Abstract
Cancer neovascularization plays a key role in the metastasis of larynx carcinoma. However, the molecular mechanism for the neovascularization control in larynx carcinoma is poorly understood. Since placental growth factor (PLGF) has been reported to be involved in pathological angiogenesis, and since matrix metalloproteinases (MMPs) are essential for extracellular matrix degradation during neovascularization, here we were prompted to examine whether PLGF and MMPs may play a coordinate role in the metastasis of larynx carcinoma. Our data showed that the expression of PLGF and MMP3 strongly correlated in the larynx carcinoma in the patients, and significant higher levels of PLGF and MMP3 were detected in the larynx carcinoma from the patients with metastasis of the primary cancer. Thus, we used a human larynx carcinoma cell line, Hep-2, to examine whether expression of PLGF and MMP3 may affect each other. We found that overexpression of PLGF in Hep-2 cells increased expression of MMP3, while inhibition of PLGF in Hep-2 cells decreased expression of MMP3. However, neither overexpression, nor inhibition of MMP3 in Hep-2 cells affected the expression level of PLGF. These data suggest that PLGF may function upstream of MMP3 in larynx carcinoma cells. We then analyzed how PLGF affected MMP3. Application of a specific ERK1/2 inhibitor to PLGF-overexpressing Hep-2 cells substantially abolished the effect of PLGF on MMP3 activation, suggesting that PLGF may increase expression of MMP3 via ERK/MAPK signaling pathway. Since anti-PLGF was recently applied in clinical trials to inhibit cancer-related angiogenesis, here our data further demonstrate that inhibition of cancer neovascularization by anti-PLGF is mediated not only by direct effect on endothelial growth and capillary permeability, but also by indirect effect via MMP3 on the extracellular matrix degradation in larynx carcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The larynx carcinoma in the diagnosed patients has often reached advanced stages with metastasis, resulting in a rather low 5-year survival [1]. It may largely result from that larynx carcinoma is often asymptomatic or non-specifically symptomatic in its early stages. Therefore, understanding the molecular basis of the metastasis of larynx carcinoma appears substantially critical for improving the therapy of larynx carcinoma.
Cancer-related angiogenesis plays an essential role in invasion and metastasis of various cancers, including larynx carcinoma [2–4], by providing oxygen and nutrients to tumor and a channel for its hematogenous metastasis. Cancer cells often secrete proteinases or acquire proteinase activity from host stromal cells or inflammatory cells to allow cancer cells to break through protein barriers in the extracellular matrix [5]. Vascular endothelial growth factor (VEGF) family is the most important signal protein produced by cells that stimulates vasculogenesis and angiogenesis [6]. The VEGF family is composed of six secreted proteins: VEGFa, VEGFb, VEGFc, VEGFd, VEGFe, and placental growth factor (PLGF) [7, 8]. PLGF may play an important role in the pathological angiogenesis, in a coordinated way with other VEGF family members. However, the exact effect of PLGF on cancer neovascularization may be case-dependent. For example, PLGF produced by tumor and host cells has been reported to promote angiogenesis and tumor growth [9], or inhibit tumor angiogenesis by forming inactive VEGF/PLGF heterodimer [10].
The matrix metalloproteinase (MMP) family members are involved in the breakdown of extracellular matrix in normal physiological processes, such as embryonic development, reproduction, and tissue remodeling, as well as in disease processes, such as arthritis and metastasis [11, 12]. MMP3 is a member of the MMP family. MMP3 is an important matrix proteinase that is secreted by various cancer cells to break down extracellular matrix. Overexpression of MMP3 has been reported to facilitate metastatic spread of different cancer cells and appears to be an important molecule to directly promote cancer metastasis [13, 14]. Nevertheless, whether MMP3 may be activated in larynx carcinoma cells and its possible crosstalk with PLGF have not been examined before.
Here, we reported that the expression of PLGF and MMP3 strong correlated in the larynx carcinoma in the patients, and significant higher levels of PLGF and MMP3 were detected in the larynx carcinoma from the patients with metastasis of the primary cancer. Thus, we used a human larynx carcinoma cell line, Hep-2, to examine whether expression of PLGF and MMP3 may affect each other. We found that overexpression of PLGF in Hep-2 cells increased expression of MMP3, while inhibition of PLGF in Hep-2 cells decreased expression of MMP3. However, neither overexpression, nor inhibition of MMP3 in Hep-2 cells affected the expression level of PLGF. These data suggest that PLGF may function upstream of MMP3 in larynx carcinoma cells. We then analyzed how PLGF affected MMP3. Application of a specific extracellular single-regulated kinase (ERK)1/2 inhibitor to PLGF-overexpressing Hep-2 cells substantially abolished the effect of PLGF on MMP3 activation, suggesting that PLGF may increase expression of MMP3 via ERK/mitogen activated protein kinase (MAPK) signaling pathway. Since anti-PLGF was recently applied in clinical trials to inhibit cancer-related angiogenesis, here our data further demonstrate that inhibition of cancer neovascularization by anti-PLGF is mediated not only by direct effect on endothelial growth and capillary permeability, but also by indirect effect via MMP3 on the extracellular matrix degradation in larynx carcinoma.
Materials and methods
Cell lines and reagents
PD98059 is a human larynx carcinoma line purchased from ATCC, and was cultured in Dulbecco’s modified Eagle’s media (DMEM) supplemented with 15 % fetal bovine serum (Invitrogen, Carlsbad, CA, USA). Inhibitors PD98059, LY294002, and SP600125 were purchased from Sigma (USA).
Patient tissue specimens
A total of 43 resected specimens from larynx carcinoma patients were collected for this study. All specimens had been histologically and clinically diagnosed at the Otorhinolaryngology Department of Zhongshan Hospital of Fudan University from 2007 to 2014. For the use of these clinical materials for research purposes, prior patient’s consents and approval from the Institutional Research Ethics Committee were obtained.
Transfection with constitutively nuclear FoxO1 and selection of positive cells
Hep-2 cells were transfected with a PLGF-overexpressing plasmid (PLGF), or a small short hairpin interfering RNA for PLGF (shPLGF), or MMP3-overexpressing plasmid, or a small short hairpin interfering RNA for MMP3 (shMMP3), as has been previously described [15].
Transwell matrix penetration assay
5X105 cells were plated into the top side of polycarbonate Transwell filter coated with Matrigel in the upper chamber of the BioCoatTM Invasion Chambers (BD, Bedford, MA, USA) and incubated at 37 °C for 22 h. The cells inside the upper chamber with cotton swabs were then removed. Migratory and invasive cells on the lower membrane surface were fixed, stained with hematoxylin, and counted for 10 random ×100 fields per well. Cell counts are expressed as the mean number of cells per field of view. Five independent experiments were performed, and the data are presented as mean ± standard deviation (SD).
ELISA assay
The concentration of MMP3 in the conditioned media from cultured cells was determined by an MMP3 ELISA Kit (Sigma, USA). The concentration of PLGF in the cultured cells was determined by a PLGF ELISA kit (Raybio, USA). ELISAs were performed according to the instructions of the manufacturer. Briefly, the collected condition media was added to a well coated with MMP3/PLGF polyclonal antibody, and then immunosorbented by biotinylated monoclonal anti-human MMP3/PLGF antibody at room temperature for 2 h. The color development catalyzed by horseradish peroxidase was terminated with 2.5 mol/l sulfuric acid, and the absorption was measured at 450 nm. The protein concentration was determined by comparing the relative absorbance of the samples with the standards.
Western blot
The protein was extracted from the resected larynx carcinoma from the patient specimen, or from cultured Hep-2 cells. Primary antibodies were anti-PLGF (Santa Cruz, USA), anti-MMP3, and anti-β-actin (Cell Signaling, USA). β-actin was used as a protein loading control.
RT-qPCR
RNA was extracted from cultured cells with RNAeasy kit (Qiagen, Hilden, Germany) and used for cDNA synthesis. Quantitative PCR (RT-qPCR) were performed in duplicates with QuantiTect SYBR Green PCR Kit (Qiagen). All primers were purchased from Qiagen. Values of genes were normalized against β-actin and then compared with control (=1).
Statistical analysis
All statistical analyses were carried out using the SPSS 17.0 statistical software package. All data were statistically analyzed using one-way ANOVA with a Bonferoni Correction. Bivariate correlations between PLGF and MMP3 levels were calculated by Spearman’s Rank Correlation Coefficients. All values are depicted as mean ± standard deviation from five individuals and are considered significant if p < 0.05.
Results
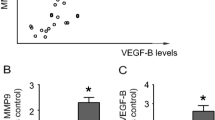
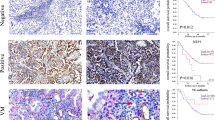
PLGF and MMP3 levels strongly correlated each other and metastasis in the larynx carcinoma patients
Since MMPs are closely related to tumor invasiveness, we thus examined the different levels of MMPs in larynx carcinoma from the patients by Western blot. Among all MMPs that have been examined, we found that MMP3 appeared to express in high level (not shown). Since both PLGF and MMP3 are essential for neovascularization, we would like to detect whether there is a causative link between PLGF and MMP3 in larynx carcinoma. Thus, we compared the PLGF and MMP3 levels in the resected larynx carcinoma from the patients. We found a strong positive correlation of PLGF and MMP3 levels in these patients (Fig. 1a, R 2 = 0.46, p < 0.001). Moreover, patients who had metastasis of the primary larynx carcinoma expressed significantly higher levels of MMP3 (Fig. 1b) and PLGF (Fig. 1c). These data suggest that expression of PLGF and MMP3 in larynx carcinoma strongly correlated with metastasis.
PLGF and MMP3 levels positively correlated each other, and with the metastasis in larynx carcinoma patients. a PLGF and MMP3 levels were measured by Western blot in the resected larynx carcinoma tissue from 25 patients. A strong correlation was detected (ɤ2 = 0.46; P < 0.001. b–c Patients who had metastasis of the primary larynx carcinoma had significantly higher levels of MMP3 (b) and PLGF (c). *p < 0.05
PLGF-regulated MMP3 expression in Hep-2 cells
Then, we used a human larynx carcinoma cell line, Hep-2, to examine whether expression of PLGF and MMP3 may affect each other. We transfected the Hep-2 cells with either a PLGF expressing plasmid (transgene PLGF or PLGF), or a small short hairpin interfering RNA for PLGF (shPLGF). We found that overexpression of PLGF in Hep-2 cells increased MMP3 expression, while inhibition of PLGF in Hep-2 cells decreased MMP3 expression, by mRNA (Fig. 2a), by Western blot for protein (Fig. 2b), or by ELISA on the conditioned media (Fig. 2c). These data suggest that the MMP3 levels were positively regulated by PLGF levels in larynx carcinoma cells. Next, we examined the invasion ability of the Hep-2 cells in a transwell matrix penetration assay. We found that PLGF overexpression significantly increased the invasiveness of Hep-2 cells, while inhibition of PLGF in Hep-2 cells significantly decreased the invasiveness of Hep-2 cells (Fig. 2d).
PLGF regulated MMP3 expression in Hep-2 cells. a–c A human larynx carcinoma cell line, Hep-2, was transfected with either a PLGF expressing plasmid (PLGF), or shPLGF. Overexpression of PLGF in Hep-2 cells increased expression of MMP3, while inhibition of PLGF in Hep-2 cells decreased expression of MMP3, by mRNA (a), by Western blot (b), or by ELISA on the conditioned media (c). d The invasion ability of the Hep-2 cells in a transwell matrix penetration assay. *p < 0.05
PLGF was not regulated by MMP3
On the other hand, we aimed to examine whether MMP3 may similarly affect the PLGF levels in Hep-2 cells. Therefore, we transfected the Hep-2 cells with either an MMP3 expressing plasmid (transgene MMP3 or MMP3), or a small short hairpin interfering RNA for MMP3 (shMMP3). We found that neither overexpression nor inhibition of MMP3 in Hep-2 cells changed the levels of PLGF, by mRNA (Fig. 3a), by Western blot (Fig. 3b), or by ELISA on the conditioned media (Fig. 3c) or on cultured cells (not shown), suggesting that PLGF was not regulated by MMP3. Next, we examined the invasion ability of the Hep-2 cells in a transwell matrix penetration assay. We found that MMP3 overexpression significantly increased the invasiveness of Hep-2 cells, while inhibition of MMP3 in Hep-2 cells decreased it significantly (Fig. 3d). This adaptation of Hep-2 invasiveness apparently resulted from the levels of MMP3 itself.
PLGF was not regulated by MMP3. a–c Hep-2 was transfected with either an MMP3 expressing plasmid (MMP3), or shMMP3. Neither overexpression nor inhibition of MMP3 in Hep-2 cells changed the levels of PLGF, by mRNA (a), by Western blot (b), or by ELISA on the conditioned media (c). d The invasion ability of the Hep-2 cells in a transwell matrix penetration assay. *p < 0.05
PLGF controlled expression of MMP3 via ERK/MAPK signaling pathway
We then analyzed the signaling pathway through which PLGF affects MMP3 levels. Application of a specific ERK/MAPK signaling pathway inhibitor, PD98059 (10 μmol/l), but not the application of a specific PI3k/Akt signaling pathway inhibitor, LY294002 (20 μmol/l), or a specific JNK pathway inhibitor, SP600125 (10 μmol/l), to PLGF-overexpressing Hep-2 cells substantially abolished the effect of PLGF on MMP3 activation, by mRNA (Fig. 4a), by Western blot (Fig. 4b), or by ELISA on the conditioned media (Fig. 4c). Moreover, in a transwell matrix penetration assay, application of only PD98059 significantly decreased the increase in the invasiveness of Hep-2 cells by PLGF overexpression (Fig. 4d). These data suggest that PLGF may increase expression of MMP3 via ERK/MAPK signaling pathway. Taken together, our data suggest that anti-PLGF therapy in larynx carcinoma may inhibit neovascularization by abolishing the direct effect of PLGF on endothelial mitogenesis and capillary permeability, and by abolishing the effect of MMP3 on extracellular matrix degradation.
PLGF controlled expression of MMP3 via ERK/MAPK signaling pathway. a–c Application of a specific ERK/MAPK signaling pathway inhibitor, PD98059 (10 μmol/l), but not application of a specific PI3k/Akt signaling pathway inhibitor, LY294002 (20 μmol/l), or a specific JNK pathway inhibitor, SP600125 (10 μmol/l), to PLGF-overexpressing Hep-2 cells substantially abolished the effect of PLGF on MMP3 activation, by mRNA level (a), by Western blot (b), and by ELISA on conditioned media (c). d Application of only PD98059 significantly decreased the increase in the invasiveness of Hep-2 cells by PLGF overexpression in a transwell matrix penetration assay. *p < 0.05
Discussion
Understanding the molecular basis on the cancer metastasis may substantially improve the prevention and treatment of larynx carcinoma. Angiogenesis is one of the most important process by which larynx carcinoma invade and migrate. Tumor cells not only secrete angiogenetic molecules like PLGF to increase capillary permeability and promote endothelial cell proliferation and survival, but also secrete MMPs to degrade extracellular matrix [16]. All these events are critical for cancer angiogenesis and metastasis. MMP3 is a member of the MMP family. Nevertheless, whether PLGF and MMP3 may play a role in the metastasis of larynx carcinoma has not been examined.
Here, we found strong correlation of PLGF and MMP3 levels in the larynx carcinoma in the patients. Moreover, significant higher levels of PLGF and MMP3 were detected in the larynx carcinoma from the patients with metastasis of the primary cancer. These data suggest a possible relationship between PLGF and MMP3 during metastasis of larynx carcinoma. To prove this hypothesis, we used a human larynx carcinoma cell line, Hep-2, to examine the interaction of PLGF and MMP3. We found that overexpression of PLGF in Hep-2 cells increased expression of MMP3, while inhibition of PLGF in Hep-2 cells decreased expression of MMP3. However, neither overexpression, nor inhibition of MMP3 in Hep-2 cells affected expression of PLGF. These data suggest that PLGF may function upstream of MMP3 in larynx carcinoma cells. We then analyzed how PLGF may affect the expression of MMP3. Application of a specific ERK1/2 inhibitor to PLGF-overexpressing Hep-2 cells substantially abolished the effect of PLGF on MMP3 activation, suggesting that PLGF may increase expression of MMP3 via ERK/MAPK signaling pathway. Anti-PLGF was recently applied in the clinical trials targeting cancer-related angiogenesis, but the mechanism has been regarded as inhibition of endothelial growth and capillary permeability in the cancer tissue. Now our data suggest that anti-PLGF may also decrease MMP3 expression to impair the extracellular matrix degradation, at least in larynx carcinoma.
Our study thus illustrates a novel model of the molecular mechanism underlying the angiogenesis and invasiveness of larynx carcinoma. Further delineation of the precise molecular mechanism that mediates the regulation of MMP3 by PLGF may substantially improve our understanding of the controls for metastasis of larynx carcinoma.
References
Zhao X, Li X, Yuan H. MicroRNAs in gastric cancer invasion and metastasis. Front Biosci. 2013;18:803–10.
Kim JG. Molecular targeted therapy for advanced gastric cancer. Korean J Intern Med. 2013;28:149–55.
Ilson DH. Angiogenesis in gastric cancer: hitting the target? Lancet. 2014;383:4–6.
Scartozzi M, Giampieri R, Loretelli C, Bittoni A, Mandolesi A, Faloppi L, et al. Tumor angiogenesis genotyping and efficacy of first-line chemotherapy in metastatic gastric cancer patients. Pharmacogenomics. 2013;14:1991–8.
Dufour A, Overall CM. Missing the target: matrix metalloproteinase antitargets in inflammation and cancer. Trends Pharmacol Sci. 2013;34:233–42.
Ferrara N. Vascular endothelial growth factor. Arterioscler Thromb Vasc Biol. 2009;29:789–91.
Xiao X, Prasadan K, Guo P, El-Gohary Y, Fischbach S, Wiersch J, et al. Pancreatic duct cells as a source of VEGF in mice. Diabetologia. 2014;57:991–1000.
Xiao X, Guo P, Chen Z, El-Gohary Y, Wiersch J, Gaffar I, et al. Hypoglycemia reduces vascular endothelial growth factor a production by pancreatic beta cells as a regulator of beta cell mass. J Biol Chem. 2013;288:8636–46.
Carmeliet P, Moons L, Luttun A, Vincenti V, Compernolle V, De Mol M, et al. Synergism between vascular endothelial growth factor and placental growth factor contributes to angiogenesis and plasma extravasation in pathological conditions. Nat Med. 2001;7:575–83.
Eriksson A, Cao R, Pawliuk R, Berg SM, Tsang M, Zhou D, et al. Placenta growth factor-1 antagonizes VEGF-induced angiogenesis and tumor growth by the formation of functionally inactive PLGF-1/VEGF heterodimers. Cancer Cell. 2002;1:99–108.
Davidson B, Reich R, Risberg B, Nesland JM. The biological role and regulation of matrix metalloproteinases (mmp) in cancer. Arkh Patol. 2002;64:47–53.
Rhee JS, Coussens LM. Recking mmp function: implications for cancer development. Trends Cell Biol. 2002;12:209–11.
Zhang C, Li C, Zhu M, Zhang Q, Xie Z, Niu G, et al. Meta-analysis of mmp2, mmp3, and mmp9 promoter polymorphisms and head and neck cancer risk. PLoS ONE. 2013;8:e62023.
Mendes O, Kim HT, Stoica G. Expression of mmp2, mmp9 and mmp3 in breast cancer brain metastasis in a rat model. Clin Exp Metastasis. 2005;22:237–46.
Biggs 3rd WH, Meisenhelder J, Hunter T, Cavenee WK, Arden KC. Protein kinase B/Akt-mediated phosphorylation promotes nuclear exclusion of the winged helix transcription factor FKHR1. Proc Natl Acad Sci U S A. 1999;96:7421–6.
Bagri A, Kouros-Mehr H, Leong KG, Plowman GD. Use of anti-VEGF adjuvant therapy in cancer: challenges and rationale. Trends Mol Med. 2010;16:122–32.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
The Publisher and Editor retract this article in accordance with the recommendations of the Committee on Publication Ethics (COPE). After a thorough investigation we have strong reason to believe that the peer review process was compromised.
An erratum to this article can be found online at http://dx.doi.org/10.1007/s13277-017-5487-6.
About this article
Cite this article
Zhou, X., Qi, Y. RETRACTED ARTICLE: PLGF inhibition impairs metastasis of larynx carcinoma through MMP3 downregulation. Tumor Biol. 35, 9381–9386 (2014). https://doi.org/10.1007/s13277-014-2232-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-2232-2