity rather than chance, where I 2 = 0 % indicates no observed heterogeneity, with 25 % regarded as low, 50 % as moderate, and 75 % as high [207]. If results were not heterogeneous, the pooled ORs were calculated by the fixed-effect model (we used the Q statistic, which represents the magnitude of heterogeneity between-studies) [208]. Otherwise, a random-effect model was used (when the heterogeneity between-studies were significant) [209]. In addition to the comparison among all subjects, we also performed stratification analyses by cancer type (if one cancer type contained less than three individual studies, it was combined into the “other cancers” group), source of control, and ethnicity. Moreover, the extent to which the combined risk estimate might be affected by individual studies was assessed by consecutively omitting every study from the meta-analysis (leave-one-out sensitivity analysis). This approach would also capture the effect of the oldest or first positive study (first study effect). In addition, we also ranked studies according to sample size, and then repeated this meta-analysis. Sample size was classified according to a minimum of 200 participants and those with fewer than 200 participants. The cite criteria were previously described [210]. Last, sensitivity analysis was also performed, excluding studies whose allele frequencies in controls exhibited significant deviation from the Hardy–Weinberg equilibrium (HWE), given that the deviation may denote bias. Deviation of HWE may reflect methodological problems such as genotyping errors, population stratification, or selection bias. HWE was calculated by using the goodness-of-fit test, and deviation was considered when P < 0.05. Begg’s funnel plots [211] and Egger’s linear regression test [212] were used to assess publication bias. A meta-regression analysis was carried out to identify the major sources of between-studies variation in the results, using the log of the ORs from each study as dependent variables and cancer type, ethnicity, and source of controls as the possible sources of heterogeneity. All of the calculations were performed using STATA version 10.0 (STATA Corporation, College Station, TX).
Results
Eligible studies and meta-analysis databases
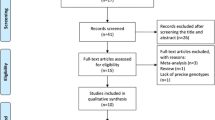
Figure 1 graphically illustrates the trial flow chart. A total of 1,544 articles regarding XRCC1 polymorphisms with respect to cancer were identified. After screening the titles and abstracts, 689 articles were excluded because they were duplicated. In addition, 660 articles were excluded because they were review articles, case reports, and other polymorphisms of XRCC1. Last, of these published articles, six publications [52,63,78,162,170,201] were excluded because their populations overlapped with another six included studies [33,49,65,76,109,126]. As summarized in supplemental Table 1, 189 publications with 201 case–control studies were selected among the meta-analysis, including 59,227 cases and 81,587 controls. Among these studies, eghit studies were included in the dominant model only because they provided the genotypes of Arg/Trp + Trp/Trp versus Arg/Arg. In addition, there were 14 bladder cancer studies, 30 breast cancer studies, 4 cervical cancer studies, 18 colorectal cancer studies, 7 esophageal cancer studies, 10 gastric cancer studies, 11 glioma studies, 32 head and neck cancer studies, 18 leukemia studies, 25 lung cancer studies, 5 lymphoma studies, 3 pancreatic cancer studies, 9 prostate cancer studies, 6 skin cancer studies, and 9 studies with the “other cancers.” All of the cases were pathologically confirmed.
Quantitative synthesis
The evaluations of the association of XRCC1 Arg194Trp polymorphism with cancer risk are shown in Table 1. Overall, significantly increased cancer risk was observed (recessive model: OR = 1.18, 95 % CI = 1.09–1.27, P h = 0.015, I 2 = 19.6 %; homozygous model: OR = 1.21, 95 % CI = 1.10–1.33, P h < 0.001, I 2 = 33.6 %; additive model: OR = 1.05, 95 % CI = 1.01–1.09, P h < 0.001, I 2 = 59.6 %) when all the eligible studies were pooled the meta-analysis. Then, we performed subgroup analysis by cancer type. We found that individuals with the minor variant genotypes had a higher risk of esophageal cancer (recessive model: OR = 1.36, 95 % CI = 1.10–1.70, P h = 0.175, I 2 = 34.8 %; homozygous model: OR = 1.32, 95 % CI = 1.05–1.66, P h = 0.271, I 2 = 21.7 %), glioma (recessive model: OR = 1.77, 95 % CI = 1.41–2.22, P h = 0.805, I 2 = 0.0 %; homozygous model: OR = 2.03, 95 % CI = 1.61–2.57, P h = 0.176, I 2 = 29.2 %), leukemia (heterozygous model: OR = 1.18, 95 % CI = 1.04–1.33, P h = 0.121, I 2 = 29.7 %), and lung cancer (recessive model: OR = 1.16, 95 % CI = 1.01–1.35, P h = 0.182, I 2 = 20.9 %), as shown in Table 1. For the lung cancer studies, we also performed subgroup analysis by smoker habits, no significant association was found among smokers and non-smokers.
Ethnicity and cancer risk attributed to the XRCC1 Arg194Trp polymorphism
We further examined the association of the XRCC1 Arg194Trp polymorphism and cancer risk according to cancer type and ethnicity (Table 2) because there was significant heterogeneity between studies. For samples of Asians, we found that individuals with the minor variant genotypes had a higher risk of esophageal cancer (recessive model: OR = 1.34, 95 % CI = 1.07–1.68, P h = 0.122, I 2 = 41.5 %; homozygous model: OR = 1.30, 95 % CI = 1.03–1.65, P h = 0.185, I 2 = 35.4 %) and glioma (dominant model: OR = 1.23, 95 % CI = 1.09–1.39, P h = 0.237, I 2 = 26.4 %; recessive model: OR = 1.80, 95 % CI = 1.40–2.31, P h = 0.625, I 2 = 0.0 %; homozygous model: OR = 1.87, 95 % CI = 1.45–2.41, P h = 0.569, I 2 = 0.0 %; additive model: OR = 1.29, 95 % CI = 1.11–1.51, P h = 0.057, I 2 = 53.5 %). For samples of Caucasians, significantly increased cancer risk was observed among leukemia (dominant model: OR = 1.28, 95 % CI = 1.06–1.54, P h = 0.186, I 2 = 28.0 %; heterozygous model: OR = 1.26, 95 % CI = 1.04–1.53, P h = 0.496, I 2 = 0.0 %) and significantly decreased cancer risk was observed among lung cancer (dominant model: OR = 0.84, 95 % CI = 0.74–0.95, P h = 0.139, I 2 = 32.4 %; additive model: OR = 0.83, 95 % CI = 0.73–0.93, P h = 0.254, I 2 = 19.9 %) and lymphoma (additive model: OR = 0.77, 95 % CI = 0.59–0.99, P h = 0.400, I 2 = 0.0 %).
Source of controls and cancer risk attributed to the XRCC1 Arg194Trp polymorphism
We also examined the association of the XRCC1 Arg194Trp polymorphism and cancer risk according to cancer type and source of controls (Table 3). For the population-based studies, the XRCC1 Arg194Trp polymorphism was associated with risk of breast cancer (dominant model: OR = 0.91, 95 % CI = 0.84–0.99, P h = 0.117, I 2 = 30.7 %; heterozygous model: OR = 0.91, 95 % CI = 0.81–0.99, P h = 0.174, I 2 = 24.8 %), esophageal cancer (recessive model: OR = 1.44, 95 % CI = 0.81–0.99, P h = 0.174, I 2 = 24.8 %; homozygous model: OR = 1.41, 95 % CI = 1.11–1.78, P h = 0.386, I 2 = 1.2 %), gastric cancer (dominant model: OR = 0.79, 95 % CI = 0.63–0.98, P h = 0.727, I 2 = 0.0 %), and glioma (recessive model: OR = 1.93, 95 % CI = 1.07–3.46, P h = 0.525, I 2 = 0.0 %; homozygous model: OR = 4.90, 95 % CI = 2.46–9.76, P h = 0.641, I 2 = 0.0 %). For the hospital-based studies, significant association was observed among bladder cancer (recessive model: OR = 1.78, 95 % CI = 1.10–2.88, P h = 0.217, I 2 = 27.7 %; homozygous model: OR = 1.81, 95 % CI = 1.11–2.95, P h = 0.170, I 2 = 33.9 %), breast cancer (dominant model: OR = 1.17, 95 % CI = 1.05–1.30, P h = 0.266, I 2 = 17.6 %; heterozygous model: OR = 1.16, 95 % CI = 1.04–1.29, P h = 0.423, I 2 = 2.3 %; additive model: OR = 1.14, 95 % CI = 1.01–1.29, P h = 0.085, I 2 = 37.3 %), colorectal cancer (dominant model: OR = 1.17, 95 % CI = 1.03–1.33, P h = 0.238, I 2 = 21.6 %; heterozygous model: OR = 1.17, 95 % CI = 1.02–1.33, P h = 0.244, I 2 = 20.9 %; additive model: OR = 1.14, 95 % CI = 1.02–1.27, P h = 0.254, I 2 = 19.9 %), gastric cancer (recessive model: OR = 1.48, 95 % CI = 1.17–1.87, P h = 0.135, I 2 = 40.5 %), giloma (recessive model: OR = 1.75, 95 % CI = 1.37–2.23, P h = 0.682, I 2 = 0.0 %; homozygous model: OR = 1.81, 95 % CI = 1.41–2.32, P h = 0.611, I 2 = 0.0 %), and lung cancer (heterozygous model: OR = 0.86, 95 % CI = 0.75–1.00, P h = 0.025, I 2 = 47.4 %).
Anatomical site, histological type, and association of the XRCC1 Arg194Trp polymorphism with cancer risk
We next completed a subgroup analysis by cancer type and histological type or anatomical location (Table 4). Overall, there was no association between the XRCC1 Arg194Trp polymorphism and risk of lung adenocarcinoma, lung squamous cell carcinoma, and cardia gastric cancer. For head and neck cancer, significant increased oral cancer risk was observed among heterozygous model (OR = 1.34, 95 % CI = 1.07–1.68, P h = 0.183, I 2 = 35.7 %). For leukemia, significant increased acute myeloblastic leukemia (AML) risk was observed among dominant model (OR = 1.32, 95 % CI = 1.11–1.56, P h = 0.120, I 2 = 48.6 %) and heterozygous model (OR = 1.31, 95 % CI = 1.10–1.57, P h = 0.380, I 2 = 2.4 %).
Heterogeneity analysis
There was significant heterogeneity among these studies for dominant model comparison (P h < 0.001), recessive model comparison (P h = 0.015), homozygous model comparison (P h < 0.001), heterozygous model comparison (P h < 0.001), and additive model comparison (P h < 0.001). Then, we assessed the source of heterogeneity by ethnicity, cancer type, source of controls, HWE, and sample size. Table 5 lists the results of meta-regression analysis. The results of meta-regression indicated that source of controls (dominant model: P = 0.008; heterozygous model: P = 0.012; additive model: P = 0.012) and HWE (dominant model: P = 0.002; homozygous model: P = 0.022; heterozygous model: P = 0.016; additive model: P = 0.004) but not ethnicity (dominant model: P = 0.857; recessive model: P = 0.877; homozygous model: P = 0.902; heterozygous model: P = 0.994; additive model: P = 0.955), cancer type (dominant model: P = 0.637; recessive model: P = 0.503; homozygous model: P = 0.380; heterozygous model: P = 0.658; additive model: P = 0.458), and sample size (dominant model: P = 0.082; recessive model: P = 0.394; homozygous model: P = 0.080; heterozygous model: P = 0.182; additive model: P = 0.058) contributed to substantial heterogeneity among the meta-analysis.
High between-studies heterogeneity was observed among gastric cancer (dominant model: I 2 = 81.4; heterozygous model: I 2 = 77.9; additive model: I 2 = 82.6), glioma (dominant model: I 2 = 81.4; heterozygous model: I 2 = 80.3; additive model: I 2 = 82.9), pancreatic cancer (dominant model: I 2 = 88.2; heterozygous model: I 2 = 88.1; additive model: I 2 = 87.7), Asians of gastric cancer (dominant model: I 2 = 87.1; homozygote model: I 2 = 75.9; heterozygous model: I 2 = 84.0; additive model: I 2 = 87.3), Asians of head and neck cancer (dominant model: I 2 = 80.8; homozygote model: I 2 = 77.1; additive model: I 2 = 83.5), Asians of prostate cancer (dominant model: I 2 = 86.4; heterozygous model: I 2 = 86.5; additive model: I 2 = 81.1), Indians of head and neck cancer (dominant model: I 2 = 81.6; heterozygous model: I 2 = 77.7; additive model: I 2 = 83.0), population-based studies of glioma (dominant model: I 2 = 94.3; heterozygous model: I 2 = 97.2; additive model: I 2 = 96.2), hospital-based studies of gastric cancer (dominant model: I 2 = 84.0; homozygote model: I 2 = 80.7; additive model: I 2 = 83.7), hospital-based studies of pancreatic cancer (dominant model: I 2 = 88.2; heterozygous model: I 2 = 88.1; additive model: I 2 = 87.7), hospital-based studies of prostate cancer (heterozygous model: I 2 = 75.4), nasopharyngeal cancer (dominant model: I 2 = 89.2; recessive model: I 2 = 81.6; homozygote model: I 2 = 86.6; heterozygous model: I 2 = 84.1; additive model: I 2 = 91.1), and Asians of thyroid cancer (homozygote model: I 2 = 79.8; additive model: I 2 = 80.7). Significant deviation from HWE was detected in the ten articles. When these studies were excluded, the high between-studies heterogeneity was deleted among glioma (dominant model: I 2 = 34.5; heterozygous model: I 2 = 23.7; additive model: I 2 = 53.8) and population-based studies of glioma (dominant model: I 2 = 0.0). When the small studies were excluded, the high between-studies heterogeneity was deleted among glioma (dominant model: I 2 = 54.7; heterozygous model: I 2 = 31.1; additive model: I 2 = 70.6) and population-based studies of glioma (dominant model: I 2 = 0.0).
Sensitivity analysis
Examining genotype frequencies in the controls, significant deviation from HWE was detected in the ten articles [106,118,145,156,161,169,180,182,185,200]. When these studies were excluded, the result was changed among population-based studies of glioma (recessive model: OR = 3.34, 95 % CI = 0.56–20.06; homozyhous model: OR = 3.30, 95 % CI = 0.55–19.80), as shown in Table 6. When the study of small sample was excluded, the results was changed among leukemia (heterozygous model: OR = 1.14, 95 % CI = 0.96–1.36), lung cancer (recessive model: OR = 1.17, 95 % CI = 0.97–1.41), Caucasians of lymphoma (additive model: OR = 0.79, 95 % CI = 0.61–1.03), population-based studies of glioma (recessive model: OR = 3.34, 95 % CI = 0.56–20.06; homozyhous model: OR = 3.30, 95 % CI = 0.55–19.80), hospital-based studies of bladder cancer (recessive model: OR = 1.34, 95 % CI = 0.69–2.58; homozygous model: OR = 1.42, 95 % CI = 0.74–2.75), and hospital-based studies of lung cancer (heterozygous model: OR = 0.86, 95 % CI = 0.74–1.01), as shown in Table 7. Last, when the study of Xing et al. [103] was excluded, the results were changed among esophageal cancer (recessive model: OR = 1.18, 95 % CI = 0.91–1.52; additive model: OR = 1.15, 95 % CI = 0.88–1.51), Asians of esophageal cancer (recessive model: OR = 1.13, 95 % CI = 0.86–1.48; additive model: OR = 1.12, 95 % CI = 0.84–1.48), and population-based studies of esophageal cancer (recessive model: OR = 1.26, 95 % CI = 0.96–1.65; additive model: OR = 1.24, 95 % CI = 0.93–1.64). When the study of Mitra et al. [27] was excluded, the results were changed among the population-based studies of breast cancer (dominant model: OR = 0.93, 95 % CI = 0.86–1.01; heterozygous model: OR = 0.93, 95 % CI = 0.86–1.01). When the study of Li et al. [206] was excluded, the results were changed among hospital-based studies of colorectal cancer (dominant model: OR = 1.08, 95 % CI = 0.93–1.25; heterozygous model: OR = 1.08, 95 % CI = 0.92–1.25; additive model: OR = 1.07, 95 % CI = 0.94–1.22). When the study of Shen et al. [113] was excluded, the results were changed among hospital-based studies of gastric cancer (recessive model: OR = 1.27, 95 % CI = 0.96–1.68). When the study of Ramachandran et al. [83] was excluded, the results were changed among oral cancer (heterozygous model: OR = 1.21, 95 % CI = 0.95–1.54).
Publication bias
Both Begg’s funnel plot and Egger’s test were performed to access the publication bias of this meta-analysis. Begg’s funnel plots did not reveal any evidence of obvious asymmetry in any genetic model in the overall meta-analysis (Fig. 2). The Egger’s test results also suggested no evidence of publication bias in the meta-analysis of Arg194Trp (dominant model: P = 0.651; heterozygous model: P = 0.697; recessive model: P = 0.534; additive model: P = 0.533; homozygous model: P = 0.678), indicating that our results were statistically robust.
Discussion
Cancer is the result of a series of DNA alternations in single cell or clone of that cell, which lead to loss of normal function, aberrant or uncontrolled cell growth, and often metastases. BER is initiated by recognition and excision of damaged base by the specific DNA glycosylase. X-ray repair cross-complementing groups 1 protein is a scaffold protein directly associated with polymerase beta, DNA ligase III, and poly (ADP-ribose) polymerase in a complex to facilitate the BER and single-strand break repair (SSBR) processes [213–215]. A recent report provides data showing that the E2F1 transcription factor regulates XRCC1 and promotes DNA repair [216]. A XRCC1 deletion mutation in null homozygous mice is embryonic lethal [217]. XRCC1 has two BRCA1 carboxyl-terminal (BRCT) domains (BRCT1 and BRCT2), located centrally and at the C-terminal end, respectively. BRCT2 is responsible for binding and stabilizing DNA ligase III and is required for single-strand breaks and gaps repair (SSBR), specifically during the G0/G1 phases of the cell cycle [218]. The center of BRCT1 domain binds to and down-regulates the single-strand breaks and gaps recognition protein PARP1 and is required for efficient SSBR during both G1 and S/G2 phases of the cell cycle. Arg194Trp is located in a domain that separates but connects the XRCC1 NH2 terminal and BRCT. Arg194Trp mutation will change XRCC1’s structure but may not influence the function of XRCC1. A number of studies have reported the association of XRCC1 Arg194Trp polymorphism with risk of cancer; however, the results remained controversial, although some original studies thought that Arg194Trp polymorphism was associated with risk of cancer, others had different opinions. In order to resolve this conflict, the meta-analysis of 201 eligible studies including 59,227 cases and 81,587 controls was performed to derive a more precise estimation of the association between XRCC1 Arg194Trp polymorphism and risk of different types of cancer.
Overall, significantly increased cancer risk was found when all eligible studies were pooled into the meta-analysis of Arg194Trp. In further stratified and sensitivity analyses, significantly increased glioma risk was found among Asians, significantly decreased lung cancer risk was found among Caucasians, and significant increased breast cancer risk was found among hospital-based studies. It also should be considered that the apparent inconsistency of these results may underlie differences in ethnicity, lifestyle, and disease prevalence as well as possible limitations due to the relatively small sample size. The current knowledge of carcinogenesis indicates a multi-factorial and multistep process that involves various genetic alterations and several biological pathways. Thus, it is unlikely that risk factors of cancer work in isolation from each other. And the same polymorphisms may play different roles in cancer susceptibility because cancer is a complicated multi-genetic disease, and different genetic backgrounds may contribute to the discrepancy. And even more importantly, the low penetrance genetic effects of single polymorphism may largely depend on interaction with other polymorphisms and/or a particular environmental exposure. We observed a wide variation of the Trp allele frequencies of control resources in Asians (0.296), Indians (0.200), Caucasians (0.077), and Africans (0.082), and this different allele frequency might account for the association between the XRCC1 Arg194Trp polymorphism and cancer susceptibility among different ethnicity.
Based on biochemical properties described for XRCC1 polymorphism, we would expect that the Trp allele would be associated with higher susceptibility for all types of cancer. However, our results showed that such association was observed just for breast cancer, glioma, and lung cancer, suggesting that other factors may be modulating the XRCC1 polymorphism functionality. However, the exact mechanism for association between different cancer types and XRCC1 Arg194Trp polymorphism was not clear, carcinogenetic mechanism may differ by different tumor sites and the XRCC1 genetic variants may exert varying effects in different cancers. Several previous meta-analyses assessed the association of XRCC1 Arg194Trp polymorphism with risk of gastric and lung cancer, and so on. Wang et al. [219] in 2009 found decreased lung cancer risk among subjects carrying XRCC1 194 Arg/Trp genotype (OR = 0.88, 95 % CI = 0.79–0.97). However, Dai et al. [203] in 2012 found that the risk for lung cancer was increased among the variant homozygote Trp/Trp of codon 194 polymorphism, compared with the wild-type Arg/Arg (OR: 1.19; 95 % CI = 1.01–1.39). In the subgroup analyses by ethnicity, the OR for the variant homozygote Trp/Trp of codon 194 was 1.21(95 % CI = 1.02–1.43) for Asian. Chen et al. [220] in 2012 suggested XRCC1 Arg194Trp homozygous mutant genotype (Trp/Trp) was found to be associated with increased risk of gastric cancer. However, our meta-analysis indicates that Arg194Trp polymorphism is associated with decreased lung cancer in Caucasians and new study is important for Arg194Trp association in gastric cancer. Our meta-analysis should be more stringent and comprehensive. Firstly, more up to date studies were recruited to provide statistically significant results. Secondly, the association of Arg194Trp with risk of cancer had been explored in detail.
In the present meta-analysis, highly between-studies heterogeneity was observed in the hospital-based controls for some cancer types, such as gastric, prostate, and pancreatic cancers. The reason may be that the hospital-based studies have some biases because such controls may contain certain benign diseases which are prone to develop malignancy and may not be very representative of the general population. Thus, the use of a proper and representative cancer-free control subjects is very important in reducing biases in such genotype association studies. The results of meta-regression also indicated that source of controls contributed to substantial heterogeneity among the meta-analysis. And this indicates that it may be not appropriate to use an overall estimation of the relationship between XRCC1 Arg194Trp polymorphism and risk of cancer.
The current meta-analysis has some strength compared with individual studies and previous meta-analyses. First, differently from previous meta-analyses, we explored the impact of XRCC1 Arg194Trp on a great diversity of cancer sites, allowing for a general view of its influence on cancer susceptibility. Second, our meta-analysis explores and analyzes the sources of heterogeneity between studies about XRCC1 Arg194Trp in cancer. Third, more up to date studies were recruited to provide statistically significant results. As an example of these crucial features, differently from a recent pooled analysis of nine studies with a total of 1,709 colorectal cancer cases and 3,233 controls [221], we found 18 studies with 5,267 cases and 8,713 controls on colorectal cancer risk.
In summary, this meta-analysis suggests Arg194Trp polymorphism may be associated with increased breast cancer risk, Arg194Trp polymorphism is associated with increased glioma risk among Asians, and Arg194Trp polymorphism is associated with decreased lung cancer risk among Caucasians. In addition, our work also points out the importance of new studies for Arg194Trp association in some cancer types, such as gastric, pancreatic, prostate, and nasopharyngeal cancers, where at least some of the covariates responsible for heterogeneity could be controlled, to obtain a more conclusive understanding about the function of the XRCC1 Arg194Trp polymorphism in cancer development (I 2 > 75 %).
References
Wood RD, Mitchell M, Sgouros J, Lindahl T. Human DNA repair genes. Science. 2001;291:1284–9.
Yu Z, Chen J, Ford BN, Brackley ME, Glickman BW. Human DNA repair systems: an overview. Environ Mol Mutagen. 1999;33:3–20.
Thacker J, Zdzienicka MZ. The mammalian XRCC genes: their roles in DNA repair and genetic stability. DNA Repair (Amst). 2003;2:655–72.
Vidal AE, Boiteux S, Hickson AD, Radicella JP. XRCC1 coordinates the initial and late stages of DNA abasic site repair through protein–protein interactions. EMBO J. 2001;20:6530–9.
Lu AL, Li XH, Gu YS, Wright PM, Chang DY. Repair of oxidative DNA damage–mechanisms and functions. Cell Biochem Biophys. 2001;35:141–70.
Kubota Y, Nash RA, Klungland A, Schär P, Barnes DE, Lindahl T. Resconstitution of DNA base excision repair with purified human proteins: Interaction between DNA polymerase beta and the XRCC1 protein. EMBO J. 1996;15:6662–70.
Shen MR, Jones IM, Mohrenweiser H. No conservative amino acid substitution variants exist at polymorphic frequency in DNA repair genes in healthy humans. Cancer Res. 1998;58:604–8.
Duell EJ, Millikan RC, Pittman GS, Winkel S, Lunn RM, Tse CK, et al. Polymorphisms in the DNA repair gene XRCC1 and breast cancer. Cancer Epidemiol Biomarkers Prev. 2001;10:217–22.
Kim SU, Park SK, Yoo KY, Yoon KS, Choi JY, Seo JS, et al. XRCC1 genetic polymorphism and breast cancer risk. Pharmacogenetics. 2002;12:335–8.
Smith TR, Levine EA, Perrier ND, Miller MS, Freimanis RI, Lohman K, et al. DNA-repair genetic polymorphisms and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2003;12:1200–4.
Moullan N, Cox DG, Angèle S, Romestaing P, Gérard JP, Hall J. Polymorphisms in the DNA repair gene XRCC1, breast cancer risk, and response to radiotherapy. Cancer Epidemiol Biomarkers Prev. 2003;12:1168–74.
Smith TR, Miller MS, Lohman K, Lange EM, Case LD, Mohrenweiser HW, et al. Polymorphisms of XRCC1 and XRCC3 genes and susceptibility to breast cancer. Cancer Lett. 2003;190:183–90.
Han J, Hankinson SE, De Vivo I, Spiegelman D, Tamimi RM, Mohrenweiser HW, et al. A prospective study of XRCC1 haplotypes and their interaction with plasma carotenoids on breast cancer risk. Cancer Res. 2003;63:8536–41.
Deligezer U, Dalay N. Association of the XRCC1 gene polymorphisms with cancer risk in Turkish breast cancer patients. Exp Mol Med. 2004;36:572–5.
Patel AV, Calle EE, Pavluck AL, Feigelson HS, Thun MJ, Rodriguez C. A prospective study of XRCC1 (X-ray cross-complementing group 1) polymorphisms and breast cancer risk. Breast Cancer Res. 2005;7:R1168–73.
Chacko P, Rajan B, Joseph T, Mathew BS, Pillai MR. Polymorphisms in DNA repair gene XRCC1 and increased genetic susceptibility to breast cancer. Breast Cancer Res Treat. 2005;89:15–21.
Shen J, Gammon MD, Terry MB, Wang L, Wang Q, Zhang F, et al. Polymorphisms in XRCC1 modify the association between polycyclic aromatic hydrocarbon-DNA adducts, cigarette smoking, dietary antioxidants, and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2005;14:336–42.
Brewster AM, Jorgensen TJ, Ruczinski I, Huang HY, Hoffman S, Thuita L, et al. Polymorphisms of the DNA repair genes XPD (Lys751Gln) and XRCC1 (Arg399Gln and Arg194Trp): relationship to breast cancer risk and familial predisposition to breast cancer. Breast Cancer Res Treat. 2006;95:73–80.
Zhang Y, Newcomb PA, Egan KM, Titus-Ernstoff L, Chanock S, Welch R, et al. Genetic polymorphisms in base-excision repair pathway genes and risk of breast cancer. Cancer Epidemiol Biomarkers Prev. 2006;15:353–8.
Pachkowski BF, Winkel S, Kubota Y, Swenberg JA, Millikan RC, Nakamura J. XRCC1 genotype and breast cancer: functional studies and epidemiologic data show interactions between XRCC1 codon 280 His and smoking. Cancer Res. 2006;66:2860–8.
Jin MJ, Chen K, Zhang SS, Zhang YJ, Ren YJ, Xu H, et al. Association of single nucleotide polymorphisms and haplotypes in DNA repair gene XRCC1 with susceptibility of breast cancer. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2006;35:370–6.
Thyagarajan B, Anderson KE, Folsom AR, Jacobs Jr DR, Lynch CF, Bargaje A, et al. No association between XRCC1 and XRCC3 gene polymorphisms and breast cancer risk: Iowa Women's Health Study. Cancer Detect Prev. 2006;30:313–21.
Silva SN, Moita R, Azevedo AP, Gouveia R, Manita I, Pina JE, et al. Menopausal age and XRCC1 gene polymorphisms: role in breast cancer risk. Cancer Detect Prev. 2007;31:303–9.
Sangrajrang S, Schmezer P, Burkholder I, Waas P, Boffetta P, Brennan P, et al. Polymorphisms in three base excision repair genes and breast cancer risk in Thai women. Breast Cancer Res Treat. 2008;111:279–88.
Loizidou MA, Michael T, Neuhausen SL, Newbold RF, Marcou Y, Kakouri E, et al. Genetic polymorphisms in the DNA repair genes XRCC1, XRCC2 and XRCC3 and risk of breast cancer in Cyprus. Breast Cancer Res Treat. 2008;112:575–9.
Smith TR, Levine EA, Freimanis RI, Akman SA, Allen GO, Hoang KN, et al. Polygenic model of DNA repair genetic polymorphisms in human breast cancer risk. Carcinogenesis. 2008;29:2132–8.
Mitra AK, Singh N, Singh A, Garg VK, Agarwal A, Sharma M, et al. Association of polymorphisms in base excision repair genes with the risk of breast cancer: a case–control study in North Indian women. Oncol Res. 2008;17:127–35.
Sterpone S, Mastellone V, Padua L, Novelli F, Patrono C, Cornetta T, et al. Single-nucleotide polymorphisms in BER and HRR genes, XRCC1 haplotypes and breast cancer risk in Caucasian women. J Cancer Res Clin Oncol. 2010;136:631–6.
Ming-Shiean H, Yu JC, Wang HW, Chen ST, Hsiung CN, Ding SL, et al. Synergistic effects of polymorphisms in DNA repair genes and endogenous estrogen exposure on female breast cancer risk. Ann Surg Oncol. 2010;17:760–71.
Liu L, Yuan P, Liu L, Wu C, Zhang X, Guo H, et al. A functional -77 T > C polymorphism in XRCC1 is associated with risk of breast cancer. Breast Cancer Res Treat. 2011;125:479–87.
Zipprich J, Terry MB, Brandt-Rauf P, Freyer GA, Liao Y, Agrawal M, et al. XRCC1 polymorphisms and breast cancer risk from the New York Site of the Breast Cancer Family Registry: A family-based case–control study. J Carcinog. 2010;9:4.
Qian Y, Zhang JP, Dong J, Wang FR, Lin YD, Xu M, et al. Relationship between polymorphisms of X-ray repair cross-complementing group 1 gene Arg194Trp, Arg399Gln and susceptibility of breast cancer. Zhonghua Yu Fang Yi Xue Za Zhi. 2010;44:242–6.
Sobczuk A, Romanowicz-Makowska H, Fiks T, Baszczyński J, Smolarz B. XRCC1 and XRCC3 DNA repair gene polymorphisms in breast cancer women from the Lodz region of Poland. Pol J Pathol. 2009;60:76–80.
Forsti A, Angelini S, Festa F, Sanyal S, Zhang Z, Grzybowska EB, et al. Single nucleotide polymorphisms in breast cancer. Oncol Rep. 2004;11:917–22.
Ratnasinghe D, Yao SX, Tangrea JA, Qiao YL, Andersen MR, Barrett MJ, et al. Polymorphisms of the DNA repair gene XRCC1 and lung cancer risk. Cancer Epidemiol Biomarkers Prev. 2010;10:119–23.
David-Beabes GL, London SJ. Genetic polymorphism of XRCC1 and lung cancer risk among African-Americans and Caucasians. Lung Cancer. 2001;34:333–9.
Chen S, Tang D, Xue K, Xu L, Ma G, Hsu Y, et al. DNA repair gene XRCC1 and XPD polymorphisms and risk of lung cancer in a Chinese population. Carcinogenesis. 2002;23:1321–5.
Hung RJ, Brennan P, Canzian F, Szeszenia-Dabrowska N, Zaridze D, Lissowska J, et al. Large-scale investigation of base excision repair genetic polymorphisms and lung cancer risk in a multicenter study. J Natl Cancer Inst. 2005;97:567–76.
Schneider J, Classen V, Bernges U, Philipp M. XRCC1 polymorphism and lung cancer risk in relation to tobacco smoking. Int J Mol Med. 2005;16:709–16.
Shen M, Berndt SI, Rothman N, Mumford JL, He X, Yeager M, et al. Polymorphisms in the DNA base excision repair genes APEX1 and XRCC1 and lung cancer risk in Xuan Wei, China. Anticancer Res. 2005;25:537–42.
Chan EC, Lam SY, Fu KH, Kwong YL. Polymorphisms of the GSTM1, GSTP1, MPO, XRCC1, and NQO1 genes in Chinese patients with non-small cell lung cancers: relationship with aberrant promoter methylation of the CDKN2A and RARB genes. Cancer Genet Cytogenet. 2005;162:10–20.
Hu Z, Ma H, Lu D, Zhou J, Chen Y, Xu L, et al. A promoter polymorphism (–77 T > C) of DNA repair gene XRCC1 is associated with risk of lung cancer in relation to tobacco smoking. Pharmacogenet Genomics. 2005;15:457–63.
Zienolddiny S, Campa D, Lind H, Ryberg D, Skaug V, Stangeland L, et al. Polymorphisms of DNA repair genes and risk of non-small cell lung cancer. Carcinogenesis. 2006;27:560–7.
Matullo G, Dunning AM, Guarrera S, Baynes C, Polidoro S, Garte S, et al. DNA repair polymorphisms and cancer risk in non-smokers in a cohort study. Carcinogenesis. 2006;27:997–1007.
Hao B, Miao X, Li Y, Zhang X, Sun T, Liang G, et al. A novel T–77C polymorphism in DNA repair gene XRCC1 contributes to diminished promoter activity and increased risk of non-small cell lung cancer. Oncogene. 2006;25:3613–20.
Landi S, Gemignani F, Canzian F, Gaborieau V, Barale R, Landi D, et al. DNA repair and cell cycle control genes and the risk of young-onset lung cancer. Cancer Res. 2006;66:11062–9.
De Ruyck K, Szaumkessel M, De Rudder I, Dehoorne A, Vral A, Claes K, et al. Polymorphisms in base-excision repair and nucleotide-excision repair genes in relation to lung cancer risk. Mutat Res. 2007;631:101–10.
Pachouri SS, Sobti RC, Kaur P, Singh J. Contrasting impact of DNA repair gene XRCC1 polymorphisms Arg399Gln and Arg194Trp on the risk of lung cancer in the north-Indian population. DNA Cell Biol. 2007;26:186–91.
Yin J, Vogel U, Ma Y, Qi R, Sun Z, Wang H. The DNA repair gene XRCC1 and genetic susceptibility of lung cancer in a northeastern Chinese population. Lung Cancer. 2007;56:153–60.
Improta G, Sgambato A, Bianchino G, Zupa A, Grieco V, La Torre G, et al. Polymorphisms of the DNA repair genes XRCC1 and XRCC3 and risk of lung and colorectal cancer: a case–control study in a Southern Italian population. Anticancer Res. 2008;28:2941–6.
Li M, Yin Z, Guan P, Li X, Cui Z, Zhang J, et al. XRCC1 polymorphisms, cooking oil fume and lung cancer in Chinese women nonsmokers. Lung Cancer. 2008;62:145–51.
Yin J, Vogel U, Ma Y, Qi R, Wang H. Association of DNA repair gene XRCC1 and lung cancer susceptibility among nonsmoking Chinese women. Cancer Genet Cytogenet. 2009;188:26–31.
Tanaka Y, Maniwa Y, Bermudez VP, Doi T, Nishio W, Ohbayashi C, et al. Nonsynonymous single nucleotide polymorphisms in DNA damage repair pathways and lung cancer risk. Cancer. 2010;116:896–902.
Janik J, Swoboda M, Janowska B, Cieśla JM, Gackowski D, Kowalewski J, et al. 8-Oxoguanine incision activity is impaired in lung tissues of NSCLC patients with the polymorphism of OGG1 and XRCC1 genes. Mutat Res. 2011;709–710:21–31.
Sliwinski T, Krupa R, Wisniewska-Jarosinska M, Lech J, Morawiec Z, Chojnacki J, et al. No association between the Arg194Trp and Arg399Gln polymorphisms of the XRCC1 gene and colorectal cancer risk and progression in a Polish population. Exp Oncol. 2008;30:253–4.
Skjelbred CF, Saebø M, Wallin H, Nexø BA, Hagen PC, Lothe IM, et al. Polymorphisms of the XRCC1, XRCC3 and XPD genes and risk of colorectal adenoma and carcinoma, in a Norwegian cohort: a case–control study. BMC Cancer. 2006;6:67.
Narter KF, Ergen A, Agaçhan B, Görmüs U, Timirci O, Isbir T. Bladder cancer and polymorphisms of DNA repair genes (XRCC1, XRCC3, XPD, XPG, APE1, hOGG1). Anticancer Res. 2009;29:1389–93.
Sak SC, Barrett JH, Paul AB, Bishop DT, Kiltie AE. DNA repair gene XRCC1 polymorphisms and bladder cancer risk. BMC Genet. 2007;8:13.
Matullo G, Guarrera S, Sacerdote C, Polidoro S, Davico L, Gamberini S, et al. Polymorphisms/haplotypes in DNA repair genes and smoking: a bladder cancer case–control study. Cancer Epidemiol Biomarkers Prev. 2005;14:2569–78.
Figueroa JD, Malats N, Real FX, Silverman D, Kogevinas M, Chanock S, et al. Genetic variation in the base excision repair pathway and bladder cancer risk. Hum Genet. 2007;121:233–42.
Wu X, Gu J, Grossman HB, Amos CI, Etzel C, Huang M, et al. Bladder cancer predisposition: a multigenic approach to DNA-repair and cell-cycle-control genes. Am J Hum Genet. 2006;78:464–79.
Stern MC, Umbach DM, van Gils CH, Lunn RM, Taylor JA. DNA repair gene XRCC1 polymorphisms, smoking, and bladder cancer risk. Cancer Epidemiol Biomarkers Prev. 2001;10:125–31.
Andrew AS, Nelson HH, Kelsey KT, Moore JH, Meng AC, Casella DP, et al. Concordance of multiple analytical approaches demonstrates a complex relationship between DNA repair gene SNPs, smoking and bladder cancer susceptibility. Carcinogenesis. 2006;27:1030–7.
Wang M, Qin C, Zhu J, Yuan L, Fu G, Zhang Z, et al. Genetic variants of XRCC1, APE1, and ADPRT genes and risk of bladder cancer. DNA Cell Biol. 2010;29:303–11.
Andrew AS, Karagas MR, Nelson HH, Guarrera S, Polidoro S, Gamberini S, et al. DNA repair polymorphisms modify bladder cancer risk: a multi-factor analytic strategy. Hum Hered. 2008;65:105–18.
Winsey SL, Haldar NA, Marsh HP, Bunce M, Marshall SE, Harris AL, et al. A variant within the DNA repair gene XRCC3 is associated with the development of melanoma skin cancer. Cancer Res. 2000;60:5612–6.
Kang SY, Lee KG, Lee W, Shim JY, Ji SI, Chung KW, et al. Polymorphisms in the DNA repair gene XRCC1 associated with basal cell carcinoma and squamous cell carcinoma of the skin in a Korean population. Cancer Sci. 2007;98:716–20.
Demokan S, Demir D, Suoglu Y, Kiyak E, Akar U, Dalay N. Polymorphisms of the XRCC1 DNA repair gene in head and neck cancer. Pathol Oncol Res. 2005;11:22–5.
Kietthubthew S, Sriplung H, Au WW, Ishida T. Polymorphism in DNA repair genes and oral squamous cell carcinoma in Thailand. Int J Hyg Environ Health. 2006;209:21–9.
Cao Y, Miao XP, Huang MY, Deng L, Hu LF, Ernberg I, et al. Polymorphisms of XRCC1 genes and risk of nasopharyngeal carcinoma in the Cantonese population. BMC Cancer. 2006;6:167.
Kowalski M, Przybylowska K, Rusin P, Olszewski J, Morawiec-Sztandera A, Bielecka-Kowalska A, et al. Genetic polymorphisms in DNA base excision repair gene XRCC1 and the risk of squamous cell carcinoma of the head and neck. J Exp Clin Cancer Res. 2009;28:37.
Chiang FY, Wu CW, Hsiao PJ, Kuo WR, Lee KW, Lin JC, et al. Association between polymorphisms in DNA base excision repair genes XRCC1, APE1, and ADPRT and differentiated thyroid carcinoma. Clin Cancer Res. 2008;14:5919–24.
Varzim G, Monteiro E, Silva RA, Fernandes J, Lopes C. CYP1A1 and XRCC1 gene polymorphisms in SCC of the larynx. Eur J Cancer Prev. 2003;12:495–9.
Tae K, Lee HS, Park BJ, Park CW, Kim KR, Cho HY, et al. Association of DNA repair gene XRCC1 polymorphisms with head and neck cancer in Korean population. Int J Cancer. 2004;111:805–8.
Ruwali M, Khan AJ, Shah PP, Singh AP, Pant MC, Parmar D. Cytochrome P450 2E1 and head and neck cancer: interaction with genetic and environmental risk factors. Environ Mol Mutagen. 2009;50:473–82.
Majumder M, Sikdar N, Ghosh S, Roy B. Polymorphisms at XPD and XRCC1 DNA repair loci and increased risk of oral leukoplakia and cancer among NAT2 slow acetylators. Int J Cancer. 2007;120:2148–56.
Applebaum KM, McClean MD, Nelson HH, Marsit CJ, Christensen BC, Kelsey KT. Smoking modifies the relationship between XRCC1 haplotypes and HPV16-negative head and neck squamous cell carcinoma. Int J Cancer. 2009;124:2690–6.
Majumder M, Sikdar N, Paul RR, Roy B. Increased risk of oral leukoplakia and cancer among mixed tobacco users carrying XRCC1 variant haplotypes and cancer among smokers carrying two risk genotypes: one on each of two loci, GSTM3 and XRCC1 (Codon 280). Cancer Epidemiol Biomarkers Prev. 2005;14:2106–12.
Sturgis EM, Castillo EJ, Li L, Zheng R, Eicher SA, Clayman GL, et al. Polymorphisms of DNA repair gene XRCC1 in squamous cell carcinoma of the head and neck. Carcinogenesis. 1999;20:2125–9.
Yang ZH, Du B, Wei YS, Zhang JH, Zhou B, Liang WB, et al. Genetic polymorphisms of the DNA repair gene and risk of nasopharyngeal carcinoma. DNA Cell Biol. 2007;26:491–6.
Yen CY, Liu SY, Chen CH, Tseng HF, Chuang LY, Yang CH, et al. Combinational polymorphisms of four DNA repair genes XRCC1, XRCC2, XRCC3, and XRCC4 and their association with oral cancer in Taiwan. J Oral Pathol Med. 2008;37:271–7.
Olshan AF, Watson MA, Weissler MC, Bell DA. XRCC1 polymorphisms and head and neck cancer. Cancer Lett. 2002;178:181–6.
Ramachandran S, Ramadas K, Hariharan R, Rejnish Kumar R, Radhakrishna Pillai M. Single nucleotide polymorphisms of DNA repair genes XRCC1 and XPD and its molecular mapping in Indian oral cancer. Oral Oncol. 2006;42:350–62.
Jin MJ, Chen K, Zhang Y, Zhang W, Liu B, Zhang YJ. Correlations of single nucleotide polymorphisms of DNA repair gene XRCC1 to risk of colorectal cancer. Ai Zheng. 2007;26:274–9.
Moreno V, Gemignani F, Landi S, Gioia-Patricola L, Chabrier A, Blanco I, et al. Polymorphisms in genes of nucleotide and base excision repair: risk and prognosis of colorectal cancer. Clin Cancer Res. 2006;12:2101–8.
Improta G, Sgambato A, Bianchino G, Zupa A, Grieco V, La Torre G, et al. Polymorphisms of the DNA repair genes XRCC1 and XRCC3 and risk of lung and colorectal cancer: a case–control study in a Southern Italian population. Anticancer Res. 2008;28:2941–6.
Curtin K, Samowitz WS, Wolff RK, Ulrich CM, Caan BJ, Potter JD, et al. Assessing tumor mutations to gain insight into base excision repair sequence polymorphisms and smoking in colon cancer. Cancer Epidemiol Biomarkers Prev. 2009;18:3384–8.
Hong YC, Lee KH, Kim WC, Choi SK, Woo ZH, Shin SK, et al. Polymorphisms of XRCC1 gene, alcohol consumption and colorectal cancer. Int J Cancer. 2005;116:428–32.
Abdel-Rahman SZ, Soliman AS, Bondy ML, Omar S, El-Badawy SA, Khaled HM, et al. Inheritance of the 194Trp and the 399Gln variant alleles of the DNA repair gene XRCC1 are associated with increased risk of early-onset colorectal carcinoma in Egypt. Cancer Lett. 2000;159:79–86.
Gil J, Ramsey D, Stembalska A, Karpinski P, Pesz KA, Laczmanska I, et al. The C/A polymorphism in intron 11 of the XPC gene plays a crucial role in the modulation of an individual's susceptibility to sporadic colorectal cancer. Mol Biol Rep. 2012;39:527–34.
Berndt SI, Huang WY, Fallin MD, Helzlsouer KJ, Platz EA, Weissfeld JL, et al. Genetic variation in base excision repair genes and the prevalence of advanced colorectal adenoma. Cancer Res. 2007;67:1395–404.
Stern MC, Siegmund KD, Corral R, Haile RW. XRCC1 and XRCC3 polymorphisms and their role as effect modifiers of unsaturated fatty acids and antioxidant intake on colorectal adenomas risk. Cancer Epidemiol Biomarkers Prev. 2005;14:609–15.
Stern MC, Conti DV, Siegmund KD, Corral R, Yuan JM, Koh WP, et al. DNA repair single-nucleotide polymorphisms in colorectal cancer and their role as modifiers of the effect of cigarette smoking and alcohol in the Singapore Chinese Health Study. Cancer Epidemiol Biomarkers Prev. 2007;16:2363–72.
McWilliams RR, Bamlet WR, Cunningham JM, Goode EL, de Andrade M, Boardman LA, et al. Polymorphisms in DNA repair genes, smoking, and pancreatic adenocarcinoma risk. Cancer Res. 2008;68:4928–35.
Jiao L, Bondy ML, Hassan MM, Wolff RA, Evans DB, Abbruzzese JL, et al. Selected polymorphisms of DNA repair genes and risk of pancreatic cancer. Cancer Detect Prev. 2006;30:284–91.
Xu Z, Hua LX, Qian LX, Yang J, Wang XR, Zhang W, et al. Relationship between XRCC1 Polymorphisms and susceptibility to prostate cancer in men from Han. South China Asian J Androl. 2007;9:331–8.
van Gils CH, Bostick RM, Stern MC, Taylor JA. Differences in base excision repair capacity may modulate the effect of dietary antioxidant intake on prostate cancer risk: an example of polymorphisms in the XRCC1 gene. Cancer Epidemiol Biomarkers Prev. 2002;11:1279–84.
Hamano T, Matsui H, Sekine Y, Ohtake N, Nakata S, Suzuki K. Polymorphisms of DNA repair genes, XRCC1 and XRCC3, and susceptibility to familial prostate cancer in a Japanese population. Asian Pac J Clin Oncol. 2008;4:21–6.
Agalliu I, Kwon EM, Salinas CA, Koopmeiners JS, Ostrander EA, Stanford JL. Genetic variation in DNA repair genes and prostate cancer risk: results from a population-based study. Cancer Causes Control. 2010;21:289–300.
Hirata H, Hinoda Y, Tanaka Y, Okayama N, Suehiro Y, Kawamoto K, et al. Polymorphisms of DNA repair genes are risk factors for prostate cancer. Eur J Cancer. 2007;43:231–7.
Lee JM, Lee YC, Yang SY, Yang PW, Luh SP, Lee CJ, et al. Genetic polymorphisms of XRCC1 and risk of the esophageal cancer. Int J Cancer. 2001;95:240–6.
Casson AG, Zheng Z, Evans SC, Veugelers PJ, Porter GA, Guernsey DL. Polymorphisms in DNA repair genes in the molecular pathogenesis of esophageal (Barrett) adenocarcinoma. Carcinogenesis. 2005;26:1536–41.
Xing D, Qi J, Miao X, Lu W, Tan W, Lin D. Polymorphisms of DNA repair genes XRCC1 and XPD and their associations with risk of esophageal squamous cell carcinoma in a Chinese population. Int J Cancer. 2002;100:600–5.
Hao B, Wang H, Zhou K, Li Y, Chen X, Zhou G, et al. Identification of genetic variants in base excision repair pathway and their associations with risk of esophageal squamous cell carcinoma. Cancer Res. 2004;64:4378–84.
Yu HP, Zhang XY, Wang XL, Shi LY, Li YY, Li F, et al. DNA repair gene XRCC1 polymorphisms, smoking, and esophageal cancer risk. Cancer Detect Prev. 2004;28:194–9.
Ratnasinghe LD, Abnet C, Qiao YL, Modali R, Stolzenberg-Solomon R, Dong ZW, et al. Polymorphisms of XRCC1 and risk of esophageal and gastric cardia cancer. Cancer Lett. 2004;216:157–64.
Shen H, Xu Y, Qian Y, Yu R, Qin Y, Zhou L, et al. Polymorphisms of the DNA repair gene XRCC1 and risk of gastric cancer in a Chinese population. Int J Cancer. 2000;88:601–6.
Palli D, Polidoro S, D'Errico M, Saieva C, Guarrera S, Calcagnile AS, et al. Polymorphic DNA repair and metabolic genes: a multigenic study on gastric cancer. Mutagenesis. 2010;25:569–75.
Wen YY, Pan XF, Loh M, Tian Z, Yang SJ, Lv SH, et al. ADPRT Val762Ala and XRCC1 Arg194Trp polymorphisms and risk of gastric cancer in Sichuan of China. Asian Pac J Cancer Prev. 2012;13:2139–44.
Duarte MC, Colombo J, Rossit AR, Caetano A, Borim AA, Wornrath D, et al. Polymorphisms of DNA repair genes XRCC1 and XRCC3, interaction with environmental exposure and risk of chronic gastritis and gastric cancer. World J Gastroenterol. 2005;11:6593–600.
Yan L, Yanan D, Donglan S, Na W, Rongmiao Z, Zhifeng C. Polymorphisms of XRCC1 gene and risk of gastric cardiac adenocarcinoma. Dis Esophagus. 2009;22:396–401.
Capellá G, Pera G, Sala N, Agudo A, Rico F, Del Giudicce G, et al. DNA repair polymorphisms and the risk of stomach adenocarcinoma and severe chronic gastritis in the EPIC-EURGAST study. Int J Epidemiol. 2008;37:1316–25.
Shen X, Zhang J, Yan Y, Yang Y, Fu G, Pu Y. Analysis and estimates of the attributable risk for environmental and genetic risk factors in gastric cancer in a Chinese population. J Toxicol Environ Health. 2009;72:759–66.
Lee SG, Kim B, Choi J, Kim C, Lee I, Song K. Genetic polymorphisms of XRCC1 and risk of gastric cancer. Cancer Lett. 2002;187:53–60.
Ganster C, Neesen J, Zehetmayer S, Jäger U, Esterbauer H, Mannhalter C, et al. DNA repair polymorphisms associated with cytogenetic subgroups in B-cell chronic lymphocytic leukemia. Genes Chromosome Cancer. 2009;48:760–7.
Huang WY, Gao YT, Rashid A, Sakoda LC, Deng J, Shen MC, et al. Selected base excision repair gene polymorphisms and susceptibility to biliary tract cancer and biliary stones: a population-based case–control study in China. Carcinogenesis. 2008;29:100–5.
Ho T, Li G, Lu J, Zhao C, Wei Q, Sturgis EM. X-ray repair cross-complementing group 1 (XRCC1) single-nucleotide polymorphisms and the risk of salivary gland carcinomas. Cancer. 2007;110:318–25.
Hirata H, Hinoda Y, Matsuyama H, Tanaka Y, Okayama N, Suehiro Y, et al. Polymorphisms of DNA repair genes are associated with renal cell carcinoma. Biochem Biophys Res Commun. 2006;342:1058–62.
Kumar A, Pant MC, Singh HS, Khandelwal S. Associated risk of XRCC1 and XPD cross talk and life style factors in progression of head and neck cancer in north Indian population. Mutat Res. 2012;729:24–34.
Liu Y, Scheurer ME, El-Zein R, Cao Y, Do KA, Gilbert M, et al. Association and interactions between DNA repair gene polymorphisms and adult glioma. Cancer Epidemiol Biomarkers Prev. 2009;18:204–14.
Baris S, Celkan T, Batar B, Guven M, Ozdil M, Ozkan A, et al. Association between genetic polymorphism in DNA repair genes and risk of B-cell lymphoma. Pediatr Hematol Oncol. 2009;26:467–72.
Csejtei A, Tibold A, Koltai K, Varga Z, Szanyi I, Gobel G, et al. Association between XRCC1 polymorphisms and head and neck cancer in a Hungarian population. Anticancer Res. 2009;29:4169–73.
Fard-Esfahani P, Fard-Esfahani A, Fayaz S, Ghanbarzadeh B, Saidi P, Mohabati R, et al. Association of Arg194Trp, Arg280His and Arg399Gln polymorphisms in X-ray repair cross-complementing group 1 gene and risk of differentiated thyroid carcinoma in Iran. Iran Biomed J. 2011;15:73–8.
Yuan T, Deng S, Chen M, Chen W, Lu W, Huang H, et al. Association of DNA repair gene XRCC1 and XPD polymorphisms with genetic susceptibility to gastric cancer in a Chinese population. Cancer Epidemiol. 2011;35:170–4.
Ho T, Li G, Lu J, Zhao C, Wei Q, Sturgis EM. Association of XRCC1 polymorphisms and risk of differentiated thyroid carcinoma: a case–control analysis. Thyroid. 2009;19:129–35.
Mittal RD, Mandal RK, Gangwar R. Base excision repair pathway genes polymorphism in prostate and bladder cancer risk in North Indian population. Mech Ageing Dev. 2012;133:127–32.
Fontana L, Bosviel R, Delort L, Guy L, Chalabi N, Kwiatkowski F, et al. DNA repair gene ERCC2, XPC, XRCC1, XRCC3 polymorphisms and associations with bladder cancer risk in a French cohort. Anticancer Res. 2008;28:1853–6.
Gugatschka M, Dehchamani D, Wascher TC, Friedrich G, Renner W. DNA repair gene ERCC2 polymorphisms and risk of squamous cell carcinoma of the head and neck. Exp Mol Pathol. 2011;91:331–4.
Batar B, Güven M, Bariş S, Celkan T, Yildiz I. DNA repair gene XPD and XRCC1 polymorphisms and the risk of childhood acute lymphoblastic leukemia. Leuk Res. 2009;33:759–63.
Joseph T, Kusumakumary P, Chacko P, Abraham A, Pillai MR. DNA repair gene XRCC1 polymorphisms in childhood acute lymphoblastic leukemia. Cancer Lett. 2005;217:17–24.
Liu J, Song B, Wang Z, Song X, Shi Y, Zheng J, et al. DNA repair gene XRCC1 polymorphisms and non-Hodgkin lymphoma risk in a Chinese population. Cancer Genet Cytogenet. 2009;191:67–72.
Kim IS, Kim DC, Kim HG, Eom HS, Kong SY, Shin HJ, et al. DNA repair gene XRCC1 polymorphisms and haplotypes in diffuse large B-cell lymphoma in a Korean population. Cancer Genet Cytogenet. 2010;196:31–7.
Pakakasama S, Sirirat T, Kanchanachumpol S, Udomsubpayakul U, Mahasirimongkol S, Kitpoka P, et al. Genetic polymorphisms and haplotypes of DNA repair genes in childhood acute lymphoblastic leukemia. Pediatr Blood Cancer. 2007;48:16–20.
Yin G, Morita M, Ohnaka K, Toyomura K, Hamajima N, Mizoue T, et al. Genetic polymorphisms of XRCC1, alcohol consumption, and the risk of colorectal cancer in Japan. J Epidemiol. 2012;22:64–71.
Settheetham-Ishida W, Yuenyao P, Natphopsuk S, Settheetham D, Ishida T. Genetic risk of DNA repair gene polymorphisms (XRCC1 and XRCC3) for high risk human papillomavirus negative cervical cancer in Northeast Thailand. Asian Pac J Cance Prev. 2011;12:963–6.
Han J, Hankinson SE, Colditz GA, Hunter DJ. Genetic variation in XRCC1, sun exposure, and risk of skin cancer. Br J Cancer. 2004;91:1604–9.
Harth V, Schafer M, Abel J, Maintz L, Neuhaus T, Besuden M, et al. Head and neck squamous-cell cancer and its association with polymorphic enzymes of xenobiotic metabolism and repair. J Toxicol Environ Health A. 2008;71:887–97.
Monroy CM, Cortes AC, Lopez M, Rourke E, Etzel CJ, Younes A, et al. Hodgkin lymphoma risk: role of genetic polymorphisms and gene–gene interactions in DNA repair pathways. Mol Carcinog. 2011;50:825–34.
Canalle R, Silveira VS, Scrideli CA, Queiroz RG, Lopes LF, Tone LG. Impact of thymidylate synthase promoter and DNA repair gene polymorphisms on susceptibility to childhood acute lymphoblastic leukemia. Leuk Lymphoma. 2011;52:1118–26.
Gonçalves FT, Francisco G, de Souza SP, Luiz OC, Festa-Neto C, Sanches JA, et al. European ancestry and polymorphisms in DNA repair genes modify the risk of melanoma: a case–control study in a high UV index region in Brazil. J Dermatol Sci. 2011;64:59–66.
Yu H, Fu C, Wang J, Xue H, Xu B. Interaction between XRCC1 polymorphisms and intake of long-term stored rice in the risk of esophageal squamous cell carcinoma: a case-control study. Biomed Environ Sci. 2011;24:268–74.
Duman N, Aktan M, Ozturk S, Palanduz S, Cakiris A, Ustek D, et al. Investigation of Arg399Gln and Arg194Trp polymorphisms of the XRCC1 (X-ray cross-complementing group 1) gene and its correlation to sister chromatid exchange frequency in patients with chronic lymphocytic leukemia. Genet Test Mol Biomark. 2012;16:287–91.
Muñiz-Mendoza R, Ayala-Madrigal ML, Partida-Pérez M, Peregrina-Sandoval J, Leal-Ugarte E, Macías-Gómez N, et al. MLH1 and XRCC1 polymorphisms in Mexican patients with colorectal cancer. Genet Mol Res. 2012;11:2315–20.
Gsur A, Bernhart K, Baierl A, Feik E, Führlinger G, Hofer P, et al. No association of XRCC1 polymorphisms Arg194Trp and Arg399Gln with colorectal cancer risk. Cancer Epidemiol. 2011;35:e38–41.
Kiran M, Saxena R, Chawla YK, Kaur J. Polymorphism of DNA repair gene XRCC1 and hepatitis-related hepatocellular carcinoma risk in Indian population. Mol Cell Biochem. 2009;327:7–13.
Santos LS, Branco SC, Silva SN, Azevedo AP, Gil OM, Manita I, et al. Polymorphisms in base excision repair genes and thyroid cancer risk. Oncol Rep. 2012;28:1859–68.
Brevik A, Joshi AD, Corral R, Onland-Moret NC, Siegmund KD, Le Marchand L, et al. Polymorphisms in base excision repair genes as colorectal cancer risk factors and modifiers of the effect of diets high in red meat. Cancer Epidemiol Biomarkers Prev. 2010;19:3167–73.
Dianzani I, Gibello L, Biava A, Giordano M, Bertolotti M, Betti M, et al. Polymorphisms in DNA repair genes as risk factors for asbestos-related malignant mesothelioma in a general population study. Mutat Res. 2006;599:124–34.
Shen M, Purdue MP, Kricker A, Lan Q, Grulich AE, Vajdic CM, et al. Polymorphisms in DNA repair genes and risk of non-Hodgkin's lymphoma in New South Wales. Aust Haematol. 2007;92:1180–5.
Zhou LQ, Ma Z, Shi XF, Yin XL, Huang KX, Jiu ZS, et al. Polymorphisms of DNA repair gene XRCC1 and risk of glioma: a case–control study in Southern China. Asian Pac J Cancer Prev. 2011;12:2547–50.
Sobczuk A, Poplawski T, Blasiak J. Polymorphisms of DNA repair genes in endometrial cancer. Pathol Oncol Res. 2012;18:1015–20.
Bianchino G, Cittadini A, Grieco V, Traficante A, Zupa A, Improta G, et al. Polymorphisms of the CYP1A1, CYP2E1 and XRCC1 genes and cancer risk in a Southern Italian population: a case–control study. Anticancer Res. 2011;31:1359–65.
Wang L, Lin DX, Lu XH, Miao XP, Li H. Polymorphisms of the DNA repair genes XRCC1 and XPC: relationship to pancreatic cancer risk. Wei Sheng Yan Jiu. 2006;35:534–6.
Srivastava A, Srivastava K, Pandey SN, Choudhuri G, Mittal B. Single-nucleotide polymorphisms of DNA repair genes OGG1 and XRCC1: association with gallbladder cancer in North Indian population. Ann Surg Oncol. 2009;16:1695–703.
Hsu LI, Chiu AW, Huan SK, Chen CL, Wang YH, Hsieh FI, et al. SNPs of GSTM1, T1, P1, epoxide hydrolase and DNA repair enzyme XRCC1 and risk of urinary transitional cell carcinoma in southwestern Taiwan. Toxicol Appl Pharmacol. 2008;228:144–55.
Han X, Xing Q, Li Y, Sun J, Ji H, Huazheng P, et al. Study on the DNA repair gene XRCC1 and XRCC3 polymorphism in prediction and prognosis of hepatocellular carcinoma risk. Hepatogastroenterology. 2012;59:2285–9.
Rydzanicz M, Wierzbicka M, Gajecka M, Szyfter W, Szyfter K. The impact of genetic factors on the incidence of multiple primary tumors (MPT) of the head and neck. Cancer Lett. 2005;224:263–78.
Huang J, Ye F, Chen H, Lu W, Xie X. The nonsynonymous single nucleotide polymorphisms of DNA repair gene XRCC1 and susceptibility to the development of cervical carcinoma and high-risk human papillomavirus infection. Int J Gynecol Cancer. 2007;17:668–75.
Smedby KE, Lindgren CM, Hjalgrim H, Humphreys K, Schöllkopf C, Chang ET, et al. Variation in DNA repair genes ERCC2, XRCC1, and XRCC3 and risk of follicular lymphoma. Cancer Epidemiol Biomarkers Prev. 2006;15:258–65.
Kiuru A, Lindholm C, Heinävaara S, Ilus T, Jokinen P, Haapasalo H, et al. XRCC1 and XRCC3 variants and risk of glioma and meningioma. J Neurooncol. 2008;88:135–42.
Chiyomaru K, Nagano T, Nishigori C. XRCC1 Arg194Trp polymorphism, risk of nonmelanoma skin cancer and extramammary Paget's disease in a Japanese population. Arch Dermatol Res. 2012;304:363–70.
Mittal RD, Singh R, Manchanda PK, Ahirwar D, Gangwar R, Kesarwani P, et al. XRCC1 codon 399 mutant allele: a risk factor for recurrence of urothelial bladder carcinoma in patients on BCG immunotherapy. Cancer Biol Ther. 2008;7:645–50.
Wang N, Wu Y, Zhou X, Wu Y. Association between genetic polymorphism of metabolizing enzymes and DNA repairing enzymes and the susceptibility of lung cancer in Henan population. Wei Sheng Yan Jiu. 2012;41:251–6.
Meza-Espinoza JP, Peralta-Leal V, Gutierrez-Angulo M, Macias-Gomez N, Ayala-Madrigal ML, Barros-Nuñez P, et al. XRCC1 polymorphisms and haplotypes in Mexican patients with acute lymphoblastic leukemia. Genet Mol Res. 2009;8:1451–8.
Ryu RA, Tae K, Min HJ, Jeong JH, Cho SH, Lee SH, et al. XRCC1 polymorphisms and risk of papillary thyroid carcinoma in a Korean sample. J Korean Med Sci. 2011;26:991–5.
Gao R, Price DK, Dahut WL, Reed E, Figg WD. Genetic polymorphisms in XRCC1 associated with radiation therapy in prostate cancer. Cancer Biol Ther. 2010;10:13–8.
Tumer TB, Yilmaz D, Tanrikut C, Sahin G, Ulusoy G, Arinç E. DNA repair XRCC1 Arg399Gln polymorphism alone, and in combination with CYP2E1 polymorphisms significantly contribute to the risk of development of childhood acute lymphoblastic leukemia. Leuk Res. 2010;34:1275–81.
Zhu R, Lu FJ, Zhang ZB, Zhai XW, Liu J, Lu G, et al. Association of genetic polymorphism of XRCC1 with susceptibility to acute childhood leukemia. Wei Sheng Yan Jiu. 2005;34:300–2.
Barbisan G, Pérez LO, Difranza L, Fernández CJ, Ciancio NE, Golijow CD. XRCC1 Arg399Gln polymorphism and risk for cervical cancer development in Argentine women. Eur J Gynaecol Oncol. 2011;32:274–9.
Romanowicz-Makowska H, Smolarz B, Kulig A. Polymorphisms in XRCC1 and ERCC4/XPF DNA repair genes and associations with breast cancer risk in women. Pol Merkur Lekarski. 2007;22:200–3.
Seedhouse C, Bainton R, Lewis M, Harding A, Russell N, Das-Gupta E. The genotype distribution of the XRCC1 gene indicates a role for base excision repair in the development of therapy-related acute myeloblastic leukemia. Blood. 2002;100:3761–6.
Matullo G, Dunning AM, Guarrera S, Baynes C, Polidoro S, Garte S, et al. DNA repair polymorphisms and cancer risk in non-smokers in a cohort study. Carcinogenesis. 2006;27:997–1007.
Gajecka M, Rydzanicz M, Jaskula-Sztul R, Wierzbicka M, Szyfter W, Szyfter K. Reduced DNA repair capacity in laryngeal cancer subjects. A comparison of phenotypic and genotypic results. Adv Otorhinolaryngol. 2005;62:25–37.
Laantri N, Jalbout M, Khyatti M, Ayoub WB, Dahmoul S, Ayad M, et al. XRCC1 and hOGG1 genes and risk of nasopharyngeal carcinoma in North African Countries. Mol Carcinog. 2011;50:732–7.
Mandal RK, Gangwar R, Mandhani A, Mittal RD. DNA repair gene X-ray repair cross-complementing group 1 and xeroderma pigmentosum group D polymorphisms and risk of prostate cancer: a study from North India. DNA Cell Biol. 2010;29:183–90.
Yin JY, Vogel U, Gerdes LU, Dybdahl M, Bolund L, Nexø BA. Twelve single nucleotide polymorphisms on chromosome 19q13.2-13.3: Linkage disequilibria and associations with basal cell carcinoma in Danish psoriatic patients. Biochem Genet. 2003;41:27–37.
Farkasova T, Gurska S, Witkovsky V, Gabelova A. Significance of amino acid substitution variants of DNA repair genes in radiosusceptibility of cervical cancer patients; a pilot study. Neoplasma. 2008;55:330–7.
Chang JS, Wrensch MR, Hansen HM, Sison JD, Aldrich MC, Quesenberry Jr CP, et al. Base excision repair genes and risk of lung cancer among San Francisco Bay Area Latinos and African-Americans. Carcinogenesis. 2009;30:78–87.
Celkan T, Güven M, Batar B, Alhaj S. The diff erence between pre-B cell acute lymphoblastic leukemia and Burkitt lymphoma in relation to DNA damage repair gene polymorphisms in childhood. Leuk Lymphoma. 2008;49:1638–40.
Custódio AC, Almeida LO, Pinto GR, Santos MJ, Almeida JR, Clara CA, et al. Analysis of the polymorphisms XRCC1Arg194Trp and XRCC1Arg399Gln in gliomas. Genet Mol Res. 2011;10:1120–9.
Rajaraman P, Melin BS, Wang Z, McKean-Cowdin R, Michaud DS, Wang SS, et al. Genome-wide association study of glioma and meta-analysis. Hum Genet. 2012;131:1877–88.
Hu XB, Feng Z, Fan YC, Xiong ZY, Huang QW. Polymorphisms in DNA repair gene XRCC1 and increased genetic susceptibility to glioma. Asian Pac J Cancer Prev. 2011;12:2981–4.
McKean-Cowdin R, Barnholtz-Sloan J, Inskip PD, Ruder AM, Butler M, Rajaraman P, et al. Associations between polymorphisms in DNA repair genes and glioblastoma. Cancer Epidemiol Biomarkers Prev. 2009;18:1118–26.
Wang D, Hu Y, Gong H, Li J, Ren Y, et al. Genetic polymorphisms in the DNA repair gene XRCC1 and susceptibility to glioma in a Han population in northeastern China: a case–control study. Gene. 2012;509:223–7.
Liu HB, Peng YP, Dou CW, Su XL, Gao NK, Tian FM, et al. Comprehensive study on associations between nine SNPs and glioma risk. Asian Pac J Cancer Prev. 2012;13:4905–8.
Pardini B, Naccarati A, Novotny J, et al. DNA repair genetic polymorphisms and risk of colorectal cancer in the Czech Republic. Mutat Res. 2008;638:146–53.
Li Y, Li S, Wu Z, Hu F, Zhu L, Zhao X, et al. Polymorphisms in genes of APE1, PARP1, and XRCC1: risk and prognosis of colorectal cancer in a northeast Chinese population. Med Oncol. 2013;30:505.
Huang M, Dinney CP, Lin X, Lin J, Grossman HB, Wu X. High-order interactions among genetic variants in DNA base excision repair pathway genes and smoking in bladder cancer susceptibility. Cancer Epidemiol Biomarkers Prev. 2007;16:84–91.
Buch SC, Diergaarde B, Nukui T, Day RS, Siegfried JM, Romkes M, et al. Genetic variability in DNA repair and cell cycle control pathway genes and risk of smoking-related lung cancer. Mol Carcinog. 2012;51:E11–20.
Guo S, Li X, Gao M, Li Y, Song B, Niu W. The relationship between XRCC1 and XRCC3 gene polymorphisms and lung cancer risk in northeastern Chinese. PLoS ONE. 2013;8:e56213.
Zhu QX, Bian JC, Shen Q, et al. Genetic polymorphisms in X-ray repair cross-complementing gene 1 and susceptibility to papillary thyroid carcinoma. Zhonghua Liu Xing Bing Xue Za Zhi. 2004;25:702–5.
Sigurdson AJ, Land CE, Bhatti P, Pineda M, Brenner A, Carr Z, et al. Thyroid nodules, polymorphic variants in DNA repair and RET-related genes, and interaction with ionizing radiation exposure from nuclear tests in Kazakhstan. Radiat Res. 2009;171:77–88.
Dos Reis MB, Losi-Guembarovski R, de Souza Fonseca Ribeiro EM, Cavalli IJ, Morita MC, et al. Allelic variants of XRCC1 and XRCC3 repair genes and susceptibility of oral cancer in Brazilian patients. J Oral Pathol Med. 2013;42:180–5.
Mahimkar MB, Samant TA, Kannan S, Patil T. Influence of genetic polymorphisms on frequency of micronucleated buccal epithelial cells in leukoplakia patients. Oral Oncol. 2010;46:761–6.
Annamaneni S, Gorre M, Kagita S, Addepalli K, Digumarti RR, Satti V, et al. Association of XRCC1 gene polymorphisms with chronic myeloid leukemia in the population of Andhra Pradesh, India. Hematology. 2013;18:163–8.
Banescu C, Duicu C, Trifa AP, Dobreanu M. XRCC1 Arg194Trp and Arg399Gln polymorphisms are significantly associated with shorter survival in acute myeloid leukemia. Leuk Lymphoma. 2014;55:365–70.
Kim HN, Kim NY, Yu L, Tran HT, Kim YK, Lee IK, et al. Association of GSTT1 polymorphism with acute myeloid leukemia risk is dependent on smoking status. Leuk Lymphoma. 2012;53:681–7.
Shi JY, Ren ZH, Jiao B, Xiao R, Yun HY, Chen B, et al. Genetic variations of DNA repair genes and their prognostic significance in patients with acute myeloid leukemia. Int J Cancer J Int du Cancer. 2011;128:233–8.
Zhu R, Wu Y, Lu FJ, Wang AH, Tang JY, Zhao JC, et al. Polymorphisms and haplotypes of XRCC1 and APE1 and risk of childhood leukaemia in China: a case-control analysis. Eur J Oncol. 2008;13:187–92.
Luo KQ, Mu SQ, Wu ZX, Shi YN, Peng JC. Polymorphisms in DNA repair genes and risk of glioma and meningioma. Asian Pac J Cancer Prev. 2013;14:449–52.
Pan XF, Xie Y, Loh M, Yang SJ, Wen YY, Tian Z, et al. Polymorphisms of XRCC1 and ADPRT genes and risk of noncardia gastric cancer in a Chinese population: a case–control study. Asian Pac J Cancer Prev. 2012;13:5637–42.
Pan WR, Li G, Guan JH. Polymorphisms in DNA repair genes and susceptibility to glioma in a Chinese population. Int J Mol Sci. 2013;14:3314–24.
Dai L, Duan F, Wang P, Song C, Wang K, Zhang J. XRCC1 gene polymorphisms and lung cancer susceptibility: a meta-analysis of 44 case–control studies. Mol Biol Rep. 2012;39:9535–47.
Jiang L, Fang X, Bao Y, Zhou JY, Shen XY, Ding MH, et al. Association between the XRCC1 polymorphisms and glioma risk: a meta-analysis of case–control studies. PLoS ONE. 2013;8:e55597.
Wang L, Yin F, Xu X, Hu X, Zhao D. X-ray repair cross-complementing group 1 (XRCC1) genetic polymorphisms and risk of childhood acute lymphoblastic leukemia: a meta-analysis. PLoS ONE. 2012;7:e34897.
Davey SG, Egger M. Meta-analyses of randomized controlled trials. Lancet. 1997;350:1182.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analysis. Br Med J. 2003;327:557–60.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. Natl Cancer Inst. 1959;22:719–48.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Klug SJ, Ressing M, Koenig J, Abba MC, Agorastos T, Brenna SM, et al. TP53 codon 72 polymorphism and cervical cancer: a pooled analysis of individual data from 49 studies. Lancet Oncol. 2009;10:772–84.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Egger M, Smith DG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. 1997;315:629–34.
Caldecott KW, Aoufouchi S, Johnson P, Shall S. XRCC1 polypeptide interacts with DNA polymerase beta and possiblypoly (ADP-ribose) polymerase, and DNA ligase III is a novelmolecular “nick-sensor” in vitro. Nucleic Acids Res. 1996;24:4387–94.
Kubota Y, Nash RA, Klungland A, Schar P, Barnes DE, Lindahl T. Reconstitution of DNA base excision-repair withpurified human proteins: interaction between DNA polymerasebeta and the XRCC1 protein. Eur Mol Biol Org J. 1996;15:6662–70.
Cappelli E, Taylor R, Cevasco M, Abbondandolo A, Caldecott K, Frosina G. Involvement of XRCC1 and DNA ligase III gene products in DNA base excision repair. J Biol Chem. 1997;272:23970–5.
Chen D, Yu Z, Zhu Z, Lopez CD. E2F1 regulates the base excision repair gene XRCC1 and promotes DNA repair. J Biol Chem. 2008;283:15381–9.
Tebbs RS, Flannery ML, Meneses JJ, Hartmann A, Tucker JD, Thompson LH, et al. Requirement for the Xrcc1 DNA base excision repair gene during early mouse development. Dev Biol. 1999;208:513–29.
Moore DJ, Taylor RM, Clements P, Caldecott KW. Mutation of a BRCT domain selectively disrupts DNA singlestrand break repair in noncycling Chinese hamster ovary cells. Proc Natl Acad Sci U S A. 2000;97:13649–54.
Wang Y, Yang H, Li H, Li L, Wang H, Liu C, et al. Association between X-ray repair cross complementing group 1 codon 399 and 194 polymorphisms and lung cancer risk: a meta-analysis. Cancer Lett. 2009;285:134–40.
Chen B, Zhou Y, Yang P, Wu XT. Polymorphisms of XRCC1 and gastric cancer susceptibility: a meta-analysis. Mol Biol Rep. 2012;39:1305–13.
Wang B, Wang D, Huang G, Zhang C, Xu DH, Zhou W. XRCC1 polymorphisms and risk of colorectal cancer: a meta-analysis. Int J Colorectal Dis. 2010;25:313–21.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Yan-Zhong Feng and Yi-Ling Liu contributed equally to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 479 kb)
Rights and permissions
About this article
Cite this article
Feng, YZ., Liu, YL., He, XF. et al. Association between the XRCC1 Arg194Trp polymorphism and risk of cancer: evidence from 201 case–control studies. Tumor Biol. 35, 10677–10697 (2014). https://doi.org/10.1007/s13277-014-2326-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-2326-x