Abstract
The relationship between the GSTP1 A313G and GSTM1 null/present polymorphisms and the treatment response (TR) of platinum-based chemotherapy in non-small cell lung cancer (NSCLC) patients have been extensively investigated by many studies, but the results were inconsistent and inconclusive. The aim of this meta-analysis was to further explore the predictive value of the GSTP1 and GSTM1 polymorphisms by collecting currently available evidence. Relevant studies were searched in PubMed, Embase, and CNKI. Inclusion criteria were NSCLC patients receiving platinum-based treatment, evaluated GSTP1 A313G or GSTM1 null/present polymorphisms, and TR. Odds ratio (OR) with 95 % confidence interval (CI) was calculated to assess the strength of the associations. Subgroup analysis by race was also conducted to explore the source of heterogeneity. A total of nine studies including 961 NSCLC patients were qualified for analysis. We found that GSTM1 null/present but not GSTP1 A313G polymorphism was associated with platinum-based TR (for GSTM1, null vs present: OR = 1.77, 95% CI = 1.19–2.62). When subgroup analysis by race was done, both GSTP1 and GSTM1 polymorphisms were significantly associated with TR in East-Asian patients, but not in Caucasians. In addition, the heterogeneity disappeared in Asian and Caucasian patients when subgroup analysis by race was done. Our study suggested that the GSTP1 A313G and GSTM1 null/present polymorphisms could predict the treatment response of the platinum-based chemotherapy in NSCLC patients, especially in East-Asian patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer remains the leading cause of cancer-related mortality worldwide. Non-small cell lung cancer (NSCLC) accounts for 85 % of primary lung cancers, and nearly two-thirds of NSCLC cases are diagnosed at advanced stages [1, 2]. Platinum-based double-agent chemotherapy is still one of the major therapeutic choices for NSCLC, especially for patients in advanced stages [3]. However, the efficacy of platinum-based chemotherapy is usually very heterogeneous and unpredictable even in NSCLC patients with similar clinical and pathologic features. Genetic factors such as SNPs, gene expression products may influence the treatment effectiveness [4].
Platinum agents could bind to DNA and induce intrastrand, interstrand DNA, as well as DNA-protein cross-links. This platinum-induced DNA adducts will block replication and inhibit transcription and result in apoptosis and cell growth inhibition [5]. Decreasing of platinum compounds through the glutathione metabolic pathway may contribute to the development of resistance to the platinum-based chemotherapy. Glutathione S-transferases (GSTs) are phase II metabolic enzymes involved in the platinum detoxification mediated by glutathione (GSH) conjugation. Increase in GSH content would decrease platinum-DNA binding, as a result, intracellular platinum accumulation was decreased, and platinum resistance was usually accompanied as an outcome. In contrast, downregulation of glutathione-related enzymes may improve platinum sensitivity [6–8]. The most important human GST genes are GSTM1, GSTP1, GSTT1, and GSTA1 [9]. In the present study, we only focus on the effect of GSTP1 and GSTM1 polymorphisms on platinum-based treatment as the polymorphisms in these two genes were mostly investigated. One nonsynonymous polymorphism occurring in GSTP1, a single nucleotide substitution (A to G) at position 313 induces replacement of isoleucine (IIe) with valine (Val) at codon 105, has been shown to result in reduced glutathione conjugating ability whereas the GSTM1 polymorphism (null genotype) has been associated with diminished GST enzyme activity [10, 11]. Some studies have explored the relationship between GSTP1 A313G and GSTM1 null/present polymorphisms and the treatment response in NSCLC patients receiving platinum-based chemotherapy. But the results were inconclusive and sometimes were even conflicting due to the small sample size and the limited statistic power in a single study. To further evaluate this relationship, we conducted the present meta-analysis to comprehensively evaluate the association between GSTP1 A313G and GSTM1 null/present polymorphisms and the treatment response (TR) in NSCLC patients receiving platinum-based chemotherapy.
Materials and methods
Literature search and selection criteria
Relevant studies were searched in PubMed, Embase, and the China National Knowledge Infrastructure (CNKI) databases. The literature search was updated to October 31, 2013. The following terms were used: (“GSTP1” or “GSTM1” or “GST”) and (“polymorphism” or “SNP” or “mutation” or “variation”) and (“lung cancer” or “lung neoplasm”) and (“platinum” or “cisplatin” or “carboplatin” or “oxaliplatin”). References from retrieved articles or previous meta-analyses were searched manually for additional studies.
The following inclusion criterias were used: (1) assess the relationship between GSTP1/GSTM1 polymorphisms and TR, (2) pathologically proven NSCLC patients receiving any of the platinum drugs (“cisplatin” or “carboplatin” or “oxaliplatin”), and (3) GSTP1 A313G (rs1695) and GSTM1 null polymorphisms should be genotyped independently. Also, the following exclusion criterias were provided: (1) lack of sufficient data to extract the information we need such as genotype and TR; (2) studies which included patients with small cell lung cancer (SCLC) or samples mixed with SCLC that makes extraction of sufficient information for NSCLC impossible; and (3) case reports, reviews, meta-analyses, cell line, and animal experiment studies. For the studies with overlapping data, only the most rounded studies with more information were included.
Two investigators (YYL and XL) independently extracted the data; any disagreement was solved unanimously via discussion. For each study, general characteristics such as authors, year of publication, country, ethnic group of the study population, sample size, tumor stage, chemotherapy drug, SNP genotyping methods, SNPs, and allele frequency were collected.
Statistical Analysis
The treatment response (TR) was used to measure chemotherapy efficacy, to summarize this information, the patients were divided as responders [complete responders (CR) or partial responders (PR)] and non-responders [stable disease (SD) or progressive disease (PD)] according to the WHO criteria [12] or Response Evaluation Criteria in Solid Tumors (RECIST) criteria [13]. For GSTP1 A313G, five genetic comparison models were analyzed (A: dominant model, AG + GG vs AA; B: heterozygote model, AG vs AA; C: homozygote model, GG vs AA; D: allele model, G vs A; E: recessive model, GG vs AA + AG); for GSTM1, null versus present genotype was applied for analysis. The pooled odds ratio (OR) with its 95 % confidence interval (CI) was calculated for CR + PR vs SD + PD.
To take into account the possibility of heterogeneity across the studies, chi-square–based Q test and I2 statistics were applied. P > 0.10 for Q test was considered statistically significant; for I2, the value ranged from 0 to 100 % present different degree of heterogeneity (0 to 25 %: no heterogeneity; 25 to 50 %: moderate heterogeneity; 50 to 75 %: large heterogeneity; 75 to 100 %: extreme heterogeneity) [14]. A fixed-effect model analysis was performed when I2 > 50 % or P < 0.10 for Q test [15]; otherwise, a random-effect model was conducted [16]. Further subgroup analysis according to the original population (East-Asian and Caucasian) was done to explore the potential heterogeneity between studies. The main publication bias was investigated by Begg’s test and Egger’s test. All P values were two-sided, and most of our analyses were performed by the Stata software version 11.2 (StataCorp, College station, TX).
Results
Eligible studies
The initial search strategy yielded 87 publications, after carefully screening the title and abstract, 24 publications seemed to meet our selection criteria. After reading the full text, 15 studies were excluded for the following reasons: six studies did not report TR, one meta-analysis, patients in three studies did not receive platinum doublets, two studies were mixed with SCLC samples, three studies exist with data overlapping, and finally, nine publications including 961 NSCLC patients were included in our study [17–25]. Among the nine studies, eight studies including 724 patients evaluated the relationship between GSTP1 A313G polymorphism and TR in NSCLC patients [17, 18, 20–25], and four studies including 455 patients investigated the effect of GSTM1 null polymorphism on TR [17, 19, 23, 24]. The samples sizes vary from 59 to 137. Six studies were conducted on East-Asian patients (mainly in Chinese) [19, 18, 20–22, 24] and three studies were conducted on Caucasian patients [17, 23, 25]. In our included studies, except two studies [21, 22] using WHO criteria to evaluated treatment response, RECIST criteria 1.0 was applied in the remaining studies [20, 18, 24, 19, 23, 17, 25]. Most of the studies included advanced NSCLC patients. Figure 1 showed the literature search and study selection procedures. The baseline characteristics of the included studies were summarized in Table 1.
GSTP1 A313G
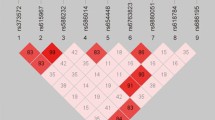
Eight studies including 724 NSCLC patients were pooled to estimate the association strength of GSTP1 A313G polymorphism with TR [17, 18, 20–25]. The main results were presented in Table 2 and Figs 2, 3, 4 and 5. As the between study heterogeneity was obvious under four comparison models (dominant: I2 = 68.6 %, P = 0.002; heterozygous model: I2 = 53.2 %, P = 0.06; homozygous model: I2 = 56.4 %, P = 0.06; allele model: I2 = 75.7 %, P = 0.002), random-effect model was applied for overall analysis. In the overall analysis, no association was found between the GSTP1 A313G polymorphism and the TR in any of the five comparison models (Table 2). When we conducted stratified analysis by race, we found that the variant G allele was significantly associated with good response to platinum-based chemotherapy in East-Asian patients (dominant model, AG + GG vs AA: OR = 2.95, 95 % CI = 1.90–4.60; heterozygous model, AG vs AA: OR = 2.37, 95 % CI = 1.29-4.34; homozygous model, GG vs AA: OR = 3.87, 95 % CI = 1.17–12.8; allele model, G vs A: OR = 2.28, 95 % CI = 1.43–3.63). However, this association was not significant in Caucasian patients (Table 2). Notably, no heterogeneity was observed in both Asian and Caucasian subgroups under five comparison models (Table 2).
GSTM1
A total of four studies with 455 individuals were included in the analysis for GSTM1 polymorphism and TR [17, 19, 23, 24]. As no significant heterogeneity exist (I2 = 20.7 %, P = 0.29), fixed-effect model was applied. The pooled analysis suggested that GSTM1 null genotype was significantly associated with good response compared with the present genotype (null vs present: OR = 1.77, 95 % CI = 1.19–2.62). In subgroup analysis by race, this association was found in East-Asian patients (OR = 2.32, 95 % CI = 1.30–4.12) but not in Caucasian patients (OR = 1.39, 95 % CI = 0.81–2.39). No heterogeneity was detected in Asian and Caucasian subgroups (Fig 6).
Publication bias
Publication bias was examined by using funnel plot analysis. The shape of the funnel plot did not reveal any evidence of obvious asymmetry under dominant, allele, and heterozygous models (figure not shown). In addition, Begg’s and Egger’s tests were applied to detect publication bias. For GSTP1 A313G, no significant bias was found under dominant, heterozygous, homozygous, and allele models (dominant model: P Begg = 0.27, P Egger = 0.14; heterozygous model: P Begg = 0.13, P Egger = 0.23; homozygous model: P Begg = 0.46, P Egger = 0.11; allele model: P Begg = 0.22, P Egger = 0.12). For GSTM1, no significant bias was detected (P Begg = 0.31, P Egger = 0.49).
Discussion
This meta-analysis, involving a total of 961 NSCLC patients from nine studies examined the association of two polymorphisms of GST (P1 and M1) and the treatment response of platinum-based chemotherapy in NSCLC patients. Our analysis provides support that genetic polymorphism of GSTP1 A313G (AG + GG vs AA, AG vs AA, GG vs AA and G vs A) and GSTM1 polymorphism (null vs present) relate to better treatment response in NSCLC patients receiving platinum-based chemotherapy. This association was mainly observed in Asians but not in Caucasians.
Previous meta-analysis by Yin et al. also investigated the relationship between GSTP1 A313G and GSTM1 null polymorphisms and the TR in NSCLC patients receiving platinum-based regimen [26]. In Yin’s study, they found GSTP1 A313G polymorphism was associated with TR in Asian patients, but not in overall patients, which was consistent with our result. They did not found significant association between GSTM1 null polymorphism and TR in overall patients; however, our result found the significant association, the inconsistent result may belong to another two studies including 196 patients included in our analysis. When compared with previous meta-analysis, our result showed some advantages. Firstly, our result included more studies and larger sample size than the previous one (four studies including 360 patients were included in our analysis). Secondly, our analysis is more comprehensive and detailed than the previous one. Yin only evaluated the relationship between GSTP1 polymorphism and platinum-based treatment response under dominant model. Our study explored this relationship under five models (dominant, heterozygote, homozygote, allele, and recessive models), and the significant association was found in four models (dominant, heterozygote, homozygote, and allele models). At last, we comprehensively assessed the publication biases by funnel plot, Begg’s, and Egger’s test and all found no significant publication bias exist. In Yin’s study, potential publication bias was detected by funnel plot. In the view of this, we convinced that the result of our meta-analysis, in essence, was more robust and reliable.
It is known that the allele frequencies of metabolic genes are not equally distributed throughout the human population but follow diverse ethnic patterns [27]; therefore, the subgroups by race were done. Our results indicated that GSTP1 A313G and GSTM1 null genotype were more likely to respond to platinum in East-Asians but not in Caucasians. GSTP1 A313G is one nonsynonymous polymorphism, and this SNP has been shown to result in reduced glutathione conjugating ability. GSTM1 deletion polymorphisms (null genotype) have been associated with diminished GST enzyme activity. Previous study showed that GSTP1 G allele and GSTM1 null genotype resulted in reduced glutathione conjugating ability. Thus, individuals with variant GSTP1 and GSTM1 genotypes may possess increased susceptibility to cancer but have good responses to chemotherapy due to decreased detoxification of carcinogens and chemotherapeutic agents [7, 20].
One of the major concerns in a sound meta-analysis is the degree of heterogeneity. We carried out the Q test and I2 statistics to test the significance of heterogeneity. Obvious heterogeneity between studies was observed in overall comparisons. When we conducted subgroup analysis by race, heterogeneity disappeared in both East-Asian and Caucasian subgroups under all comparisons, respectively, indicating the major heterogeneity could be accounted for the genetic distribution in different race. In addition, the inconsistency of these studies may be also due to population background, source of patients, disease condition, or by chance. Further large sample multi-center studies are needed.
Additional limitations should also be taken into consideration. Firstly, our sample size was not large enough; only nine studies including 961 NSCLC patients were included in our analysis. Such limited sample size still could not draw a robust conclusion. In the analysis of GSTM1 polymorphism and platinum-based chemotherapy response of NSCLC in East-Asian patients, only two publications (Li, 2012; Mao 2007) of 204 patients [19, 24] were included, the sample size was not large enough, so the result maybe not valid. Also, lack of original data in some studies limited our further evaluation of other parameters such as overall survival (OS), progression-free survival (PFS), and toxicity. Secondly, the potential heterogeneity and publication bias exist. Although the heterogeneity in our study could be accounted for race, maybe some substantial factors such as age, sex, cigarette smoking status, histology type, tumor stage, chemotherapy regime, treatment cycle, additional surgery, or radiotherapy may play a role. However, we were unable to conduct further stratified analysis as most studies did not report the information in details. Besides, publication bias may exist. Other articles published in non-English and non-Chinese, or studies that fail to get published with negative or null results cannot be examined by us. Even in publications we could identify, some failed to be included in our analysis due to lack of sufficient data.
In conclusion, our meta-analysis indicated that GSTP1 A313G and GSTM1 null polymorphisms can be associated with the treatment response of the platinum-based chemotherapy in NSCLC, mainly in East-Asians. The insight into future platinum-based chemotherapy in NSCLC using these polymorphisms would make it more attractive. However, as the limitations, heterogeneities, and bias of meta-analysis show, our conclusion needs to be interpreted with caution. Also, additional prospective large studies with strict designed methodology are warranted to further confirm our findings.
References
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300. doi:10.3322/caac.20073.
Herbst RS, Heymach JV, Lippman SM. Lung cancer. N Engl J Med. 2008;359(13):1367–80. doi:10.1056/NEJMra0802714.
Molina JR, Adjei AA, Jett JR. Advances in chemotherapy of non-small cell lung cancer. Chest. 2006;130(4):1211–9. doi:10.1378/chest.130.4.1211.
Custodio AB, Gonzalez-Larriba JL, Bobokova J, Calles A, Alvarez R, Cuadrado E, et al. Prognostic and predictive markers of benefit from adjuvant chemotherapy in early-stage non-small cell lung cancer. J Thorac Oncol. 2009;4(7):891–910. doi:10.1097/JTO.0b013e3181a4b8fb.
Rabik CA, Dolan ME. Molecular mechanisms of resistance and toxicity associated with platinating agents. Cancer Treat Rev. 2007;33(1):9–23. doi:10.1016/j.ctrv.2006.09.006.
Mannervik B, Danielson UH. Glutathione transferases—structure and catalytic activity. CRC Crit Rev Biochem. 1988;23(3):283–337.
Stewart DJ. Tumor and host factors that may limit efficacy of chemotherapy in non-small cell and small cell lung cancer. Crit Rev Oncol Hematol. 2010;75(3):173–234. doi:10.1016/j.critrevonc.2009.11.006.
Ikeda K, Miura K, Himeno S, Imura N, Naganuma A. Glutathione content is correlated with the sensitivity of lines of PC12 cells to cisplatin without a corresponding change in the accumulation of platinum. Mol Cell Biochem. 2001;219(1–2):51–6.
Ekhart C, Rodenhuis S, Smits PH, Beijnen JH, Huitema AD. An overview of the relations between polymorphisms in drug metabolising enzymes and drug transporters and survival after cancer drug treatment. Cancer Treat Rev. 2009;35(1):18–31. doi:10.1016/j.ctrv.2008.07.003.
Hayes JD, Pulford DJ. The glutathione S-transferase supergene family: regulation of GST and the contribution of the isoenzymes to cancer chemoprotection and drug resistance. Crit Rev Biochem Mol Biol. 1995;30(6):445–600. doi:10.3109/10409239509083491.
Zimniak P, Nanduri B, Pikula S, Bandorowicz-Pikula J, Singhal SS, Srivastava SK, et al. Naturally occurring human glutathione S-transferase GSTP1-1 isoforms with isoleucine and valine in position 104 differ in enzymic properties. Eur J Biochem. 1994;224(3):893–9.
Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer. 1981;47(1):207–14.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92(3):205–16.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. doi:10.1136/bmj.327.7414.557.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22(4):719–48.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Joerger M, Burgers SA, Baas P, Smit EF, Haitjema TJ, Bard MP, et al. Germline polymorphisms in patients with advanced nonsmall cell lung cancer receiving first-line platinum-gemcitabine chemotherapy: a prospective clinical study. Cancer. 2012;118(9):2466–75. doi:10.1002/cncr.26562.
Zhang YP, Sheng GF, Liu YP, Xue HP, Ling Y. The relationship of GSTP1 and clinical response to platinum based chemotherapy in advanced non-small cell lung cancer. J Med Theory Practice. 2012;25(24):3003–4.
Li W, Yue W, Zhang L, Zhao X, Ma L, Yang X, et al. Polymorphisms in GSTM1, CYP1A1, CYP2E1, and CYP2D6 are associated with susceptibility and chemotherapy response in non-small-cell lung cancer patients. Lung. 2012;190(1):91–8. doi:10.1007/s00408-011-9338-8.
Zhou F, Yu Z, Jiang T, Lv H, Yao R, Liang J. Genetic polymorphisms of GSTP1 and XRCC1: prediction of clinical outcome of platinum-based chemotherapy in advanced non-small cell lung cancer (NSCLC) patients. Swiss Med Wkly. 2011;141:w13275. doi:10.4414/smw.2011.13275.
Sun N, Sun X, Chen B, Cheng H, Feng J, Cheng L, et al. MRP2 and GSTP1 polymorphisms and chemotherapy response in advanced non-small cell lung cancer. Cancer Chemother Pharmacol. 2010;65(3):437–46. doi:10.1007/s00280-009-1046-1.
Yue Z, Xu Q, Xu Y, Dong NN, Zhang Y, Zhu LB, et al. GSTP 1 gene polymorphism and susceptibility as well as chemotherapy sensitivity to non-small cell lung cancer. Chin J Cancer Prev Treat. 2009;16(19):1441–4.
Kalikaki A, Kanaki M, Vassalou H, Souglakos J, Voutsina A, Georgoulias V, et al. DNA repair gene polymorphisms predict favorable clinical outcome in advanced non-small-cell lung cancer. Clin Lung Cancer. 2009;10(2):118–23. doi:10.3816/CLC.2009.n.015.
Mao Y, Huang CH, Hua D, Deng JZ, Wei W, Yao Q. The relationshhip between glutathione S-transferase gene polymorphisms and chemotherapy response in NSCLC patients. Shandong Med J. 2007;47(36):68–9.
Booton R, Ward T, Heighway J, Ashcroft L, Morris J, Thatcher N. Glutathione-S-transferase P1 isoenzyme polymorphisms, platinum-based chemotherapy, and non-small cell lung cancer. J Thorac Oncol. 2006;1(7):679–83.
Yin JY, Huang Q, Zhao YC, Zhou HH, Liu ZQ. Meta-analysis on pharmacogenetics of platinum-based chemotherapy in non small cell lung cancer (NSCLC) patients. PLoS One. 2012;7(6):e38150. doi:10.1371/journal.pone.0038150.
Gong M, Dong W, Shi Z, Xu Y, Ni W, An R. Genetic polymorphisms of GSTM1, GSTT1, and GSTP1 with prostate cancer risk: a meta-analysis of 57 studies. PLoS One. 2012;7(11):e50587. doi:10.1371/journal.pone.0050587.
Acknowledgments
This research was supported by Guangxi scientific research and technology development projects (Grant No.10124001A-44).
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, Y., Xian, L. The association between the GSTP1 A313G and GSTM1 null/present polymorphisms and the treatment response of the platinum-based chemotherapy in non-small cell lung cancer (NSCLC) patients: a meta-analysis. Tumor Biol. 35, 6791–6799 (2014). https://doi.org/10.1007/s13277-014-1866-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-1866-4