Abstract
Osteosarcoma is the most malignant bone tumor characterized by high local aggressiveness and poor therapeutic outcome. Tumor-associated macrophages (TAM) have been shown to participate in the development and progress of many types of cancer cells. However, whether TAM may play a role in the pathogenesis of osteosarcoma is largely unknown. In a mouse model of human osteosarcoma implantation, we showed that the recruited macrophages at the site of the implanted tumor were polarized to an M2 subtype (same as TAM) during the development and growth of the osteosarcoma. In a loss-of-function experiment, we deleted these TAM with a specific macrophage-eliminating liposome, which resulted in decreased tumor growth. Moreover, when the epidermal growth factor receptor (EGFR) in the implanted cancer cells was inhibited by shRNA, the tumor failed to grow in response to the recruited macrophages. Taken together, for the first time, we show that the growth of an osteosarcoma is EGFR signaling-dependent and TAM-mediated. Our data suggest that TAM and EGFR may be good targets for treating human osteosarcoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An osteosarcoma (OS) is highly locally aggressive and rapidly metastasizing, resulting in an early onset tumor with poor survival [1]. OS is highly histologically heterogenic, suggesting an origin of mesenchymal stem cells, along their path of differentiation to the OS lineage [2]. OS is the most common primary bone tumor in the pediatric age group. Treatment-refractory pulmonary metastasis continues to be the major complication of OS, reducing the 5-year survival rate for these patients to 10–20 % [2]. The mechanisms underlying the metastatic process in OS are still unclear. A greater understanding of the factors and interactions involved in its regulation will open new and much-needed opportunities for therapeutic intervention. Therefore, there is an urgent need for studying the tumor biology in order to increase our comprehension and to treat it efficiently [1, 3, 4]. A number of human OS cell lines have been established, among which the U2OS [5] cell line has been extensively characterized and widely used for OS research.
Macrophages have been suggested to play a substantial role in the pathogenesis of tumor growth, progress, and metastasis. The traditional macrophages can kill and remove tumor cells. However, besides the classically activated macrophages (also called M1 macrophages), which respond to type I helper T cells and generate reactive oxygen species and nitric oxide to kill pathogens and cells, there are also the alternatively activated macrophages (M2 macrophages or tumor-associated macrophages (TAM)), which respond to type II helper T cells to mediate humoral immunity and tissue repair [6–9]. At the site of tumor formation, M1 macrophages are the first to be recruited to kill tumor cells, while M2 macrophages are preferentially recruited later to hypoxic and necrotic regions, and secrete a wide range of chemokines, enzymes, and growth factors, to promote tumor neovascularization, growth, and metastasis [6, 10–12].
However, whether TAM may play a role in the pathogenesis of an osteosarcoma is largely unknown. Here, in a mouse model of human osteosarcoma implantation, we studied the role of TAM in the growth of OS and how it functions. Our data show that the growth of an osteosarcoma is epidermal growth factor receptor (EGFR) signaling-dependent and TAM-mediated, suggesting that TAM and EGFR may be good targets for treating a human osteosarcoma.
Materials and methods
Culture and labeling of human OS cell line
The human osteosarcoma U2OS [5] cell line was purchased from ATCC and maintained in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10 % fetal bovine serum (PAA, Austria). To trace the U2OS cells in vivo, we infected the cells with a recombinant lentivirus expressing luciferase and green fluorescence protein (GFP) under the control of a CMV promoter at a multiplicity of infection (MOI) of 100, which resulted in nearly 100 % infection efficiency based on green fluorescence. The reporter-carrying U2OS cells were termed OS-GFP-LUC. To knock down the EGFR in U2OS cells, we infected the cells with a recombinant lentivirus expressing luciferase and ShEGFR-IRES-GFP under the control of the CMV promoter at the MOI of 100, which resulted in nearly 100 % infection efficiency based on green fluorescence. These EGFR-KO U2OS cells were termed OS-ShEGFR-GFP-LUC. All plasmids were produced by Genema (Shanghai, China).
Mouse manipulations
All mouse experiments were in accordance with the general principles contained in the Guide for the Care and Use of Laboratory Animals published by Liaoning Medical University. Ten-week-old male nonobese diabetic/severe combined immunodeficiency (NOD/SCID) mice were used for experiments, and 105 OS-GFP-LUC or OS-ShEGFR-GFP-LUC cells were orthotopically injected into the tibia of 10-week-old female NOD/SCID mice in order for them to develop the tumor. Tumor growth was monitored by bioluminescence imaging. For macrophage depletion, 0.2 ml clodronate liposomes (ClodronateLiposomes, Netherlands) was i.v.-injected every 3 days, from 3 weeks after OS implantation until 10 weeks. Control mice were injected with the same amount of control liposome at the same frequency.
Imaging of OS by bioluminescence
Bioluminescence was measured with the IVIS imaging system (Xenogen Corp., Alameda, CA). All of the images were taken 10 min after intraperitoneal injection of luciferin (Sigma) at 150 mg/kg body weight, as a 60-s acquisition and 10-s binning. During image acquisition, mice were sedated continuously via inhalation of 3 % isoflurane. Image analysis and bioluminescent quantification were performed using Living Image software (Xenogen Corp).
Tumor digestion and analysis and isolation of macrophages (subtypes) by flow cytometry
The implanted OS tumor was dissected out and chopped into small pieces of 2–3 mm in diameter, followed by 30 min digestion with 30 mg/dl collagenase and 0.5 mg/dl trypsin (Sigma, St. Louis, USA) in a 37 °C shaker at 150 rpm. The digestion appeared to be complete, since most of the digests passed a 70-nm filter. The filtered tumor digests were then incubated with APC-conjugated F4/80 antibody and/or PEcy7-conjugated CD163 (Serotec, St. Louis, USA) for flow cytometry analysis or sorting.
Western blot
Proteins were extracted from the brain tissue by RIPA buffer (Sigma, St. Louis, USA) and used for Western blot. Primary antibodies for Western blot are rabbit epidermal growth factor (EGF), EGFR, and β-actin (Cell Signaling, LA, USA). The secondary antibody is HRP-conjugated antirabbit (Jackson Labs, LA, USA). Images shown in the figure were representative of five mice in one group.
RNA extraction, reverse transcription and quantitative PCR
Total RNA was extracted using Trizol (Invitrogen, USA) according to the manufacturer’s instructions. For messenger RNA (mRNA) analysis, complementary DNA (cDNA) was randomly primed from 2 μg of total RNA using the Omniscript reverse transcription kit (Qiagen, USA). Real-time PCR was subsequently performed in triplicate with a 1:4 dilution of cDNA using the Quantitect SyBr green PCR system (Qiagen) on a Rotor-Gene 6000 series PCR machine (Corbett Research, USA). Data were collected and analyzed using the Rotor-Gene software accompanying the PCR machine. Relative expression levels were determined using the comparative quantification feature of the Rotor-Gene software. All mRNA quantification data were normalized to β-actin. Sequences of PCR primers and RNA oligonucleotides for real-time PCR were generated by the Shanghai Sangon company.
Statistics
All data were statistically analyzed using one-way ANOVA with a Bonferroni correction. All values are depicted as mean ± standard deviation (SD) and are considered significant if p < 0.05.
Results
A mouse model to allow in vivo tracing of OS growth
To trace the U2OS cells in vivo, we infected U2OS cells with a recombinant lentivirus expressing luciferase and GFP under the control of the CMV promoter at the MOI of 100, which resulted in nearly 100 % infection efficiency based on green fluorescence (Fig. 1a). The reporter-carrying U2OS cells were termed OS-GFP-LUC. In order to evaluate the role of TAM in the development and growth of OS, we generated a mouse model by orthotopically injecting 105 OS-GFP-LUC into the tibia of NOD/SCID mice, since it is one of the most common locations of primary osteosarcoma in humans. Tumor growth was monitored by bioluminescence imaging. We found a continuous growth of the implanted tumor in the recipient mice (Fig. 1b, c). Thus, this model allows the tracing of the growth of OS in vivo.
A mouse model to allow in vivo tracing of OS growth. a Cultured U2OS cells carrying luciferase and GFP under the control of a CMV promoter were termed OS-GFP-LUC; b, c 105 OS-GFP-LUC were implanted into the tibia of NOD/SCID mice, and tumor growth was monitored by bioluminescence imaging, shown by representative images of the same mouse at different time points (b) and quantification (c). Quantification was shown as fold change to the luminescence levels at 1 week after implantation. GFP green fluorescence protein, DAPI nuclei. *p < 0.05. The bar is 10 μm
Macrophage polarization occurred at the site of human OS implantation
Since macrophages have two subtypes (M1 and M2 macrophages) with very different biological functions, we aimed to examine whether macrophage polarization may occur during the development and growth of OS. Therefore, at 1 week, 3 weeks, or 10 weeks after OS implantation, we digested the tumor implants and analyzed the infiltrated macrophages (based on the pan-macrophage marker F4/80) and differentiated their subtypes (based on the M2-macrophage marker CD163) in the tumor digests by flow cytometry. We found that most F4/80-positive macrophages in the tumor 1 week after OS implantation were CD163-negative M1 macrophages, while most F4/80-positive macrophages in the tumor 3 or 10 weeks after OS implantation were CD163-positive M2 macrophages (Fig. 2a, b), suggesting that macrophage polarization to a M2 subtype, or TAM, occurs during the first 3 weeks after tumor implantation.
Macrophage polarization occurred at the site of human OS implantation (a, b). At 1 week, 3 weeks, or 10 weeks after OS implantation, we digested the tumor implants and analyzed the infiltrated macrophages (based on the pan-macrophage marker F4/80) and differentiated their subtypes (based on the M2-macrophage marker CD163) in the tumor digests by flow cytometry. Representative FAC charts (a) and quantification (b) were shown. Macrophage polarization to an M2 subtype, or TAM, occurs during the first 3 weeks after tumor implantation. *p < 0.05
Elimination of TAM significantly decreased OS growth
To examine whether M2 macrophages, TAM, have any effect on the growth of the implanted OS, we chemically depleted the infiltrated macrophage infiltration with clodronate [13]. Clodronate is a hydrophilic molecule that is packaged in a liposome to mediate internalization clodronate into macrophages. This molecule has a short half-life when released in the circulation, but does not easily cross phospholipid bilayers of liposomes or cell membranes. As a consequence, once ingested by a macrophage in a liposome-encapsulated form, it will accumulate within the cell to induce the apoptosis of the macrophage. Given the fact that neither the liposomal phospholipids chosen nor the clodronate is toxic to other nonphagocytic cells, this method has proven its efficacy and specificity for depletion of macrophage subsets in various organs [13–17].
Thus, we gave multiple injections of clodronate every 3 days since 3 weeks after OS implantation, to continuously eliminate TAM, as majority of the macrophages 3 weeks after OS implantation at the tumor site are M2 macrophages, or TAM (Figs. 2a, b, and 3a). Our data showed that clodronate administration reduced most of the (M2) macrophages at the tumor site (Fig. 3b, c). Moreover, analysis of the bioluminescence showed that reduction in TAM resulted in a significant decrease in the tumor growth (Fig. 3d, e). Our data thus demonstrate that elimination of TAM significantly decreased OS growth.
Elimination of TAM significantly decreased OS growth. a Multiple injections of clodronate were performed every 3 days, since 3 weeks after OS implantation, to continuously eliminate TAM. b, c Clodronate administration reduced most of the (M2) macrophages at the tumor site, shown by representative FAC charts (b) and quantification (c). d, e Analysis of the bioluminescence showed that reduction in TAM resulted in a significant decrease in the tumor growth. The data were shown by representative images (d) and quantification (e). *p < 0.05
TAM from OS expressed a high level of EGF, and OS expressed a high level of EGFR
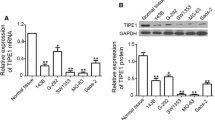
Since many reports have shown that inhibition of EGFR signaling may reduce the growth of many tumors, we examined whether it may also account for the TAM-mediated promotion of OS growth. We extracted RNA and protein from the implanted OS cells (based on GFP) and from the sorted TAM cells (based on F4/80 and CD163). We analyzed EGFR mRNA levels by reverse transcription and quantitative PCR (RT-qPCR) (Fig. 4a) and protein levels by Western blot (Fig. 4b). We found that OS expressed high levels of EGFR, but little EGF, while TAM expressed high levels of EGF, but not EGFR, suggesting their cross-talk may be through EGF/EGFR signaling. Interestingly, macrophage depletion did not overtly affect the EGF and EGFR expressions by TAM and OS, respectively (Fig. 4b).
TAM from OS expressed a high level of EGF, and OS expressed a high level of EGFR. a, b RNA and protein were extracted from the implanted OS cells (based on GFP) and from the sorted TAM cells (based on F4/80 and CD163). a We analyzed mRNA levels of EGF/EGFR by RT-qPCR. b We analyzed protein levels of EGF/EGFR by Western blot. Clo clodronate; β-actin is a protein loading control. c OS-ShEGFR-GFP-LUC was implanted into the mice. Inhibition of EGFR signaling in OS significantly decreased the tumor. *p < 0.05
TAM-mediated promotion of OS growth is EGFR signaling-dependent
To examine whether TAM-mediated promotion of OS growth is EGFR signaling-dependent, we used short hairpin RNA (shRNA) to knock down EGFR expression in U2OS cells and prepared OS-ShEGFR-GFP-LUC lines for implantation into the mice (Fig. 4b). We found that inhibition of EGFR signaling in OS significantly decreased tumor growth (Fig. 4c), without affecting the TAM number or polarization (not shown). Thus, TAM-mediated promotion of OS growth is EGFR signaling-dependent.
Discussion
High-grade OS is a malignant bone tumor that predominantly occurs in adolescent patients. Despite wide-margin surgery and intensification of chemotherapeutic treatment, overall survival rates are not reaching satisfaction [1]. Novel administration modalities are needed although data on critical biological mechanisms allowing the development of novel therapeutic agents are scarce. TAM may promote tumorigenesis of OS through immunosuppression, expression of matrix-degrading proteins, and support of angiogenesis. Therefore, in addition to conventional chemotherapeutic agents, immune regulatory strategies may be novel and effective, by modulating TAM [6, 7, 11, 12, 18]. However, only limited information on macrophage infiltration and activation in OS is available [3, 4].
Here, in a mouse model of human OS implantation, we showed that the recruited macrophages at the site of the implanted tumor were polarized to an M2 subtype (same as TAM) with the development and growth of the OS. In a loss-of-function experiment, we deleted those TAM with a specific macrophage-eliminating liposome, which resulted in decreased tumor growth. These data suggest that TAM play a nonredundant role during the development and growth of OS.
According to literature, TAM can secret the immunosuppressive cytokines IL-10, transforming growth factor beta (TGF-β), and prostaglandin E2 (PGE2) and numerous growth factors including VEGF, basic fibroblast growth factor (bFGF), EGF, platelet-derived growth factor (PDGF), and TGF-α [6, 7, 11, 12, 17, 18]. Among these factors, EGF signals through its receptor EGFR and has been reported to be involved in the tumor growth and progress in many kinds of cancers [19]. Moreover, we found that U2OS expressed high levels of EGFR. Therefore, we decided to study whether TAM may promote the growth of OS through EGF/EGFR signaling. Inhibition of EGFR expression in the cancer cells with shRNA prevented the tumor to grow in response to the recruited macrophages. These data demonstrate that the growth of osteosarcoma is EGFR signaling-dependent and TAM-mediated. Future experiments may be applied to further dissect the signaling pathway that regulates this model and to provide evidence for using TAM and EGFR as novel targets for treating human osteosarcoma.
References
Yang J, Zhang W. New molecular insights into osteosarcoma targeted therapy. Curr Opin Oncol. 2013;25:398–406.
Tsuchiya H, Tomita K, Mori Y, Asada N, Morinaga T, Kitano S, et al. Caffeine-assisted chemotherapy and minimized tumor excision for nonmetastatic osteosarcoma. Anticancer Res. 1998;18:657–66.
Buddingh EP, Kuijjer ML, Duim RA, Burger H, Agelopoulos K, Myklebost O, et al. Tumor-infiltrating macrophages are associated with metastasis suppression in high-grade osteosarcoma: a rationale for treatment with macrophage activating agents. Clin Cancer Res. 2011;17:2110–9.
Endo-Munoz L, Evdokiou A, Saunders NA. The role of osteoclasts and tumour-associated macrophages in osteosarcoma metastasis. Biochim Biophys Acta. 1826;2012:434–42.
Ponten J, Saksela E. Two established in vitro cell lines from human mesenchymal tumours. Int J Cancer. 1967;2:434–47.
Gordon S. Alternative activation of macrophages. Nat Rev Immunol. 2003;3:23–35.
Gordon S, Martinez FO. Alternative activation of macrophages: mechanism and functions. Immunity. 2010;32:593–604.
Geissmann F, Manz MG, Jung S, Sieweke MH, Merad M, Ley K. Development of monocytes, macrophages, and dendritic cells. Science. 2010;327:656–61.
Ricardo SD, van Goor H, Eddy AA. Macrophage diversity in renal injury and repair. J Clin Invest. 2008;118:3522–30.
Biswas SK, Mantovani A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm. Nat Immunol. 2010;11:889–96.
Coffelt SB, Hughes R, Lewis CE. Tumor-associated macrophages: effectors of angiogenesis and tumor progression. Biochim Biophys Acta. 2009;1796:11–8.
Lamagna C, Aurrand-Lions M, Imhof BA. Dual role of macrophages in tumor growth and angiogenesis. J Leukoc Biol. 2006;80:705–13.
van Rooijen N, Bakker J, Sanders A. Transient suppression of macrophage functions by liposome-encapsulated drugs. Trends Biotechnol. 1997;15:178–85.
van Rooijen N, van Nieuwmegen R. Elimination of phagocytic cells in the spleen after intravenous injection of liposome-encapsulated dichloromethylene diphosphonate. An enzyme-histochemical study. Cell Tissue Res. 1984;238:355–8.
Plosker GL, Goa KL. Clodronate. A review of its pharmacological properties and therapeutic efficacy in resorptive bone disease. Drugs. 1994;47:945–82.
Kanis JA, McCloskey EV. Clodronate. Cancer. 1997;80:1691–5.
Xiao X, Gaffar I, Guo P, Wiersch J, Fischbach S, Peirish L, et al. M2 macrophages promote beta-cell proliferation by up-regulation of smad7. Proc Natl Acad Sci U S A. 2014;111:E1211–20.
Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. J Clin Invest. 2012;122:787–95.
Klambt C. Egf receptor signalling: the importance of presentation. Curr Biol. 2000;10:R388–91.
Acknowledgments
This work was supported by internal funding from Liaoning Medical University.
Conflicts of interest
The authors have declared that no competing interests exist.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xiao, Q., Zhang, X., Wu, Y. et al. Inhibition of macrophage polarization prohibits growth of human osteosarcoma. Tumor Biol. 35, 7611–7616 (2014). https://doi.org/10.1007/s13277-014-2005-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-2005-y