Abstract
Glioblastoma is known as one of the most aggressive human cancers. To gain access of the brain, therapeutic agents must overcome blood–brain barrier (BBB). In this study, Cisplatin (Cispt)-loaded polybutylcyanoacrylate (PBCA) nanoparticles (NPs) were prepared through miniemulsion polymerization technique. They were coated with polysorbate 80 to cross the BBB of glioblastoma-bearing rats. Prepared NPs were characterized with respect to their size, size distribution, zeta potential, drug loading and encapsulation efficiency, cytotoxicity effects, drug release, and stability pattern. Size and zeta potential of nanodrug were found to be 489 nm and −20 mV, while drug loading and encapsulation efficiency were determined to be 5 % and 25 %, respectively. Release studies demonstrated high retention capability of nanodrug in that 3.18 % of Cispt was released from NPs in a period of 51 h. NPs presented acceptable stability after 2 months and lyophilization. Mean survival time in nanodrug receivers was 19.6 days, while it was 17.5 days for free drug receivers. Histological studies demonstrated efficacy of PBCA NPs in reducing side effects. Finally, such preparation can be considered as a promising nanocarrier for other types of tumor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Presently, treatment of glioblastoma multiforme tumors is a challenging issue due to the fact that median survival time of patients is less than 1 year [1]. For such tumors, chemotherapy fails owing to the existence of blood–brain barrier (BBB) [2]. BBB separates brain extracellular flow from the blood in the central nervous system (CNS). It is formed by endothelial cells connected by tight junctions that only allow transport of molecules essential for functional activities of brain and limit transport of therapeutic agent [3]. BBB inhibits transport of 100 % of large-molecule and 98 % of small-molecule drugs [4, 5]. As a result, finding an effective approach for facilitated transport of drugs and improving bioavailability of therapeutics look indispensable [2]. Different strategies have been tried to permit drugs to pass BBB. Such techniques are ranged from invasive strategies like disruption and osmotic opening to biological or chemical modification [6, 7]. Among such various approaches, using polymeric nanoparticles (NPs) is a promising strategy. NPs are capable of entrapping several BBB-impermeable drugs and delivering them to brain in original characteristics [3, 8]. In addition to overcoming BBB, NPs have some unique features such as biological and chemical stability, protecting drug against chemical and enzymatic degradation, controlled and sustained drug release, effective drug accumulation, possibility of targeted delivery, and reducing side effects and toxicity for peripheral organs [6, 9, 10]. Among several NPs used for brain delivery system, polybutylcyanoacrylate (PBCA) nanocarriers have demonstrated promising features [1, 8, 11] due to properties such as small size, simplicity of synthesize, purification and scale up, easy penetration to capillaries, in vitro stability as well as rapid elimination from body because of low molecular weight and successful delivery of functional proteins to neurons and neuronal cell lines [6, 8].
Cispt (PtII (NH3)2) Cl2 is an extremely effective anticancer drug with extensive application in treatment of solid tumors such as brain tumor. In spite of high cure rates, it has several side effects including nephrotoxicity, weight loss, diarrhea, vomiting, and nausea [11, 12]. PBCA nanoparticles were used in this study to evaluate their capability to cross the blood–brain barrier and deliver Cispt to brain tumor.
In the present study, we aimed at synthesizing Cispt-loaded PBCA NPs as well as evaluating in vitro and in vivo potential of the system in brain drug delivery. Cispt-PBCA NPs were synthesized by miniemulsion polymerization. We have also used honey and olive oil because of their attractive properties including stabilizing, surfactant, and anti-cancer activity [13, 14].
Materials and methods
Materials
Butylcyanoacrylate monomer was purchased from Evobond®Tong Shen Enterprise Co., Ltd. (Taiwan). Dextran was obtained from Zhejiang Chemicals Import and Export Corporation (China). Hydrogen chloride, sodium hydroxide, mannitol, and Cispt were purchased from Zhechem (China). Polysorbate 80 and polyethylene glycol were obtained from Sigma (USA) and Kimiagaran Emrooz Chemical Ind. (Iran), respectively. All other materials were from analytical grade. Deionized water was used throughout the study. C6 cell lines were supplied by the Pasteur Institute of Iran.
Preparation of NPs
Preparation of NPs was carried out by miniemulsion polymerization method. Two hundred microliter butylcyanoacrylate monomers was added to mixture of 100 μl HCl (0.01 N), 50 μl olive oil (Faraz Rahbar Saba Co. Iran), 100 mg honey (Sabalan Co. Iran), and 100 μl polyethylene glycol 400. Afterward, 150 mg dextran and 60 mg Cispt were added and mixed. Then, 20 ml distillated water was added and stirred (400 rpm) for 10 min in order to obtain pre-emulsion solution. Finally, it was sonicated (Bandelin Sonopuls HD 2070, Bandelin Elec., Germany) for 5 min (50 W) and stirred for 3 h (150 rpm) to complete the polymerization process. After 3 h, the mixture was neutralized with NaOH.
Coating Cispt-PBCA NPs with polysorbate 80
Lyophilized powder of Cispt-PBCA NPs was added to PBS containing 1 % polysorbate 80 in which final concentration of Cispt reached to 0.5 mg/ml. Resultant suspension was stirred for 30 min and injected to animals in 2 h.
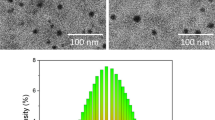
Characterization of NPs
Mean size, size distribution, and zeta potential of particles were determined by Zetasizer (Nano-Zs Zen 3600, Malvern instruments, UK). Morphology of NPs was studied by scanning electron microscope (XL30, Philips, Netherlands) after adding mannitol solution (200 mg/ml) and lyophilization (Edwards High Vacuum, Manor Royal, Crawley, Sussex, England). Cispt was analyzed by Fourier transform infrared spectroscopy (FTIR) to determine type of loading (chemical or physical). For this purpose, the suspension of the drug was centrifuged, and the supernatant was removed. Resultant was dried in room temperature, and bromide potassium tablet was prepared and analyzed by FTIR (Nicolet 740SX FTIR spectrophotometer with an MCT-B detector (USA)).
Determining drug loading and encapsulation
In order to determine drug loading efficiency and encapsulation, two below formulas were used. For this purpose, emulsion of NPs was centrifuged at 21,000 rpm and 4 °C for 50 min. Amount of drug in supernatant was recognized by ICP-EOS (Inductively Coupled Plasma Optical Emission Spectrometry) elemental analysis (730-OES, Varian).
In vitro study of drug release
Seventy-five milligrams of centrifuged drug-loaded NPs was redispersed in 7.5-ml fresh human serum in a capped centrifuge tube. Tube was incubated at 37 °C and shaken in a 120 cycles/min shaker incubator (Kühner, Birsfelden, Switzerland). At the predetermined times, tube was centrifuged (21,000 rpm, 4 °C for 50 min), and supernatant was removed. Collected NPs were again redispersed in 7.5 fresh human sera for continuous release study. The released Cispt in supernatant was determined by ICP-EOS elemental analysis.
In vitro cytotoxicity of nanocapsulated Cispt
Cytotoxicity of Cispt loaded into PBCA NPs was determined by MTT assay on C6 cell line. Cells were seeded in a 96-well plate at a density of 1 × 104 and cultivated with 5 % CO2 at 37 °C in RPMI-1640 culture medium containing 10 % fetal bovine serum and 1 % penicillin/streptomycin antibiotics. They were allowed to attach for 24, 48, 72, and 96 h. After removing supernatant, cells were treated with free Cispt and Cispt-loaded NPs in concentrations of 0, 5, 10, and 20 μM. Cytotoxicity was evaluated after 24 h incubation. Absorbance was measured at 570 nm by Elisa reader (BioTek Instruments, VT, USA). IC50 amount was determined by statistical package Pharm-PCS software.
Evaluating stability of NPs
Resultant NPs were suspended in PBS (0.02 M, pH 7.4) again after lyophilization. Size and size distribution were evaluated, and stability was determined by studying cell toxicity with MTT assay and C6 cell line. Two months after preparing nanodrug, MTT assay was repeated for concentrations of 0, 5, 10, and 20 μM of nanodrug and free drug. Results were compared with MTT results of the first days.
In vivo toxicity of blank NP
To assess NP toxicity, nine male Wistar rats (250–350 g) were selected. Animals were obtained from Pasteur Institute (Karaj). Throughout the experiments, all rats had ad libitum access to food and water. They were housed in a controlled environment with 12 h dark/light cycle. After 1 week, blank NPs (20 mg/kg) in PBS (0.02 M, pH 7.4) were injected to six rats, while PBS was injected intraperitoneally to others considered as control group. Weight changes in both groups were evaluated for a period of 1 month every 3 days.
In vivo antitumor efficacy of Cispt-PBCA NPs
In 18 male rats (200–250 g), the tumor was formed by injecting C6 cells (50,000 cells in 10 μl of PBS) into the frontal lobe of skull according to Miura et al. [15].
Animals with tumors were randomly divided into three groups (n = 6). The groups received the following formulations: Cispt-PBCA NPs coated with PS 80, free Cispt dissolved in distilled water, and untreated control group.
Cispt products were injected intraperitoneally at dose of 1 mg/kg, 2, 5, 8, and 11 days after cancerous cell injection with 72-h intervals. Antitumor efficacy of the drug in different formulations was analyzed by measuring the lifetime of different groups. Two animals from each group were randomly selected, and organs such as brain, kidneys, and liver were evaluated macroscopically and histologically.
Histological analysis
Successive sections of paraffin embedded tissue were prepared for hematoxylin and eosin staining. Assessment of organ toxicity was carried out by a semiquantitative scoring system [16]. Toxicity of organs was estimated as 0 in case of no toxicity symptom, 1 as observing any slight change, and 2 for medium change in organs.
Statistical analysis
SPSS version 13.0 software was employed for statistical analysis of data, and P < 0.05 was considered significant.
Result and discussion
Characterization of NPs
In this study, we succeeded to synthesize PBCA NPs containing high level of Cispt, which confirmed miniemulsion polymerization as an appropriate method. The experiment was performed three times. Results showed that trial had sufficient validity and reliability. Additionally, honey and olive oil were used in preparation of NPs for the first time. They were chosen since they have excellent biocompatibility and low toxicity. In addition, they are found abundant in nature. It has been demonstrated that honey has positive effects on the nanoparticle properties [17, 18]. Sreelakshmi et al. reported that gold and silver NPs coated with honey represent superlative antimicrobial activity [17]. The positive effects of honey on the carbon nanoparticles were also demonstrated by Wu et al. where naked carbon NPs were derived from commercial food grade honey. These nanoparticles represented rapid signal enhancement in imaging sentinel lymph nodes [18]. These observations were also reported about olive oil [19]. After adding water and sonication, polymerization occurred, and the color of medium changed from nearly colorless to milky color, which was completed after sonication. Blank PBCA NPs had a size, size distribution, and zeta potential of 373 nm, 0.429, and −28 mV (Fig. 1), while it was 489.3 nm, 0.429, and −20 mV for Cispt-PBCA NPs (Fig. 2). As expected, loading drug into NPs led to an increase in size from 373 to 489 nm and reduction in stability. The entrapment efficiency was estimated 25 %. In the other words, 25 % of used drug was associated with NPs. Drug loading was estimated to be 5 %.
FTIR results demonstrated no change in the chemical structure of Cispt. Platinum and ammonium bond emerged in 463 cm−1 and platinum and chloride in 338 cm−1 and 362 cm−1. Tensional trembles of ammonium groups emerged in 1,550 cm−1, 1,680 cm−1, 3,300 cm−1, and 3,500 cm−1 [20, 21]. As represented in Fig. 3, Cispt chemical bonds did not alter. In other words, drug was entrapped and loaded onto NP physically.
In vitro release study
Cumulative release rate of Cispt from Cispt-PBCA NPs was presented in Fig. 4. It was found that NPs have a high drug retention capability in that only 3.18 % (W/W) of drug was released after 51 h. However, in the first 3 h of evaluation, a burst release (34 % of total release) of drug was observed. This event probably reflects the release of adsorbed drug on the surface of NPs. Release rate decreased with time so that at the last time interval with approximately 22 h, only 0.35 % of drug was released. It is probable that the presence of polyethylene glycol has led to low level of release. It also resulted in improving stability and increasing probability of drug delivery to tumor and increasing efficiency as a result [22].
Release pattern of Cispt from Cispt-PBCA NPs synthesized by miniemulsion polymerization. Pattern is presented as percentage of release in different time intervals. An initial burst release occurred and was followed with a steady trend. Release rate decreases with time in which at the last time interval (22 h), only 0.35 % of drug was released
In vitro cytotoxicity of nanocapsulated Cispt
The safe concentration of control NPs was estimated to be 40 μg/ml. Other studies have identified higher safe concentrations of these NPs [23]. Cytotoxicity of Cispt-PBCA NPs in comparison with free drug is illustrated in Fig. 5.
IC50 (μM) of free Cispt and Cispt-PBCA NPs synthesized by miniemulsion polymerization in different time intervals. As the figure shows, the highest and lowest cytotoxicity difference between free Cispt and Cispt-loaded NP occurs at 24 h and 96 h, respectively. Cispt cytotoxicity increases with time. Results are presented as mean ± 5 % error from three independent tests
As presented by results, no considerable change in cytotoxicity was observed and IC50 was estimated to be 8, 7, 6.7, and 6.5 μM (Fig. 5), which verifies continuous release. Cytotoxicity results largely coincide with the release curve. While maximum release occurred in the first 24 h, highest cytotoxicity was also observed at this time. In the first 24 h, the cytotoxicity was approximately 4 times that of free Cispt. Downward trend was continued after 96 h free drug demonstrated higher level of toxicity. IC50 amount was 6.5 μM for nanodrug and 4 μM for free drug after 96 h.
Evaluating stability of NPs
Results of zeta sizer tests confirmed stability of lyophilized NPs. Alteration in size and size distribution after lyophilization were negligible.
Also, MTT results verified stability as cytotoxicity after 2 months was not changed considerably compared with the first day (Fig. 6). One of the problems related to Cispt is poor stability of drug [24] that could be resolved when loaded onto PBCA nanoparticle.
In vivo toxicity of blank NPs
Figure 7 demonstrates weight changes for blank NPs as well as control group of animals kept beside the blank NP-bearing animals, respectively. As indicated in the figure, there is not any considerable weight change in control NP receivers, and they showed weight changes similar to control group. Other studies demonstrated safety of higher concentrations [25].
As presented in Fig. 7, no considerable weight change was observed in both groups. Therefore, individual PBCA NPs cannot influence weight and survival time of rats, and consequently changes in weight and survival of animals can just come from drug in free or NP form.
In vivo antitumor efficacy of Cispt-PBCA NPs
Malignant glioblastoma is one of the most aggressive cancers. Despite extensive improvements in neurosurgical techniques, chemotherapy, and radiotherapy [26–28], there is no effective treatment for these tumors yet. Failing chemotherapy in treatment of brain tumors is due to existence of blood–brain barriers, which inhibits passage of 98 % of therapeutic molecules. Nanotechnology is one of the most promising ways of overcoming this barrier [4].
The main criterion in evaluating efficacy of the drug was survival time, and concentration of drug was based on previous studies [29]. Initially, it was found that mean survival time of rats with tumor is 16 days. Previously, Parsa et al. reported survival time less than 30 days [30]. Due to immunogenicity properties of C6 cells [31], tumor was not formed in one of the rats receiving Cispt in free form. Mean survival time was 17.5 days and 19.6 days for Cispt-PBCA and free drug receivers, respectively (Fig. 8).
Weight changes in free drug receivers were more severe compared with nanodrug receivers. As the graph shown in Fig. 9, it can be observed that free drug animals faced more weight changes as well as longer time between emerging symptoms and death. In other words, drugs can cause an increase in survival time in case of passing BBB; however, nanodrugs failed to pass BBB. It is probable that by reducing the size of NPs, they can pass BBB and improve survival time. However, the exact mechanism—by which this NP works—is unknown yet. Several proposals have been presented in this regard. One of them was using polysorbate 80 as endocytosis receptor via endothelial cells of the brain. Polysorbate 80 prefers absorption of apolipoprotein E in plasma. NPs coated with apolipoprotein E are identified as LDL, and they are absorbed into the brain [32]. It has been suggested that PBCA NPs coated with polysorbate 80 exert a toxic effect on the brain capillaries and cause unfolding of strong ties [33]. Our study indicated inefficiency of such NPs in passing BBB. Furthermore, auxiliary role of doxorubicin in overcoming glycoprotein pump is identified [34]. It forms pair ion with product of PBCA degradation, which is able to pass through the membrane without being followed by glycoprotein pump [32]. Further studies are necessary for confirmation of this matter.
Graph of weight changes over time in the group receiving free Cispt (right) and Cispt loaded onto nanoparticles (left). As the graph shows, initiation of illness signs till death is longer in the free Cispt receivers compared to nanodrug receivers. Moreover, at this time, weight loss is more severe in Cispt receivers
Histological studies performed by hematoxylin and eosin staining of tumor demonstrated less bleeding in free drug receivers (Fig. 10). Although nanodrug showed poor ability of passing, histological studies confirmed less damage of liver and kidney in group of nanodrug receivers (Table 1).
Results show that acute tubular necrosis (ATN) and liver necrosis were more prevalent in nanodrug receivers (Fig. 11).
Reducing in vivo side effects and in vitro toxicity of nanodrug suggests its efficacy for other tumors like breast cancer [35]. At the present time, the efficacy of this formulation was experienced on the treatment of breast cancer-bearing mouse.
Conclusion
In this study, miniemulsion polymerization was determined as an appropriate method for synthesizing Cispt-PBCA NPs. NP properties such as size, size distribution, drug release, cytotoxicity, and stability were investigated and confirmed to be acceptable. Honey and olive oil were used as anticancer surfactants, which led to improving efficacy. Using PEG resulted in higher stability and slower release.
Although nanodrugs demonstrated less efficacy compared with free drug, reducing in vivo side effects suggests applying them for treating other tumors. Surface modification and size reduction may lead to success in passing BBB.
References
Beduneau A, Saulnier P, Benoit J. Active targeting of brain tumors using nanocarriers. Biomaterials. 2007;28:4947–67.
Tian XH, Lin XN, Wei F, Feng W, Huang ZC, Wang P, et al. Enhanced brain targeting of temozolomide in polysorbate-80 coated polybutylcyanoacrylate nanoparticles. Int J Nanomedicine. 2011;6:445–52.
Chakraborty C, Sarkar B, Hsu C, Wen Z, Lin C, Shieh P. Future prospects of nanoparticles on brain targeted drug delivery. J Neurooncol. 2009;93:285–6.
Pardridge W. Blood–brain barrier delivery. Drug Discov Today. 2007;12:54–61.
Wolburg H, Lippoldt A. Tight junctions of the blood–brain barrier: development, composition and regulation. Vascul Pharmacol. 2002;38:323–37.
Masserini M. Nanoparticles for brain drug delivery. ISRN Biochem. 2013;2013:18.
Garcia-Garcia E, Andrieux K, Gilb S, Couvreur P. Colloidal carriers and blood–brain barrier (BBB) translocation: a way to deliver drugs to the brain? Int J Pharm. 2005;298:274–92.
Koffie R, Farrar C, Saidi L, William C, Hyman B, Spires-Jones T. Nanoparticles enhance brain delivery of blood–brain barrier-impermeable probes for in vivo optical and magnetic resonance imaging. Proc Natl Acad Sci U S A. 2011;108:18837–42.
Hasadsri L, Kreuter J, Hattori H, Iwasaki T, George JM. Functional protein delivery into neurons using polymeric nanoparticles. J Biol Chem. 2009;284:6972–81.
Dikpati A, Madgulkar AR, Kshirsagar SJ, Bhalekar MR, Singh Chahal A. Targeted drug delivery to CNS using nanoparticles. JAPS. 2012;2:179–91.
De Jonghe B, Horn C. Chemotherapy agent cisplatin induces 48-h Fos expression in the brain of a vomiting species, the house musk shrew (Suncus murinus). Am J Physiol Regul Integr Comp Physiol. 2009;296:902–11.
Wilson JJ, Lopes JF, Lippard SJ. Synthesis, characterization, and photophysical properties of three platinum(II) complexes bearing fluorescent analogues of the Di-2-pyridylmethane ligand. Inorg Chem. 2010;49:5303–15.
Savrikar S, Lagad C. Study of preparation and standardization of ‘Maadhutailika Basti’ with special reference to emulsion stability. Ayu. 2010;31:1–6.
Fontes G, Amaral P, Nele M, Coelho M. Factorial design to optimize biosurfactant production by Yarrowia lipolytica. J Biomed Biotechnol. 2010;2010:1–8.
Miura F, Alves M, Rocha M, Silva R, Oba-Shinjo S, Uno M, et al. Experimental model of C6 brain tumors in athymic rats Arq. Neuro-Psiquiatria. 2008;66:238–41.
Steiniger SC, Kreuter J, Khalansky AS, Skidan IN, Bobruskin AI, Smirnova ZS, et al. Chemotherapy of glioblastoma in rats using doxorubicin-loaded nanoparticles. Int J Cancer. 2004;109:759–67.
Sreelakshmi C, Datta KK, Yadav JS, Reddy BV. Honey derivatized Au and Ag nanoparticles and evaluation of its antimicrobial activity. J Nanosci Nanotechnol. 2011;11:6995–7000.
Wu L, Cai X, Nelson K, Xing W, Xia J, Zhang R, et al. A green synthesis of carbon nanoparticle from honey for real-time photoacoustic imaging. Nano Res. 2013;6:312–25.
Palanisamy KL, Meenakshi Sundaram N, Devabharathi V, Thangarasu P. Synthesis and characterization of olive oil mediated iron oxide nanoparticles. Dig J Nanomater Bios. 2013;2:607–12.
Yan X, Gemeinhart RA. Cisplatin delivery from poly (acrylic acid-co-methyl methacrylate) microparticles. J Control Release. 2005;106:198–208.
Ebrahimi Shahmabadi H, Akbarzadeh A, Mokhtari MJ, Mortazavi M, Ghasemi S, Mohammadi H, et al. In vitro evaluation of the effects of acetone, on the potency of cisplatin: is it a good candidate for cisplatin carrier preparation? E3 J Biotechnol Pharm Res. 2012;3:137–40.
Otsuka H, Nagasaki Y, Kataoka K. PEGylated nanoparticles for biological and pharmaceutical applications. Adv Drug Deliv Rev. 2012;64:246–55.
Duan J, Zhang Y, Han S, Chen Y, Li B, Liao M, et al. Synthesis and in vitro/in vivo anti-cancer evaluation of curcumin-loaded chitosan/poly (butyl cyanoacrylate) nanoparticles. Int J Pharm. 2010;400:211–20.
Macka M, Borák J, Seménková L, Kiss F. Decomposition of cisplatin in aqueous solutions containing chlorides by ultrasonic energy and light. J Pharm Sci. 1994;83:815–8.
Kante B, Couvreur P, Dubois-Krack G, De Meester C, Guiot P, Roland M, et al. Toxicity of polyalkylcyanoacrylate nanoparticles I: free nanoparticles. J Pharm Sci. 1982;71:786–90.
De Angelis LM. Brain tumours. N Engl J Med. 2001;344:114–23.
Nelson DF, Nelson JS, Davis DR, Chang CH, Griffin TW, Pajak TF. Survival and prognosis of patients with astrocytoma with atypical or anaplastic features. J Neurooncol. 1985;3:99–103.
Kornblith PL, Walker M. Chemotherapy for malignant gliomas. J Neurosurg. 1998;68:1–17.
Gao H, Yang Z, Zhang S, Cao S, Shen S, Pang Z, et al. Ligand modified nanoparticles increases cell uptake, alters endocytosis and elevates glioma distribution and internalization. Sci Rep. 2013;3:2534.
Parsa AT, Chakrabarti I, Hurley PT, Chi JH, Hall JS, Kaiser MG, et al. Limitations of the C6/Wistar rat intracerebral glioma model: implications for evaluating immunotherapy. Neurosurgery. 2000;47:993–9.
Barth R, Kaur B. Rat brain tumor models in experimental neuro-oncology: the C6, 9L, T9, RG2, F98, BT4C, RT-2 and CNS-1 gliomas. J Neurooncol. 2009;94:299–312.
Petri B, Bootz A, Khalansky A, Hekmatara T, Muller R, Uhl R. Chemotherapy of brain tumour using doxorubicin bound to surfactant-coated Poly(butyl cyanoacrylate) nanoparticles: revisiting the role of surfactants. J Control Release. 2007;117:51–8.
Olivier JC, Fenart L, Chauvet R, Pariat C, Cecchelli R, Couet W. Indirect evidence that drug brain targeting using polysorbate 80-coated polybutylcyanoacrylate nanoparticles is related to toxicity. Pharm Res. 1999;16:1836–42.
de Verdière AC, Dubernet C, Némati F, Soma E, Appel M, Ferté J, et al. Reversion of multidrug resistance with polyalkylcyanoacrylate nanoparticles: towards a mechanism of action. Br J Cancer. 1997;76:198–205.
Silver DP, Richardson AL, Eklund AC, Wang ZC, Szallasi Z, Li Q, et al. Efficacy of neoadjuvant Cisplatin in triple-negative breast cancer. J Clin Oncol. 2010;28:1145–53.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Ebrahimi Shahmabadi, H., Movahedi, F., Koohi Moftakhari Esfahani, M. et al. Efficacy of Cisplatin-loaded polybutyl cyanoacrylate nanoparticles on the glioblastoma. Tumor Biol. 35, 4799–4806 (2014). https://doi.org/10.1007/s13277-014-1630-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-1630-9