Abstract
Genetic polymorphisms of RAD51 135 G>C and XRCC2 G>A (rs3218536) have been reported to change the risk of ovarian cancer, but the results are controversial. To get a more precise result, a meta-analysis was performed. A comprehensive literature search in PubMed, Excerpta Medica Database, and China National Knowledge Infrastructure was carried out to get case–control studies published up to November 2013. The pooled odds ratio (OR) and its corresponding 95 % confidence interval (CI) were conducted to estimate the effect of RAD51 135 G>C and XRCC2 G>A (rs3218536) polymorphisms on ovarian cancer risk. A total of 13 independent case–control studies with 5,927 cases and 10,303 controls were included in this meta-analysis. There was no significant association between RAD51 135 G>C polymorphism and risk of ovarian cancer. However, the result of total studies indicated the XRCC2 G>A (rs3218536) polymorphism could reduce the risk of ovarian cancer (heterozygote model AG vs. GG: OR = 0.877, 95 % CI = 0.770–0.999, P = 0.048; dominant model AA/AG vs. GG: OR = 0.864, 95 % CI = 0.763–0.979, P = 0.022). The result was still significant after Hardy–Weinberg equilibrium-violating studies were excluded (allele contrast A vs. G: OR = 0.836, 95 % CI = 0.74–0.943, P = 0.004; homozygote model AA vs. GG: OR = 0.562, 95 % CI = 0.317–0.994, P = 0.048; heterozygote model AG vs. GG: OR = 0.859, 95 % CI = 0.753–0.98, P = 0.023; dominant model AA/AG vs. GG: OR = 0.842, 95 % CI = 0.74–0.958, P = 0.009). In the stratified analysis by ethnicity, significantly reduced risk was observed among Caucasians in dominant model (AA/AG vs. GG: OR = 0.867, 95 % CI = 0.764–0.984, P = 0.027). No significant association was found between the RAD51 135G>C polymorphism and the risk of ovarian cancer. Interestingly, XRCC2 G>A (rs3218536) polymorphism might reduce the risk of ovarian cancer. Larger-scale and well-designed studies are needed to further clarify the association.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian cancer (OC) is one of the most common cancers of the female genital tract and is the most fatal gynecologic cancer. The incidence of OC in Europe was 13.1 per 100,000, and the mortality was 7.6 per 100,000 on the basis of EUCAN investigation, in 2012 (http://eco.iarc.fr/EUCAN/Country.aspx?ISOCountryCd=968). What is worse is that the pathogenesis of OC is not completely understood yet. As roughly as 85 % of ovarian cancers are sporadic and 15 % are familial; it has been assumed that both genetic and environmental factors might be important in the development of ovarian cancer [1]. Multiple factors for ovarian cancer include age, family history of ovarian cancer, gravidity, and potentially the long-term use of hormone supplement therapy [1, 2]. Incessant ovulation may contribute to the evolution of ovarian cancer. During ovulation, the period in which the ovarian surface epithelium releases the ovum, the ovarian surface cells are exposed to inflammatory cytokines and oxidants that could bring about DNA damage into the ovarian epithelial layer [3]. In addition, repetitive ovulation increases the quantity of epithelial cell division, which finally induces DNA damage and lesions. If the lesions cannot be recognized and repaired, there will be an accumulation of potentially carcinogenic mutations [4, 5]. If these mutations are left unrepaired, these may result in carcinoma [6].
DNA damage interferes mitosis and the isolation of chromosomes. Such problems can be solved by homologous recombination repair (HRR) [7]. HRR is a key pathway to repair the DNA double-strand breaks (DSBs) and maintain the genetic stability [8, 9]. The central HR protein is RAD51, which propels strand exchange between unimpaired and impaired homologous DNA fragments insuring high quality of reproduction of DNA repair [7, 9]. RAD51 is a homologue of the RecA protein and is involved in the HRR of DNA double-strand break repair (DSBR) [10]. RAD51-deficient cells demonstrate genetic instability [8]. DNA repair protein RAD51 contains 339 amino acids and is encoded by the RAD51 gene. RAD51 gene is located at the human chromosome 15q15.1 and is highly polymorphic [11]. It has been identified that the single-nucleotide polymorphism (SNP)-135G>C (rs1801320) in the 5′untranslated region (UTR) of RAD51 may alter disease risk [12].
The X-ray repair cross-complementing group 2 protein (XRCC2), encoded by XRCC2, is one of the members of RAD51-related proteins. It may take part in the HRR of DNA DSBR and maintain genomic stability [7–9]. The XRCC2 gene, located on 7q36.1, is a functional candidate in neoplasia [13]. A number of studies have been preformed to investigate the relationship of XRCC2 polymorphism on various neoplasm, such as breast cancer, pancreatic cancer, cervical cancer, and upper aerodigestive tract cancer [14–17]. Common SNP Arg188His (R188H, rs3218536) of XRCC2 has been identified yet.
Hitherto, a number of molecular epidemiologic studies have been preformed to evaluate the effect of RAD51 135 G>C and XRCC2 G>A (rs3218536) polymorphisms on ovarian cancer risk in different populations [18–25]. However, the results were controversial. To further evaluate the role of RAD51 135 G>C and XRCC2 G>A (rs3218536) polymorphisms in ovarian cancer, we conducted a meta-analysis.
Materials and methods
Search strategy
To insure all case–control studies on the effect of RAD51 135 G>C and XRCC2 G>A (rs3218536) polymorphisms on ovarian cancer risk published up to November 2013, we conducted a comprehensive literature search in PubMed, Excerpta Medica Database (Embase), and China National Knowledge Infrastructure (CNKI), using the following key words: (ovarian cancer, ovarian carcinoma, or ovarian tumor) and (RAD51, XRCC2, or X-ray repair cross-complementing group 2) and (polymorphism or polymorphisms). All eligible studies were retrieved, and their references were searched manually. There was no language or population restriction. The literature retrieval was performed in duplication by two independent reviewers (Shujing Shi and Lingyan Qin). When the same or overlapping data was used in multiple publications, we chose the most complete one.
Inclusion and exclusion criteria
Human-associated studies included in the meta-analysis must meet the following criteria. They (a) have case–control designs, (b) evaluated the effect of RAD51 135 G>C and XRCC2 G>A (rs3218536) polymorphisms on ovarian cancer risk, and (c) supplied sufficient reported genotypic frequencies in both cases and controls for estimating an odds ratio (OR) with its 95 % confidence interval (CI). Exclusion criteria were as follows: They are (a) not case–control studies; (b) case reports, reviews, or letters; (c) control population including patients; and (d) studies contained overlapping data.
Data extraction
Information was carefully extracted from all eligible publications by two authors independently according to the inclusion criteria listed above, and consensus was finally reached on all items. The following information was collected: first author's surname, year of publication, country of origin, ethnicity, source of control, method of genotyping, numbers of cases and controls, Hardy–Weinberg equilibrium (HWE) of controls, and the frequency of genotypes in both cases and controls. Ethnic backgrounds were categorized as Caucasian and mixed.
Statistical analysis
The risked associations of ovarian cancer and polymorphisms of RAD51 135 G>C and XRCC2 G>A (rs3218536) genes were estimated by OR, together with its 95 % CI. The significance of the pooled OR was determined by Z test, and a P value of less than 0.05 was considered significant. The pooled ORs were performed in five genetic comparisons. For RAD51 135 G>C polymorphism, there were allele contrast (C vs. G), homozygote model (CC vs. GG), heterozygote model (CG vs. GG), dominant model (CC/CG vs. GG), and recessive model (CC vs. CG/GG). For XRCC2 G>A (rs3218536) polymorphism, there were allele contrast (A vs. G), homozygote model (AA vs. GG), heterozygote model (AG vs. GG), dominant model (AA/AG vs. GG), and recessive model (AA vs. AG/GG). Subgroup analyses were done by ethnicity (Caucasian and mixed) and studies obeying HWE.
Heterogeneity was calculated by the chi-square-based Q test. In addition, the percentage of total variation due to heterogeneity was quantified by the I 2 value [26]. If P Q ≥ 0.1 and I 2 < 50 %, we used the fixed-effects model (the Mantel–Haenszel method) to pool the results [27]. Otherwise, the random-effects model (the DerSimonian and Laird's method) was used [28]. If heterogeneity was observed, meta-regression and subgroup analyses were used to identify the sources of heterogeneity. Furthermore, the Galbraith plot was also used to identify the outliers as the possible sources of between-study heterogeneity [29].
The stability of our pooled results in the meta-analysis was measured by a sensitivity analysis, which was carried out by sequential omission of a single study [30]. The distribution of genotypes in the controls was assessed for HWE by a goodness-of-fit chi-square test. Begg's funnel plot and Egger's test were applied to examine the publication bias (P < 0.05 of Egger's test was considered statistically significant publication bias) [31, 32]. All analyses were performed using Stata software, version 12.0 (StataCorp, College Station, TX). Two-tailed P < 0.05 was considered statistically significant.
Results
Study characteristics
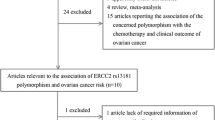
There were 28 articles relevant to searching strategy through PubMed, Embase, and CNKI. Eleven eligible articles were selected by screening the title, abstract, or content. Regarding one article [33], we e-mailed the author, but we still did not get its data. After excluding the two duplicated articles, there were eight eligible literatures that remained finally. According to the exclusion criteria, study 1 by Beesley et al. [21] was excluded, because the study had been previously reported by Webb et al. [20]. Thus, a total of eight articles (13 independent case–control studies) including 5,927 cases and 10,303 controls were included in this meta-analysis. The characteristics of the selected studies are shown in Tables 1 and 2.
For RAD51 135 G>C polymorphism, a total of five articles containing ten studies were included in the meta-analysis with 2,648 cases and 4,369 controls. There were nine studies of Caucasians and one mixed. Most of the controls (70 %) were population-based participants [18, 19, 24]. Two genotyping methods were used, including PCR-RFLP and TaqMan. The genotype distributions of the controls in three studies [19, 20, 25] violated HWE.
For XRCC2 G>A (rs3218536) polymorphism, totally, five articles including nine studies met the inclusion criteria and were selected in this meta-analysis with 3,279 cases and 5,934 controls. There were eight studies of Caucasians and one mixed in this part. Five studies were population-based [18, 21], and four were hospital-based studies. There were two genotyping methods including PCR-RFLP and TaqMan. The genotype distributions of the controls in two studies [22, 23] did not conform to HWE.
Meta-analysis
For RAD51 135 G>C polymorphism, the association between RAD51 135 G>C polymorphism and ovarian cancer risk is listed in Table 3. No significant heterogeneity was observed in the pooled analysis (P Q ≥ 0.1 and I 2 < 50 %); thus, fixed-effects model was applied. The results of total studies showed that there was no association between the RAD51 135 G>C polymorphism and ovarian cancer risk (C vs. G: OR = 1.056, 95 % CI = 0.912–1.222, P = 0.467; CC vs. GG: OR = 1.264, 95 % CI = 0.621–2.573, P = 0.519; CG vs. GG: OR = 1.046, 95 % CI = 0.894–1.225, P = 0.571; CC/CG vs. GG: OR = 1.001, 95 % CI = 0.867–1.155, P = 0.988 (Fig. 1); CC vs. CG/GG: OR = 1.244, 95 % CI = 0.611–2.531, P = 0.547). The association was not observed neither in ethnic subgroups nor genotyping methods. Detailed data are shown in Table 3.
For XRCC2 G>A (rs3218536) polymorphism, association between XRCC2 G>A (rs3218536) polymorphism and ovarian cancer risk is summarized in Table 4. The between-study heterogeneity was significant in allele contrast (A vs. G) and homozygote model (AA vs. GG), when all studies were pooled into meta-analysis (P Q < 0.1 or I 2 ≥ 50 %). Thus, the random-effects model was used to pool the results. The results of the total studies showed that XRCC2 G>A (rs3218536) polymorphism was associated with reduced risk of ovarian cancer (heterozygote model AG vs. GG: OR = 0.877, 95 % CI = 0.770–0.999, P = 0.048; dominant model AA/AG vs. GG: OR = 0.864, 95 % CI = 0.763–0.979, P = 0.022) (Fig. 2). After omitting the HWE-violating studies, significantly reduced risks were still found in allele contrast (A vs. G: OR = 0.836, 95 % CI = 0.74–0.943, P = 0.004), homozygote model (AA vs. GG: OR = 0.562, 95 % CI = 0.317–0.994, P = 0.048), heterozygote model (AG vs. GG: OR = 0.859, 95 % CI = 0.753–0.98, P = 0.023), and dominant model (AA/AG vs. GG: OR = 0.842, 95 % CI = 0.74–0.958, P = 0.009).When stratified by ethnicity, significant associations were observed for Caucasian subgroup in dominant model (AA/AG vs. GG: OR = 0.867, 95 % CI = 0.764–0.984, P = 0.027).
Heterogeneity analysis
For RAD51 135 G>C polymorphism, we did not find any between-study heterogeneity in all of the genetic models among the overall populations and the subgroup analyses.
For XRCC2 G>A (rs3218536) polymorphism, there was a significant heterogeneity found in allele contrast (A vs. G: P Q = 0.057, I 2 = 48.9) and homozygote model (AA vs. GG: P Q = 0.099, I 2 = 41.9) among the overall populations. We performed a meta-regression and subgroup analysis to explore the source of heterogeneity. Ethnicity and studies of HWE might lead to heterogeneity. When we performed subgroup analyses stratified by ethnicity, heterogeneity still existed in all the above two models in Caucasians. Beyond that, there was a significant heterogeneity which appeared in heterozygote model among Caucasians. To further find out the heterogeneity, we performed Galbraith plot analysis to spot the outliers which might lead to the heterogeneity. The results revealed that the study by Mohamed et al. [22] was the outlier in allele contrast, homozygote model, heterozygote model, and dominant model (Fig. 3). After excluding this study [22], we found that all I 2 values decreased obviously and P Q values were greater than 0.1 in all genetic models in the overall populations (allele contrast A vs. G: P Q = 0.921, I 2 = 0; homozygote model AA vs. GG: P Q = 0.772, I 2 = 0) and Caucasians (allele A vs. G: P Q = 0.857, I 2 = 0; homozygote model AA vs. GG: P Q = 0.651, I 2 = 0). When the HWE-violating studies were omitted, the results showed that there was no heterogeneity in any models among the overall populations.
Sensitivity analyses and publication bias
Sensitivity analysis was carried out by sequential deletion of individual studies. The summary result was not completely influenced after exclusion of individual study in sensitivity analyses. The result of sensitivity analysis affirmed the stability of our overall results.
Both Begg's funnel plot and Egger's test were used to assess the publication bias of the literatures included in this meta-analysis. The shapes of the funnel plot were relatively straightforward to discover the publication bias, but they did not reveal obvious evidence of asymmetry. P values of Egger’s tests provided statistical evidence of funnel plots’ symmetry. As a result, both the shape of the funnel plot (Fig. 4) and Egger's test value did not suggest any evidence of obvious asymmetry (Tables 3 and 4).
Discussion
Maintenance of genome stability by reliable DNA DSB repair is an indispensable part of the cell. If the proteins included in discovering DSBs cannot work normally, they might lead to a malignancy [34]. RAD51 is the central HR protein. XRCC2 is one of the members of RAD51-related proteins involved in the HRR pathway responsible for DNA double-strand break repair and genomic stability [7–9]. Genetic polymorphisms can reduce DNA repair capability and increase risk to human solid tumors [35]. Many literatures have reported the role of RAD51 and XRCC2 polymorphisms on ovarian cancer risk [18–25]. But the conclusions are controversial. In order to estimate the effect of RAD51 135 G>C and XRCC2 G>A (rs3218536) polymorphisms on ovarian cancer risk precisely, we performed this meta-analysis.
This paper included eight articles (13 independent case–control studies) with 5,927 cases and 10,303 controls. The results of the meta-analysis showed that RAD51 135 G>C polymorphism was not associated with ovarian cancer risk in the overall populations and all subgroups. However, we found that the XRCC2 G>A (rs3218536) polymorphism was associated with the reduced risk of ovarian cancer when all studies were pooled into meta-analysis (heterozygote model AG vs. GG: OR = 0.877, 95 % CI = 0.770–0.999, P = 0.048; dominant model AA/AG vs. GG: OR = 0.864, 95 % CI = 0.763–0.979, P = 0.022). In the stratified analysis by ethnicity, significantly reduced risks were observed among Caucasians in dominant model (AA/AG vs. GG: OR = 0.867, 95 % CI = 0.764–0.984, P = 0.027). As we all know, if the distributions of genotypes in the control groups were not in HWE, the results of genetic association might be not reliable [36]. Then, we performed an analysis by HWE-obeying studies. Subsequently, significantly reduced risks were still found in allele contrast, homozygote model, heterozygote model, and dominant model.
Heterogeneity was a common problem in meta-analysis. To find out the source of it is very important. We performed subgroup analyses stratified by ethnicity, but heterogeneity still existed. To further find out the between-study heterogeneity, we carried out Galbraith plots analysis to find out the outliers which might result in the heterogeneity. After excluding the outlier study [22], the between-study heterogeneity disappeared. Interestingly, significant associations were observed after omitting this article in allele contrast (A vs. G: OR = 0.873, 95 % CI = 0.768–0.991, P = 0.036), homozygote model (AA vs. GG: OR = 0.537, 95 % CI = 0.298–0.968, P = 0.039), and recessive model (AA vs. AG/GG: OR = 0.543, 95 % CI = 0.301–0.980, P = 0.043) among the overall populations. It indicated that the main source of heterogeneity might be the outlier study [22]. By subgroup analysis, we also found that ethnicity and studies of HWE might contribute to heterogeneity. It is widely believed that the source of heterogeneity is varied extensively. Genetic backgrounds, environmental exposures, methodology, sample size, etc. may influence results. Sensitivity analyses and publication bias were used in our study to guarantee that our results are more stable.
Although comprehensive meta-analysis was used to demonstrate the association, several limitations should be noted. Firstly, in this meta-analysis, only published studies were included, while some unpublished studies were omitted. Secondly, most studies were performed in Caucasians, so there were insufficient original studies which investigated the Africans, Asians, and other populations. Further studies will be needed in other ethnic groups in order to assess the effect of RAD51 135 G>C and XRCC2 G>A (rs3218536) polymorphisms on ovarian cancer risk. Thirdly, there were 5 of the 13 included studies which violated the law of HWE.
In summary, this meta-analysis suggested that no significant association was found between the RAD51 135 G>C polymorphism and the risk of ovarian cancer. Interestingly, XRCC2 G>A (rs3218536) polymorphism might reduce the risk of ovarian cancer. Larger-scale and well-designed studies are needed to further clarify the association.
References
Romero I, Bast Jr RC. Minireview: human ovarian cancer: biology, current management, and paths to personalizing therapy. Endocrinology. 2012;153(4):1593–602.
Brekelmans CT. Risk factors and risk reduction of breast and ovarian cancer. Curr Opin Obstet Gynecol. 2003;15(1):63–8.
Murdoch WJ, Martinchick JF. Oxidative damage to DNA of ovarian surface epithelial cells affected by ovulation: carcinogenic implication and chemoprevention. Exp Biol Med (Maywood). 2004;229(6):546–52.
Fathalla MF. Incessant ovulation—a factor in ovarian neoplasia? Lancet. 1971;2(7716):163.
Godwin AK et al. Spontaneous transformation of rat ovarian surface epithelial cells: association with cytogenetic changes and implications of repeated ovulation in the etiology of ovarian cancer. J Natl Cancer Inst. 1992;84(8):592–601.
Scully C, Field JK, Tanzawa H. Genetic aberrations in oral or head and neck squamous cell carcinoma 2: chromosomal aberrations. Oral Oncol. 2000;36(4):311–27.
Thacker J. A surfeit of RAD51-like genes? Trends Genet. 1999;15(5):166–8.
Thacker J. The RAD51 gene family, genetic instability and cancer. Cancer Lett. 2005;219(2):125–35.
Tambini CE et al. The importance of XRCC2 in RAD51-related DNA damage repair. DNA Repair (Amst). 2010;9(5):517–25.
Baumann P, West SC. Role of the human RAD51 protein in homologous recombination and double-stranded-break repair. Trends Biochem Sci. 1998;23(7):247–51.
Shinohara A et al. Cloning of human, mouse and fission yeast recombination genes homologous to RAD51 and recA. Nat Genet. 1993;4(3):239–43.
Hasselbach L et al. Characterisation of the promoter region of the human DNA-repair gene Rad51. Eur J Gynaecol Oncol. 2005;26(6):589–98.
Thacker J, Zdzienicka MZ. The XRCC genes: expanding roles in DNA double-strand break repair. DNA Repair (Amst). 2004;3(8–9):1081–90.
Lin WY et al. A role for XRCC2 gene polymorphisms in breast cancer risk and survival. J Med Genet. 2011;48(7):477–84.
Perez LO et al. XRCC2 R188H (rs3218536), XRCC3 T241M (rs861539) and R243H (rs77381814) single nucleotide polymorphisms in cervical cancer risk. Pathol Oncol Res. 2013;19(3):553–8.
Benhamou S et al. DNA repair gene XRCC2 and XRCC3 polymorphisms and susceptibility to cancers of the upper aerodigestive tract. Int J Cancer. 2004;112(5):901–4.
Jiao L et al. XRCC2 and XRCC3 gene polymorphism and risk of pancreatic cancer. Am J Gastroenterol. 2008;103(2):360–7.
Auranen A et al. Polymorphisms in DNA repair genes and epithelial ovarian cancer risk. Int J Cancer. 2005;117(4):611–8.
Jakubowska A et al. The RAD51 135 G>C polymorphism modifies breast cancer and ovarian cancer risk in Polish BRCA1 mutation carriers. Cancer Epidemiol Biomarkers Prev. 2007;16(2):270–5.
Webb PM et al. Double-strand break repair gene polymorphisms and risk of breast or ovarian cancer. Cancer Epidemiol Biomarkers Prev. 2005;14(2):319–23.
Beesley J et al. Association between single-nucleotide polymorphisms in hormone metabolism and DNA repair genes and epithelial ovarian cancer: results from two Australian studies and an additional validation set. Cancer Epidemiol Biomarkers Prev. 2007;16(12):2557–65.
Mohamed FZ et al. Role of DNA repair and cell cycle control genes in ovarian cancer susceptibility. Mol Biol Rep. 2013;40(5):3757–68.
Jakubowska A et al. BRCA1-associated breast and ovarian cancer risks in Poland: no association with commonly studied polymorphisms. Breast Cancer Res Treat. 2010;119(1):201–11.
Wang WW et al. A single nucleotide polymorphism in the 5′ untranslated region of RAD51 and risk of cancer among BRCA1/2 mutation carriers. Cancer Epidemiol Biomarkers Prev. 2001;10(9):955–60.
Levy-Lahad E et al. A single nucleotide polymorphism in the RAD51 gene modifies cancer risk in BRCA2 but not BRCA1 carriers. Proc Natl Acad Sci U S A. 2001;98(6):3232–6.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22(4):719–48.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Galbraith RF. A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med. 1988;7(8):889–94.
Attia J, Thakkinstian A, D'Este C. Meta-analyses of molecular association studies: methodologic lessons for genetic epidemiology. J Clin Epidemiol. 2003;56(4):297–303.
Stuck AE, Rubenstein LZ, Wieland D. Bias in meta-analysis detected by a simple, graphical test. Asymmetry detected in funnel plot was probably due to true heterogeneity. BMJ. 1998;316(7129):469. author reply 470-1.
Egger M et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Romanowicz-Makowska H et al. A single nucleotide polymorphism in the 5′ untranslated region of RAD51 and ovarian cancer risk in Polish women. Eur J Gynaecol Oncol. 2012;33(4):406–10.
Khanna KK, Jackson SP. DNA double-strand breaks: signaling, repair and the cancer connection. Nat Genet. 2001;27(3):247–54.
Garcia-Closas M et al. Genetic variation in the nucleotide excision repair pathway and bladder cancer risk. Cancer Epidemiol Biomarkers Prev. 2006;15(3):536–42.
Trikalinos TA et al. Impact of violations and deviations in Hardy-Weinberg equilibrium on postulated gene-disease associations. Am J Epidemiol. 2006;163(4):300–9.
Acknowledgments
We would like to thank the students who give us help.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Shujing Shi and Lingyan Qin contributed equally to this work so that they should be considered as the co-first authors.
Rights and permissions
About this article
Cite this article
Shi, S., Qin, L., Tian, M. et al. The effect of RAD51 135 G>C and XRCC2 G>A (rs3218536) polymorphisms on ovarian cancer risk among Caucasians: a meta-analysis. Tumor Biol. 35, 5797–5804 (2014). https://doi.org/10.1007/s13277-014-1769-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-1769-4