Abstract
Immune dysregulation plays a key role in the development of osteosarcoma (OS). Peripheral blood CD4+CXCR5+ T cells can induce B-cell activation and produce various cytokines and therefore may play critical roles in tumorigenesis. The purpose of the study was to investigate changes of peripheral CD4+CXCR5+ T cells in OS. Peripheral CD4+CXCR5+ T cells and its subtypes were determined by measuring CD3, CD4, CXCR5, CXCR3, and CCR6 in 38 OS patients and 42 healthy controls using flow cytometry. Data demonstrated that percentage of peripheral CD4+CXCR5+ T cells was significantly increased in OS patients (13.9 %) than in controls (8.6 %, p < 0.001). Further analysis identified a profound skewing of peripheral CD4+CXCR5+ T cell subsets toward Th2 and Th17 cells in OS patients. Investigating clinical status of the patients showed that prevalence of peripheral CD4+CXCR5+ T cells was significantly elevated in cases with metastasis (17.4 %) than those without metastasis (12.7 %). Similarly, patients with high tumor grade revealed increased percentage of CD4+CXCR5+ T cells compared to those with low tumor grade (15.3 versus 11.0 %). Interestingly, the upregulation of peripheral CD4+CXCR5+ T cells in patients with metastasis or high tumor grade was contributed by Th1 and Th17 subtypes. This study suggests the involvement of peripheral CD4+CXCR5+ T cells in the pathogenesis and progression of OS and provides novel knowledge for understanding this disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteosarcoma (OS) is the most common pediatric bone malignancy in the world [1]. Surgery used to be the only available treatment, and survival rate was as low as 17 % [2]. Treatment of patients with OS was transformed in the last 20 years with advances in chemotherapy and orthopedic surgical techniques, leading to long-term survival rates that now approach 70 % [2, 3]. However, further development of survival has not occurred despite multiple attempts at intensifying chemotherapy and utilizing new agents in trials [3]. Therefore, it is necessary to understand the natural history and biology of OS to improve our therapeutic approaches. Recent researches have provided evidence that dysregulation of immune system may be greatly involved in the pathogenesis of OS [2, 3].
T follicular helper cell (Tfh) is a recently identified CD4+ T helper lineage which is specialized in assisting the development and proliferation of B cells during germinal centers (GC) reactions in secondary lymphoid tissue [4, 5]. Tfh cells arise from activated T cells that express Bcl-6, a master transcription factor for Tfh cell differentiation [6]. The distinguishing characteristics of Tfh cells lie in that they express CXCR5, PD-1, ICOS, and CD40L and secrete interleukin (IL) 21 [6, 7]. These molecules can cause differentiation, proliferation, and class switching of B cells in the absence of Blimp-1 [7–10]. Researches have reported that Tfh cells may play important roles in the development of different cancers such as follicular lymphoma and peripheral T-cell lymphomas [11–13]. The mechanism remains unknown. It is possible that these cells may affect the pathogenesis of cancers through regulating IL-21. IL-21 is considered as a possible therapy for cancers including OS. Therefore, it is possible that Tfh cells may be involved in the development of OS.
In humans, most of the Tfh cells are located in the light zone of GC in secondary lymph nodules [14, 15]. Studies of human Tfh cells remain limited because it is difficult to access the lymphoid tissue of patients and controls. Therefore, studies of these cells with diseases mostly remain in animal models. This has created a strong need to establish surrogate strategies to assess the quality of Tfh cell responses in humans. In the recent years, researchers have identified peripheral CD4+CXCR5+ T cells in blood, which share functional properties with Tfh cells and appear to represent their circulating memory compartment [16]. Therefore, it may be used as a counterpart to measure Tfh cell disorders. Several studies have reported dysregulation of peripheral CD4+CXCR5+ cells in patients with autoimmune disorders or tumors [17–20]. However, little is known about the frequency of peripheral CD4+CXCR5+ T cells in OS patients. In this study, we explored the peripheral CD4+CXCR5+ T cells and their subtypes in OS patients and examined the potential effect of these cells on the progression of this disease.
Materials and methods
Study subjects
The study was approved by the Ethic Review Board of the Third Military Medical University (XQ083066). Written informed consent was obtained from each participant or guardians on the behalf of the children participants involved in the study. A total of 38 OS patients and 42 healthy controls were included in the research. The diagnosis of OS was established with histological examination in all cases. The grade of OS was determined by histologic types. All the patients received surgery, in which 25 patients had both surgery and chemotherapy, and one patient had surgery and radiation therapy. However, peripheral blood for this study was obtained before any treatment. The control population was recruited from people who came for general health exams. People who are relatives or have histories of malignancy and other major diseases were excluded from this study. All the control subjects were matched with patient population in terms of age, sex, and residence area (urban or rural). To exclude the possible effects of ethnicity, only Han Chinese were included in this study.
Surface and intracellular staining and flow cytometry
Peripheral blood mononuclear cells (PBMCs) were extracted according to Ficoll–Hypaque centrifugation of heparinized blood method. Purified PBMCs were washed and cultivated in RPMI tissue culture medium containing 10 % fetal calf serum (GIBCO, Grand Island, USA), penicillin, and streptomycin. Before flow cytometry, human PBMCs were stained in with FITC-CXCR5, PerCP-CD4, PE/Cy5-CD3, PE-CCR6, APC-CXCR3, or isotype-matched control IgG (BD Biosciences San Diego, CA, USA) at room temperature for 30 min. Cells were then washed with PBS, and we conducted analyses by flow cytometry using a FACSCalibur (Becton Dickinson) and FlowJo software. The cells were gated on the forward scatter of living cells and then centered on CD4+CXCR5+ T cells. Then, the numbers of subtype of CD4+CXCR5+ T cells were determined by flow cytometric analysis.
Statistical analysis
The Student’s t-test was used for comparison between groups. P value less than 0.05 is considered as statistical significance. Data were analyzed using SPSS 19.0 software.
Results
Clinical characteristics of the study subjects
Clinical characteristics of the subjects are presented in Table 1. There was no significant difference in age (p > 0.05) and gender (p > 0.05) between OS patients and healthy controls. In the 38 OS patients, 73.7 % of the tumor was located in long tubular bones, and 26.3 % was in axial skeleton. Twelve patients (31.6 %) were low tumor grade, whereas 26 (68.4 %) were high tumor grade. This study included two intermediate-grade OSs. These uncommon tumors are treated as if they are low-grade OSs. Therefore, we put them under low-grade category. Seven patients (18.4 %) presented pathological bone fracture. Based on metastasis status, ten patients presented metastatic cancer (Table 1).
Peripheral CD4+CXCR5+ T cells in OS patients and controls
We first quantified by flow cytometry the peripheral CD4+CXCR5+ T cells in healthy controls with different ages and genders. Data showed no significant differences (p > 0.05).
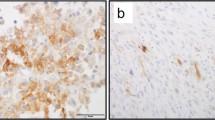
We then compared the peripheral CD4+CXCR5+ T cells in 38 OS cases and 42 controls. As presented in Fig. 1a, upregulated percentage of circulating CD4+CXCR5+ T cells was observed in OS patients than in controls (mean ± SEM 13.9 ± 0.7 % vs. 8.6 ± 0.4 %, p < 0.001). Similarly, absolute number of these cells was also elevated in patients (p < 0.001). It has been reported that peripheral CD4+CXCR5+ T cells can be divided into different subtypes including Th1 (CXCR3+CCR6−), Th2 (CXCR3−CCR6−), and Th17 (CXCR3+CCR6+); we therefore analyzed the levels of these three subtypes in patients and controls (Fig. 1b, e). Data showed that Th1, Th2, and Th17 subtypes of peripheral CD4+CXCR5+ T cells accounted for 3.0, 2.5, and 2.4 % of CD4+ T cells in healthy donors, respectively (Fig. 1b), whereas these cell subtypes in OS patients accounted for 2.7, 4.6, and 5.2 % of CD4+ T cells (Fig. 1b). Th1 subtype was slightly decreased in patients than in controls (p = 0.154, Fig. 1c). However, Th2 (Fig. 1d) and Th17 (Fig. 1e) subtypes were significantly elevated in OS patients (1.86-fold, p < 0.001, and 2.15-fold, p < 0.001, respectively). These data suggest a dysregulation of peripheral CD4+CXCR5+ T cells in OS, and indicate a potential involvement of these cells in the malignancy. To further understand the correlation between peripheral CD4+CXCR5+ T cells and OS, we compared levels of these cells in patients with different tumor locations (Fig. 2). However, no significant difference was found in levels of peripheral CD4+CXCR5+ T cells or its subsets between patients whose tumors were in long tubular bones and in axial skeleton (Fig. 2). In addition, we analyzed CD4+CXCR5+ T cells in OS patients with different pathological fracture statuses, and data revealed no significant differences (p > 0.05).
Peripheral CD4+CXCR5+ T cells in OS cases with metastasis
OS often spreads to the lungs, but it can also spread to other bones, the brain, or other organs. Patients with metastasis are harder to treat and indicate poor prognosis. We analyzed levels of peripheral CD4+CXCR5+ T cells in patients with or without metastasis (Fig. 3). Results revealed that percentage of these cells significantly elevated in metastatic OS patients (17.4 ± 1.3 % vs. 12.7 ± 0.8 %, p = 0.004, Fig. 3a). Further, we investigated changes in the subtypes of peripheral CD4+CXCR5+ T cells in regard to metastasis. Interestingly, Th1 and Th17 but not Th2 revealed a significant augment in metastatic patients (Fig. 3b, d). These results suggest that peripheral CD4+CXCR5+ T cells may be associated with the metastasis of OS.
Peripheral CD4+CXCR5+ T cells in OS cases with different grades
High-grade OSs are the fastest growing types of OS such as osteoblastic, chondroblastic, small cell, etc. Patients with high-grade OSs have rapid disease progression and indicate poor prognosis. We analyzed levels of peripheral CD4+CXCR5+ T cells in patients with different grades (Fig. 4). Results revealed that percentage of these cells significantly elevated in high-grade OS (15.3 ± 0.8 % vs. 11.0 ± 1.1 %, p = 0.006, Fig. 4a). Also, we investigated changes in the subtypes of peripheral CD4+CXCR5+ T cells in regard to tumor grades. Again, Th1 and Th17 but not Th2 revealed a significant augment in high-grade OSs (Fig. 4b, d). These results suggest that peripheral CD4+CXCR5+ T cells may be associated with the progression of OS.
Discussion
In the current study, we, for the first time, investigated peripheral CD4+CXCR5+ T cells in osteosarcoma and identified elevated proportion of these cells in the disease. Further analysis displayed a profound skewing of peripheral CD4+CXCR5+ T cell subsets toward Th2 and Th17 cells in patients compared to controls. Interestingly, we also observed positive correlation between peripheral CD4+CXCR5+ T cells and tumor metastasis or high grade, in which the skewing was contributed by Th1 and Th17 subsets. Our study suggests that peripheral CD4+CXCR5+ T cells may be involved in the pathogenesis and progression of osteosarcoma.
Peripheral CD4+CXCR5+ T cells share functional properties with Tfh cells and appear to represent their circulating memory compartment [16]. Tfh cells have diverse functions in human bodies. They can induce B-cell-mediated systemic autoimmunity and provide great assistance to B cells with respect to the formation of GC in humoral immunity. It is possible that the best-characterized B-cell helper signal offered by Tfh cells is CD40L, which can induce proliferation and activation of B cells [21]. Secreting cytokines is another important pathway by which Tfh cells regulate B-cell responses. Tfh cells are characterized by expressing IL-21, a cytokine capable of modulating B-cell proliferation, differentiation, and GC responsiveness [22]. More importantly, researchers have reported that IL-21 plays critical roles in the development of cancers and is considered as a therapy for some tumors. Recent study has shown that administrating a plasmid DNA encoding murine IL-21 can cause high systemic levels of IL-21 and may slow down the growth of tumor in mice with fibrosarcoma or B16 melanoma. Since peripheral CD4+CXCR5+ T cells in blood also reveal high capacity of producing IL-21, it is reasonable that Tfh may modulate the development and progression of cancers through IL-21 pathway. In osteosarcoma, we identified increased level of peripheral CD4+CXCR5+ T cells. It would be interesting to conduct further experiments on the correlation between these cells and IL-21 in the OS patients.
Peripheral CD4+CXCR5+ T cells can be divided into three major subsets: Th1, Th2, and Th17 cells. These subsets are defined based on the expression of chemokine receptors, expression of transcription factors, and the type of cytokine secretion patterns. Th1 subset does not excrete IL-21 and lack the ability to assist in naive B cells [16]. Th2 and Th17 cells within CD4+CXCR5+ compartment efficiently induce naive B cells to produce immunoglobulins and to switch isotypes through IL-21 secretion. While CXCR5+ Th2 cells promote IgG and IgE secretion, CD4+CXCR5+ Th17 cells are efficient at promoting IgG and, in particular, IgA secretion. Our data demonstrated that Th2-Tfh and Th17-Tfh cells were significantly increased in OS cases (Fig. 1d), indicating that IL-21-mediated immune responses may play a critical role in the development of OS. In addition, we observed that Th-1 subset presented the highest percentages and Th-17 subset presented the lowest percentages in healthy controls. However, the ratio was totally reversed in patients, in which Th-17 cells revealed the highest level. These data suggest a profound dysregulation of peripheral Tfh in OS.
Studies have shown that peripheral CD4+CXCR5+ T cells might provide diagnostic and/or prognostic biomarkers in human autoimmune diseases and cancers. Cha et al. have reported that the proportion of peripheral CD4+CXCR5+ T cells in CD4+ T cells is correlated with Binet stages in chronic lymphocytic leukemia [23]. Our results also demonstrated an elevated level of peripheral CD4+CXCR5+ T cells in OS patients with metastasis (Fig. 3) or high grade (Fig. 4). Although the skewing of peripheral CD4+CXCR5+ T cell subsets was toward Th2 and Th17 cells in patients compared to controls, patients with metastasis or high grade revealed significantly higher proportion of Th1 and Th17 subsets than those with localized OS or low grade (Figs. 3 and 4), indicating different roles of peripheral CD4+CXCR5+ T cell subsets in the pathogenesis and progression of OS. A recent study reported that CCR7(lo)PD-1(hi) CXCR5+ CD4+ T cells indicate Tfh cell activity and promote antibody responses upon antigen reexposure, suggesting a novel subset of peripheral Tfh [24]. It would be interesting to perform researches on these cells and OS.
In summary, this is the first report investigating peripheral CD4+CXCR5+ T cells in OS. The study identified increased frequency of these cells in the disease, especially in patients with metastasis or high grade. Also, a profound skewing of CD4+CXCR5+ T cell subsets was observed in OS patients. These findings would be useful to defining pathogenesis of OS and identifying potential targets for therapeutic action.
References
Schwab JH, Springfield DS, Raskin KA, Mankin HJ, Hornicek FJ. What’s new in primary bone tumors. J Bone Joint Surg Am. 2012;94:1913–9.
Szuhai K, Cleton-Jansen AM, Hogendoorn PC, Bovée JV. Molecular pathology and its diagnostic use in bone tumors. Cancer Genet. 2012;205:193–204.
Arndt CA, Rose PS, Folpe AL, Laack NN. Common musculoskeletal tumors of childhood and adolescence. Mayo Clin Proc. 2012;87:475–87.
Crotty S. Follicular helper CD4 T cells (T(FH)). Annu Rev Immunol. 2011;29:621–63.
Johnston RJ, Poholek AC, DiToro D, Yusuf I, Eto D, Barnett B, et al. Bcl6 and Blimp-1 are reciprocal and antagonistic regulators of T follicular helper cell differentiation. Science. 2009;325:1006–10.
Ma CS, Suryani S, Avery DT, Chan A, Nanan R, Santner-Nanan B, et al. Early commitment of naive human CD4(+) T cells to the T follicular helper (T(FH)) cell lineage is induced by IL-12. Immunol Cell Biol. 2009;87:590–600.
Kissin MW, Querci della Rovere G, Easton D, Westbury G. Risk of lymphoedema following treatment of breast cancer. Br J Surg. 1986;73:580–4.
Giuliano AE, Dale PS, Turner RR, Morton DL, Evans SW, Krasne DL. Improved axillary staging of breast cancer with sentinel lymphadenectomy. Ann Surg. 1995;222:394–9.
Veronesi U, Paganelli G, Galimberti V, Viale G, Zurrida S, Bedoni M, et al. Sentinel-node biopsy to avoid axillary dissection in breast cancer with clinically negative lymph-nodes. Lancet. 1997;349:1864–7.
You Z, Ouyang H, Lopatin D, Polver PJ, Wang CY. Nuclear factor-kappa B-inducible death effector domain-containing protein suppresses tumor necrosis factor-mediated apoptosis by inhibiting caspase-8 activity. J Biol Chem. 2001;276:26398–404.
Zhang HG, Hyde K, Page GP, Brand JP, Zhou J, Yu S, et al. Novel tumor necrosis factor alpha-regulated genes in rheumatoid arthritis. Arthritis Rheum. 2004;50:420–31.
Zhang C, Chakravarty D, Sakabe I, Mewani RR, Boudreau HE, Kumar D, et al. Role of SCC-S2 in experimental metastasis and modulation of VEGFR-2, MMP-1, and MMP-9 expression. Mol Ther. 2006;13:947–55.
Laliberte B, Wilson AM, Nafisi H, Mao H, Zhou YY, Daigle M, et al. TNFAIP8: a new effector for Galpha(i) coupling to reduce cell death and induce cell transformation. J Cell Physiol. 2010;225:865–74.
Inoue T, Hagiyama M, Enoki E, Sakurai MA, Tan A, Wakayama T, et al. Cell adhesion molecule 1 is a new osteoblastic cell adhesion molecule and a diagnostic marker for osteosarcoma. Life Sci. 2013;92:91–9.
Shatz M, Menendez D, Resnick MA. The human TLR innate immune gene family is differentially influenced by DNA stress and p53 status in cancer cells. Cancer Res. 2012;72:3948–57.
Baumhoer D, Smida J, Zillmer S, Rosemann M, Atkinson MJ, Nelson PJ, et al. Strong expression of CXCL12 is associated with a favorable outcome in osteosarcoma. Mod Pathol. 2012;25:522–8.
Gu-Trantien C, Loi S, Garaud S, Equeter C, Libin M, de Wind A, et al. CD4+ follicular helper T cell infiltration predicts breast cancer survival. J Clin Invest. 2013;123:2873–92.
Lim HW, Kim CH. Loss of IL-7 receptor alpha on CD4+ T cells defines terminally differentiated B cell-helping effector T cells in a B cell-rich lymphoid tissue. J Immunol. 2007;179:7448–56.
Ame-Thomas P, Maby-El Hajjami H, Monvoisin C, Jean R, Monnier D, Caulet-Maugendre S, et al. Human mesenchymal stem cells isolated from bone marrow and lymphoid organs support tumor B-cell growth: role of stromal cells in follicular lymphoma pathogenesis. Blood. 2007;109:693–702.
Linterman MA, Pierson W, Lee SK, Kallies A, Kawamoto S, Rayner TF, et al. Foxp3(+) follicular regulatory T cells control the germinal center response. Nat Med. 2011;17:975–82.
Chung Y, Tanaka S, Chu F, Nurieva RI, Martinez GJ, Rawal S, et al. Follicular regulatory T cells expressing Foxp3 and Bcl-6 suppress germinal center reactions. Nat Med. 2011;17:983–8.
Clear AJ, Lee AM, Calaminici M, Ramsay AG, Morris KJ, Hallam S, et al. Increased angiogenic sprouting in poor prognosis FL is associated with elevated numbers of CD163+ macrophages within the immediate sprouting microenvironment. Blood. 2010;115:5053–6.
Cha Z, Zang Y, Guo H, Rechlic JR, Olasnova LM, Gu H, et al. Association of peripheral CD4+ CXCR5+ T cells with chronic lymphocytic leukemia. Tumour Biol. 2013;34:3579–85.
He J, Tsai LM, Leong YA, Hu X, Ma CS, Chevalier N, et al. Circulating precursor CCR7(lo)PD-1(hi) CXCR5+ CD4+ T cells indicate Tfh cell activity and promote antibody responses upon antigen reexposure. Immunity. 2013;39:770–81.
Acknowledgments
This work was supported by the grants from the Natural Science Foundation of China (Nos. 81271982 and 81071498) and the key project of Chinese Ministry of Health (No. 201002018).
Conflicts of interest
No competing financial interests exist.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xiao, H., Luo, G., Son, H. et al. Upregulation of peripheral CD4+CXCR5+ T cells in osteosarcoma. Tumor Biol. 35, 5273–5279 (2014). https://doi.org/10.1007/s13277-014-1686-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-1686-6